Design and Development of a Pupilometer for the Automatic Detection of Relative Afferent Pupillary Defect
Received: 10-Jan-2023 / Manuscript No. omoa-23- 86203 / Editor assigned: 12-Jan-2023 / PreQC No. omoa-23- 86203 / Reviewed: 24-Jan-2023 / QC No. omoa-23- 86203 / Revised: 27-Jan-2023 / Manuscript No. omoa-23- 86203 / Published Date: 31-Jan-2023 DOI: 10.4172/2476-2075.1000187
Abstract
The presence of Relative Afferent Pupillary Defect (RAPD) indicates serious ocular disease, if untreated may lead to loss of vision. Swinging Flash Test (SFT) has been a traditional way of testing for RAPD since decades, quantification of RAPD, its reliability and accuracy are still not a reality. In this study a novel Pupilometer device is proposed which uses custom built hardware and software to perform the test with an objective of determining the RAPD at an early stage. The hardware of the device consists of components to produce a light stimulus into each eye and record the response of the pupils to the stimulus with a high-resolution camera. A Graphical User Interface (GUI) developed is responsible for the timing of the stimulus, processing the recorded response of the pupil in calculating the area of pupil through image segmentation and analysis. RAPD test was conducted on 30 patients who are diagnosed with RAPD by using the pupilometer designed. The Pupil area of 30 RAPD patients has shown to be significant with p<0.001 in the diagnosis of RAPD.
Keywords
RAPD; SFT; Constriction and dilation; Light stimulus; Pupil identification and tracking; Pupillary light reflex
Introduction
The eye is a complex, important and special sense organ of the five sense organs of human body. It helps us in viewing the world and plays a vital role in our day to day lives. Vision is a complex phenomenon of perceiving the information about the environment in the form of reflection of light from the objects falls on the eye. The human visual system comprises of various complex structures each one performs a specific task, and they are interconnected to each other [1, 2]. Retina is the main functional unit of eye causes transformation of light energy into action potentials and generates a neural signal, which is further transferred to brain through the optic nerve. The optic nerve fibers are responsible for one of the important neurological reflexes called the light reflex, which refers to constriction of both pupils when light is flashed into either eye, through afferent fibers called pupillary fibers, via afferent nerve pathway. In a nervous system, the afferent pathway indicates the signal transmission from sensory organ to brain (from eye to midbrain). When the normal afferent pathway of pupil is disturbed by any Ocular disorders the pupillary light reflex is affected leading to Relative Afferent Pupillary Defect (RAPD). The pupils respond briskly on stimulation of good eye and weakly on stimulation of diseased eye [3-7].
Normal pupils when light is projected into one eye, pupils of both eyes constrict equally and then relax a little. They dilate again when the light is removed. When the light is swung rapidly between both the pupils (within the mean time pupillary constriction), they maintain their state of constriction. If the time that the light present in front of each eye exceeds the mean pupillary constriction time of those pupils, they relax a little, equally when light is swung to both eyes. The characteristics within both eyes should be same in as a response to stimulus [8].
The paradoxical dilation of both pupils when light is shone in front of diseased eye is called RAPD. Since RAPD can be observed in anterior optic tract lesions, it provides a clue that how much afferent input must differ between the eyes to produce a clinically visible RAPD. The grading of RAPD is a useful indicator of the degree of damage that occurred in a diseased Optic Nerve [9-14]. RAPD has a major role in determining the ocular health status.
Pupil Evaluation involves examination of size of the pupil, pupillary response, shape of the pupil and pupillary reflexes. Swinging Flashlight Test (SFT) is performed for Pupil Evaluation, where a flashlight is swung alternatively between both eyes and the pupillary responses are observed relative to each other [15,16]. The difference between the pupillary reactions of the two eyes in RAPD patients is highlighted by the Swinging Flashlight Test. We will miss a RAPD if we do not perform SFT, as it is only by comparing the relative strengths of the signals reaching the brain that it is detected [17].
Though the test is standardized along all these years, it is a subjective test, and the findings vary between observers. It requires a lot of learning, skills, and experience to perform SFT correctly and to interpret the results properly. All the characteristics of SFT should be met by every single practitioner to get correct and comparable results from everyone. Due to these limitations, utility of the device for detecting RAPD must be tested on patients with known grades of RAPD and Normal subjects and comparing the results obtained between both the groups [18-21].
Radzius, Aleksandras, et al. worked on Infrared pupilometer that measures the pupil diameter and the change in pupil diameter after its response to a light stimulus and the values obtained were comparable to a photographic measurement [21-24].
Lada Kalaboukhova, Vanja Fridhammar, and Bertil Lindblom studied on patients with Optic Atrophy due to Unilateral Open-angle glaucoma with an aim to develop a new technique to analyze RAPD and to find the optimum stimulus parameters for RAPD detection in those patients [25]. They used custom built pupillometer and different sets of stimulus-pause combinations were studied (1s-0.5s, 0.5s-1s, 1s-1s, 1s-1.5s, and 1.5s-1.5s) and their study results showed that the combination of a stimulus duration of 0.5 s and a pause duration of 1 s at a light intensity of 1000 cd/m2 was best suited for the detection of glaucoma.
The relative afferent pupillary defect was shown quantitatively in an eye contralateral to dense unilateral cataract, recorded using a binocular infrared video Pupillography. The difference between contraction amplitudes (which was defined as the difference between maximal and minimal diameters of the pupil of an eye) was larger when compared between right eye stimulation and left eye stimulation before the surgery with constrictions being higher when the cataractous eye was stimulated [26, 27]. This difference in contraction amplitude disappeared after surgery in the cataractous eye.
Pupillary responses were examined quantitatively in three patients with unilateral extensive myelinated nerve fibers and amblyopia using binocular infrared video pupillographic device (Vision module; Newopto, Kawasaki, Japan) in a darkened room by presenting stimuli with white light-emitting diodes to the right and left eyes alternatively [28]. They noticed that there was percent reduction in pupil contraction amplitude (the sum of both pupils) during the stimulation of the affected eye. The average of constriction amplitudes (constriction amplitude for each light reflex was defined as the difference between maximum and minimum diameters) for the four right eye stimulations was then compared with the average of the four left eye stimulations [29].
Cohen, Liza M., et al., worked on a Novel and Computerized pupillometer. The pupil responses obtained in RAPD patient are correlated with the RAPD’s stimulated by presenting different illumination intensity (LUX) to both eyes and clinician determined RAPD was correlated with the device calculated RAPD. They found a significant correlation in both cases [30]. They determined the eye with RAPD, and the degree of it is calculated with the ratio of percentage change in the constriction amplitude to the right eye and left eye under stimulation. Based on study results they concluded that the device had high sensitivity and specificity. As per literature, this is the only available device which can detect the eye with RAPD and the degree of RAPD.
Volpe, Nicholas J., et al., say that the pupillometer device distinguishes between healthy volunteers and patients with RAPD greater than 0.9 log units of neutral density filter reducing its sensitivity. In this study, there is the significant statistical difference between normal and RAPD patients and significant correlation between patients with true APD’s and subjects with stimulated RAPD’s using neutral density filters.
Cox, Terry A worked with a binocular television pupillometer and recorded the pupillary responses of normal subjects after stimulating RAPD using neutral density filters to dim the light in front of one eye while performing the swinging flashlight test [31]. They aimed to determine the best indicator of RAPD by comparing contraction amplitude, minimum size, final size, and redilatation amplitude. Their study concluded that the contraction amplitude as best indicator.
Volpe, Nicholas J et al., again worked on a computerized pupillometer device. They compared the Neutral Density Filter (NDF) strength required to neutralize the RAPD of the patient for whom the device also calculates the absolute inter-eye difference, and they found a significant correlation between both findings. But there is also an intereye difference found by the device in normal subjects, which questions the device capability in distinguishing normal from abnormal.
A study carried using pupillometer to determine whether there is any difference in constriction amplitude between both the eyes in 10 patients with various degrees of amblyopia showed that only small proportion of amblyopes shows difference in constriction amplitude [32]. Dara Lankaranian compared the sensitivity and specificity of detecting RAPD using routine Swinging flashlight test method and Pupillography method on patients having glaucoma and concluded that the Pupillography with a magnified view of pupils helps in better detection of RAPD.
A study, done by Benson, M. T., et al. showed a positive scope for the further development of the device using which the mean difference of pupillary responses between right and left eye were calculated. They found a significant difference between the mean differences of normal subjects and patients with RAPD [33]. The mean difference between right and left eyes was 8.84 ms for normals and 78.6 for patients with RAPD.
Shwe-Tin calibrated pupillometer output with the neutral density filters of attenuation: 0.0, 0.3, 0.6, and 0.9 log units and tested it on healthy volunteers by stimulating RAPD with NDF’s of the same attenuation [34]. The sensitivity and specificity of the device detecting stimulated RAPD with NDF was high. Thus, they gave future directions for using this device to detect RAPD in actual patients.
Although there have been multiple studies describing many pupilometers and their use in detecting RAPD throughout many decades, till date there is no pupillometer that got incorporated into clinical practice and achieved widespread use.
This could be because of the lack of availability of an established pupillometer that is accepted and believed by clinicians which can replace a traditional swinging light test performed by a well- experienced doctor in detecting the RAPD. RAPDx designed by Konan Medical a US based company, is the only pupillomotor device which determines the pupil function and gives quantitative score of RAPD [35].
Therefore, we are proposing a Novel device to standardize this test using a custom designed hardware and a software routine. Initial prototype of the device was designed and used on the RAPD patients as an alternative method for SFT.
Methodology
The main objective of the project is to design and develop a Pupilometer for the detection of RAPD from the pupillary response obtained under external visual stimulus. The response of the pupils recorded by a high-resolution camera, and the video file is processed by using an image processing algorithm. Hardware Components and Software tools used in developing custom designed hardware and software for the device are given in different sections. Pupilometer can be used on children above 6 years of age to adults who need an examination of the pupil in the fields of Ophthalmology, Critical Care, Neurology and General Medicine. The idea behind the design is to keep the design robust, simple, safe, portable, tamper proof, minimal fixtures or fastening, light weight and cost-efficient. The design avoids problem of light escaping to other eye when stimulus is in front of other eye and illuminates one eye at a time correctly [36].
For better detection of RAPD the intensity of light stimulus is maintained constant (Right eye – 1330 LUX and Left eye – 1140 LUX) throughout all the 5 pairs of stimuli to each person. Light stimulus is ON for 3 seconds in front of each eye. Gap between each stimulus in the same pair and in between different pairs is 0.5s.
Hardware Assembly
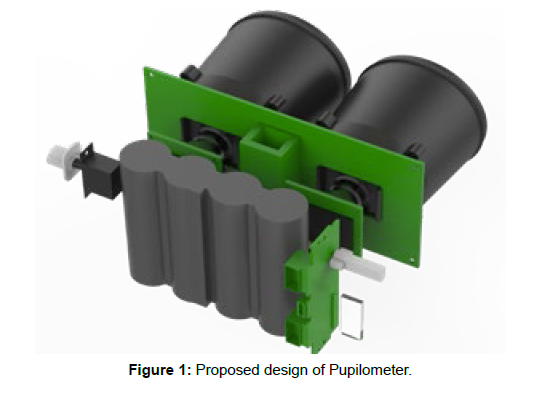
The proposed design of the pupilometer is shown in (Figure 1). The components of the proposed Novel Pupilometer device are as mentioned below
• Eight White LED’s
• Four IR LED’s
• Camera’s
• Arduino Nano
• PCB
• Ambrane P-1000 Star Power Bank 10400 mA The device comprises of eight visible LED’s four in front of each eye. They emit monochromatic light occurring at a single wavelength. Four Infrared light emitting diodes (IR LED) are positioned two in front of each eye helps in viewing the pupil under darkness. The device comprises two cameras ELP series USB webcams, one in front of each eye records the pupil reactions to light stimulus. The main assembly of the proposed novel Pupilometer is centered on the PCB mount. The PCB, apart from holding the Arduino Nano board and acting as a mount for the Cameras, helps connecting all the LED’s [37]. Arduino is programmed to provide visual stimulus through LED’s and pupillary response is recorded by the high-resolution cameras. A binocular eye piece surrounds the webcams so that field of view of camera and the line of sight of eye are along a straight line.
Specifications of the Hardware
Consistency of stimulus: The stimulus is constant throughout all the pairs of Stimulus
Intensity of stimulus: Right eye – 1330 LUX and Left eye – 1140 LUX
Number of Stimulus pairs – Five pairs of stimuli for each person
ON time and OFF time - ON time is 3 seconds in front of each eye and the gap between each stimulus in the same pair and in between different pairs is 0.5s.
Number of access ports: Ease of accessing the device - 2 ports connecting device and Laptop/Computer
Neglected Components
Distant target: To check if the distant target is mandatory for the detection of RAPD, patients with known grades RAPD were tested by giving a near stimulus and allowing them to accommodate and then checked RAPD. The patients not only showed RAPD but also the grading was same when they were given distant and near target. So, we neglected the distant target compulsion to check RAPD [38].
Scotoma free stimulus: The reason for using scotoma free collimated stimulus source is to illuminate one eye at a time and avoid illuminating another eye, the scotoma free collimated light source is also neglected in the device.
Data Collection
This study is conducted in collaboration with the Neuro Ophthalmology department at L V Prasad Eye Institute (LVPEI). The outpatient department in LVPEI has been screened for RAPD patients on day-to-day basis. The Electronic Medical Record system at LVPEI facilitated the easy screening of patients for RAPD. Information Posters were used to get patients, to keep Optometrists and Ophthalmologists informed about the need of RAPD patients for the study.
In LVPEI, patients are initially seen and worked up by the Optometrists. As part of routine work up, Pupil examination by Swinging Flashlight test is also performed by the Optometrists. Any abnormality present in the pupils is noted down [39]. All the patients are seen by the doctors before dilating them. If RAPD is present, the Senior Ophthalmologist tests and confirm the presence and grade of RAPD by doing Swinging Flashlight test before dilating them for further examination.
Data Collection Protocol:
Study Design: Experimental Case Control Study Study Site: L V Prasad Eye Institute, Hyderabad Sample Size: 60 participants Study group: 30 patients with RAPD Control group: 30 Normal volunteers
Inclusion Criteria
Study group:
• All grades of RAPD
• No efferent pupillary defects
• No other pupil disorders (Anisocoria, Irregular pupil, displaced pupils)
Control group:
• No ocular or systemic disorders
• No h/o any ocular or systemic medication that alters pupil size
• No RAPD
Exclusion Criteria
Subjects Who Are Not Falling Under the Inclusion Criteria: Patients confirmed with RAPD and falling under the inclusion criteria were considered and explained briefly about the study before dilating them. If the patient agrees to take part in the study the patient along with their attendant were taken to the clinical setting room with the experimental set up is shown in (Figure 2). The consent form is given, and patient and the attendant were explained about the study in detail. They are allowed to read the consent and signature is taken from the patient and the attended signature as witness. If the patients are not attended by anyone the signature of one of the team members is taken as witness [40].
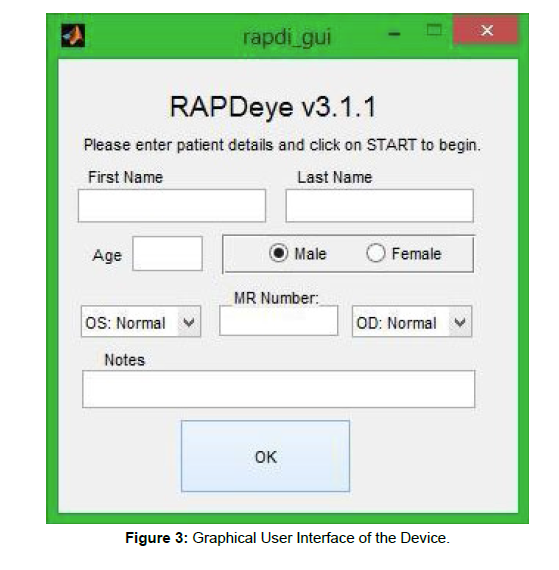
The patient details are entered into the RAPD eye Graphic User Interface shown in (Figure 3). The GUI has a provision of creating the database consists of personal information and patient history. Patients are asked to view from the window, and the device is adjusted so that pupils of both eyes are visible correctly in the preview pane. The test starts by pressing the start button, stimulus alternates between both eyes by lasting in front of each eye for three seconds and a rapid alternation with a gap of 0.5 seconds between each stimulus pair. The cameras present inside the device records a live video of pupil of each eye separately when they are reacting to light stimulus. Once the five stimulus pairs are completed the test will be stopped automatically. The video will get saved with patients’ MR Num. The total time taken for stimulus is 34.5 seconds and the whole procedure of explanation and taking signature on the consent took less than 10minutes.
The testing procedure is same for the control group also except the inclusion criteria which varied between them.
Open CV, a computer vision and machine learning software library, is used to program the cameras to detect and track the pupil through from the images of the recording. Both Arduino IDE and OpenCV have MATLAB interfaces. MATLAB code returns a video file saved with patients’ ID into the same storage device to which the pupilometer is connected. After the required number of stimulus pairs is given to the patient, the device is stopped manually. The video recordings obtained from the study group are processed and analyzed to observe the changes in pupil diameter with respect to time [41]. MATLAB program segregates the video file into multiple frames at a predefined rate. For each given frame, area of the pupil, state of light and the time interval of the frame is calculated. A graph is plotted with area of pupil vs. time to get a pictorial and quantitative representation of the pupil responses. The proposed device was used on control group of 30 normal volunteers and a study group of 30 RAPD patients as shown in (Table 1-6).
| Gender | Number of patients |
|---|---|
| Males | 13 |
| Females | 17 |
Table 1: Number of Patients with RAPD.
| Eye with RAPD | Number of patients |
|---|---|
| Right | 14 |
| Left | 16 |
Table 2: No. of RAPD Patients with left and right.
| Age Range | Number of Patients |
|---|---|
| 20-29 | 14 |
| 30-39 | 7 |
| 40-49 | 6 |
| 50-59 | 3 |
Table 3: RAPD patients with different age groups.
| Grade | Right | Left |
|---|---|---|
| Grade 1 | 3 | 4 |
| Grade 2 | 2 | 4 |
| Grade 3 | 9 | 7 |
| Grade 4 | 0 | 1 |
Table 4: RAPD grading of Left and right eyes.
Gender |
Number of subjects |
|---|---|
| Males | 3 |
| Females | 27 |
Table 5: Normal subjects gender wise.
| Age range | Number of subjects |
|---|---|
| 20-29 | 13 |
| 20-39 | 8 |
| 40-49 | 6 |
| 50-59 | 3 |
Table 6: Normal subjects with different age groups.
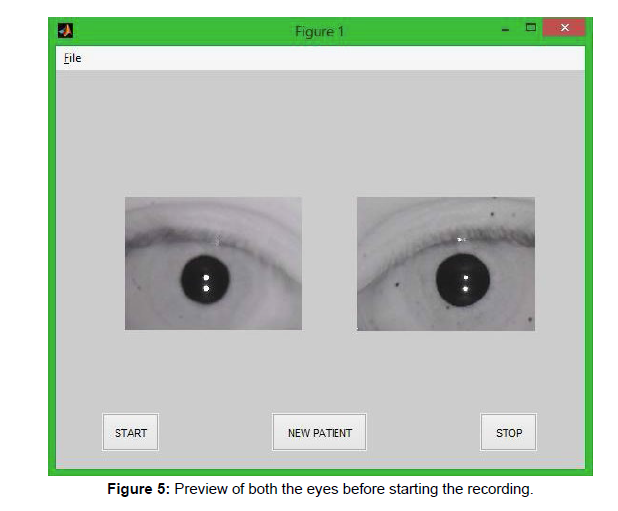
Experimental setup shown consists of the data collection pupilometer connected to a desktop/laptop with a Graphical User Interface (GUI) as shown in (Figure 4). Images acquired are preprocessed and the initial image displayed in the preview pane as shown in (Figure 5).
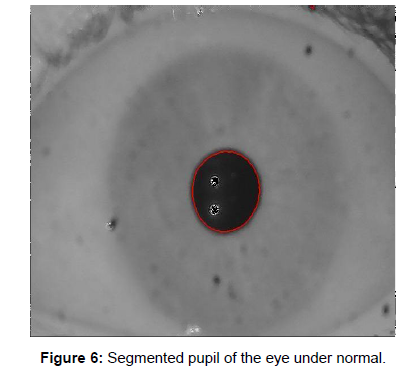
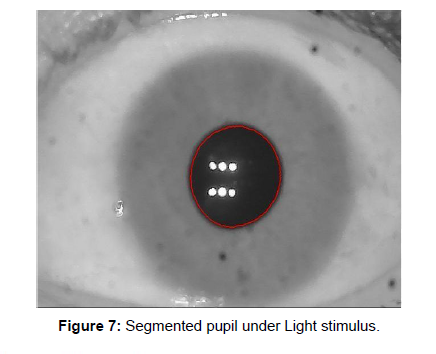
Every video is divided into many frames. Each frame is processed using OpenCV libraries to detect pupils. The Open CV software enables live detection and tracking of pupils in each frame followed by radius calculation of the same. Area of pupil is calculated for all the frames in Pixels as shown in (Figure 6 & 7).
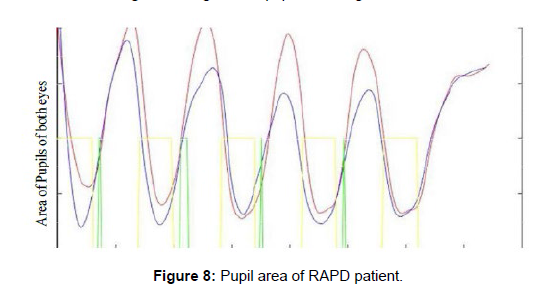
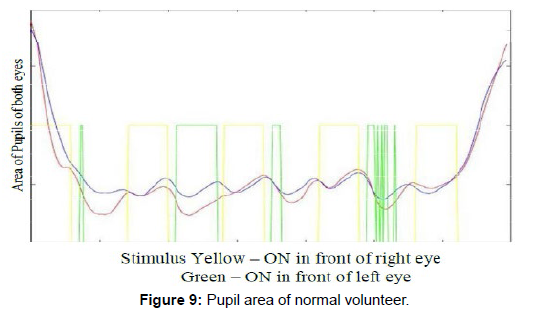
Pupil area of RAPD patients under the visual stimulus of both eyes is plotted in (Figure 8) in which the left eye is under the stimulation of yellow LED, right eye is with Green LED [42]. Similarly the pupil area of normal volunteers is plotted in (Figure 9).
Results and Discussions
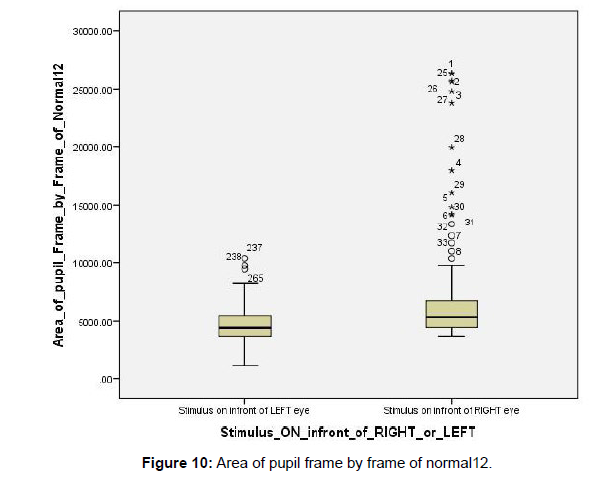
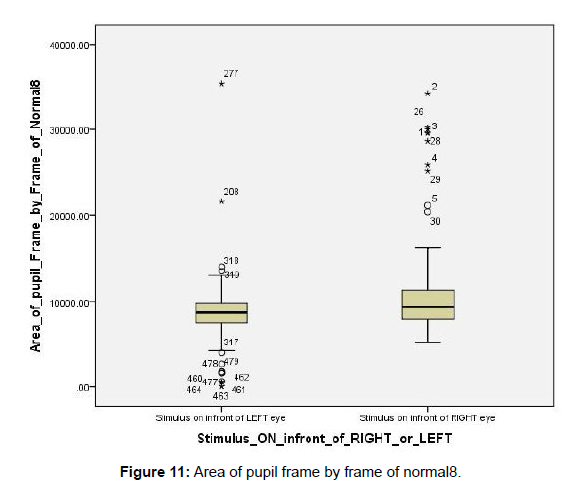
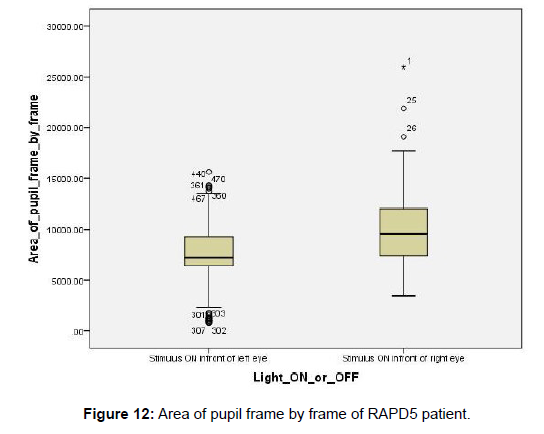
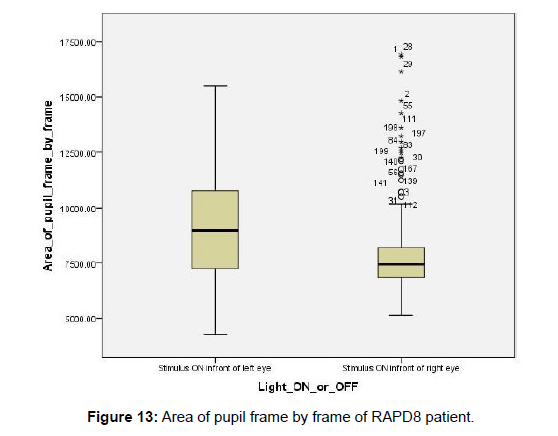
The difference between “Mean ranks” score of area of pupil when “Stimulus ON in Right eye” vs. “Stimulus ON in Left eye” are checked in both “Normal group” (Figures 10 and 11) and “RAPD group” (Figures 12 and 13). The Asymptomatic Significance (2-tailed) value indicates if the difference is significant between the two independent values “Stimulus ON in Right eye” and “Stimulus On in Left eye” with regard to the dependent variable “Area of pupil”. The difference between “Sum of ranks” score of area of pupil when “Stimulus ON in Right eye” vs. “Stimulus ON in Left eye” can also be checked in both “RAPD group” and “Normal Group”.
RAPD Group
In RAPD group, all the results clearly show that the Mean rank and Sum of rank of area are high in the “Eye with RAPD” when stimulus is ON in that eye compared to the good eye (Unaffected eye) in all patients except three. The Asymptomatic Significance (2 tailed) score shows that the difference of Mean ranks when Stimulus is ON in RAPD eye vs. Stimulus ON in Good eye is highly significant in all the patients [43]. In Patient 13 (grade 3), Patient 19 (grade 1), Patient 24 (grade 1) the Mean ranks are high in the good eye rather than the RAPD eye and the Significance of the difference between these two groups is also high.
Normal Group
When Stimulus ON in Right the Mean ranks are high in 22 Normal volunteers and when Stimulus ON in Left Mean ranks are high in 8 Normal volunteers. The difference is always present between the two variables “Stimulus ON in Right” vs. “Stimulus ON in Left”. The difference is significant in 21 Normal volunteers and not significant in the rest 9 Normal volunteers. Out of 21 significant Normal volunteers, when Stimulus is ON in Right the Mean rank are high in 16 Normal and for the rest 5 Normal the Mean rank is high when Stimulus is ON in left. Out of 9 significant Normal volunteers, the Mean rank are high in 6 Normal’s when Stimulus is ON in Right and 3 Normals when Stimulus is ON in Left. The reasons for the presence of significant area difference when Stimulus ON in Right” vs. “Stimulus ON in Left” in Normal’s also could be due to the limitations present which are still being worked on. In patients with RAPD, due to damage in pupillary pathway, the pupils are eye is larger by default [44, 45]. When light falls on eye with RAPD, as the pupils dilate naturally, most of the time the LED flashes are within the pupil and area is calculated correctly. When light falls on good eye the pupils constrict naturally and the area of pupil which is already smaller is calculated much lesser. In Normal subjects, because there is no damage at all the pupils are normal and when light falls on either of them both pupils constrict very small. This leads to LED flashes fall on pupil boarders and the area is calculated improperly.
No repeatability: As we cannot make sure that each time when the same patient is tested the pupils of positioned exactly at same place in a frame, the area calculated for the same patient are completely different every single time.
No relativity: As we cannot say that in a relative or same frame of both eyes the LED flash reflections are always within the pupil or outside the pupil similarly for both eyes, we cannot compare both eyes relatively. This could be the cause for high difference in areas in Normal subjects [46].
Statistical Analysis
Statistical Analysis using Mann-Whitney U test, a non-parametric test is performed to calculate the difference between obtained areas of pupil in Right vs. Left eye stimulation [47]. As the distribution of two groups (area values when stimulus is in Right and Left) have a different shape, mean ranks are compared rather than medians. In RAPD study group, the results clearly show that the Mean rank and Sum of rank of area are high in the “Eye with RAPD” when stimulus is ON than that compared to the unaffected eye in nearly 80% of the patients [48].
Conclusion and Future Scope
The proposed Novel device christened as Pupil+ is helpful in diagnosing the ocular disease called, RAPD. At current stage, the device met its objective of removing the human element in testing RAPD and differentiating between a Normal and RAPD patient only if the light stimulus falls within pupil area of the eyes. The proposed project offers a wide scope of further improvements. Quality of the device can be improved in every aspect so that fully automated equipment which produces a complete report of pupil evaluation with several parameters can be developed at industrial level for public use.
Acknowledgement
This work is financially supported by Department of Science and Technology, Govt. of India under TSCOST-DST, GoI-project related grants Lr.No.03/TSCOST/DST-PRG/2021-22.The authors also thank the TEQIP (Technical Education and Quality Improvement Program) Phase-III of World Bank initiative to promote technical education in India, for extending the financial support to procure the equipment, and Software.
References
- Richard Snell S, Michael Lemp A. Clinical Anatomy of the Eye; Second Edition.
- Clinical Anatomy of the Visual System; Second Edition – LEE ANN REMINGTON.
- Jack Kanski J. Clinical Ophthalmology; Sixth Edition.
- Bell, Raymond A. (1993) Clinical grading of relative afferent pupillary defects. Arch Ophthalmol
- Clinical-content-the-relative-afferent- pupillary-defect.
- Thompson H, Stanley, James J, Corbett (1991) Asymmetry of pupillomotor input. Eye 1: 36-39.
- Cox Terry A. Pupillary escape. Neurology 42: 1271-1271.
- Enyedi, Laura B, Sundeep Dev, Terry Cox A (1998) A comparison of the Marcus Gunn and alternating light tests for afferent pupillary defects. Ophthalmology 105: 871-873.
- Graefe VA (1855) Mitteilungen vermischten Inhalts: 12: Ueber ein einfaches Mittel, Simulation einseitiger Amaurose zu entdecken, nebst Bemerkungen ueber die Pupillar- Kontraction b^i Erblindeten. Arch f Ophth 2:266.
- Gerold, Hugo (1846) Die Lehre vom schwarzen Staar u. dessen Heilung. Rubach.
- Hirschberg J (1884) Neuritis retrobulbaris. Z Prak Augenh 8: 185.
- Baquis E (1901) La reazione pupillare come elemento diagnostico differenziale tra l'amaurosi isterica e quella da nevrite retro-bulbare. Ann. Ottal 30: 901.
- Gunn, Marcus R (1904) Discussion on retro-ocular neuritis. BMJ 1285-1287.
- Kestenbaum, Alfred (2013) Clinical methods of neuro-ophthalmologic examination. Elsevier.
- LEVATIN, PAUL (1959) Pupillary escape in disease of the retina or optic nerve. AMA Arch Ophthalmol 62: 768-779.
- Thompson, Stanley H (1966) Afferent pupillary defects: Pupillary findings associated with defects of the afferent arm of the pupillary light reflex arc. Am J Ophthalmol 62: 860-873.
- Thompson, Stanley H (1976) Pupillary signs in the diagnosis of optic nerve disease. Trans Opthal Soc UK 96: 377.
- Digre KB. Principles and techniques of examination of the pupils, accommodation, and the lacrimal system. Walsh & Hoyt’s clinical neuro-ophthalmology 1: 933-1040.
- Thompson, Stanley H, James J, Corbett, Terry Cox A. How to measure the relative afferent pupillary defect. Surv Ophthalmol 26: 39-42.
- Arnold, Robert W. Quantification of afferent pupillary defect by double polarized filter. Arch Ophthalmol 108: 1666-1667.
- Rosenberg, Michael L, Armando Oliva (1990) The use of crossed polarized filters in the measurement of the relative afferent pupillary defect. Am J Ophthalmol 110: 62-65.
- Ramsay, Andrew (1995) Crossed polarising filters to measure relative afferent pupillary defects: reproducibility, correlation with neutral density filters and use in central retinal vein occlusion. Eye 9: 624-628.
- McCormick A (2002) Quantifying relative afferent pupillary defects using a Sbisa bar. Br J Ophthalmol 86: 985-987
- Bremner FD (2004) Pupil assessment in optic nerve disorders. Eye 18: 1175-1181.
- Kawasaki Aki, Paula Moore, Randy Kardon H (1996) Long-term fluctuation of relative afferent pupillary defect in subjects with normal visual function. Am J Ophthalmol 122: 875-882.
- Lam, Byron L, Stanley Thompson H (1999) An anisocoria produces a small relative afferent pupillary defect in the eye with the smaller pupil. Neuro-Ophthalmol 19: 153-159.
- Lam, Byron L, Stanley Thompson H (1990) A unilateral cataract produces a relative afferent pupillary defect in the contralateral eye. Ophthalmology 97: 334-338.
- Stern, HJ (1944) A simple method for the early diagnosis of abnormalities of the pupillary reaction. Br J Ophthalmol 28: 275.
- Miller, Stephen D, Stanley Thompson H (1978) Edge-light pupil cycle time. Br J Ophthalmol 62: 495-500.
- Miller, Stephen D, Stanley Thompson H (1978) Pupil cycle time in optic neuritis. Am J Ophthalmol 85: 635-642.
- Hamilton W, Drewry RD (1983) Edge-light pupil cycle time and optic nerve disease. Annals of ophthalmology 15: 714-721.
- Kirkham TH, Coupland SG (1981) Multiple regression analysis of diagnostic predictors in optic nerve disease. Can J Neurol Sci 8: 67-72.
- Manor RS, Yassur Y, Sira Ben I (1982) Pupil cycle time in noncompressive optic neuropathy. Annals of ophthalmology 14: 546-550.
- Weinstein JM, Van Gilder JC, Thompson HS (1980) Pupil cycle time in optic nerve compression. Am J Ophthalmol 89: 263-267.
- Manor RS, Yassur Y, Sira Ben I (1982) Pupil cycle time in space occupying lesions of anterior optic pathways. Annals of ophthalmology14: 1030-1031.
- Wilhelm, Helmut (2007) The prevalence of relative afferent pupillary defects in normal subjects. J Neuroophthalmol 27: 263-267.
- Radzius, Aleksandras (1989) A portable pupilometer system for measuring pupillary size and light reflex. Behav res meth instrum comput 21: 611-618.
- Kalaboukhova, Lada, Vanja Fridhammar, Bertil Lindblom (2006) An objective method for measuring relative afferent pupillary defect in glaucomatous optic neuropathy-stimulus optimization. J Neuro-Ophthalmol 30: 7-15.
- Miki, Atsushi (2006) Pupillography of relative afferent pupillary defect contralateral to monocular mature cataract. Can J Ophthalmol 41: 469-471.
- Miki, Atsushi (2008) Pupillography of relative afferent pupillary defects in amblyopia associated with peripapillary myelinated nerve fibres and myopia. J Pediatr Ophthalmol Strabismus 45: 309-312.
- Cohen, Liza M (2015) A novel computerized portable pupillometer detects and quantifies relative afferent pupillary defects. Curr Eye Res 40: 1120-1127.
- Volpe, Nicholas J (2000) Portable pupillography of the swinging flashlight test to detect afferent pupillary defects. Ophthalmology 107: 1913-1921.
- Cox, Terry A (1989) Pupillographic characteristics of simulated relative afferent pupillary defects. Investigative ophthalmology & visual science 30: 1127-1131.
- Volpe, Nicholas J (2009) Computerized binocular pupillography of the swinging flashlight test detects afferent pupillary defects. Current eye research 34: 606-613.
- Miki, Atsushi (2008) Pupillography of automated swinging flashlight test in amblyopia. Clinical ophthalmology 2: 781.
- Dara Lankaranian MD, George Spaeth L (2005) The usefulness of a new method of testing for a relative afferent pupillary defect in patients with ocular hypertension and glaucoma. Trans Am Ophthalmol Soc 103: 200-208.
- Benson MT (1991) A novel approach to the assessment of afferent pupillary defects. Eye 5: 40-44.
- Shwe-Tin, Audrey (2012) Evaluation and calibration of a binocular infrared pupillometer for measuring relative afferent pupillary defect. Journal of Neuro-Ophthalmology 32: 111-115.
Indexed at, Google Scholar, Crossref
111: 938-942.
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Citation: Srinivas M, Krupa Rani G, Das AV, Suman D (2023) Design andDevelopment of a Pupilometer for the Automatic Detection of Relative AfferentPupillary Defect. Optom Open Access 8: 187. DOI: 10.4172/2476-2075.1000187
Copyright: © 2023 Srinivas M, et al. This is an open-access article distributedunder the terms of the Creative Commons Attribution License, which permitsunrestricted use, distribution, and reproduction in any medium, provided theoriginal author and source are credited.
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 2138
- [From(publication date): 0-2023 - Apr 24, 2025]
- Breakdown by view type
- HTML page views: 1775
- PDF downloads: 363