Dermatologic Complications of Dermabond after Orthopaedic Surgery: A Case Report and Review of the Literature
Received: 17-Jun-2016 / Accepted Date: 20-Jul-2016 / Published Date: 22-Jul-2016 DOI: 10.4172/2161-0681.1000286
Abstract
We present a case of allergic contact dermatitis in a patient after multiple orthopaedic procedures. The patient demonstrated a foreign body reaction as well as classic contact dermatitis in response to two exposures to Dermabond. Both reactions were successfully treated with topical corticosteroids. As the popularity of Dermabond increases within the medical community, awareness of potential complications is necessary to improve patient care and outcomes.
Keywords: Dermabond; Contact dermatitis; 2-Octylcyanoacrylate; Cyanoacrylate
314272Introduction
Dermabond (2-octylcyanoacrylate) use has gained popularity due to its convenient quick application without comprising the cosmetic or functional integrity of the surgical wound. Reports of dermatitis after Dermabond use are rare in the medical literature, although there appears to be a recent rise in the report of complications with Dermabond use [1-10]. We present a case of an adult patient who developed allergic contact dermatitis to Dermabond after multiple orthopaedic operations.
Case Report
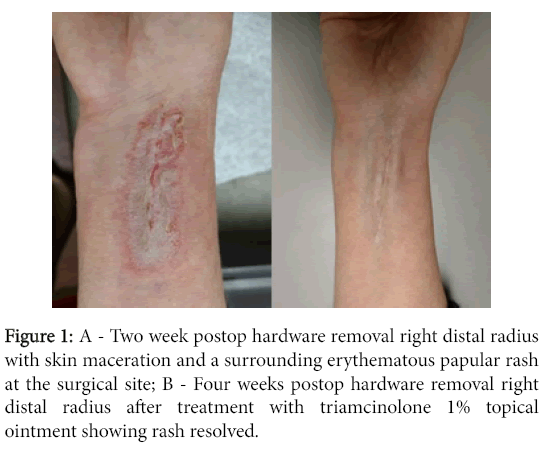
A 57-year-old woman underwent uneventful removal of symptomatic hardware at her right distal radius. Preoperative cefazolin was given. The wound was closed in layers with 4-0 monocryl subcuticularly and Dermabond on the skin. There were no complaints of pruritus or rashes noted postoperatively. The dressings were removed at the two week follow-up visit. At this time, skin maceration with a surrounding erythematous papular rash was noted at the surgical site (Figure 1).
There was no residual Dermabond noted on the skin. The surgeon and an attending dermatologist agreed that the rash was consistent with an allergic contact dermatitis (type IV hypersensitivity) reaction to the Dermabond. The patient was treated with triamcinolone 1% topical ointment which resolved the rash within 2 weeks.
This patient had no previous known contact allergies. She had 2 prior surgeries; first with right distal radius open reduction internal fixation and then following with ganglion cyst removal of the foot. Both surgeries were performed by the same surgeon. All wound closure methods utilized 4-O monocryl subcuticularly followed by Dermabond superficially (Figure 1).
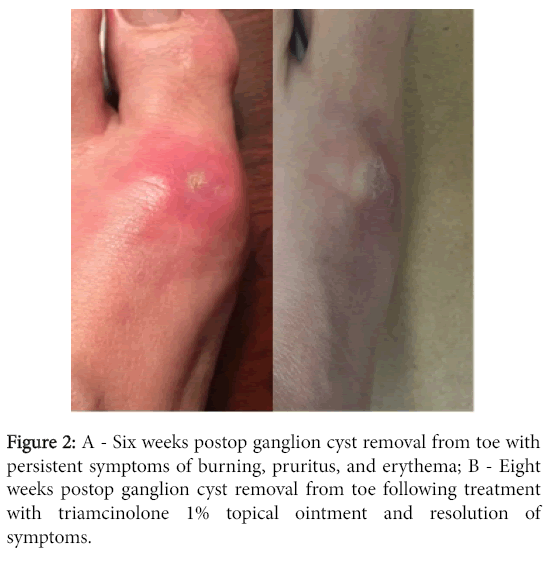
After 1 week following ganglion cyst removal, the patient noted mild erythema and serous drainage at her surgical site without fever or chills. She initially presented to her primary care physician who prescribed cephalexin for presumed surgical site infection. At the 2 week postoperative follow-up visit, erythema and persistent Dermabond overlying the wound were noted.
There were no signs of drainage or infection at that time. At the 6 week postoperative follow-up visit, the patient reported persistent symptoms of burning, pruritus, and erythema (Figure 2). No remaining Dermabond was noted on her skin at that time. She was prescribed triamcinolone 1% topical ointment and the symptoms resolved (Figure 2).
Discussion
Dermabond is a liquid adhesive composed of 94%, 2- octylcyanoacrylate (2OCA) and 6% plasticizers. The cyanoacrylate monomer polymerizes after contact with moisture on the skin surface to bridge the edges of the wound. This exothermic reaction generates heat and formaldehyde, which may cause inflammation at the site of application. Dermabond releases less degradation products than alternative cyanoacrylates (e.g. ethyl cyanoacrylate) and is expected to disappear in 7-14 days along with the sloughing epidermis [4].
Dermabond’s rapidity and reactivity should theoretically prevent its haptens from reaching immunomodulators due to the immediate bonding of the cyanoacrylate to keratinocytes [7]. However, as demonstrated in our patient, type IV hypersensitivity reactions can occur if haptens are engulfed by antigen presenting cells that live in cutaneous tissue. This can result in sensitization of local Tlymphocytes and a subsequent T-cell mediated inflammatory reaction at the skin.
Eight previous reports describe sensitization to 2OCA in adult patients [2-9]. Durando et al. reported 15 patients who complained of rash ranging from 1-3 weeks postoperatively, none of the patients had a history allergic reaction to skin adhesives. It is unclear whether any patients had prior exposures to Dermabond. All patients were treated with topical steroids. McDonald et al. described two patients complaining of rash. One patient had no previous Dermabond exposure and complained of rash three weeks postoperatively. The rash was reported to be refractory to topical steroids, and lasted three months. The other patient had been previously exposed to 2OCA and her rash developed within thirty six hours of Dermabond application. The rash was stated to persist two weeks although no treatment methods were reported. Sachse et al. reported one patient who noted rash immediately postoperatively. It is unclear if the patient had prior exposure to Dermabond. The authors initially suspected wound infection and treated the patient with ciprofloxacin. The rash resolved with topical gentamicin and steroids. Howard et al. described two patients complaining of rash one week postoperatively. It is unclear if either patient had previous exposure to Dermabond. Both patients were treated by removing residual Dermabond using dilute acetone. Bowen et al. reported on four patients, all complained of rash one week postoperatively. One patient reported no prior exposure to 2OCA or history of contact dermatitis. Three patients reported prior Dermabond exposure with no subsequent reaction. Hivnor et al. reported one patient with no known allergies who developed rash one week postoperatively. However, it is unclear whether this patient had prior exposure to 2OCA. The patient was treated with Dermabond removal and topical steroids. Perry et al. described one patient who reported rash one week postoperatively. The patient’s history was significant for prior exposure to Dermabond that embedded within the surgical wound, causing chronic wound drainage for four months. The drainage resolved with excision of residual Dermabond. El-Dars et al. described one patient who developed rash at four weeks postoperatively. The patient had a history of atopic eczema but no prior Dermabond exposure. Sensitization to Dermabond was attributed to prolonged adhesive exposure.
One report described sensitization to Dermabond in pediatric patients [10]. All patients complained of pruritus or rash within two weeks of their operations. All patients had histories of multiple orthopaedic operations. However, the report suggested that none of the patients had any prior exposure to Dermabond.
Allergic contact dermatitis due to Dermabond most frequently presents rapidly after patients’ exposure to the adhesive. However, two previous reports noted a gradual sensitization to Dermabond in their patients. El-Dars et al. noted their patient still had Dermabond present over the surgical site at four week follow-up, indicating a delay in the expected sloughing off of Dermabond [4]. They concluded that this prolonged skin exposure led to sensitization to Dermabond, and recommended removal of residual adhesive beyond two weeks. Perry et al. reported on a patient with rash after multiple exposures to Dermabond [6]. The authors believed that haphazard application of Dermabond during a prior surgery led to embedded adhesive in the surgical wound and ultimately sensitization to Dermabond. The authors noted that careful wound closure and Dermabond application were necessary to prevent any embedding of Dermabond in the wound. Bowen et al. reported on two patients who developed 2OCA allergy after their initial exposure, however were not allergic to 2-butyl cyanoacrylate containing compounds upon further investigation. They proposed a technique for identifying the component of acrylate adhesives responsible for patients’ reactions [5].
Our patient had no complaints or visible reaction after her first exposure to Dermabond. After her second exposure, however, the patient complained of pruritus, erythema, burning, and drainage from her surgical site. This may have been due to Dermabond embedded in the wound that caused a foreign body reaction, which has been described in previous reports [1,6]. Additionally, our patient maintained her postoperative dressings after all surgeries for 2 full weeks, which may have further contributed to prolonged Dermabond contact. These symptoms resolved with cephalexin and later topical steroid administration, without Dermabond excision or invasive manipulation of the surgical site (Figure 2). The final exposure to Dermabond resulted in an allergic contact dermatitis that quickly resolved with topical steroid application.
As the popularity of Dermabond continues to rise, it becomes increasingly important to understand its risks and the presentation of allergic contact dermatitis. In particular, distinguishing the presentation of contact dermatitis from postoperative infection prevents unnecessary interventions and expedites resolution of any inflammatory processes at the surgical site. Meticulous wound closure and Dermabond application, as well as prevention of prolonged adhesive exposure, decrease the likelihood of sensitization to Dermabond. For patients who have previously had erythema or drainage from wounds closed with Dermabond, clinicians should be mindful of the possibility of sensitization and allergic contact dermatitis with subsequent exposures. The use of an alternative closure method may be warranted under these circumstances. Should a foreign body reaction develop to Dermabond, a trial of topical steroids may be considered prior to invasive manipulation of the surgical wound.
References
- Dragu A, Unglaub F, Schwarz S, Beier JP, Kneser U, et al. (2009) Foreign body reaction after usage of tissue adhesives for skin closure: a case report and review of the literature. Arch Orthop Trauma Surg 129: 167-169.
- McDonald BS, Buckley DA(2014) Severe dermatitis from Dermabond ® surgical glue. British Journal of Dermatology 170:739-741.
- Durando D, Porubsky C, Winter S, Kalymon J, O’Keefe T, et al. (2014) Allergic contact dermatitis to dermabond (2-octyl cyanoacrylate) after total knee arthroplasty. Dermatitis 25: 99-100.
- El-Dars LD, Chaudhury W, Hughes TM, Stone NM (2010) Allergic contact dermatitis to Dermabond after orthopaedic joint replacement. Contact Dermatitis 62: 315-317.
- Bowen C, Bidinger J,Hivnor C, Hoover A, Henning JS(2014) Allergic Contact Dermatitis to 2-Octyl Cyanoacrylate. Cutis 94:183-186.
- Perry AW, Sosin M(2009) Severe Allergic Reaction to Dermabond. Aesthetic Surg J 29:314-316.
- Hivnor CM, Hudkins ML(2008) Allergic Contact Dermatitis After Postsurgical Repair with 2-Octylcyanoacrylate. Arch Dermatology 144: 814-815.
- Sachse MM, Junghans T, Rose C, Wagner G (2013) Allergic contact dermatitis caused by topical 2-octyl-cyanoacrylate. Contact Dermatitis 68:317-319.
- Howard BK, Downey SE (2010) Contact dermatitis from Dermabond. Plastic and Reconstructive Surgery 125:252e-253e.
- Gonzalo-Garijo MA, Perez-Calderon R, Perez-Rangel I, Sanchez-Vega S, Constantino JA, et al. (2009) Contact dermatitis after orthopaedic surgery. Contact Dermatitis 61: 299-300.
Citation: Carayannopoulos N, Sun D (2016) Dermatologic Complications of Dermabond after Orthopaedic Surgery: A Case Report and Review of the Literature. J Clin Exp Pathol 6:286. DOI: 10.4172/2161-0681.1000286
Copyright: © Carayannopoulos N, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 31565
- [From(publication date): 8-2016 - Apr 04, 2025]
- Breakdown by view type
- HTML page views: 30506
- PDF downloads: 1059