Depression and Stress Management for Caregivers of Traumatic Brain Injury Patients
Received: 06-Jan-2019 / Accepted Date: 18-Feb-2019 / Published Date: 25-Feb-2019 DOI: 10.4172/2375-4494.1000383
Abstract
Aim of the Study: The aim of this study is to help the professionals to understand what it means for families to be confronted with Traumatic Brain Injury (TBI).
Materials and Methods: We performed a literature review on the scales used for caregivers of head trauma patients and related psychological constructs. This study analyzed the life of the family and reactions to stress event such as head trauma.
Results: The scientific literature on this topic, however, is poorly organized, and general articles are rare. Furthermore, although several specific aspects of the impact of brain trauma on the family system were analyzed, others were overlooked.
Conclusions: Recent state of the science reports have acknowledged the importance of family intervention and have encouraged researchers to conduct studies that benefit caregivers.
Keywords: Anxiety; Brain damage; Depression; Mourning; Caregiver
Introduction
Traumatic Brain Injury (TBI) is one of the leading causes of death and disability around the world. TBI often results in cognitive, behavioral, and emotional deficits which can negatively impact the injured individual’s ability to lead an independent life, maintain employment, and sustain relationships. Because of the wide-ranging difficulties associated with TBI, individuals often require supervision and support from caregivers, most typically partner or parents. A high level of burden can lead to deterioration in caregivers’ health status, social life and well-being and can have negative effects on the wellbeing of TBI subject and on the outcome of their rehabilitative treatment [1]. TBI caregivers, compared to the general population, also have higher rates of psychiatric elasticity and can experience significant levels of stress, anxiety, depression, and burden. Rates of depression among TBI caregivers are often high (22% to 77%), and symptoms can persist for years after the onset of TBI. It is not so much care for the patient, but the constant sense of responsibility towards him/her and worries about the person with brain damage that leads to a state of stress. In this perspective, experienced burden is to a large extent an emotional construct [2].
Rehabilitative programs addressing the patients’ level of functioning and participation can reduce the level of emotional stress on the caregiver [3]. This review revisits all literature data regarding TBI caregiver’s outcome, focusing on relatives' stress and burden. Different works, using various samples of relatives caring individuals with a range of TBI severity and different psychosocial outcome measures, have showed findings of outcome in caregivers following TBI. The aim of the present review is to show which factors are highly associated with stress and depression in caregivers of persons with TBI and to assess the correct management for these caregiver’s perceptions.
Materials and Methods
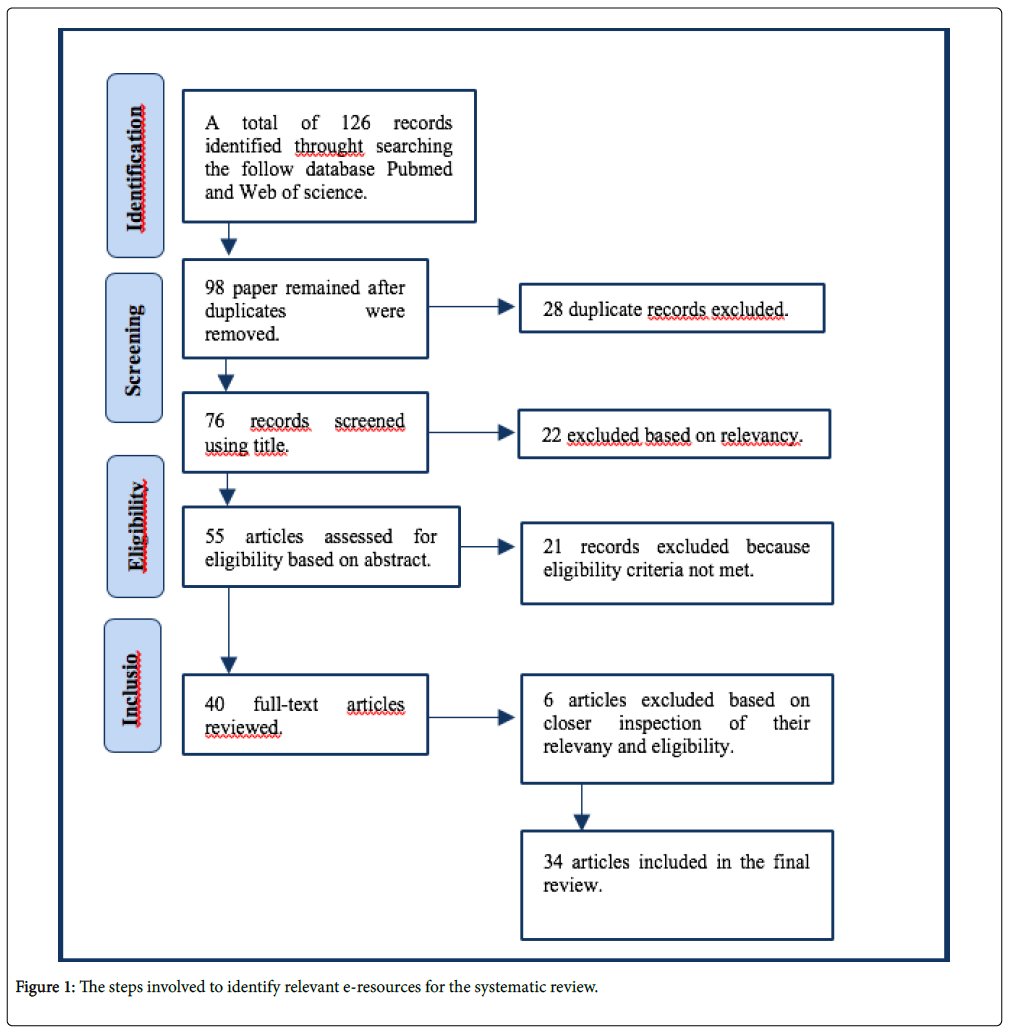
Studies on stress and depression in caregivers of persons with TBI and to assess the correct management for these caregiver’s perceptions were selected for this descriptive review. Studies were identified by searching electronic databases, scanning reference lists of articles and consultation with experts in the field. This search was applied to the PubMed database and Web of Science and was performed on everything prior to January 2018 (Figure 1).
Results
Family stress
Stress and depression are two clinical conditions often considered by those who care for family members of patients with TBI [4]. Previous research in developmental disability, mental health has found that carer distress is also associated with a number of beliefs about these behavioral difficulties, including the belief that the person being cared for is able to control the behavior, and the belief that the behavior is motivated by hostile intentions towards the carer [5]. When a subject suffering from severe TBI, it happens that all family members are subjected to a shock because suddenly and unexpectedly an event "steals" the related from everyday life; they are hospitalized in Intensive Care Units (ICU). For the whole family there is a real ordeal waiting for a revival, while waiting for a contact with medical doctors, waiting for "good news" [6]. The need to "take care" of their loved one in the family increases, a need that cannot always be met in the ICU: in fact, this pressure makes caregivers them extremely attentive to every gesture and expression of who takes care in place of them. This often creates tension and conflict among family members and operators. Family members often live the care of the medical and nursing staff as "technical practices", little "emotional", and greatly suffer of not being able to provide enough love to their loved ones and to satisfy their needs in this acute phase [7]. Emerging from the stories of families and field studies, at this stage a number of needs of family members can be summarized as follows: the need of information and education about what is happening to their loved one and what is his/her forthcoming for the future and the need for instruction and training in order to perform the practices of care [8]. Among the factors that influence the lives of the families of people in a state of minimal responsiveness, are the type of severity of the trauma, the diversity of practices of care needed, and the presence of more family members or significant others [8].
As there are strengths that help to sustain the family members at this stage, so there are weaknesses that may further aggravate the psychological state of each family, removing and preventing first of all an effective reorganization [9]. Difficult relationships, lack of sharing and dialogue, social isolation, the tendency to "dwell on the pain," unrealistic expectations, lack of information, a period of stress that goes on too long and becomes chronic, are factors that must be kept under control and which deserve early intervention. In fact the risk is that these factors can become chronic and may hinder the process of development that must be fulfilled in the later stages [9].
In many occasions this kind of trauma has the power to change the skills of families to deal with the problem. Assessed the impact on the family structure, it is seen that in the acute phase previous methods used in other periods of stress are subverted: the ability to face the problem goes to the behavior dictated by emotions, alternating instinctive and rational modes [10].
The trauma, from the first moments, directly involves the whole family, so in early phases a treatment is required for all members. The analysis of strengths that need to be stimulated and developed and of weaknesses that have to be clarified and limited, is really important from the first moments.
Family members are entitled to assistance as well as their loved ones who have suffered trauma, interventions must be multiple and tailored to meet the needs arising from the first days after the event [11].
Arango-Lasprilla et al., [12] evaluated levels of anxiety and depression in partner of TBI subjects on the Symptom Checklist -90 (-90 SCL), scales demonstrate significantly elevated affective symptoms, with 73% recognizing the symptoms of depression and 55% showed symptoms of anxiety. To estimate the percentage of affective symptoms in respondent’s partner of TBI subjects, these researchers showed increases in depression and anxiety with different stage [12]. However, the same data also reported that an elevate percentage of partners not showed or only have mild elevations of depression and anxiety levels. In addition, Linn et al. noted that the increase of anxiety and depression symptoms is not necessarily related to a serious behavioral condition [12]. Kreutzer et al. [13] reported the neuropsychological status and family functioning of an elevated number of primary TBI caregivers, 16 months after injury. They showed that family members benefit from interventions planned to meet their specific needs after TBI. Not sure findings remain about the benefits of intervention for general family functioning and life level satisfaction. Measures of functioning caregiving are the Brief Symptom Inventory [14] and the Family Assessment Device (FAD) [15]. The FAD is a good tool for the self-assessment, which consists of 60 multiple choice items rated on a 4-point Likert scale.
The awareness of family
Given the burden on the individual and the family resulting from a TBI, it is not surprising that caregivers have many important family needs. Kreutzer et al. [13] identified caregiver needs, including the importance to have information on the exact problems of the patient, the access to someone who can answer questions about patient care in a truthful manner, the access to professionals’ advice to ensure the best care for the patient and the respect by all health professionals [16]. Similarly, Leith et al. [17] identified five major family needs in TBI care as reported by caregivers: 1. A statewide agency, a delivery system and support services that can facilitate appropriate placement and treatment; 2. Facilities and outlets for information and education on TBI; 3. Support and encouragement given to TBI patients and caregivers from health professionals; 4. Aid in creating an enthusiastic and positive environment for TBI patients and families; and 5. Emotional support and enhanced community re-integration after injury. In general, a family caregiver needs to emphasize communication of information regarding patient care and improving communication with medical staff [18]. Several studies also describe important unmet family needs in relation to caring for an individual with TBI [13]. The awareness of the family comes gradually over time, thanks to the daily contact with the person who is not really him/her, who has a different look, who no longer has the same body and does not think as before the trauma. Indeed, the perception of the patient's quality of life is usually better than that of caregivers [19]. The desire and the hope that all this will change a lot, which is the only way that allows familiars to get up in the morning. At this stage the depression of the family can be found in every word and movement [20].
It is known that the denial of the family freezes or slows down the recovery of the patients. In some cases, home devalues the work of rehabilitative professionals, for example replacing the person in the gestures and actions that has learned to do because it is too slow, instead other times they have made excessive demands to the person: "If you want to remember or walking, if you commit yourself you really can do it" or otherwise, the requests are too basic and undermine the person which makes them feel excluded from the family and social life: "You cannot go out with friends in a wheelchair" [21-22].
Among the factors facilitating the path of awareness of family members there is social support, the possibility of access to services and a good level of social integration. Family’s need to understand what is being accessed and how to deal with it, and the information given, and needs must be carefully tailored to both in the amount of time [23]. The Family Needs Questionnaire (FNQ) is a 40-item, self-administered questionnaire designed to determine family needs of TBI patients. It measures a wide range of educational and psychosocial needs important in the acute and post-acute phases of TBI and can be used for clinical or research purposes. The most frequently met needs in the study of Edilene et al. [24] fell within Health Information, Involvement with Care and Instrumental Support sub-scales and the most frequently unmet needs fell within the Emotional Support, Instrumental Support and Professional Support sub-scales [25]. It has been shown that loss of interest, friendships and activities of each staff continue until they are completely shut off from the world of entire families. Support actions for the family at this stage are also preventive measures of future damage, in addition to the specific psychological support for individual or group as required. It is very important to facilitate and create a dense social network and support to attend daily practices (hygiene care, free time management of the disabled, holiday periods), so that each member can find relief and are able to maintain, at least in part, work, friendships and interests [12].
Family mourning
Mourning is the psychological state that follows the loss of something of important. People lose their identity, and consequently many aspects that make it up, such as autonomy and independence, work, friends, partner. In a family, this kind of mourning involves both the loss of the loved one, and the loss of the habits, dreams and projects [25]. The pain that accompanies the experience of grief is the pain of depression. In general, the feelings that arise from this state are the feelings of worthlessness, hopelessness, sleep disorders and feeding, lethargy, agitation, anxiety attacks and obsessive thoughts [26]. The mental process required to make the depressive pain more tolerable, is called a "work of mourning." It is long and complex and leads to a conscious resignation of them self to the loss. More the loss is significant, more the process is slow.
The physiological processes of mourning usually last more than one year. The necessary element for the grieving process is to be in the process of crisis and pain, without avoiding it or pretending not to feel it, then handle the painful emotion without escape. It could be argued that the loss of TBI is not a real and serious mourning, some authors have called the loss due to the severe permanent disability as "partial death" and grief as "inconstant mourning." These definitions have been given to differentiate it from traditional mourning where, probably, it is easier to internalize the loss, contrasting it to this paradoxical state in which the person is there but not there. This is true both for patients and their families. Considering the complexity of this type of mourning, it is necessary to consider different feelings and point of view respect to the patients and their families. In difficult moments the typical tendency of human mind is to remind the best part of the past, often idealizing it. Expectation, moral values, perception of reality, they all play an important role in the mourning process. This provides new perceptions of themselves, new and more functional behaviors, new goals and life plans. At this time, it is very important not to leave people alone with their own pain: it is essential to share this painful experience with someone who really understands it. Sharing in a group, with people having a similar experience, is functional to support. Rehabilitative models, that actively involve the family, have been also described; so that the path is actually functional and shared [26].
The outcome of family
In the family, the renunciation to their own lives, social withdrawal, the almost complete loss of their personal interests and friends are the first factors of permanent change that studies have highlighted, even with the difference between the primary, secondary and tertiary caregiver [13]. Generally, this happens to the disabled person and to primary caregiver, sometimes the secondary; they live almost exclusively at home, in a "closed" place, full of loneliness [27].
Some variables that influence the outcome are the severity of the trauma, the pre-morbid dynamics of the family and the role of the relative, if it is primary caregiver (mother, wife), secondary caregiver (father), or tertiary caregiver (brothers, sisters) [28]. This classification seems to us highly relevant because it describes all the aspects that are simultaneously involved in these families.
The person most exposed to psychosocial consequences is the primary caregiver, but also between the secondary and tertiary there are signs of great suffering. Between the primary caregivers there is a high incidence of psychosomatic disorders, an increase in the use of drugs and other substances, a high incidence of depression, anxiety, social withdrawal and isolation. As it can be noted, these issues overlap with those of the traumatized person, as if the type of psychological stress was the same [15]. The literature shows that the discomfort is proportional to the duration of caregiving. If the primary caregiver is the wife, the rates of depression increase dramatically (73%) and the 55% show anxiety symptoms. The difficulty of having an equal relationship, the physical and psychological dependence, the change of sexuality, make the relationship a source of anger and frustration [29].
The secondary caregivers tend to react with anger and frustration rather than with depression and anxiety. Tertiary caregivers are a resource: in a fraternal relationship the disabled person can confront and, through it, go out and have social inclusion. They are the reason of disorder and suffering, they make parents feeling guilty because "they are left on their own, having to deal with the disabled", they feel neglected and unfortunate, they are jealous of the attention to a disabled brother, they feel guilty because they are healthy [30].
Often family members have pathological defense mechanisms, such as denial, by not accepting the patient's dysfunction [31].
It should be important that operators should notice those situations even at the stage of the outcome. In fact, there is a whole core to take charge; some professionals often have to work in synergy and close contact, for example, the psychologist with the family, sharing and clarifying objectives and instruments [32].
Discussion
Problems arise as a result of a serious head injury, are complex and different. They are related to physical, cognitive and emotional, aspect but also to personal, family and social life. The approach of the intervention is necessarily the network, in the sense of multidisciplinary teams that communicate with a shared and common language. An example is the awareness. It is par excellence, the border territory, or rather of union between clinical psychology and clinical neuropsychology. The contributions of the literature highlight the influence that has on TBI caregivers. Further researches were carried out on primary caregivers, and in recent years has increased the interest in these families. A significant finding that emerges from these studies is that there are no shared instruments to measure the degree of stress and depression for these families. There is a need to identify assessment tools to orientate in a more appropriate manner to the families and find the most efficient allocation to favor the rehabilitative process. It would be necessary to identify specific tools especially for those families with poor psychosocial outcome. One tool that seems to give more guidance to these families is the Brain Injury Family (BIFI). The BIFI contemplate to act to fill all the needs of a family with a dependent TBI patient. This tool has a cognitive behavioral approach to family systems [13], and the purpose is to promote coping strategies [33]. The current review highlights the need of assessment tools for TBI, which have cross-cultural validity and outcome measures that are reliable, valid, standardized, sensitive, feasible, and can produce generalizable data. Social reintegration is a complex process and its success depends both on an early holistic approach to people with BITs and their carers, but also on psycho-educational support to accompany the whole family to reintegration into the community [34]. Create more opportunities for cross-cultural, collaborative research and international meetings focused on the measurement of TBI–a specific result could help the development of useful tools for rehabilitation, in a broader professional community. These factors can be roughly grouped into three categories: patient characteristics (e.g., socio-demographic variables, injury severity, cognitive and neurobehavioral functioning, etc.), caregiver characteristics (e.g., socio-demographic variables, relationship, etc.), and caregiver perceptions (of patient functioning, of their own coping, of impact on family, etc.).
However, the majority of studies that attempt to determine predictors of caregiver burden and depression fail to include all categories of variables. Further, most studies that examine the role of subjective caregiver perceptions of patient functioning do not include objective data regarding the TBI patients’ actual functioning (Table 1).
| Questionnaire | Investigated Area | Results |
|---|---|---|
| Zung’s Self-Rating Depression Scale | Perceived Stress Scale, Social Support Questionnaire, a measure of the severity of difficult behaviors shown by the person cared for and two measures of carer beliefs about the behavior. | Higher depression and stress scores were associated with more severe behaviours and less social support. Carer belief in their own ability to control the behaviours was associated with less stress. Belief that the behaviour was under the control of the person with traumatic brain injury and/or was motivated by hostile intentions was associated with more depression but less stress. |
| Ways of Coping Questionnaire | Measures the thoughts and actions people use to handle stressful encounters | Results revealed that the majority of caregivers in those with moderate to severe brain injuries experienced dissatisfaction with many aspects of caregiving, especially with respect to feelings of burden and mastery. Additionally, interestingly, caregiving ideology was most closely related to avoidance-oriented coping. |
| FNQ | Depression and the Responses to Stress | A structural equation model indicated that secondary control coping was associated with less grief and depressive symptoms, whereas primary control coping and disengagement were associated with more symptoms. Emotional and instrumental supports were directly associated with less depressive symptoms. In addition, emotional and professional supports were associated with symptoms through the use of primary control and disengagement coping. |
| SCL-90-R | General symptom distress | The psychometric properties of the SCL-90 were evaluated. Its reliability proved to be good. Its validity as a measure of general symptom distress was also good as it discriminated and screened patients from the community as well as two widely used screening instruments. |
| FAD | Reliably assessment the family functioning | The FAD has been found to have good reliability, internal coherence and good content validity. |
| BSI | Mood & Anxiety Symptoms | Discriminative power of the BSI, MASQ-D30 and SF-36 was good, but it was poor for the DAPP-SF. For all instruments, the internal consistency of the subscales ranged from adequate to excellent. |
Abbreviation: ROM: Routine Outcome Monitoring; BSI: The Brief Symptom Inventory; SCL-90-R: The Symptom Checklist-90-R (SCL-90-R); FAD: Family Assessment Device; FNQ: Family Needs Questionnaire; MASQ D30: Mood & Anxiety Symptom Questionnaire −30; SF-36: Short Form Health Survey 36.
Table 1: Instruments of management psychological distress.
We hope that the operators will accept the challenge of this complexity and establish better and more effective inter-professional dialogues, that are definitely costly in terms of time and energy but needed to grasp all the aspects involved in these dramatic personal stories of the family. In addition to the health and social workers, it is desirable also, that this dialogue increasingly involved professionals in the legal and justice, whose sensitivity and competence are vital aspects for the entrusted, and often the fate of entire families, and even future generations.
References
- Ponsford J, Willmott C, Rothwell A (2002) Impact of early intervention on outcome following mild head injury in adults. J Neurol Neurosurg Psychiatry 73: 330-332.
- Rohling ML, Faust ME, Beverly B, Demakis G (2009) Effectiveness of cognitive rehabilitation following acquired brain injury. Neuropsychology 23: 20-39.
- Behn N, Togher L, Power E, Heard R (2012) Evaluating communication training for paid carers of people with traumatic. Brain Inj 26: 1702-1715.
- Gerard AR (2007) Stress and depression in family carers following traumatic brain injury: the influence of beliefs about difficult behaviours. Clin Rehabil 21: 82-88.
- Etchegary H (2011) Healthcare experiences of families affected by Huntington disease: Need for improved care. Chronic Illn 22: 225-238.
- Ferrara M, Langiano E, Di Brango T, Cioccio LD, Bauco C (2008) Prevalence of stress, anxiety and depression in with Alzheimer caregivers. Health Qual Life Outcomes 6: 93.
- Wilkin K, Slevin E (2004) The meaning of caring to nurses: an investigation into the nature of caring work in an intensive care unit. J Clinic Nurs 1: 50-59.
- Meyers SJ, Tomlinson PS (2003) Family-nurse co-construction of meaning: a central phenomenon of family caring. Scand J Caring Sci 17: 193-201.
- Fleming J, Sampson J, Cornwell P, Turner B, Griffin J (2012) Brain injury rehabilitation: the lived experience of inpatients and their family caregivers. Scand J Occup Ther 19: 184-193.
- Perrin PB, Stevens LF, Sutter M et al. (2013) Exploring the connections between traumatic brain injury caregiver mental health and family dynamics in Mexico city. PM&R 2: 839-849.
- Rotondi AJ, Sinkule K, Balzer J, Jeffrey H, Rene M (2007) A qualitative needs assessment of persons who have experienced traumatic brain injury and their primary caregivers. J Head Trauma Rehabil 22: 14-25.
- Arango-Lasprilla JC, Quijano MC, Aponte M, Cuervo MT, Nicholls E, et al. (2010) Family needs in caregivers of individuals with traumatic brain injury from Colombia, South America. Brain Inj 24: 1017-1026.
- Kreutzer JS, Stejskal TM, Ketchum JM, Marwitz JH, Taylor LA, et al. (2009) A preliminary investigation of the Brain Injury Family Intervention: Impact on family members. Brain Inj 23: 535-547.
- Yvonne WM, Schulte-van M, Carlier IVE, Zitman FG, van Hemert AM et al, (2012) Reference values for generic instruments used in routine outcome monitoring: the leiden routine outcome monitoring study. BMC Psychiatry 12: 203.
- Pinquart M, Sörensen S (2003) Differences between caregivers and non caregivers in psychological health and physical health: Ameta-analysis. Psychol Aging 18: 250-267.
- Friedrich RM, Lively RN, Rubenstein LM (2008) Siblings’ coping strategies and mental health services: A national study of siblings of persons with schizophrenia. Psychiatric Services 59: 261-267.
- Leith JE, Stein CH (2012) The role of personal loss in the caregiving experiences of well siblings of adults with serious mental illness. J Clinic Psychol 68: 1075-1088.
- Gana CJ, Gargarob C, Clare B, Gary G, Kathryn B (2010) Family caregivers’ support needs after brain injury: A synthesis of perspectives from caregivers, programs, and researchers. Neuro Rehabil 27: 5-18.
- Formisano R, Longo E, Azicnuda E, Silvestro D, D’Ippolito M, et al. (2017) Quality of life in persons after traumatic brain injury as self-perceived and as perceived by the caregivers. Neurol Sci 38: 279-286.
- Savage S, Bailey S (2004) The impact of caring on caregivers’ mental health: A review of the literature. Australian Health Review 27: 111-117.
- Anderson MI, Parmenter TR, Mok M (2002) The relationship between neurobehavioural problems of severe traumatic brain injury (TBI), family functioning and the psychological well-being of the spouse/caregiver: path model analysis. Brain Inj 16: 743-757.
- Lohrer S, Lukens E, Thorning H (2007) Economic expenditures associated with instrumental caregiving roles of adult siblings of persons with severe mental illness. Health J 43: 129-151.
- Lefebvre HG, Cloutier M, Levert B (2009) Perspectives of survivors of traumatic brain injury and their caregivers on long term social integration. Brain Inj 22: 535-543.
- Edilene CH, Cardoso De Sousa RM (2009) Cross-cultural adaptation of the instrument “Family Need Questionnaireâ€, Rev. Latino-Am. Enfermagen.
- Corbo G, Molinari ME (2010) Burden, depression, and anxiety in caregivers of people with amyotrophic lateral sclerosis. Psychol Health & Medicine 15: 685-693.
- Ducharme JM (2003) Errorless rehabilitation: strategies of proactive intervention for individuals with brain injury and their children. J Head Trauma Rehabil 18: 88-104.
- De Silva MJ, Roberts I, Perel P, Edwards P, Kenward MG (2008) Patient outcome after traumatic brain injury on high-, middle- and low-income countries: Analysis of data on 8926 patients in 46 countries. Inter J Epidemiol 38: 1-7.
- Calvete E, De Arroyabe EL (2012) Depression and grief in Spanish family caregivers of people with traumatic brain injury: the roles of social support and coping. Brain Inj 26: 834-843.
- Lehan T, Arango-Lasprilla JC, De Los Reyes CJ, Quijano MC (2012) The ties that bind: the relationship between caregiver burden and the neuropsychological functioning of TBI survivors. Neuro Rehabilitation 30: 87-95.
- GarcÃa JF, Musitu G, Veiga F (2006) Autoconcepto en adultos de España y Portugal. Psicothema 18: 551-556.
- Rigon J, Burro R, Guariglia C, Maini M, Marin D, et al. (2017) Self-awareness rehabilitation after traumatic brain injury: a pilot study to compare two group therapies. Restor Neurol Neurosci 35: 115-127.
- Kreutzer JS, Rapport JH, Marwitz C (2009) Caregivers’ well-being after traumatic brain injury: a multicenter prospective investigation. Arch Phys Med Rehabil 90: 939-946.
- Derogatis LR (2000) Symptom Checklist-90-Revised in Handbook of psychiatric measures. American Psychiatric Association, pp: 81-84.
- Silvestro D, Mazzetti M, Melia C, Stagno MT, Carlesimo GA, et al. (2017) Educational action in the rehabilitation of severe acquired brain injuries: the role of self-awareness. Ann Ist Super Sanita 53: 82-85.
Citation: Corallo F, Di Cara M, Lo Buono V, De Salvo S, Cannistraci C, et al. (2019) Depression and Stress Management for Caregivers of Traumatic Brain Injury Patients. J Child Adolesc Behav 7: 383. DOI: 10.4172/2375-4494.1000383
Copyright: © 2019 Corallo F, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Open Access Journals
Article Tools
Article Usage
- Total views: 3322
- [From(publication date): 0-2019 - Apr 07, 2025]
- Breakdown by view type
- HTML page views: 2530
- PDF downloads: 792