Determinants of Alcohol Use Disorder among Residents of Agaro Town, Jimma, Southwest, Ethiopia: A Cross-sectional Study
Received: 15-Dec-2018 / Accepted Date: 28-Jan-2019 / Published Date: 04-Feb-2019 DOI: 10.4172/2155-6105.1000377
Abstract
Introduction: Alcohol use disorder is a common mental disorder that is associated with substantial disease burden around the world. Globally alcohol consumption caused 3.8 percent of all deaths and 4.5 percent of the total burden of disease in 2004. Alcohol use disorder is also a burden for individuals and society in Ethiopia. It is important to identify problematic alcohol use at an early stage, as this provides professionals with the opportunity to take preventive measures and hence, reduce the problems caused by this consumption.
Objective: Assessment of the prevalence and determinants of alcohol use disorder among residents of Agaro town, Jimma, Southwest Ethiopia, 2016.
Method: Community based cross-sectional study was conducted from May-June 2016 among 845 residents living in Agaro town. Multistage sampling technique was used to select study participants and assessed for alcohol use disorder using self-reported questionnaire (AUDIT). The collected data was coded, entered in to EPI-INFO 7 software and analyzed by using SPSS version 20. Logistic regression analyses were computed to determine the association between factors and alcohol use disorder.
Results: With 96.9% of response rate the prevalence of alcohol use disorder was found to be 12.4% with 95% confidence interval (9.3%, 15.8%). The likelihood of alcohol use disorder was higher in males (AOR=4.0 (1.58, 10.49). Also, high level mental distress (AOR=3.8 (1.35, 10.67)), Family history of alcohol use (AOR=3.4 (1.32, 9.17) and smoking cigarette (AOR=4 (1.26, 12.03)) were factors significantly associated with alcohol use disorder in Agaro town.
Conclusion: This study had showed that the prevalence of alcohol use disorder among urban resident of Agro town were significant public health issues that require a great emphasis. This study indicates that alcohol use disorder goes along with use of other substances. Being male sex, family history of alcohol use disorder, history of cigarette smoking and having mental distress symptoms were significantly associated with alcohol use disorder.
Keywords: Alcohol; Alcohol use disorder; Audit
Introduction
Alcoholic beverages are class of organic compounds, containing one or more hydroxyl group (OH) attached to a carbon atom [1]. Ethanol is the only type of alcohol that can be prepared and consumed at a commercial or household level. Nearly in all areas of the world, people prepare and consume some types of alcoholic beverage native to their region [2]. Some individuals do not drink at all; others drink as part of social custom; still others drink frequently and in substantial amounts [3,4].
Alcohol Use Disorder is a condition characterized by the harmful consequences of repeated alcohol use, a pattern of compulsive alcohol use, and (sometimes) physiological dependence on alcohol (i.e., tolerance and/or symptoms of withdrawal). Alcohol use disorders typically start in adolescence and the intensity of the disorder tends to peak between the ages of 20-30 years [5]. The disorder is only diagnosed when these behaviors become persistent and very disabling or distressing [6].
World Health Organization (WHO) estimates that there are about 2 billion people worldwide who consume alcoholic beverages and 76.3 million have a diagnosable alcohol-use disorder [7]. The same report estimates 1.8 million annual deaths and 58.3 millions of Disability Adjusted Life Years (DALYs) attributed to alcohol-use disorder. Alcohol constitutes the largest risk factor for DALYs lost in middle income countries and the third largest in all income group countries [8]. Against the global average of 5.1 L, France, Ireland, Uganda, Luxemburg and Czech Republic are among the top list of adult per capita consumption of alcohol, i.e. >13 L [9].
WHO reports indicated that there is steady increase in its consumption in the South East Asian region. The consumption of alcohol in most Muslim populations and in South Asian countries seems to be lower than in Europe and Americas. However, alcohol consumption is estimated to be at least two thirds of all alcohol consumption is in Latin America, in the Indian subcontinent, in Africa, and about one third in Eastern Europe [10]. Alcohol use disorders are among the most commonly occurring mental disorders and are associated with significant personal and societal costs [11].
Currently, alcohol use disorders ranked fifth most costly mental health condition among one sample of employers in the United States [12]. The calculated total economic cost of alcohol abuse and dependence as 98.6 billion US dollar for 1990 and this figure nearly doubled in less than 10 years [13].
Though preventable, it is clear that alcohol use disorders impose a staggering economic burden on society. In addition, people with alcohol use disorders engage in behaviors that have adverse effects on themselves and those around them. The risk of mortality is increased among adolescents and young adults who engage in problem drinking [14]. Acute physiological problems like coronary heart disease, stroke, hypertension, liver cirrhosis, and certain cancers can arise as a result of these disorders [3].
WHO report on alcohol-attributable deaths indicated that, 10%-14% in most part of Asian countries, 5% to 9.9% in Latin America, 2% to 4.9% in North America, central and south part of African countries and Ethiopia. Also studies indicate that up to 25% of children with an alcoholic parent will develop alcohol abuse or dependence.
History of smoking cigarette, family history of alcoholism, male sex and high level of mental distress symptoms were significant determinants of alcohol use disorder [15-18].
However, few literatures exists on the magnitude and predictors of AUDs and only a small per cent of people with alcohol use disorder actually seek treatment in south eastern part of Ethiopia. So, the current study aimed to assess the prevalence and determinants of AUDs among residents of Agaro town.
Methods
Study design and study period
Community based cross-sectional study design was conducted from May to June 2016. The study was conducted in Agaro town, Jimma zone which is located in the south-western part of Ethiopia which is 480 km far from Addis Ababa. The town has a total population of 35470 of which 17013 were male and 18457 were female. Agaro town has an estimated 7393 household and five kebeles. There is one governmental hospital and one health center. Both the hospital and health center don't have psychiatry clinic. It also has five health posts and seven private clinics.
Population
All individuals of age 18 years and above reside in Agaro town were considered as source population. Adult age 18years and above who were available during the study period was the study population.
Inclusion and exclusion criteria
Individuals of age 18 years and above in the household permanently reside in the selected kebeles for six month and above. All individuals who are unable to communicate were excluded.
Sample size determination
The sample size was determined by using a single population proportion formula considering the following assumptions: standard normal distribution with confidence interval of 95% (Z=1.96), absolute precision or tolerable margin of error (d=0.05), design effect of 2, since proportion of alcohol use disorder is unknown in Ethiopia (p=50%). So taking 10% non-response rate, the final calculated sample size was 845.
Sampling technique
Multistage sampling technique was used. At stage one from the total five kebeles of the town, three kebeles were selected randomly. Then individual households in the selected Keble were selected using a systematic sampling technique after identifying an initial starting household by use of a random number. The sample size was distributed to each kebeles proportional to the household size of the kebele. From selected kebeles; every 7th household was visited. Adults in the selected household was further selected and interviewed. In case of more than one eligible adult in the household, lottery method was used to select one. For eligible participant which was not be found at home, the interviewers had revisited the household at different intervals and when interviewers failed to get eligible participant, the household was registered as non-respondent rate.
Data analysis
Data entered in to EPi. INFO version 3.1.5 and exported in to SPSS window version 20 for analysis. A Bivarate analysis was performed to determine the effect each of factors on the outcome variable. Only factors with p value <0.2 on bivarate analyses were kept for multivariate logistic regression and a p value <0.05 on multivariate analyses was considered as statistically significant.
Instrument
Alcohol Use Disorder Identification Test (AUDIT) prepared by WHO was used for data collection. The AUDIT was determined to be the best screening instrument for the whole range of alcohol problems in primary care research, in the general population as well as in specific institutional groups such as hospital patients and it has been found to provide an accurate measure of risk across gender, age, and cultures. At a cut-off value 8 points, the sensitivity and specificity of AUDIT was 0.90 and 0.80 respectively. The AUDIT has been translated into both Amharic and Afan Oromo from previous study. Back translation into English was undertaken for both languages and final versions obtained through consensus. The cultural appropriateness of AUDIT was improved by modifying the ‘standard drink’ in question two and three as to be more understandable to participants.
Mental distress was assessed using SRQ-20 whether; the respondents had experienced symptoms associated with emotional distress within 4 weeks before the interview. The tool was developed by WHOM to screen common mental disorder in primary health care setting in low income countries [19].
Operational definition
Alcohol use disorders: AUDIT total score above 8 or equal to 8.
Medium alcohol use disorder (hazardous type of alcohol use disorder): AUDIT total scores 8-15.
Severe alcohol use disorder (harmful alcohol consumption: AUDIT total score 16-19.
Alcohol dependence: AUDIT total score above 20.
Ethical consideration
Ethical clearance was obtained from the Institutional Review Board of University of Gondar and Amanuel Mental Specialized Hospital. The confidentiality of respondents was strictly kept. Before questionnaires administered to the participant, written consent was obtained. Any participants who are not willing to participate in the study were not forced to participate. All study participants who were found to have alcohol use disorder had a detail assessment and appropriate intervention offered.
Results
Out of the total selected 845 participants, 819 were participated in the study with response rate of 96.9%.
Socio-demographic characteristics
Among the total participants 446 (54.5%) were males. The age of the respondents was between 25-34 years 358 (43.7%). The major ethnic group in the study area was Oromo 475 (58%) and Muslim by religion 335(40.9%). 457 (55.7%) study participants were single and 447 (54.1%) had achieved secondary education. According to wealth index assessment 22% of the respondents were found rich (Table 1).
| Variables | Category | Frequency | Percentage (%) |
|---|---|---|---|
| Age | 18-24 | 176 | 21.5 |
| 25-34 | 358 | 43.7 | |
| 35-44 | 201 | 24.5 | |
| 45-54 | 61 | 7.4 | |
| 55 and above | 23 | 2.8 | |
| Sex | Male | 446 | 54.5 |
| Female | 373 | 45.5 | |
| Ethnicity | Oromo | 475 | 58 |
| Amhara | 139 | 17 | |
| Kefa | 73 | 8.9 | |
| Gurage | 70 | 8.5 | |
| Dawro | 62 | 7.6 | |
| Religious | Muslim | 335 | 40.9 |
| Orthodox | 259 | 31.6 | |
| Protestant | 204 | 24.9 | |
| other | 21 | 2.6 | |
| Marital status | Single | 457 | 55.3 |
| Married | 256 | 31.8 | |
| Divorced/widowed | 106 | 12.9 | |
| Educational status | Illiterate | 64 | 7.8 |
| Primary (1-8) | 147 | 17.9 | |
| Secondary (9-12) | 447 | 54.1 | |
| Diploma & above | 165 | ||
| Occupation | Unemployed | 135 | 16.4 |
| Daily laborer | 151 | 18.4 | |
| Employed | 181 | 22.1 | |
| Farmer | 31 | 3.8 | |
| Merchant | 193 | 23.6 | |
| Student | 98 | 12 | |
| Other* | 30 | 3.7 | |
| Wealth index | poorest | 175 | 21.4 |
| Poor | 134 | 16.4 | |
| Intermediate | 182 | 22.2 | |
| Rich | 162 | 19.7 | |
| Richest | 167 | 20.4 |
Table 1: Socio-demographic characteristics of respondents (n=819) in Agaro Town, Oromia, southwest Ethiopia, 2015, *Other-House wife, house servant and driver.
Substance use history of the participants
Among the total study participants 274 (33.5%) were reported chat chewing and 96 (11.7%) smoke cigarette (Table 2).
| Variables | Category | N (%) |
|---|---|---|
| Khat Chewing | Yes | 208 (25.4) |
| No | 611 (74.6) | |
| Cigarette Smoking | Yes | 116 (14.2) |
| No | 703 (85.8) | |
| Using shisha/Cannabis | Yes | 12 (1.5) |
| No | 807 (98.5) |
Table 2: Distribution of substance use among Agaro town residents, Jimma, Southwest, Ethiopia, 2015.
Prevalence of alcohol use disorder
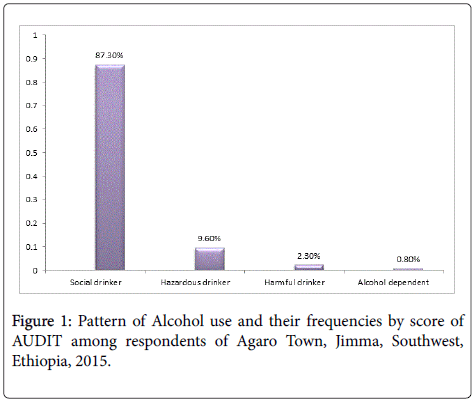
Out of the total participants, those who were drinking any of the available types of alcoholic beverage or any combination of alcohol were 355 (43.4%). The remaining 464 (56.7%) described themselves as abstainers. Among those who used alcohol, the overall prevalence of alcohol use disorder (defined as an AUDIT score ≥ 8) was 12.4% (n=45) with confidence interval (95% CI 9.3%, 15.8%).Based on AUDIT analysis Study participant were found in different pattern of drinking alcohol. Social drinkers 310 (87.3%), Hazardous drinker 34 (9.6%), Harmful drinker 8 (2.3%), Alcohol dependent 3 (0.8%) (Figure 1).
Factors associated with alcohol use disorders
Age, Sex, Marital status, Occupation, Cigarette smoking, Khat chewing, family history of alcoholism and mental distresses were significantly associated with bivarate analysis.
On multivariate analyses the association of AUDs and male sex were higher. Male had four times more likely to have AUDs as compared to females [AOR=4.0 (1.56,10.23)]. Alcohol use disorder was observed among individual who had high level mental distress symptoms as compared to who had low level mental distress symptoms [AOR=3.8 (1.35, 10.67)].
Those who reported family history of alcoholism were 3.5 times more likely to develop AUDs when compared to those did not report family history of alcoholism [AOR=3.59 (1.37, 9.39)]. Regarding to other substance, cigarette smoking are significantly associated with alcohol use disorder with [AOR=4.13 (1.35, 12.64)] when compared to non-smoker.
Environmental and psychological factors associated with initiation of alcohol use
Out of the total participants, 14.9% started drinking alcohol because of peer pressure, while 26.3% started for the sake of relieving distress and unpleasant feeling, 16.6% reported parental modelling and 17.8% for recreational value to be motive factor to keep on drinking while the remaining did not know why they started alcohol (Table 3).
| Variable | AUDs | COR(95% CI) | AOR(95% CI) | ||
|---|---|---|---|---|---|
| Yes | No | ||||
| Age | 18-24 | 12 | 64 | 1 | |
| 25-34 | 13 | 136 | 1.96 (0.84, 4.53) | ||
| 35-44 | 10 | 84 | 1.57 (0.64, 3.87) | ||
| 45-54 | 6 | 19 | 0.59 (0.19,1.790) | ||
| ≥ 55 | 3 | 8 | 0.50 (0.11, 4.63) | ||
| Sex | Male | 43 | 230 | 4.0 (1.56, 10.23) | 4.0(1.58, 10.49)* |
| Female | 1 | 81 | 1 | 1 | |
| Marital status | Married | 19 | 101 | 1 | |
| Single | 17 | 156 | 1.72 (0.85, 3.470) | ||
| Divorced | 8 | 54 | 1.27 (0.52, 3.09) | ||
| Ethnicity | Oromo | 19 | 139 | 1 | |
| Amhara | 9 | 80 | 1.21 (0.52, 2.81) | ||
| Kefa | 3 | 35 | 1.59 (0.44, 5.69) | ||
| Gurage | 4 | 30 | 1.02 (0.32, 3.23) | ||
| Dawro | 9 | 27 | 0.41 (0.16,1.00) | ||
| Occupation | Unemployed | 8 | 53 | 1 | |
| Daily labor | 10 | 82 | 1.23 (0.45, 3.33) | ||
| Employed | 9 | 71 | 1.19 (0.43, 3.29) | ||
| Farmer | 5 | 10 | 0.30 (0.08, 1.11) | ||
| Merchant | 6 | 56 | 1.40 (0.45, .4.33) | ||
| Student | 3 | 28 | 1.05 (0.29, 3.81) | ||
| Other | 2 | 11 | 0.83 (0.15, 4.45) | ||
| Wealth index | Poorest | 6 | 67 | 1.91 (0.68, 5.39) | |
| Poor | 3 | 41 | 2.34 (0.62, 8.79) | ||
| Intermediate | 15 | 73 | 0.83 (0.36, 1.90) | ||
| Rich | 8 | 60 | 1.28 (0.49, 3.35) | ||
| Richest | 12 | 70 | 1 | ||
| Smoking | Yes | 6 | 79 | 2.15 (0.81,5.29) | 4.0 (1.26, 12.03)* |
| No | 38 | 232 | 1 | 1 | |
| Chewing Khat | Yes | 6 | 104 | 3.13 (1.30, 7.76) | |
| No | 38 | 207 | 1 | ||
| Family history of alcohol use | Yes | 7 | 113 | 3.01 (1.30, 6.98) | 3.48 (1.32, 9.17)* |
| No | 37 | 198 | 1 | 1 | |
| Mental distress | Yes | 6 | 103 | 3.13 (1.28,7.65) | 3.8 (1.35, 10.67)* |
| No | 38 | 208 | 1 | 1 | |
Table 3: Bivarate and Multivariate analysis of factors associated with Alcohol use disorder among respondents living in Agaro, Jimma, Southwest, Ethiopia, 2015, *Other occupation-House wife, house servant and driver, COR: Crudes Odds Ratio; AOR: Adjusted Odds Ratio; p value ≤ 0.2 was considered as candidates for the multivariate logistic regression analysis; P value of < 0.05 on multivariate analyses was considered as statistically significant.
Discussion
The overall prevalence of alcohol use disorder was found 12.4% (males=7.6%, females 4.8%) and there was a difference in magnitude among male and female. The possible reason for the variation might be due to fact that females drink alcohol less than male because of cultural influence.
The prevalence of alcohol use disorder in the study area was higher than those studies in other part of Ethiopia, The study conducted in Addis Ababa and semi urban area of Butajira were 3.7% and 2.7% respectively [17,20]. The higher prevalence might be due to the difference between tools used and the difference in socio-cultural status of the community.
According to World Health Organization report urbanization may deleterious consequences for mental health though the influence of increase of stressors and adverse life events. This may lead to more consumption of alcohol. Also the prevalence of alcohol use disorder in this study was higher than a population based study conducted in Singapore (3.6%) [21].
However the prevalence of alcohol use disorders 12.4% found in this study was lower than cross sectional study reported from A south Africa study conducted in primary care clinic (17.6%), South wello 36.3% and Jimma University specialized Hospital 38.9%, 32.6% among HIV patient and psychiatric outpatient respectively [16,18]. The difference in prevalence could be explained by population difference and study setting. Correspondingly, the prevalence of AUDs in this study was lower than cross sectional community based study conducted in rural Tamil Nadu, India which was 29% hazardous, 33% alcohol dependent, 56% harmful effect. The smaller estimate in current study could be a reflection of the difference in culture and life style.
The estimated prevalence was similar to the results found in community based studies, Southern Brazil (3%-12%), Thailand (10.6%) and in America (15%) [15,22] respectively.
This study shows significant association of AUDs with male sex, smoking cigarettes, family history of alcoholism, and high level mental distress symptoms. Male sex had strong association with alcohol use disorder obtained in this study and the finding was in line with previous study conducted in South Africa and Ethiopia [16,17] respectively. It is plausible that societal norms restrict women from excessive use of alcohol.
Individuals who had high level of mental distress symptoms were 3.8 times more likely to have alcohol use disorders as compared to low level or no mental distress symptoms. It is possible that individuals with high level mental distress use alcohol as a self-treatment. This finding was in line with study the conducted among HIV patient in Jimma University specialized Hospital [18].
History of smoking cigarette was positively associated with alcohol use disorders. The odds of developing AUD among those who reported smoking cigarette were four times high as compared to non-smoker. This result was in line with the studies done in Brazil and Jimma University Specialized hospital respectively [15,18]. The possible explanation would be since both are habits dose-response relationship. The prevalence of AUDs was higher among those reported having history of family alcoholism.
The odds of Individuals with family history of alcoholism were 3.8 times more likely to have alcohol use disorder compared with individual who did not report. The possible explanation might be the shared genetic factor of the family.
Conclusion and Recommendation
This study had showed that prevalence of alcohol use disorder among urban resident of Agro town were significant public Health issues that require a great emphasis. This study indicates that AUDs goes along with use of other substances. Being male sex, family history of alcohol use disorder, history of smoking cigarette, had mental distress symptoms were significantly associated with alcohol use disorder.
Strengthening screening of alcohol misuse in the clinical set up and establishment of good referral linkage with mental health institutions is strongly recommended. Health professionals should be alert while giving care for those individuals having the possible higher risk for AUDs and other substance use disorder.
Limitation of the Study
Cause and effect relationship was difficult to establish by cross sectional studies. Social desirability bias could be an important limitation because persons who use alcohol and other substances tend to under-report or deny their use.
Acknowledgment
First, we would like to thank Amanuel Mental Specialized Hospital and University of Gondar, College of Medicine and Health Sciences for their technical support for overall accomplishment of research. Second, we want to thank the study participants for devoting their time voluntarily. Also we are grateful for data collectors for their cooperation during the data collection time.
Competing Interest
The authors declare no competing interest.
Funding
No Funding was received for this research work.
Authors’ Contributions
AB and MG participated in the conception, design of the study, reviewing proposal and data analysis. NY, MG and AB participated in reviewing proposal and writing the research report. AB prepared the manuscript for publication. All authors read and approved the final manuscript.
References
- Donaldson GK, Eliot AC, Flint D, Maggio-Hall LA, Nagarajan V (2014) Fermentive production of four carbon alcohols: Google Patents.
- Steinkraus KH (1986) Fermented foods, feeds and beverages. Biotechnol Adv 4: 219-243.
- Gunzerath L, Faden V, Zakhari S, Warren K (2004) National institute on alcohol abuse and alcoholism report on moderate drinking. Alcohol Clin Exp Res 28: 829-847.
- Gordis E (1988) National Institute on alcohol abuse and alcoholism. Br J Addict 83: 483-493.
- Tarter RE, Vanyukov M (1994) Alcoholism: A developmental disorder. J Consult Clin Psychol 62.
- Van Ommeren M, Saxena S, Saraceno B (2009) Mental and social health during and after acute emergencies: Emerging consensus? Bull World Health Organ 83: 71-75.
- Rehm J, Mathers C, Popova S, Thavorncharoensap M, Teerawattananon Y, et al. (2009) Global burden of disease and injury and economic cost attributable to alcohol use and alcohol-use disorders. Lancet 373: 2223-2233.
- Saxena S, Sharan P, Garrido M, Saraceno B (2006) World Health Organization's mental health atlas 2005: Implications for policy development. World Psychiatry 5.
- Browne FA, Wechsberg WM (2010) The intersecting risks of substance use and HIV risk among substance-using South African males and females. Curr Opin Psychiatry 23: 205-209.
- Goetzel RZ, Hawkins K, Ozminkowski RJ, Wang S (2003) The health and productivity cost burden of the “Top 10 physical and mental health conditions affecting six large US employers in 1999. J Occup Environ Med 45: 5-14.
- Goetzel RZ, Anderson DR, Whitmer RW, Ozminkowski RJ, Dunn RL, et al. (1998) The relationship between modifiable health risks and health care expenditures: An analysis of the multi-employer HERO health risk and cost database. J Occup Environ Med 40: 843-854.
- Harwood HJ, Fountain D, Livermore G (1998) The economic costs of alcohol and drug abuse in the United States, 1992. US Department of Health and Human Services, National Institutes of Health, National Institute on Drug Abuse, Office of Science Policy and Communications.
- Windle M (2003) Alcohol use among adolescents and young adults. Population 45: 19-15.
- Barros MBA, Botega NJ, Dalgalarrondo P, MarÃn-León L, Oliveira HB (2007) Prevalence of alcohol abuse and associated factors in a population-based study. Rev Saude Publica 41: 502-509.
- Peltzer K, Davids A, Njuho P (2011) Alcohol use and problem drinking in South Africa: Findings from a national population-based survey. Afr J Psychiatr 14: 30-37.
- Kebede D, Alem A (1999) The epidemiology of alcohol dependence and problem drinking in Addis Ababa, Ethiopia. Acta Psychiatr Scand Suppl 100: 30-34.
- Soboka M, Tesfaye M, Feyissa GT, Hanlon C (2014) Alcohol use disorders and associated factors among people living with HIV who are attending services in South West Ethiopia. BMC Res Notes 7.
- World Health Organization (1994) A user’s guide to the self-reporting questionnaire (SRQ). WHO Geneva 5: 655.
- Alem A, Kebede D, Kullgren G (1999) The epidemiology of problem drinking in Butajira, Ethiopia. Acta Psychiatr Scand Suppl 100: 77-83.
- Subramaniam M, Abdin E, Vaingankar J, Phua AMY, Tee J, et al. (2012) Prevalence and correlates of alcohol use disorders in the Singapore mental health survey. Addiction 107: 1443-1452.
- Junsirimongkol B, Kittirattanapaiboon P, Khamwongpin M, Chutha W, Kongsuk T, et al. (2011) The prevalence and psychiatric co-morbidity of alcohol use disorders in Thailand: National Epidemiological Survey 2008. J Ment Health Thailand 19: 88-102.
Citation: Bedaso A, Gobena M, Yigzaw N, Getachew M (2019) Determinants of Alcohol Use Disorder among Residents of Agaro Town, Jimma, Southwest, Ethiopia: A Cross-sectional Study. J Addict Res Ther 10:377. DOI: 10.4172/2155-6105.1000377
Copyright: © 2019 Bedaso A, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.
Select your language of interest to view the total content in your interested language
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 4487
- [From(publication date): 0-2019 - Dec 06, 2025]
- Breakdown by view type
- HTML page views: 3545
- PDF downloads: 942