Research Article Open Access
Designing, Implementing and Assessing a Novel Text-Messaging Intervention for an Adolescent Mobile Health Clinic: A Collaborative Approach
Seth D Ammerman* and Chris Weiss
Department of Pediatrics, Division of Adolescent Medicine, Lucile Packard Children’s Hospital, Stanford University, Stanford, CA, USA
- *Corresponding Author:
- Seth D Ammerman
Department of Pediatrics
Division of Adolescent Medicine
Lucile Packard Children’s Hospital
Stanford University, Stanford, CA, USA
Tel: 415-407-7047
E-mail: seth.ammerman@stanford.edu
Received date: June 09, 2016; Accepted date: June 20, 2016; Published date: June 24, 2016
Citation: Ammerman SD, Weiss C (2016) Designing, Implementing and Assessing a Novel Text-Messaging Intervention for an Adolescent Mobile Health Clinic: A Collaborative Approach. J Child Adolesc Behav 4:299. doi:10.4172/2375-4494.1000299
Copyright: © 2016 Ammerman SD, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Child and Adolescent Behavior
Abstract
Purpose: To determine if a text messaging intervention (TMI) delivering adolescent-relevant health information is feasible and effective at engaging underserved adolescents in a mobile health clinic setting. Methods: Mobile clinic adolescent patients, along with clinic staff, helped develop the text messaging content and format. Patients subsequently received text messages presenting health information in a question-and-answer format for 14 weeks. Participants could reply to receive messages with correct answers and further information. Focus groups and interviews were conducted post-intervention to evaluate messaging functionality and participant engagement. Results: All participants received and replied to texts for the duration of the study, and they reported high levels of engagement with the program. Participant input was instrumental in developing the structure and content of the text messages. Conclusions: TMIs that deliver health-related information are feasible in the mobile health care setting with high levels of engagement by underserved adolescents. Implications and contribution: Underserved adolescents will actively engage in TMI-based interventions aimed at disseminating health-related information, and these interventions have significant potential to increase knowledge and promote health-related behavior change. Moreover, adolescents can (and should) play an integral role in the development of these interventions.
Keywords
Adolescents; Medically uninsured; Underserved; Mobile health clinic; Short messaging service; Text messaging intervention; Health-related behaviors; Collaboration
Introduction
Encouraging and supporting patients efforts towards making positive changes in health-related behaviors is crucial to improving their health outcomes. There are many barriers to providing this support to patients; this is especially so when working with adolescents, where limited contact time with providers, incongruent communication styles, and lack of patient engagement can undermine clinical influence [1,2]. Providers of adolescent health care must develop interventions that address these barriers and actively engage patients in the treatment process.
Our work with adolescents is through the Teen Health Van, a mobile medical clinic which makes regularly scheduled visits to multiple sites from San Francisco to San Jose, CA. The Teen Health Van provides comprehensive primary health care services to uninsured adolescents. While ethnically diverse, members of our patient population typically share multiple biopsychosocial stressors: substance use/abuse and lack of family/economic support are common, and approximately 40% have been homeless at some point in the prior year. The Teen Health Van serves as a mobile medical home for this diverse group of adolescents; a place where they can receive treatment for illness, but also where they can gain knowledge and direction to aid them in optimizing wellness. To provide education and support to a large (700+) patient population in a way that encourages significant participant engagement, it is essential to utilize an effective medium to send messages that patients are willing and able to receive.
The medium
Short message service (SMS, or text messaging) is a communication medium widely accessible to and very popular with adolescents across a wide demographic spectrum, Most studies have found that 95-99% of adolescents have access to a texingt-enabled device [3-5]. Likewise, many adolescents report text messaging as their preferred mode of communication, even when other modes are freely available [3-6].
The message
Text-messaging interventions (TMI) have been shown to be beneficial and cost-effective as an adjunct to standard medical treatments with adolescents [3-10]. The majority of TMIs to date have utilized reminder messages (e.g., supporting medication adherence or regular blood glucose testing) or motivational messages to encourage adherence to a previously-defined treatment regimen. Notably fewer have attempted to deliver novel health information to promote healthrelated behavior change [3-5]. Fewer still have been aimed at the adolescent population, and then only in limited clinical settings [3-6]. Given its broad availability, the flexibility and adaptability of its platform and its popularity with adolescents, text messaging would seem to have great potential as a means of providing relevant health care education to adolescents.
We collaborated with the adolescent patients of our mobile health clinic to develop a TMI to disseminate health information relevant to adolescents to support change in health-related behaviors. A pilot study of the program was undertaken to test our hypotheses that: 1) TMI are feasible with an underserved adolescent population, and 2) health information disseminated in an SMS format could be engaging for adolescent patients. Additionally, we expected to find evidence that involving adolescents in the program development process would result in a more engaging intervention.
Methods
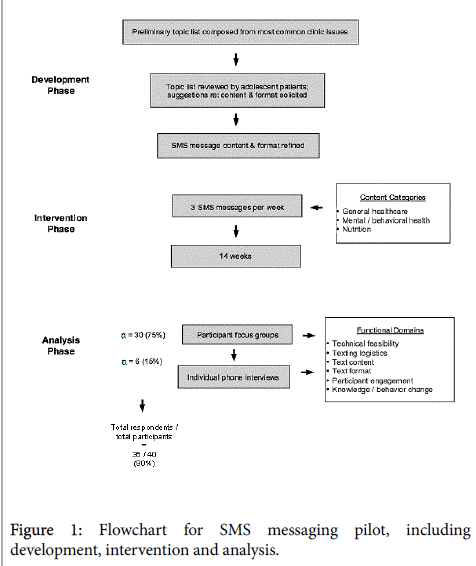
An overview of our study is shown in Figure 1. A multidisciplinary team of mobile health clinic providers (including a physician, anurse practitioner, alicensed clinical social worker, and a registered dietician) compiled a list of adolescent-relevant health topics based upon a review of visit diagnoses most frequently encountered in our clinic.
Topics were divided into three categories: General Healthcare, Mental/Behavioral Health, and Nutrition/Fitness. Prior to the intervention, informational messages were initially developed by the Teen Health Van staff noted above and then reviewed by 12 adolescent patients from several mobile health clinic sites, to provide feedback on content, clarity, format, length and timing of message delivery.
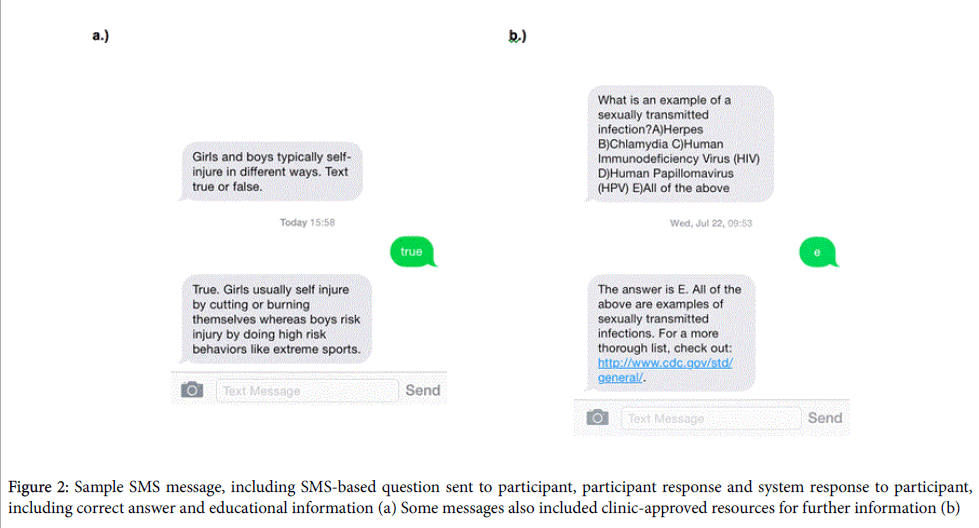
Topics favored by adolescent reviewers were chosen for inclusion in the study, and suggestions for message length and frequency were adopted. Notably, several adolescent reviewers suggested that changing the TMI structure to an interactive quiz format would be more engaging than sending TMI content as simple informative statements. In response to this, clinic staff restructured the SMS messages into a question-and-answer format (Figure 2a and 2b). Other suggestions for optimizing engagement which were integrated into the TMI included limiting the number of text messages to a total of 3 messages per week and sending text messages in the late afternoon (5 pm).
For the intervention phase, adolescents were recruited from all of our mobile health clinic sites. Participants elected to use their own SMS-enabled device or one provided to them at no cost, and all were given unlimited text messaging credit for the duration of the study. Participants were given the choice of receiving messages in English or Spanish. We contracted with a health communications developer (CareMessage) to develop a HIPAA- and PHI-compliant SMS platform to deliver message content.
All participants received three text messages per week (one from each content category) for 14 weeks in total. Thequestions(true/false and multiple-choice) invited participants to text a reply with a selected answer choice (Figure 2). Every reply received a response message with the correct answer, an explanation, and follow-up information. Using the SMS software platform, we collected data on individual and group response rates. All participants that completed the TMI and replied to 50% or more messages was given a small incentive (participant’s choice of either two free movie tickets or a gift card to a department store.)
In the post-intervention phase, participants were interviewed in focus groups or individually by phone. Focus groups consisted of 4-10 participants and were moderated by two Teen Health Van staff. A standardized script was used to solicit feedback regarding six functional domains: Feasibility, Logistics, Content, Format, Engagement and Knowledge/Behavior Change. For each domain participants were asked 1-2 closed-end quantitative and several open-ended questions. were conducted in person or by telephone using a similar script. All groups and individual interviews were recorded (with participant approval) and later transcribed to verify analyses. Quantitative data were tabulated for the group as a whole, and thematic analysis was utilized to assess qualitative responses.
This project was approved by the Stanford University Institutional Review Board.
Results
40 adolescents were recruited for the pilot intervention. Gender of participants was reported as female for 32 (80%) and male for 8 (20%). Ethnicity of participants was reported as Hispanic for 32 (80%), White/ Non-Hispanic for 4 (10%), African-American for 3 (7.5%) and Asian for 1 (2.5%). The participants ranged in age from 14 to 25 years of age, with a mean of 15.7 years. 34 (85%) of 40 participants completed the 14-week TMI, and 36 (90%) gave feedback in focus groups or individual interviews.The results for each functional domain are as follows:
Technical feasibility: 100% of participants received text messages as scheduled. 33 participants (91%) reported no technical difficulties with replying to texts. There were no significant technical issues experienced by MHC staff.
Texting logistics : 34 participants (94%) felt that the three texts per week was acceptable to ideal. They broadly agreed that message length was sufficient to impart useful information but easily manageable. Participants also liked the ability afforded by the text format to respond immediately or at another more convenient time.
Text content: 100% of participants reported interest in one or more content areas addressed in texts. All topics were considered generally relevant by a majority of participants, and all participants were able to mention several topics of significant personal interest. The most popular topics were emotional health (including stress, depression and anger management), substance abuse, social stress/peer pressure, relationships, sexually transmitted infections, and nutrition.
Text format: 100% of participants felt that the question-and-answer format was acceptable to ideal. Participants found that the ability to reply to messages and receive correct answers with further information increased motivation to engage with the intervention. When participants chose the incorrect answer, they reported increased interest in obtaining further information about a given topic.
Participant engagement: There is no universally accepted definition of engagement in the discussion of TMIs. For the purposes of our pilot intervention, we define “engagement” generally as interest in/acceptance of our intervention, and more quantitatively as responding to text messages and remaining enrolled in the intervention until it was completed. 96% of participants responded to at least 1 message over the course of the intervention. 34 participants (85%) remained enrolled in the intervention until it was completed. 100% of participants agreed that the text message format was acceptable or ideal for communicating health information. All participants that gave feedback stated they were willing to sign up for follow-up text messaging programs.
Knowledge/Behavior change: While we did not formally assess for increase in knowledge or behavior change in this pilot study, multiple participants reported that texts provided information and encouragement that helped them make more positive health behavior choices. Several participants also reported using the texts as a starting point for conversations with family and friends regarding relevant health-related issues. Participants also reported that their involvement in the program helped them feel more aware of and connected to the Teen Health Van program.
Discussion
Text messaging has become a favored method of communication for adolescents from a wide range of ethnic and socioeconomic backgrounds, and virtually all adolescents possess text messaging-enabled devices and texting data plans. Given this, text messaging would seem to be a logical choice for connecting with and providing interventions for adolescents. Our pilot program demonstrated that TMI are feasible in the mobile health care setting. Furthermore, our teens universally found the text messaging modality appealing, and the majority of participants remained enrolled in the intervention for the entire length of the pilot program. Participants also reported significant interest in the information regarding various adolescent health issues as delivered by text message. Altogether, these findings support the utility of TMIs for disseminating health-related information, with the goal of supporting improved wellness. Furthermore, the inclusion of participant critique and feedback in the pilot process resulted in specific changes to the logistics, content and format of texts. These changes were well received by participants and contributed to increased engagement.
It is notable that the positive feedback was broadly consistent across the spans of age, gender and ethnicity seen in our participant population. While this underscores the commonalities of certain health issues between adolescent subpopulations, it more importantly demonstrates the almost universal uptake of text messaging as a primary or even preferred mode of communication and information transfer among adolescents as a whole.
To generate the most effective educational messages for adolescents, it is essential to involve the adolescents themselves in the development of their interventions. Previous work has demonstrated that acknowledging adolescents as experts on their issues and enlisting them in active evaluation and development of clinical programs results in more relevant content and optimized delivery [11]. Furthermore, interventions that have been refined based on feedback from adolescents have improved patient engagement [11-13]. We involved adolescents in each step of the pilot intervention development process. We did not set up a process for comparing participant engagement with intervention material developed with and without adolescent help, , but we did note that adolescents commented very positively on aspects of the intervention suggested by their peers (e.g., the question-and- answer format, the text message length, etc.), and this suggests that adolescents should play a prominent role in the development of future projects.
While our results are encouraging, certain aspects of our study limit our ability to generalize our findings. The size and structure of a pilot study limits our ability to extrapolate our results to larger populations. Study participation was voluntary, and thus our participants may have been more receptive to TMI than the general adolescent population. Our clinic population is uninsured and primarily Latino, and our participant group was predominantly female. Given this demographic makeup, our results may be less applicable to other populations of adolescents. Additionally, though the format of our focus groups allowed us to gain valuable insight into participant's views of the texting pilot, it also places participants in the social spotlight when answering questions, which may prompt a participant to answer in a way that more closely aligns with the overall group outlook.
The most important next steps in TMI development are, broadly: 1) to refine the structure and delivery of TMI, and 2) to further assess their utility as interventions to promote behavior change. We have expanded our pilot TMI program into an ongoing intervention available to all patients of the Teen Health Van. Our goals for our current study will be to assess engagement in a more quantitative fashion and to attempt to capture and quantify both knowledge gain and behavior change. In future interventions, it would be optimal to expand TMIs to utilize two-way communication between patients and health providers, with individual questions serving as springboards to prompt participants to reach out to clinic medical staff with any personal questions or concerns.
TMI allow health care providers to connect to teen patients on a more regular and less formal basis via a broadly accessible medium with which teens are generally very comfortable and often more easily engaged. As a result, they show great promise as a means of increasing dissemination of health-related information to adolescents (and by extension, supporting them in making more positive health behavior choices) while simultaneously increasing their engagement with healthcare interventions and their medical home. Furthermore, they are an ideal venue for building a more collaborative (and thus more effective) relationship between patients and their medical home.
Acknowledgements
We would like to thank the Lucile Packard Foundation for Children’s Health and the Children’s Health Fund, who are the primary funders of the LPCH Teen Health Van. A grant from the Verizon Foundation provided support for the pilot text-messaging intervention. Care Message provided the PHI- and HIPAA-compliant texting platform.The Lucile Packard Children’s Hospital at Stanford provided a community investment grant for this project.
References
- Murphy DC, Klinghoffer I, Fernandez-Wilson JB, Rosenberg L (2000) Mobile health units. Design and implementation considerations. AAOHN J 48: 526-532.
- Redlener I, Redlener KB (1994) System-based mobile primary pediatric care for homeless children: the anatomy of a working program. Bull N Y Acad Med 71: 49-57.
- Cole-Lewis H, Kershaw T (2010) Text messaging as a tool for behavior change in disease prevention and management. Epidemiol Rev 32: 56-69.
- Hall AK, Cole-Lewis H, Bernhardt JM (2015) Mobile text messaging for health: a systematic review of reviews. Annu Rev Public Health 36: 393-415.
- Militello LK, Kelly SA, Melnyk BM (2012) Systematic review of text-messaging interventions to promote healthy behaviors in pediatric and adolescent populations: implications for clinical practice and research. Worldviews Evid Based Nurs 9: 66-77.
- Lau PW, Lau EY, Wong DP, Ransdell L (2011) A systematic review of information and communication technology-based interventions for promoting physical activity behavior change in children and adolescents. J Med Internet Res 13: e48.
- Haug S, Schaub MP, Venzin V (2013) A pre-post study on the appropriateness and effectiveness of a Web- and text messaging-based intervention to reduce problem drinking in emerging adults. J Med Internet Res 15: e196.
- Suffoletto B, Callaway CW, Kristan J (2013) Mobile phone text message intervention to reduce binge drinking among young adults: study protocol for a randomized controlled trial. Trials 14: 93.
- Haug S, Meyer C, Dymalski A, Lippke S, John U (2012) Efficacy of a text messaging (SMS) based smoking cessation intervention for adolescents and young adults: study protocol of a cluster randomised controlled trial. BMC Public Health 12: 51.
- Britto MT, Munafo JK, Schoettker PJ, Vockell AL, Wimberg JA, et al. (2012) Pilot and feasibility test of adolescent-controlled text messaging reminders. Clin Pediatr (Phila) 51: 114-121.
- Stewart TC, Harrington J, Batey B, Merritt NH, Parry NG (2015) From focus groups to production of a distracted driving video: Using teen input to drive injury prevention programming. J Trauma Acute Care Surg 79: S42-47.
- Heary CM, Hennessy E (2002) The use of focus group interviews in pediatric health care research. J Pediatr Psychol 27: 47-57.
- Crowley R, Wolfe I, Lock K, McKee M (2011) Improving the transition between paediatric and adult healthcare: a systematic review. Arch Dis Child 96: 548-553.
Relevant Topics
- Adolescent Anxiety
- Adult Psychology
- Adult Sexual Behavior
- Anger Management
- Autism
- Behaviour
- Child Anxiety
- Child Health
- Child Mental Health
- Child Psychology
- Children Behavior
- Children Development
- Counselling
- Depression Disorders
- Digital Media Impact
- Eating disorder
- Mental Health Interventions
- Neuroscience
- Obeys Children
- Parental Care
- Risky Behavior
- Social-Emotional Learning (SEL)
- Societal Influence
- Trauma-Informed Care
Recommended Journals
Article Tools
Article Usage
- Total views: 13474
- [From(publication date):
June-2016 - Apr 02, 2025] - Breakdown by view type
- HTML page views : 12528
- PDF downloads : 946