Research Article Open Access
Designing and Testing the Feasibility of a Multi-level Intervention to Treat Adolescent Obesity in the Pediatric Primary Care Setting
Lori Pbert1*, Monica L Wang2, Susan Druker3, Elizabeth A Jackson4 and Milagros C Rosal51Division of Preventive and Behavioral Medicine, University of Massachusetts Medical School,55 Lake Avenue North, Worcester, MA 01655, USA
2Department of Community Health Sciences, Boston University School of Public Health 801 Massachusetts Avenue, Boston, MA 02115, USA
3Division of Preventive and Behavioral Medicine, University of Massachusetts Medical School, 55 Lake Avenue North, Worcester, MA 01655, USA
4Department of Internal Medicine, University of Michigan Health System
1500 E. Medical Center Drive, Ann Arbor, 48109, USA
5Division of Preventive and Behavioral Medicine, University of Massachusetts Medical School, 55 Lake Avenue North, Worcester, MA 01655, USA
- *Corresponding Author:
- Lori Pbert
Division of Preventive and Behavioral Medicine
University of Massachusetts Medical School
55 Lake Avenue North, Worcester, MA 01655, USA
Tel: 508-856-3515
Fax: 508-856-3840
E-mail: Lori.Pbert@umassmed.edu
Received Date: February 14, 2014; Accepted Date: March 18, 2015; Published Date: March 23, 2015
Citation: Pbert L, Wang ML, Druker S, Jackson EA, Rosal MC (2015) Designing and Testing the Feasibility of a Multi-level Intervention to Treat Adolescent Obesity in the Pediatric Primary Care Setting. J Child Adolesc Behav 3:196. doi:10.4172/2375-4494.1000196
Copyright: © 2015 Pbert L, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Child and Adolescent Behavior
Abstract
Objective: To describe the development steps and feasibility test of a multi-level adolescent obesity intervention for delivery in pediatric primary care settings. Method: To understand the target setting and population (i.e., perceptions of and receptivity to various intervention components), focus groups were conducted with clinicians, adolescents, and parents (N=58). Findings informed the development of a multi-level intervention (i.e., office support systems, brief clinician-delivered counseling, and nutritionist-led adolescent group sessions) targeting overweight and obese adolescents (N=22). The intervention was pilot-tested for feasibility using a single group pre- and post-test comparison. Results: Families and clinicians agreed on the importance of developing approaches to address adolescent obesity in the pediatric primary care setting, and favored family involvement. The pilot-study showed that it was feasible to implement office system changes to support obesity treatment. All but one component of the cliniciandelivered counseling algorithm were feasible. Adolescents participating in the intervention reported dietary improvements and movement toward the action stage for decreasing sedentary behavior. Conclusion: Multi-level interventions for adolescent obesity in the pediatric primary care setting are feasible. Research to test the effectiveness of such interventions is warranted.
Keywords
Adolescents; Obesity; Pediatric primary care; Treatment; Clinician counseling; Diet; Physical activity
Introduction
The prevalence of obesity among adolescents has tripled over the past three decades, and currently one third of adolescents (33.6%) are either overweight or obese [1]. Excess weight is associated with adverse physiological and psychological problems in adolescence and adult life [2-4] and with increased health care costs [5]. Identification and treatment of obesity during childhood and adolescence is critical to reduce associated risks during adulthood.
Despite a plethora of research on childhood and adolescent obesity, few effective behavioral interventions for overweight and obese adolescents exist, [6] and all have limited applicability to pediatric practice settings [7]. In 2009, the majority (69.0-71.6%) of 10-17 year old children were seen by their pediatrician through wellchild visits in the past year [8]. Pediatricians have resources to provide counseling on weight loss behaviors [9] and can make referrals for more intensive weight loss support for adolescents when needed. Thus, pediatric primary care settings represent a tremendous opportunity to intervene in obesity treatment in a large segment of the adolescent population. Furthermore, adolescent obesity interventions that can be easily disseminated to pediatric primary care settings leverage existing resources and have the potential to address obesity on a larger scale.
Clinical practice guidelines for obesity treatment in pediatric primary care settings have been in existence over the past decade, [10,11] yet the majority of pediatric providers (77%) report frustration and barriers to treatment, [12] including lack of patient motivation, poor parental involvement, limited clinician time, and lack of support services. Additionally, there is a paucity of research on how best to implement guidelines in pediatric primary care practice [13].
Lessons learned from efforts to intervene for diet and physical activity behaviors and weight change in adult primary care settings [14-17] have potential to inform the treatment of adolescent obesity. Multi-level approaches that are systems-based and include physiciandelivered patient-centered counseling have shown to effectively promote change in diet, cardiovascular disease risk factors and weight loss among adults, with the systems component of the interventions enhancing clinician adherence to clinical practice guidelines and behavioral counseling [18,19]. Additional system linkages to ancillary staff (i.e., dietitian) at the patient level further support patient health behavior change and weight loss [14,15,20].
Relatively little has been researched about how to best adapt evidence-based interventions to new settings and populations, and how to do so in a manner that maximizes the potential for their dissemination in real world settings. The intervention translation model proposes that the process of adapting evidence-based interventions requires understanding of the new target setting and the target population, tailoring of the evidence-based protocols to the new setting and population, pilot-testing the feasibility of the adapted intervention, and evaluating its effectiveness [21]. The purpose of this study is to describe the initial steps of this process for adapting a multilevel intervention to treat adolescent obesity in the pediatric primary care setting: intervention adaptation and pilot testing of feasibility.
Methods
Consistent with the intervention translation framework [21], the study involved several phases and a mixed methods approach. The intervention development (formative) phase used qualitative methods, and the feasibility-testing phase used a quantitative methods. Informed by Social Cognitive Theory [22,23] and the Social Ecological framework, [24,25] the intervention translation framework emphasizes the understanding of factors and challenges specific to real world settings and populations, and the adaptation of evidence-based interventions to their characteristics. For example, examining population characteristics such as weight-related knowledge, attitudes, and behaviors can inform the tone, content, and format of interventions. Understanding of setting characteristics, such as organizational structure, capacity, and resources, can help leverage available resources and facilitate integration of the intervention, maximizing feasibility of implementation [21]. We also drew from the Trans theoretical Model [26] which proposes that health behavior change is a process involving progress through a series of stages of change from pre-contemplation (not intending to take action) through contemplation (intending to change in the next 6 months), preparation (have a plan of action and intending to take action in the immediate future), action (have made specific overt modifications in their lifestyle), and maintenance (working to prevent relapse and continue the behavior change). All study procedures received approval from the University of Massachusetts Medical School Institutional Review Board.
Intervention adaptation (formative) phase
Qualitative input. The study site was a pediatric practice serving a multi-ethnic population in central Massachusetts. In accordance with the intervention translation model, we made efforts to gain insights on the target setting by conducting focus groups with pediatric providers and office staff (n=13). Similarly, to gain insights on adolescents that the intervention would target, we conducted focus groups with adolescents (n=29) age 10-17 years and body mass index (BMI) at or above the 85th percentile who were seeking care at the study site, and separate focus groups with their parents (n=14).
Focus group discussions consisted of semi-structured, open-ended questions designed to collect data from staff, adolescents, and parents on: (1) receptivity to addressing obesity within the pediatric primary care setting; (2) perceptions of current office systems for screening for obesity and risks factors; (3) knowledge of and reactions to current obesity interventions being delivered in the pediatric practice; (4) recommendations for implementing American Academy of Pediatrics (AAP) guidelines for preventing and treating obesity in the pediatric practice; and (5) recommendations for additional resources. Focus groups were moderated by an experienced focus group facilitator, audio-taped and transcribed. Informed consent was obtained from participants prior to focus group participation, and cash incentives ranging from $25-50 were provided upon completion. Participant responses were coded and categorized (e.g., by question, theme, subtheme) in accordance with standard qualitative methods [27,28]. Theme and sub-theme instances that occurred across members within focus groups and across focus groups we considered significant findings.
Using qualitative input to adapt the evidence-based intervention. The adaptation of an evidence-based multi-level intervention [14,19] to target adolescent overweight and obesity was informed by focus group findings and a review of the cognitive behavioral obesity intervention literature [15,29]. Main intervention components included: (1) office systems devoted to obesity intervention; (2) a clinician-delivered intervention algorithm to guide obesity counseling during clinical visits with overweight or obese adolescent patients; and (3) a group-based three-session program targeting diet, physical activity, and sedentary behaviors for overweight or obese adolescents. A description of each intervention component is presented below. Based on feedback from focus group participants, the program was entitled Healthy Living.
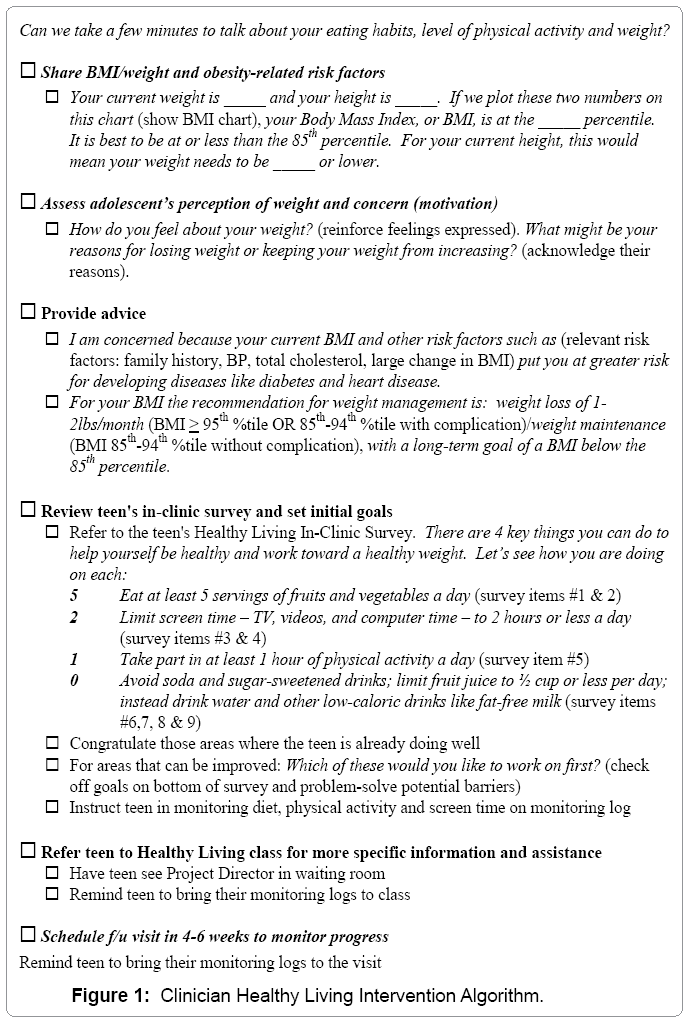
Office systems: Consistent with providers’ recommendations in focus groups, an office system was designed to identify and document adolescents’ BMI, collect written assessments of adolescents’ diet, physical activity and sedentary behavior, and support intervention delivery. Activities conducted by nursing staff included providing each overweight or obese adolescent with the survey assessment to complete and placing the Healthy Living Clinician Intervention algorithm (Figure 1) on the adolescent’s medical chart.
Clinician intervention: To address adolescents’ and parents’ stated need for concrete recommendations on achieving a healthy weight, the intervention messages were adapted from two existing childhood obesity campaigns: Blue Cross Blue Shield of Massachusetts’ “Jump Up and Go!” 5-2-1 program [30] and the Anthem Blue Cross and Blue Shield “Keep ME Healthy 5-2-1-0 Power Up” in Maine [31]. The intervention included the following recommendations around daily behaviors: consumption of 5 servings of fruits and vegetables; limiting screen time to 2 hours or less; engaging in at least 1 hour of physical activity; limiting or drinking 0 sugar-sweetened beverages.
Building from the focus group findings and the 5-2-1-0 framework, the clinician intervention included: a brief behavioral survey adolescents completed while waiting to see their clinician; an intervention algorithm to guide the clinician in discussing BMI and obesity-related risk factors, assessing adolescents’ concerns, delivering advice, reviewing the adolescent’s survey, and setting goals (Figure 1); a diet and physical activity monitoring log; and a follow-up intervention algorithm to review adolescents’ BMI and goals related to BMI, establish new goals, and schedule follow-up visits to monitor progress (Figure 2). Pediatric clinicians received a one-hour training session delivered by research staff during a lunch break.
Group sessions: Three one-hour group sessions with adolescents (gender-stratified) were designed and delivered by a pediatric nutritionist. 5-2-1-0 messages were integrated throughout all sessions. Each session included a review of prior goals set and self-monitoring logs; problem solving regarding unmet goals; presentation of the session topic; preparation and consumption of a healthy snack; and setting of new goals. A two-hour parent group session offered by the pediatric nutritionist on two Saturdays provided parents with a summary of topics and skills covered in the adolescent group sessions and included additional topics such as meal planning, food shopping and budgeting, healthy recipes, parental modeling, limit-setting, and challenges with readiness to change.
Pilot testing phase
The multi-level intervention was pilot tested in the same pediatric practice that participated in the formative research phase using a single group pre- and post-test design with assessments conducted at baseline and follow-up (1 month for adolescent measures and 3 months for clinician measures). Participant eligibility criteria included: ages 13- 17 years; BMI at or above the 85th percentile; current patients at the pediatric clinic; English-speaking; and parental consent to participate. Adolescents who participated in the formative focus groups were excluded. Nursing staff provided information about the study to all eligible adolescent patients at the time of their appointment. Interested adolescents were provided additional study information by research staff. Parental written consent and child written assent were obtained from interested individuals. All pediatric clinicians were eligible to participate.
Measures
Feasibility of intervention implementation and fidelity to intervention protocols were assessed through validated Patient Exit Interview (PEI) [32] surveys completed by the adolescent immediately following their visit with the pediatric clinician at baseline and at 1-month follow-up. These surveys assessed the degree to which clinicians delivered each of the intervention steps in the algorithm. Responses were summarized in a PEI index score. Clinicians completed a survey pre- and 3 months post-training assessing their attitudes, selfefficacy, and practices in intervening among adolescents across a range of weight statuses.
Adolescents completed a self-administered survey assessing the following: stage of change for diet, physical activity behaviors, and sedentary behaviors, [33] diet, physical activity and sedentary behaviors [34] and perceived support from the clinician, assessed via self-administered, self-report survey. A healthy diet score[33] was computed to summarize self-report regarding fruit and vegetable consumption, French fries or chips, soda and other sugar-sweetened drinks, and the number of times adolescents ate at a fast food restaurant per week, with lower scores indicating a better quality diet.
Statistical analysis
Comparisons of means at baseline, follow-up, and difference of means between times were conducted using t-tests. Differences in categorical variables were conducted using Fisher’s exact tests, and paired dichotomous outcomes were compared using McNemar’s test. Analyses were carried out using Stata 9.2.
Results
Participant characteristics
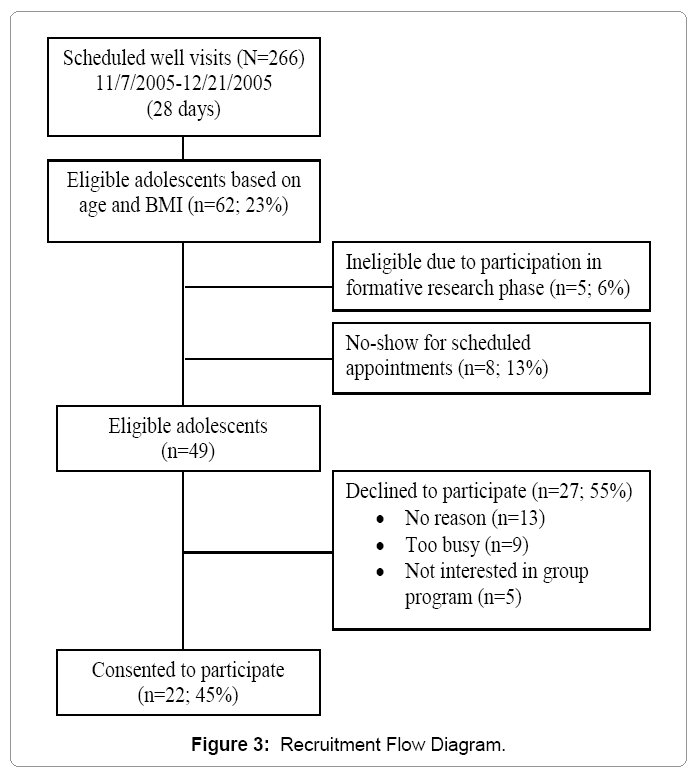
The pilot test sample consisted of 22 adolescents (Figure 3 for recruitment flow diagram). Clinicians consisted of 7 physicians and 3 nurse practitioners (70% female; mean age of 38 years (SD = 6.3)).
Intervention fidelity and feasibility
The nurse placed the intervention algorithm on 100% of the adolescent participants’ medical charts. Adolescents received the Healthy Living In-Clinic Survey with 100% completion. The completed In-Clinic Survey was placed in the patient medical record by the clinician 65% of the time. One hundred percent of adolescent baseline and follow-up surveys, post visit PEIs, and baseline and 3-month follow-up clinician surveys were completed.
PEIs indicated that clinicians completed on average 9 out of the 14 recommended intervention steps (57%) at the initial visit and 7 out of the 10 recommended steps (70%) at the follow-up visit (Table 1). Clinicians and adolescents reported similar average amount of time to go through the initial visit intervention (8.57 vs. 8.42 minutes, respectively). At least 60% of adolescents reported that the following intervention steps were delivered by their clinicians at the initial visit: discussed weight or BMI (91%); asked how the adolescent feels about his/her weight (60%); advised on the 5-2-1-0 goals (63%-86% depending on the goal); referred adolescent to the Healthy Living Classes (91%); and scheduled a follow-up appointment to assess weight and weight-related changes (91%). Intervention steps delivered less frequently included: provided recommended BMI (41%); stated concern regarding their weight (41%); congratulated adolescent on positive healthy behaviors (59%); set goals (50%); and provided monitoring log (27%). Similar patterns in intervention steps delivered were found at the follow-up visit (Table 1 for further details).
| Intervention Steps and Duration | Initial Visit | Follow-up Visit |
|---|---|---|
| Number of steps completed (Mean (SD))/total Summary Score; percent of total | 8.6 (3.6)/14; 57% | 7.3 (1.9)/10; 70% |
| Time (minutes) spent on intervention: Mean (SD) | 8.4 (5.98) | 5.2 (3.76) |
| Completion of Individual PEI Steps* | ||
| 1. Discussed weight/BMI | 91% | 76% |
| 2. Provided recommended BMI | 41% | 76% |
| 3. Asked how teen felt about weight | 60% | N/A |
| 4. Stated they were concerned about the teen’s weight | 41% | N/A |
| 5. Discussed eating at least 5 servings of fruits and vegetables | 73% | N/A |
| 6. Discussed limiting screen time to 2 hours a day | 73% | N/A |
| 7. Discussed taking part in 1 hour of physical activity a day | 86% | N/A |
| 8. Discussed avoiding soda and sugar-sweetened drinks | 63% | N/A |
| 9. Congratulated teen on positive healthy behaviors | 59% | 94% |
| 10. Set goals | 50% | 58% |
| 11. Provided monitoring log | 27% | 35% |
| 12. Told teen to schedule follow-up appointment | 91% | 71% |
| 13. Told teen about Healthy Living Classes | 91% | N/A |
| 14. Asked what changes in diet, physical activity and sedentary behavior were made | N/A | 88% |
| 15. Reviewed prior goals | N/A | 82% |
| 16. Asked what were barriers to making changes | N/A | 82% |
*N/A denotes that the step was only relevant for either the initial or follow-up visit.
Table 1: Dose of Clinician-Delivered Counseling Intervention Received Based on Adolescent Patient Exit Interview (PEI) Surveys.
Table 2 presents significant changes in frequency of intervention steps implemented by clinicians from baseline (prior to intervention training) to follow-up, stratified by adolescent weight status (nonsignificant changes not shown). Frequency was noted on a scale of 1 to 4, the latter indicating the highest frequency. Among obese adolescents, significant increases in the frequency of the following clinician intervention steps were observed from baseline to follow-up: sharing BMI information with the adolescent (3.1 to 3.7); discussing recommended BMI (2.2 to 2.9); scheduling a follow-up visit (2.4 to 3.0); and referring the adolescent to additional resources for weight-related behavior change (2.3 to 2.7) (p-values ≤ 0.05). Among overweight adolescents, the only observed difference was increase in frequency of clinician discussion of healthy diet and physical activity levels (3.4 to 4.0, p = 0.03). Over half (62%) of clinicians perceived the intervention algorithm to be moderately helpful, and half perceived adolescents to be moderately receptive to the intervention.
| Baseline | Follow-up | Difference | |||
|---|---|---|---|---|---|
| Frequency** of Intervention Steps Taken | Mean (SD) | Mean (SD) | Mean (SD) | 95% Conf. (Interval) | p-value† |
| With Obese Adolescent Patients | |||||
| Shared BMI with adolescent | 3.1 (0.93) | 3.7 (0.50) | 0.6 (0.73) | 1.11 (0.00) | 0.05 |
| Explained recommended BMI | 2.2 (1.14) | 2.9 (1.10) | 0.7 (0.95) | 1.38 (0.02) | 0.04 |
| Scheduled a follow-up visit | 2.4 (0.70) | 3.0 (1.05) | 0.6 (0.84) | 1.20 (0.00) | 0.05 |
| Referred adolescent to other resources | 2.3 (0.67) | 2.7 (0.82) | 0.4 (0.52) | 0.77 (0.03) | 0.04 |
| With Overweight Adolescent Patients | |||||
| Discussed healthy diet and physical activity | 3.4 (0.52) | 4.0 (0.00) | 0.6 (0.52) | 0.97 (0.23) | 0.01 |
*Only significant changes shown. **Scale of 1 (lowest) to 4 (highest) frequency. †Mean comparisons conducted using paired t-tests. P-values ≤ 0.05 were considered to be statistically significant.
*Only significant changes shown.
**Scale of 1 (lowest) to 4 (highest) frequency.
†Mean comparisons conducted using paired t-tests. P-values ≤ 0.05 were considered to be statistically significant.
Table 2: Change* in Counseling Intervention Steps Completed from Baseline to 3-Month Follow-up among Clinicians (N=10) Stratified by Patient Weight Status.
Over half (55%) of adolescents attended all three group-based sessions; five (23%) attended no sessions. Sessions were favorably received by the teens who attended, with the majority (88%) reporting being comfortable with discussing their weight, diet and level of physical activity with the pediatric nutritionist running the sessions. Girls reported higher level of engagement in intervention sessions than boys (4.7 vs. 3.8 out of 5, respectively; p = 0.03). No other gender differences were observed. Only two parents attended one of the two optional group classes offered for parents (a resource strongly recommended by parent participants during focus group discussions).
Clinician outcomes
No significant changes in clinicians’ perceptions of the following were observed from baseline to follow-up: extent of their role to help adolescents reduce their BMI; effectiveness of weight counseling (moderate at both time points); confidence in their counseling skills (moderate at both time points); perceived commitment of other physicians to address adolescent overweight; stage of change in addressing weight with adolescent patients; and barriers to pediatric obesity intervention. Main barriers cited included: patients having other acute medical problems, perceived lack of adolescent motivation to make changes, parents being overweight, perceived lack of effectiveness of counseling, and time-consuming nature of counseling.
Adolescent outcomes
Table 3 presents adolescents’ diet, physical activity, and sedentary behaviors at baseline and 1-month follow-up. Adolescents had improvements in healthy diet scores over time, whereas change in physical activity and sedentary behaviors were not significant. The percentage of adolescents who reported being in the action stage of change for reducing their sedentary behavior (i.e., screen time) more than doubled from baseline (33%) to 1-month follow-up (72%; p = 0.04) (results not shown). Similar trends were noted with increases in percentage of adolescents in the action stage for improving their diet (44% to 67%) and level of physical activity (44% to 72%), though these improvements were not statistically significant. The majority of adolescents (81% or higher) reported being comfortable in discussing their weight, diet, physical activity, and sedentary behavior with their clinician, and 90% felt the clinician understood how they felt about their weight and about changing these behaviors. A slightly higher percentage of adolescents reported feeling more committed to making behavior changes to reduce weight at follow-up compared to baseline (90% vs. 82%).
| Baseline | Follow-up | Difference | ||
|---|---|---|---|---|
| Variable | Mean (SD) | Mean (SD) | Mean (SD) | p-value* |
| Healthy diet score** | 0.77 (0.29) | 0.51 (0.28) | -0.25 (0.22) | 0.0001 |
| Physical activity | 3.34 (2.04) | 4.03 (1.98) | 0.69 (2.04) | 0.17 |
| Sedentary behavior (TV) | 2.20 (1.01) | 1.92 (1.10) | -0.28 (0.83) | 0.17 |
| Sedentary behavior (computer) | 1.39 (1.86) | 1.11 (1.52) | -0.19 (1.20) | 0.50 |
* Comparisons of means between baseline and follow-up were made using paired t-tests
** Lower scores indicate a healthier diet
* Comparisons of means between baseline and follow-up were made using paired
t-tests
** Lower scores indicate a healthier diet
Table 3: Dietary, Physical Activity, and Sedentary Behaviors among Adolescents (N=22) from Baseline to 1-Month Follow-up.
Discussion
Pilot study results demonstrated feasibility in recruiting overweight and obese adolescents from a large pediatric practice, with nearly half of eligible participants enrolled and high adherence to data collection procedures. However, recruitment required intensive on-site research staff resources and cooperation from clinic staff. Frequent prompting by research staff was required to ensure routine implementation of office systems to support intervention delivery. Systems barriers have been found to be related to a decreased sense of competence by clinicians in treating obesity [12]. This finding indicates the need to understand methods to maximize intervention implementation as part of routine clinical practice, consistent with research showing that systems-based interventions improve adherence to clinical practice guidelines for other behavioral interventions in primary care settings [18,19,35]. Integration into existing systems that do not require several new actions on the part of staff, including the use of electronic medical records with prompts built in may facilitate this process, as well as consideration of appropriate staff incentives and process for accountability.
Despite a clear message from adolescents and parents during focus groups that they desired group sessions to learn specifics on how to improve their diet and level of physical activity, attendance to groups by adolescents was variable and parental engagement was minimal. This is consistent with the high rate of attrition found in weight management clinics and programs [36-39]. However, girls were more likely to attend the classes than boys, suggesting that the group format may have potential for girls but needs to be revisited for assisting boys.
Discrepant views between clinicians and adolescents were observed, with adolescents reporting being very comfortable and receptive to the clinician-delivered intervention and even perceiving the intervention as part of the clinician’s job. Other research has similarly shown that adolescents perceive pediatric providers to have the credibility and the knowledge necessary to provide counseling [40] and most commonly identifying their physician or nurse practitioner as the most knowledgeable about behaviors such as how to eat a healthy diet [41]. In contrast, clinicians reported the intervention algorithm was only moderately helpful in their discussions re: weight and weight-related behaviors with adolescent patients, and perceived only moderate patient receptivity to the intervention. Although the intervention algorithm was developed based on input from clinicians, and clinicians were engaged in the process of refining and finalizing it, additional refinement through beta testing and iterative modifications may be needed to ensure the algorithm is maximally helpful to clinicians. Also, greater understanding of barriers to clinicians utilizing the intervention algorithm and strategies to overcome such barriers would be valuable.
Fidelity data from PEIs indicated that less than half of the clinicians delivered key intervention steps, such as instructing the adolescent on monitoring their diet and level of physical activity. As lack of time was cited as a major barrier for completing counseling steps, one recommendation is to incorporate established referral sources, such as nutritionists or group programs, within the clinician protocol. Previous programs, such as Maine’s Let’s Go 5-2-1-0 program, [42] have integrated a referral approach to address childhood obesity. However, the efficacy of these programs has not yet been rigorously evaluated.
Adolescents reported higher healthy diet scores at follow-up after completing the group program with the nutritionist. This may be partially mediated by adolescents’ report of being more comfortable talking with the nutritionist running the groups and feeling that the nutritionist understood how they felt about their weight to a greater extent than the clinician. As adolescents reported positive interactions with the nutritionist and increases in healthy eating, referrals to nutritionists may be routinely incorporated into pediatric obesity interventions. Further exploration is needed on how best to connect clinicians with adjunct treatment staff to facilitate referral and continuity of communication about the adolescent’s progress.
The significant increase in the percentage of adolescents reporting moving to the action stage for decreasing sedentary behavior from baseline to follow-up suggests that sedentary behavior may be perceived as the easiest weight-related behavior for adolescents to tackle first over a short period of time. However, no decreases in self-reported sedentary behaviors were observed. One possible explanation for this finding is that the intervention was primarily designed for individuals who are ready to make a change (action stage). Less than half of the adolescents at baseline reported being in the action stage of change for improving their diet and physical activity, and only a third reported being in the action stage for reducing their sedentary behavior. This may partially attribute to the lack of improvements observed for sedentary behaviors and physical activity. Another possible explanation is that the Trans theoretical Model, originally developed to decrease smoking among adults, may not be the most appropriate theoretical framework for addressing adolescent overweight and weight-related behavior change through the primary care setting.
One implication of these findings regarding stages of change is that tailoring the intervention to each adolescent’s stage of change for specific behaviors may enhance clinicians’ perceptions regarding adolescent receptivity and maximize intervention effect on stage change, behavior change, and ultimately reducing BMI among overweight and obese adolescents. For example, adolescents who report readiness to make changes in physical activity but not diet or sedentary behaviors may signal to clinicians their receptivity to physical activity as the main focus of counseling, rather than allocating an equal amount of time or emphasis on discussing change for several behaviors.
Study strengths include the systematic use of a framework for adapting and pilot-testing the multi-level intervention, the high participant retention rate, and the promising intervention acceptability as perceived by adolescents. Findings should be considered in light of a number of study limitations. Due to the short amount of time in the clinic, adolescent baseline surveys were completed immediately after the initial clinician appointment. This could constitute a potential bias and may explain why additional changes between pre- and post- attitudes were not observed. Diet, physical activity, and sedentary behaviors were self-reported using the previous week as the time framework for responses, however responses to self-reports are subject to recall and social desirability biases. As with many pilot studies, the current study’s sample size was small and collected from only one pediatric practice, thus limiting generalizability of study findings. Additionally, the singlegroup pre- and post-test study design with a short follow-up period also limits the establishment of causality. Despite these limitations, pilot study results indicate that this intervention approach is overall feasible for pediatric primary care providers and warrants further exploration.
Conclusion
Pediatric primary care settings hold strong potential for obesity intervention among adolescents. Office systems can support systematic screening for overweight and obesity of adolescents and support clinicians in delivering clinical practice guidelines, with a strong referral component to provide ongoing assistance to adolescents and their families. Further research is needed on how to effectively integrate obesity screening and treatment efforts and provide adjuncts to support adolescent in making and sustaining obesity-related behavior changes.
Acknowledgements
We would like to thank the pediatric practice and their staff who graciously took part in this study. To the adolescents and their families who agreed to participate, we extend our deepest appreciation. This study was supported by the Boston Nutrition Obesity Research Center (Lori Pbert, PhD, Principal Investigator).
References
- Ogden CL, Carroll MD, Kit BK, Flegal KM (2012) Prevalence of obesity and trends in body mass index among US children and adolescents, 1999-2010.JAMA 307: 483-490.
- Cook S, Weitzman M, Auinger P, Nguyen M, Dietz WH (2003) Prevalence of a metabolic syndrome phenotype in adolescents: findings from the third National Health and Nutrition Examination Survey, 1988-1994.Arch PediatrAdolesc Med 157: 821-827.
- Eisenberg ME, Neumark-Sztainer D, Story M (2003) Associations of weight-based teasing and emotional well-being among adolescents.ArchPediatrAdolesc Med 157: 733-738.
- Wyatt SB, Winters KP, Dubbert PM (2006) Overweight and obesity: prevalence, consequences, and causes of a growing public health problem.Am J Med Sci 331: 166-174.
- Finkelstein EA, Trogdon JG, Cohen JW, Dietz W (2009) Annual medical spending attributable to obesity: payer-and service-specific estimates.HealthAff (Millwood) 28: w822-831.
- Doyle AC, Goldschmidt A, Huang C, Winzelberg AJ, Taylor CB, et al. (2008) Reduction of overweight and eating disorder symptoms via the Internet in adolescents: a randomized controlled trial.JAdolesc Health 43: 172-179.
- Warschburger P, Fromme C, Petermann F, Wojtalla N, Oepen J (2001) Conceptualisation and evaluation of a cognitive-behavioural training programme for children and adolescents with obesity.Int J ObesRelatMetabDisord 25 Suppl 1: S93-95.
- Health Services Financing and Utilization (2011). Children Health USA 2009.
- Koplan JP, Liverman CT, Kraak VA (2004) Preventing childhood obesity: Health in the balance, in Institute of Medicine Committee on Prevention of Obesity in Children and Youth. The National Academies Press.
- Barlow SE (2007) Expert committee recommendations regarding the prevention, assessment, and treatment of child and adolescent overweight and obesity: summary report. Pediatrics. 120 Suppl 4:S164-192.
- Krebs NF, Jacobson MS; American Academy of Pediatrics Committee on Nutrition (2003) Prevention of pediatric overweight and obesity.Pediatrics 112: 424-430.
- Jelalian E, Boergers J, Alday CS, Frank R (2003) Survey of physician attitudes and practices related to pediatricobesity.ClinPediatr (Phila) 42: 235-245.
- Saelens BE, Liu L (2007) Clinician's comment on treatment of childhood overweight meta-analysis.HealthPsychol 26: 533-536.
- Hebert JR, Ebbeling CB, Ockene IS May Y, Riger L, Merriam PA, et al. (1999) A dietitian-delivered group nutrition program leads to reductions in dietary fat, serum cholesterol, and body weight: the Worcester Area Trial for Counseling in Hyperlipidemia (WATCH). J Am Diet Assoc 99:544-552.
- Carvajal R, Wadden TA, Tsai AG, Peck K, Moran CH (2013) Managing obesity in primary care practice: a narrative review.Ann N Y AcadSci 1281: 191-206.
- Wadden TA, Butryn ML, Hong PS, Tsai AG (2014) Behavioral treatment of obesity in patients encountered in primary care settings: a systematic review.JAMA 312: 1779-1791.
- Booth HP, Prevost TA, Wright AJ, Gulliford MC (2014) Effectiveness of behavioural weight loss interventions delivered in a primary care setting: a systematic review and meta-analysis.FamPract 31: 643-653.
- Ockene IS, Ockene JK (1996) Barriers to lifestyle change, and the need to develop an integrated approach to prevention.CardiolClin 14: 159-169.
- Ockene IS, Hebert JR, Ockene JK, Saperia GM, Stanek K, et al. (1999) Effect of physician-delivered nutrition counseling training and an office-support program on saturated fat intake, weight, and serum lipid measurements in a hyperlipidemic population: Worcester Area Trial for Counseling in Hyperlipidemia (WATCH). Arch Intern Med 159:725-731.
- Tol J, Swinkels IC, de Bakker DH, Seidell J, Veenhof C (2014) Dietetic treatment lowers body mass index in overweight patients: an observational study in primary health care.J Hum Nutr Diet 27: 426-433.
- Rosal MC, Lemon SC, Nguyen OH, Driscoll NE, Ditaranto L (2011) Translation of the diabetes prevention program lifestyle intervention for promoting postpartum weight loss among low-income women. TranslBehav Med 4:530-538.
- Nouwen A, Urquhart Law G, Hussain S, McGovern S, Napier H (2009) Comparison of the role of self-efficacy and illness representations in relation to dietary self-care and diabetes distress in adolescents with type 1 diabetes.Psychol Health 24: 1071-1084.
- Bandura A (1989) Human agency in social cognitive theory.AmPsychol 44: 1175-1184.
- Stokols D (1996) Translating social ecological theory into guidelines for community health promotion.Am J Health Promot 10: 282-298.
- Stokols D, Allen J, Bellingham RL (1996) The social ecology of health promotion: implications for research and practice.Am J Health Promot 10: 247-251.
- Prochaska JO, Velicer WF (1997) Thetranstheoretical model of health behaviorchange.Am J Health Promot 12: 38-48.
- Patton MQ (2002) Qualitative Research and Evaluation Methods. (3rdEdn), Sage Publications Thousand Oaks, CA.
- LaPelle NL (2004) Simplifying Qualitative Data Analysis Using General Purpose Software. Fields Methods. Sage Publications Thousand Oaks, CA.
- Rogers VW1, Hart PH, Motyka E, Rines EN, Vine J, et al. (2013) Impact of Let's Go! 5-2-1-0: a community-based, multisetting childhood obesity prevention program.JPediatrPsychol 38: 1010-1020.
- Massachusetts. Jump Up & Go! http://www.bluecrossma.com/blue-iq/health-and-wellness/popup/jump-up-and-go.html.
- Keep ME Healthy: 5-2-1-0 Power Up (2014) Childhood Obesity Prevention.
- Pbert L, Adams A, Quirk M, Hebert JR, Ockene JK, et al. (1999) The patient exit interview as an assessment of physician-delivered smoking intervention: a validation study.HealthPsychol 18: 183-188.
- Neumark-Sztainer D, Story M, Hannan PJ, Rex J (2003) New Moves: a school-based obesity prevention program for adolescent girls.Prev Med 37: 41-51.
- Glasgow RE, Ory MG, Klesges LM, Cifuentes M, Fernald DH, et al. (2005) Practical and relevant self-report measures of patient health behaviors for primary care research.AnnFam Med 3: 73-81.
- Fiore MC, Jaen CR, Baker TB, Bailey WC, Benowitz, NL, et al. (2008) Treating Tobacco Use and Dependence: 2008 Update. Clinical Practice Guideline. Department of Health and Human Services. Public Health Service. Rockville, MD: U.S.
- Cote MP, Byczkowski T, Kotagal U, Kirk S, Zeller M, et al. (2004) Service quality and attrition: an examination of a pediatric obesity program.Int J Qual Health Care 16: 165-173.
- Hampl S, Paves H, Laubscher K, Eneli I (2011) Patient engagement and attrition in pediatric obesity clinics and programs: results and recommendations.Pediatrics 128 Suppl 2: S59-64.
- Jelalian E, Hart CN, Mehlenbeck RS, Lloyd-Richardson EE, Kaplan JD, et al. (2008) Predictors of attrition and weight loss in an adolescent weight control program.Obesity (Silver Spring) 16: 1318-1323.
- Zeller M, Kirk S, Claytor R, Khoury P, Grieme J, et al. (2004) Predictors of attrition from a pediatric weight management program.JPediatr 144: 466-470.
- Klein JD, Allan MJ, Elster AB, Stevens D, Cox C, et al. (2001) Improving adolescent preventive care in community health centers.Pediatrics 107: 318-327.
- Cohen ML, Tanofsky-Kraff M, Young-Hyman D, Yanovski JA (2005) Weight and its relationship to adolescent perceptions of their providers (WRAP): a qualitative and quantitative assessment of teen weight-related preferences and concerns.JAdolesc Health 37: 163.
- (2013) Let's Go! Annual Report.
Relevant Topics
- Adolescent Anxiety
- Adult Psychology
- Adult Sexual Behavior
- Anger Management
- Autism
- Behaviour
- Child Anxiety
- Child Health
- Child Mental Health
- Child Psychology
- Children Behavior
- Children Development
- Counselling
- Depression Disorders
- Digital Media Impact
- Eating disorder
- Mental Health Interventions
- Neuroscience
- Obeys Children
- Parental Care
- Risky Behavior
- Social-Emotional Learning (SEL)
- Societal Influence
- Trauma-Informed Care
Recommended Journals
Article Tools
Article Usage
- Total views: 14707
- [From(publication date):
April-2015 - Dec 19, 2024] - Breakdown by view type
- HTML page views : 10230
- PDF downloads : 4477