Research Article Open Access
Depersonalization Disorder in Former Addicts (Prevalence of Depersonalization-Derealization Disorder in Former Addicts)
Carlos Sirvent1* and Laura Fernández21Fundación Instituto Spiral Madrid, Spain
2Department of Differential Psychology, University of Oviedo, Spain
- Corresponding Author:
- Carlos Sirvent
Psychiatrist, Fundación Instituto Spiral Madrid, Spain
Tel: 985 111 111
Fax: 985 116 163
E-mail: csr@fispiral.com
Received date: March 27, 2015; Accepted date: May 04, 2015; Published date: May 11, 2015
Citation: Sirvent C, Fernández L (2015) Depersonalization Disorder in Former Addicts (Prevalence of Depersonalization-Derealization Disorder in Former Addicts). J Addict Res Ther 6:225. doi:10.4172/2155-6105.1000225
Copyright: © 2015 Sirvent C, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Addiction Research & Therapy
Abstract
Many former addicts who have not been taking drugs for a while suffer from the so-called depersonalizationderealization disorder (DPD-DR) –a peculiar sensation of unreality and strangeness towards the environment, something like “living in a permanent dream”. It is not an altered conscious state but a different conscience of the world which makes the individual become a virtual spectator of a life that sometimes looks real to them, and sometimes looks illusory. Nearly all studies on the depersonalization-addiction binomial refer to current drug addicts, but there are no studies on former addicts.
Objective: To find out the prevalence of depersonalization-derealization disorder in former addicts.
Method: 68 former addicts were compared with 59 individuals from the control group. CDS (Cambridge Depersonalization Scale) scale, version CDS-11, and DES (Dissociative Experiences Scale by Bernstein & Putnam) scale were applied.
Results: Nearly 25% of drug-free addicts (former addicts) suffer or have suffered from severe depersonalization disorder (DES scale). If we consider mild depersonalization disorder, the number rises up to 43.55% (DES scale) and 19.38% (CDS-11 scale). It should be noted that DPD-DR prevalence in the general population is 1.5%.
Conclusions: Depersonalization-derealization disorder is a surprise both for former addicts and their relatives, as well as for the clinical staff, who is usually unaware of this phenomenon and can mistake it for nostalgia towards the consumption environment. Who knows how many drug-free or former addicts have been victims of a mistake by their therapist? DPD-DR can be overcome through an adequate intervention in 3-6 months from onset. We think healthcare professionals should be well aware of this phenomenon.
Keywords
Prevalence; Depersonalization; Derealization; Addiction; Evaluation; Dishabituation; Rehabilitation; Former addiction
Introduction
Dissociative experiences are relatively common in the general population. They are equally distributed in women and men, and they tend to be less frequent with age [1,2]. According to WHO’s CIE-10 classification, the process falls within the family of neurosis as a secondary phenomenon to stressful situations and it groups the depersonalization-derealization disorder (DPD-DR) within a single category. However, American Psychiatric Association’s 2014 DSM-5 [3] classification is more explicit, reflecting that self-strangeness or selfestrangement is the essential characteristic of this disorder. Patients feel as external observers of their mental processes, their own body, or a part of it, as if they were oblivious, dead, or empty, as if automated or living in a dream or a movie [4]. Depersonalization disorder is usually described as a set of unreality and self-estrangement experiences, or as feeling as an external observer towards internal sensations and feelings or towards the own body and actions. Derealization refers to unreality or estrangement experiences towards the environment [5,6].
The DPD-DR phenomenon or estrangement due to the direct physiopathological effects of a substance differs from conventional depersonalization disorder in that such substance (for instance, drugs, medicines, or even addictive behavior) is considered as etiologically related to estrangement [7]. Depersonalization may appear as a syndrome in acute intoxication or in alcohol or other drug abstinence. Additionally, the use of drugs may intensify the symptoms of a preexistent depersonalization disorder.
Most studies on the depersonalization-addiction binomial refer to current drug users or to substances’ immediate effects. One of them [8] compared addicts (especially to cannabis and hallucinogens) with non addicts suffering from depersonalization. Both groups presented a similar course and deterioration with suicidal tendencies and limited treatment response. A similar study [9] compared patients with drug-induced depersonalization disorder and patients with simple depersonalization disorder. No significant clinical differences were found regarding the disorder.
DPD-DR disorder is not only present during the active drug use phase, but it also reappears when patients give it up. This phenomenon is applicable to drugs, psych medications, and other addictive behavior such as gambling [10,11]. According to some studies, former alcohol users present with higher levels of depersonalization [12] than other former addicts (cocaine). However, both groups present high DPD-DR levels depending on the number of years they have been using these substances. Dissociative experiences may be a chronic residual effect of substance abuse.
Prevalence
Epidemiologic studies of DPD-DR disorder were not conducted until relatively few years ago. Nearly all researches refer to underdiagnosis as an inherent factor. Depersonalization is considered as the third most common psychopathological experience after anxiety and depression [13]. Incidence and prevalence are difficult to determine owing to the lack of consensus and the difficulty to find a reliable measurement. Depersonalization is rarely diagnosed, and isolated episodes are frequent even in the normal population [14]. According to concurrent studies [11], depersonalization disorder has a prevalence of 2.5% in the population. In an epidemiologic study with 1,567 individuals conducted in Germany, prevalence was between 1 and 2%. Michal et al. [15] carried out a study with a sample of 1,287 individuals aged between 14 and 90 which found 1.9% prevalence within the range of clinical significance. In conclusion, DPD-DR prevalence in the general population is around 1.5%.
In a previous work [11], depersonalization-derealization disorder in former addicts or current addicts in dishabituation was defined by the following target symptoms:
• Existential void: dissatisfaction, disappointment, disillusionment, and emotional void.
• Identity crisis: existential questions about the own identity which may lead patients to identify themselves with their past and with the person they were, in clear opposition to the new self that fights to open up to a new and puzzling world.
• Memory and cognition disorders: subjective sensation of deterioration and loss of intellective capacities.
• Mood changes and affective lability: culpability is usual, as well as a reiterative feeling of surrender.
• Unrealism: feeling that this is an unreal world.
• Recalling sensations and feelings that are already overcome: memories are relived with unusual emotional strength, sometimes to the point of triggering recurrence.
Research objectives
The main objective of this research was to study the prevalence of depersonalization-derealization (DPD-DR) disorder in the former addict population versus the control group by checking data from selected assessment instruments. Given the characteristics of DPD-DR disorder, an intervention and prevention plan had to be established according to data.
Secondary objectives included the incidence of associated subsyndromes and their specific weight within the DPD-DR process. This includes existential void, amnesic and cognitive disorders, mood changes, identity crises, and pseudo-identification with consumption self. The last objective was to collect the elements provided by the structure of the evaluation scales used: dissociative amnesia, associative absorption, and depersonalization/derealization from DES scale.
Evaluation instruments
There are 3 types of instruments to measure depersonalization: 1) Filtering scales, such as the Dissociative Experiences Scale by Bernstein and Putnam (DES) [16] and A-DES for adolescents, and the Somatoform Dissociation Questionnaire by Ellert Nijenhuis (SDQ) [17]. 2) Diagnostic scales such as Cambridge Depersonalization Scale (CDS) [18], with a 28-item version and an 11-item one, and the Multidimensional Inventory of Dissociation (MID) [19]. 3) Structured interviews, such as Loewenstein’s Mental Status Examination for Dissociation [20], Colin Ross’ Dissociative Disorders Interview Schedule (DDIS), and Spectrum Structured Clinical Interview for derealization-depersonalization (SCI-DER). Two instruments were selected for this research: Cambridge Depersonalization Scale (CDS- 11) and Dissociative Experiences Scale (DES) by Bernstein and Putnam.
CDS-11 (Cambridge Depersonalization Scale) self-administered scale measures the frequency and duration of depersonalization symptoms in the last 6 months. Its items describe experiences affecting different sensory modalities. There is a 28-item version and also a reduced 11-item version, which has been used in this study.
DES (Dissociative Experiences Scale) scale is a 28-item selfadministered test that seems to have predictive validity regarding dissociative disorders. It has 3 subscales: amnesia experiences or blackouts in the continuity of conscience, depersonalization, derealization and absorption (“imaginative absorption” or “common dissociative symptoms”), and identity disorder. These factors or subscales describe the severity of symptoms for each of these domains in an approximate fashion but do not lead to unquestionable diagnoses. The dissociative amnesia factor involves a deficit in memories which prevents the individual from recovering the information stored. The associative absorption factor refers to the individual being immersed in internal events such as thinking and imagination and disconnected from the environment. The depersonalization/derealization factor involves persistent periods of self-estrangement and can be used as an instrument for depersonalization disorder screening as such.
Method
Participants
The study was carried out at Fundación Instituto Spiral’s addiction facilities in Madrid, Vañes, and Oviedo. Inclusion criteria in the patient group were: being over 16, being diagnosed with addiction (drug use disorder or addictive behavior), having undergone dishabituation treatment and having remained abstinent for at least 6 months since discharge, and having sufficient intellectual ability to respond to evaluation instruments.
From a total of 724 individuals discharged in the last 3 years and meeting the aforementioned conditions, 68 former addicts who had not taken drugs for 6 months up to 3 years were randomly selected (mean was 9 months) and compared with 59 individuals from the control group (non addicts) randomly selected from the general population and belonging to diversified social statuses similar to the patient group’s. Table 1 describes some sociodemographic variables of the population studied (Table 1).
| Sociodemographic characteristics of the sample | |||||
|---|---|---|---|---|---|
| Study group | Total | Sex Valid | Age | ||
| N= | Male | Female | Age range | Mean | |
| Non addicted | 59 | 33 | 26 | 17-70 | 41.27 |
| Addicted | 68 | 24 | 44 | 19-70 | 40.86 |
Table 1: Sociodemographic characteristics of the sample.
In the non addicts sample, according to gender classification, 44.06% of individuals were female and 55.94% male, they were aged between 17 and 70 (mean=41.27, SD=11.137), mostly single (66.4%, n=38), had completed college education (20.3%, n=12 with intermediate level college education, and 18.6%, n=11 with upper level college education), were of medium socioeconomic level (81.35%, n=48), and came from households with three members or less (72.9%, n=43).
In the former addicts sample, according to gender classification, 64.7% of individuals were female and 35.23% male, they were aged between 19 and 70 (mean=40.86, SD=12.142), mostly single (69.1%, n=47), worked as unskilled workers (36.76%) and skilled workers (32.3%, n=22), and had a medium perceived socioeconomic level (66.17%, n=45). As the main sociodemographic data of interest, 25% (n=17) of addicts in the sample had had three or more partners, and 36.7% (n=25) of them had completed primary education.
Investigated variables
CDS (Cambridge Depersonalization Scale) scale, version CDS-11, and DES (Dissociative Experiences Scale by Bernstein & Putnam) scale were used.
Regarding the CSD-11 Scale, scores equal to or greater than 22.5 are considered positive, being severe those that exceed 30 points.
Regarding the DES Scale, scores equal to or above 30 are considered positive and severe those exceeding 40 (applicable both to the general scale and factors). Table 2 shows the distribution of the sample according to the instruments applied (Table 2).
| Instruments applied and distribution of sample | |||
|---|---|---|---|
| Study group | Total | Valids | |
| N= 127 | CDS-11 | DES | |
| Non addicted | 59 | 59 | 59 |
| Addicted | 68 | 68 | 62 |
Table 2: Instruments applied and distribution of sample.
Data analysis
Data were analyzed using the SPSS statistical package, version 21.
CDS-11 Scale: CDS scale’s (version 11) reliability, estimated through Cronbach’s α coefficient, was 0.85. In order to study the differences between addicts group (former addicts ) and controls (non addicts), Student’s t test was applied to independent samples. Results showed statistically significant differences between both groups, as demonstrated in (Table 3).
| Addicted-Non addicted difference study | ||||
|---|---|---|---|---|
| Study group | t | gl | Bilateral | Effect Size |
| Addicted-Non addicted | -5.636 | 92.455 | 0.000 | 0.86 |
Table 3: Addicted-Non addicted difference study.
DES Scale: Correlations between imaginative absorption, amnesia, and depersonalization/derealization factors were analyzed (Table 4), demonstrating high correlations between dimensions and their scales, suggestive of high factor discrimination. The scale’s and its three factors’ reliability, estimated through Cronbach’s α coefficient, was high: 0.939 (total), 0.792 (absorption), 0.822 (amnesia), and 0.881 (depersonalization). In order to study the differences between and controls for each factor, Student’s t test was applied to independent samples. Results showed statistically significant differences, as demonstrated in (Table 5).
| Correlations between DES factors | ||||
|---|---|---|---|---|
| Factor | Score | Absorption | Amnesia | Depersonalization |
| Absorption | Pearson correlation | 0.788* | 0.837* | |
| Sig. (bilateral) | 0.000 | |||
| Amnesia | Pearson correlation | 0.788* | 0.834 | |
| Sig. (bilateral) | ||||
| Depersonalization | Pearson correlation | 0.837* | 0.834* | |
| Sig. (bilateral) | ||||
| *Correlation is significant at 0.01 level (bilateral) | ||||
Table 4: Correlations between DES factors.
| Addicted-Non addicted difference study | |||||
|---|---|---|---|---|---|
| Factor | Study Group | T | Gl | Sig. (bilateral) | Size Effect |
| Absorption | Addicted- Non addicted | -5,855 | 93,832 | 0,000 | 0,89 |
| Amnesia | Addicted – Non addicted | -5,959 | 116,927 | 0,000 | 0,91 |
| Depersonalization | Addicted – Non addicted | -5,858 | 87,180 | 0,000 | 0,88 |
Table 5: Addicted-Non addicted difference study.
Results
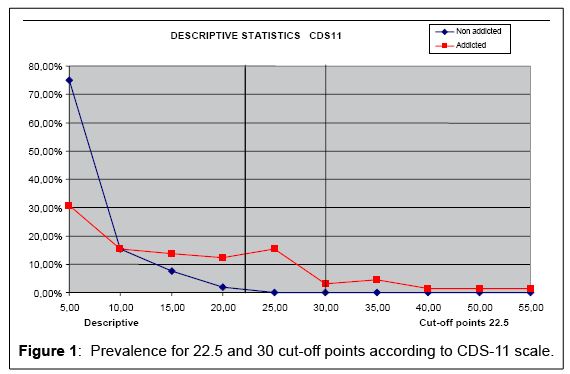
• CDS-11 Scale: For a 22.5 cut-off point, the prevalence of depersonalization in this scale was 0.00% for the non addicts group and 19.35% for the addicts group (former addicts). If we raise the cut-off point up to 30, we will see that severe depersonalization reaches 12% in the addicts group (Tables 6, 7 and Figure 1).
| Prevalence of depersonalization using CDS-11 for 22.5 and 30 cut-off points | |||
| Study Group | N | PC >22,5 | PC >30 |
| Non addicted | 59 | 0,00% | 0,00% |
| Addicted | 68 | 19,35% | 12,31% |
Table 6: Prevalence of depersonalization using CDS-11 for 22.5 and 30 cut-off points.
| Cumulative percentages according to score | ||
|---|---|---|
| Score | Non addicted | Addicted |
| 5,00 | 75,00% | 30,77% |
| 10,00 | 15,38% | 15,38% |
| 15,00 | 7,69% | 13,85% |
| 20,00 | 1,92% | 12,31% |
| 25,00 | 0,00% | 15,38% |
| 30,00 | 0,00% | 3,08% |
| 35,00 | 0,00% | 4,62% |
| 40,00 | 0,00% | 1,54% |
| 50,00 | 0,00% | 1,54% |
| 55,00 | 0,00% | 1,54% |
Table 7: Cumulative percentages according to score.
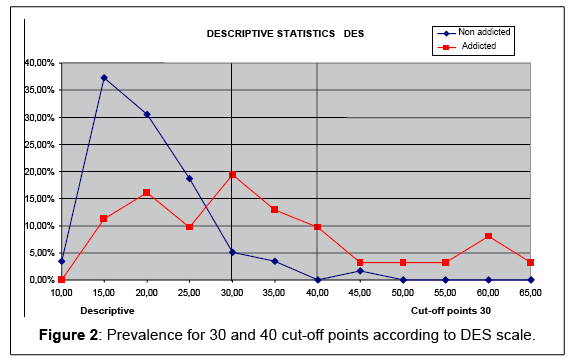
• 2) DES Scale: The prevalence of depersonalization according to this scale was 5.08% for the control group (non addicts) and 43.55% for the addicts group. If we raise the cut-off point up to 40, we will see that severe depersonalization reaches 1.69% in the control group (non addicts) and 20.97% in the addicts group (Table 8 and Figure 2). These scores seem more accurate to us.
| Prevalence of depersonalization using DES scale | |||
|---|---|---|---|
| Study Group | N | Cut-off >30 | Cut-off >40 |
| Non addicted. | 59 | 5,08% | 1,69% |
| Addicted | 62 | 43,55% | 20,97% |
Table 8: Prevalence of depersonalization using DES scale.
• According to the factors provided by DES scale, absorption factor is lower than the cut-off point, whereas depersonalization factor is slightly higher. However, the amnesia factor is clearly higher (Table 9).
| SStudy of means by factors | |||
|---|---|---|---|
| Study Group | Absorption (>30) | Amnesia (>30) | Depersonalization (>30) |
| Non addicted | 15,9 | 23,12 | 16,35 |
| Addicted | 26,87 | 37,49 | 31,08 |
Table 9: Study of means by factors.
Conclusions and Discussion
The prevalence of DPD in former addicts was higher than 20% in both scales. More specifically, DES scale showed a prevalence of 43.55%, whereas CDS-11 scale reduced it down to 19.38%. When raising the cut-off points, we see that the prevalence of severe depersonalization is 12.31% for CDS-11 scale and 20.97% for DES scale.
These scores seem more accurate to us. If we compare these data with Michal et al. [21]’s prevalence studies with broad general population samples, which estimated prevalence at 1.9% in the general population within the range of clinical significance, such percentage would correspond to 23.4% of the addict population if we follow proportionality. Consequently, it would be reasonable to state that nearly 25% of former addicts present with a remarkable level of depersonalization. A study by Simeon, D., Hwu, R., & Knutelska, M. [22] from 2007 with a similar sample (52 patients and 30 controls) concluded that temporal disintegration in depersonalized individuals is not directly attached to the main depersonalizationderealization symptoms, but it does exist when depersonalized experience involves a more prominent absorption. In our case, amnesia is the factor that best discriminates the DPD condition of the addict individual.
The number invites reflection: 25% of former addicts suffer from depersonalization-derealization disorder, a pathology ignored by most of the general population and little known amongst professionals, as confirmed by both experts and DSM classification itself. The worst thing is that such ignorance usually leads to mistaking it for therapeutic involution or nostalgia towards consumption life, that is, for a prerelapse, although it is actually an existential identity crisis related to the adaptation to the new environment. Former addicts suffering from this problem do not actually know whether their referent is this new world they are discovering or the former one, related to consumption life.
This is a surprise both for former addicts and their relatives, as well as for the clinical staff, who is usually unaware of this phenomenon and mistakes it for nostalgia towards the consumption environment. Who knows how many drug-free or former addicts have been victims of a mistake by their therapist? DPD-DR can be overcome through an adequate intervention in 3-6 months from onset.
Regarding treatment, we should make clear that depersonalizationderealization is a dissociative disorder rather than a psychosis, since the dissociative experience does not lead to disconnection with reality. In other words, the former addict feels strange but maintains a perfect sense of reality. We do not recommend psychopharmacologic treatment unless symptoms are severe or stem from another cause. Antipsychotic drugs may induce the disorder rather than neutralize it.
The most prudent attitude to be adopted is watchful waiting and accompanying. Active intervention should be carried out over cardinal symptoms if they are severe, for instance, using cognitive behavioral techniques if affective emotional alterations or strangeness experiences make the patient suffer too much.
In conclusion, nearly 25% of drug-free addicts (former addicts) suffer or have suffered from severe depersonalization disorder to a remarkable extent. If we consider milder symptoms, the number rises up to 40% of depersonalizing experiences in this important and delicate population. We think healthcare professionals should be well aware of depersonalization-derealization disorder as it is a frequent pathology in addicts in dishabituation and drug-free addicts.
References
- Baker D, Earle M, Medford N, Sierra M, Towell A, et al. (2007) Illnessperceptions in depersonalizationdisorder: Testinganillnessattributionmodel. ClinPsycholPsychother 14:105-116.
- Moyano O, Thiébaut E, Claudon P (2004) Comparaison des expériencesdissociatives à l'adolescence entre un groupe de collégiens et un groupeclinique. Ann MedPsychol (Paris) 162:533-540.
- American PsychiatricAssociation (2014) Diagnostic and Statistical Manual of Mental Disorders (5th Edn) American PsychiatricAssociation, Arlington, VA, UnitedStates. 291-308.
- Lemche E, Surguladze SA, Brammer MJ, Phillips ML, Sierra M, et al. (2012) Multipleclinicaltraitspredictclinical diagnosis of depersonalizationdisorder: Implicationsfor DSM-V. BiolPsychiatry 72(1):e1-e2.
- Bauer SF (2009) Review of feelingunreal: Depersonalizationdisorder and theloss of theself. Am J Psychiatry 166:1070.
- González Calvo JM, Rejón Altable C (2002) [Estrangement in psychopathology: depersonalization, derealization, disorders of theself?]. Actas EspPsiquiatr 30: 382-391.
- Nuller YL1, Morozova MG, Kushnir ON, Hamper N (2001) Effect of naloxonetherapyondepersonalization: a pilotstudy. J Psychopharmacol 15: 93-95.
- Simeon D, Kozin DS, Segal K, Lerch B (2009) Isdepersonalizationdisorderinitiatedbyillicitdrug use anydifferent? A survey of 394 adults. J ClinPsychiatry 70:1358-1364.
- Medford N, Baker D, Hunter E (2003) Chronicdepersonalizationfollowingillicitdrug use: A controlledanalysis of 40 cases. Addiction 98:1731-1736.
- Keshaven MS, Lishman WA (1986) Prolongeddepersonalizationfollowing cannabis abuse. Br J Addict 81: 140-142.
- Sirvent C (2015) Adicción y perpetuación del sentido de irrealidad en adicciones. In: Adicciones: Conocimiento, atención integrada y acción preventiva: XXVI Congreso de Salud Mental de la Asociación Española de Neuropsiquiatría. Madrid: Asociación Española de Neuropsiquiatría 179-208.
- Wenzel K, Bernstein DP, Handelsman L, Rinaldi P, Ruggiero J, et al. (1996) Levels of dissociation in detoxifiedsubstanceabusers and theirrelationshiptochronicity of alcohol and drug use. J NervMentDis 184: 220-227.
- Levy JS, Wachtel PL (1978) Depersonalization: aneffort at clarification. Am J Psychoanal 38: 291-300.
- luby Ed, Cohen Bd, Rosenbaum G, GottliebJs, Kelley R (1959) Studyof a new schizophrenomimeticdrug; sernyl. AMA ArchNeurolPsychiatry 81: 363-369.
- Michal M, Beutel ME, Grobe TG (2010) Wieoftwird die depersonalisations-derealisationsstörung (ICD-10: F48.1) in der ambulantenversorgungdiagnostiziert? Z PsychosomMedPsychother 56:74-83.
- Bernstein EM, Putnam FW (1986) Development, reliability, and validity of a dissociationscale. J NervMentDis 174: 727-735.
- Ellert RS (2006)Nijenhuis: SomatoformeDissoziation (Original titel: SomatoformDissociation“) JunfermannVerlag. ISBN 978-3-87387-623-1.
- Sierra M, Berrios GE (2000) The Cambridge DepersonalizationScale: a new instrumentforthemeasurement of depersonalization. Psychiatry Res 93: 153-164.
- Dell PF (2002) Dissociativephenomenology of dissociativeidentitydisorder. J NervMentDis 190: 10-15.
- Loewenstein RJ (1991) An office mental status examinationforcomplexchronicdissociativesymptoms and multiplepersonalitydisorder. PsychiatrClin North Am 14: 567-604.
- Michal M, Wiltink J, Subic-Wrana C, Zwerenz R, Tuin I et al. (2009) Prevalence, correlates, and predictors of depersonalizationexperiences in thegerman general population. J NervMentDis 197:499-506.
- Simeon D , Hwu R, Knutelska M (2007) Temporal disintegration in depersonalizationdisorder. J Trauma Dissociation 8: 11-24.
Relevant Topics
- Addiction Recovery
- Alcohol Addiction Treatment
- Alcohol Rehabilitation
- Amphetamine Addiction
- Amphetamine-Related Disorders
- Cocaine Addiction
- Cocaine-Related Disorders
- Computer Addiction Research
- Drug Addiction Treatment
- Drug Rehabilitation
- Facts About Alcoholism
- Food Addiction Research
- Heroin Addiction Treatment
- Holistic Addiction Treatment
- Hospital-Addiction Syndrome
- Morphine Addiction
- Munchausen Syndrome
- Neonatal Abstinence Syndrome
- Nutritional Suitability
- Opioid-Related Disorders
- Relapse prevention
- Substance-Related Disorders
Recommended Journals
Article Tools
Article Usage
- Total views: 21762
- [From(publication date):
June-2015 - Nov 21, 2024] - Breakdown by view type
- HTML page views : 17247
- PDF downloads : 4515