Dentigerous Cyst or Ameloblastoma in Paediatric Patient: A Diagnostic Dilemma? - A Rare Case Report
Received: 03-Mar-2016 / Accepted Date: 04-Apr-2016 / Published Date: 11-Apr-2016 DOI: 10.4172/2161-119X.1000227
Abstract
Most of the times paediatric patients report to the clinics with a chief complaint of decayed teeth, associated with pain and sometimes swellings, which regress after proper treatment. But dentist should be aware of unusual and rare pathologic conditions in children. These conditions sometimes are associated with hidden aggressive nature. These unusual and rare kinds of clinical conditions should also be included in differential diagnosis. Present case shows inadvertent finding of Unicystic Ameloblastoma (UA) in paediatric patient, which was asymptomatic and aggressive in nature. This case report shows diagnosis and surgical management of such type of lesions in paediatric patients.
Keywords: Paediatric patient, Unicystic ameloblastoma, Dentigerous cyst
251585Introduction
Too often, dental practitioners see their responsibility to the patient begin and end with the care and maintenance of the teeth and periodontium. It is also easy to focus strictly on the dental needs of the patient regarding chief complaint and remain oblivious to other things. Subtle or even not so subtle lumps, bumps, swellings or changes in texture or colour of oral mucosa may signify the presence of a reactive or a hamartomatous overgrowth of tissue or a benign or malignant disease. Common intra-oral swellings of jaws which generally are diagnosed in paediatric patients are odontomes, cysts like dentigerous cyst, radicular cyst, eruption cyst odontogenic keratocyst, juvenile ossifying fibroma, ameloblastoma and cysts or swellings of nonodontogenic origin. Some of these swellings have potential to turn up in some severe kind of pathology but these kind of changes are rare. Ameloblastomas are benign tumours which grow slowly but have the potential to enlarge to enormous size even causing deformity of bone [1]. Although, it is one of the most common benign odontogenic tumour, it is considered to be rarity in pediatric age group [2,3].
Here, we report a distinctive case of intra-oral swelling with undefined extra-oral swelling, and which was initially diagnosed as dentigerous cyst.
Case Report
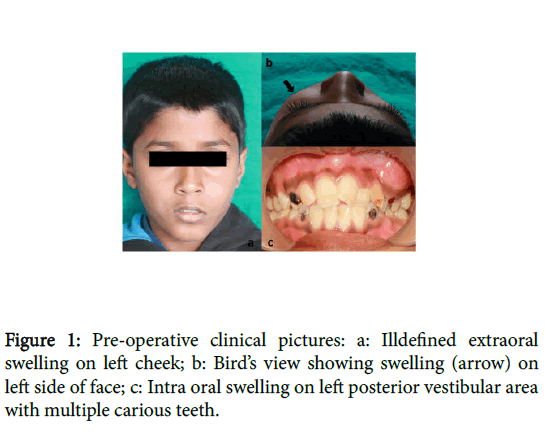
A 10 yr old male patient reported to dept. of pedodontics and preventive dentistry with the chief complain of pain in lower right back tooth region. Past medical history and past dental history was unremarkable. Family history was not significant. Intra-oral examination revealed multiple carious teeth including 53, 54, 55, 63, 64, 65, 73, 74, 75, 83, 84 and 85 and over retained maxillary primary left lateral incisor 62. On extra-oral examination, a slight ill-defined swelling was present on left side below the left eye (Figure 1a). Bird’s eye view (Figure 1b) revealed a remarkable swelling on left side. Intraoral examination revealed an ill-defined swelling on buccal vestibule in maxillary left posterior region (Figure 1c) which was felt hard on palpation, extending from distal to maxillary left primary canine (63) to mesial of maxillary left permanent first molar (26). The swelling was ill defined, firm on palpation, non-tender, extending into left maxillary vestibule. The overlying mucosa was apparently normal with no signs of inflammation or pus discharge. It was not compressible and no pulsation were felt.
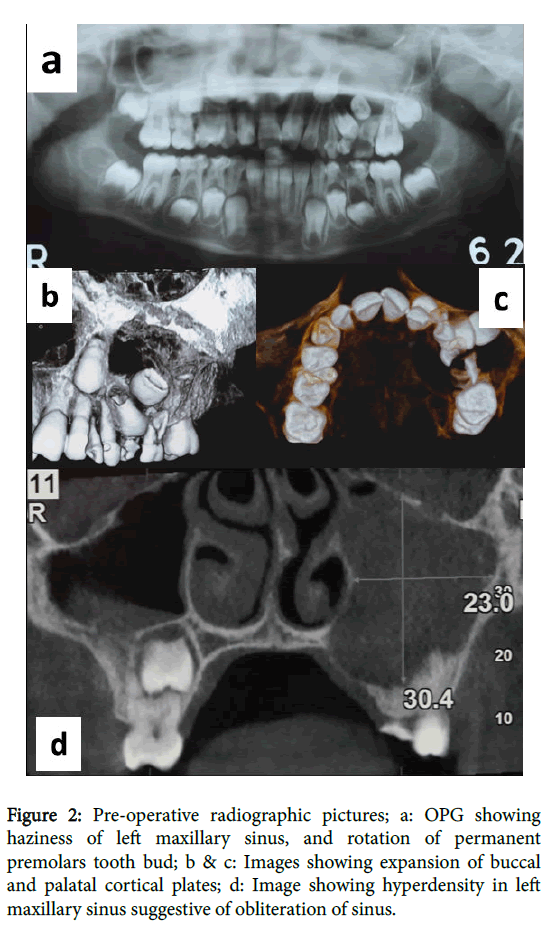
Orthopantamogram (Figure 2a) of the patient revealed radiolucency in relation to the maxillary left primary first and second molar. Computed tomography (Figure 2b) of the patient showed a welldefined radiolucency involving 64, 65 and permanent tooth bud of 24, 25. Occlusal view in 3D CBCT (Figure 2c) showed expansion of buccal and palatal cortical plates of involved area. Based on clinical and radiological findings, a provisional diagnosis of dentigerous cyst was made.
Figure 2: Pre-operative radiographic pictures; a: OPG showing haziness of left maxillary sinus, and rotation of permanent premolars tooth bud; b & c: Images showing expansion of buccal and palatal cortical plates; d: Image showing hyperdensity in left maxillary sinus suggestive of obliteration of sinus.
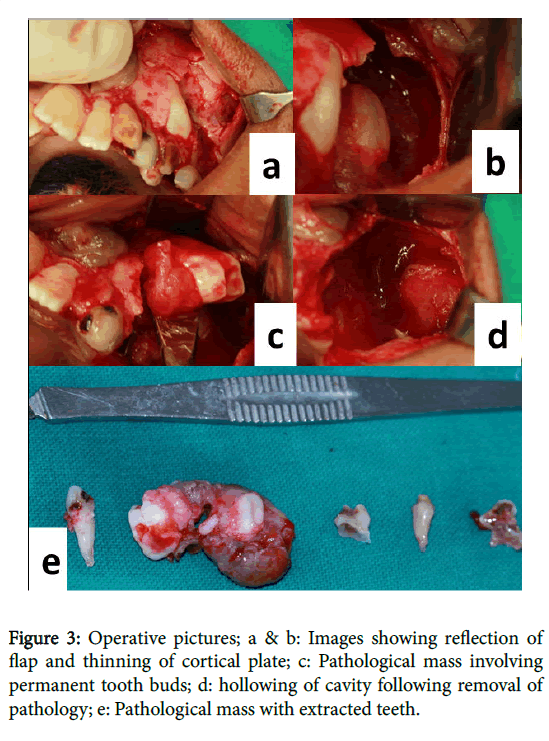
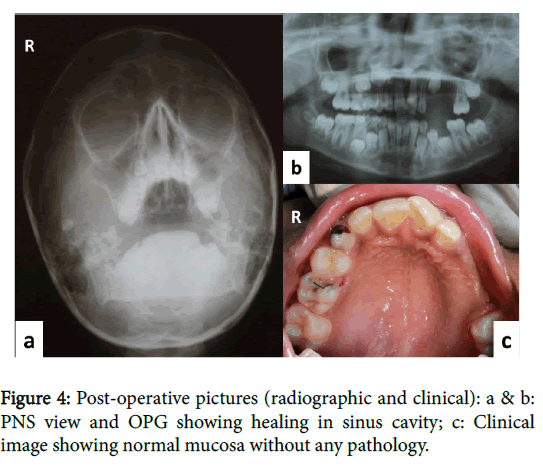
Under general anesthesia, the surgical area was exposed buccally. Crevicular incision was given from maxillary left permanent central incisor 21 to maxillary left permanent first molar 26 with releasing incision and flap was reflected (Figure 3a). Reflection of flap revealed thinning of buccal cortical plate (Figure 3b) which was removed. After which pathological mass (Figure 3c) was clearly visible with permanent tooth bud. Curettage of cystic lining was done and complete cyst was removed in toto (Figure 3d) along with tooth bud of maxillary left permanent first and second premolar i.e., 24, 25. Extractions of 62, 63, 64, and 65 were also done (Figure 3e). Flap was approximated and sutures were given. Betadiene impregnated gauge was placed inside the hollow cavity. Patient was recalled after 6 days for removal of gauge and cavity was left for secondary healing. Tissue specimen was sent for histopathological examination. Patient was recalled for follow up after every 7 days upto a month. 6 months postoperative follow-up PNS view and OPG showed no evidence of recurrence, clinical picture showed healing of involved area (Figures 4a-4c).
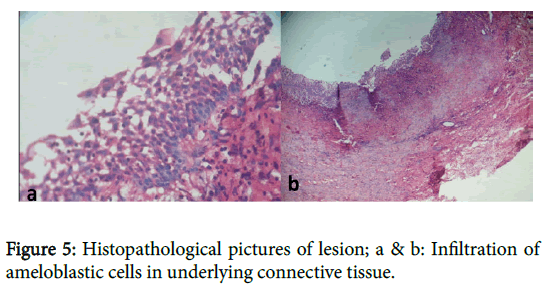
Histopathologial report confirmed the diagnosis of intraluminal unicystic ameloblastoma. Multiple histological sections were prepared from the soft tissue specimen. Unicystic ameloblastoma showing typical luminal lining of ameloblast like cells and Intral luminal proliferation of ameloblastic cells were evident in histopathological slides (Figure 5a and 5b).
Discussion
Ameloblastoma, with rare exceptions, is a benign and slow growing but relentlessly infiltrative tumour composed of odontogenic epithelium with mature, fibrous stroma without odontogenic ectomesenchyme [4]. The tumour is considered a rarity in paediatric patients, accounting for approximately 10–15% of all reported cases of ameloblastoma [5,6]. It represents 13–54% of all jaw tumours affecting all age groups, with a peak incidence in the third and fourth decade of life [7]. Bansal et al. [3] stated that the occurrence of ameloblastoma was 15.2% (39/256) in patients aged under 18 yrs, similar to Olaitan and Adekeye (14.6%) [8]. The mandible was the most common site of occurrence in all races; 225 (96.6%) tumors were encountered in the mandible and 8 (3.4%) in the maxilla, with an overall mandible:maxilla ratio of 28.1:1 [2].
World Health Organization (WHO), classified ameloblastomas into four groups: (1) solid/multicystic, (2) extraosseous/peripheral, (3) desmoplastic, and (4) unicystic. Robinson & Martinez (1977) first described Unicystic ameloblastoma (UA), usually presenting as unilocular lesion radiographically and appearing cystic in nature microscopically [9]. This special type of ameloblastoma is common in younger age group and respond to conservative treatment [10]. The term unicystic refers to macro and microscopic features of a welldefined monocystic lesion showing cavity with linning that consist of complete or focal areas of odontogenic epithelium [11].
In the present case, the pathology was provisionally diagnosed as dentigerous cyst because multiple deep carious teeth were present on the affected site, which might result in inflammation at the apex of deciduous tooth leading to the development of inflammatory follicular cyst in which premolars are commonly involved. Characteristically, Dentigerous cyst is attached to the neck of unerupted teeth, enveloping its crown. It is important that the definition of dentigerous cyst is applied strictly and that the diagnosis of dentigerous cyst is not made uncritically on radiographic evidence alone [12]. So, the differential diagnosis of OKC was made. OKC sometime remains undiagnosed because it tends to expand in medullary cavity. Occurrence of large OKCs involving maxillary sinus, that led to displacement and distruction of floor of orbit and proptosis of eye have also been mentioned in literature [12]. Radiographically OKC is well demarcated with distinct sclerotic margin and it might be expecting slow growing margins. Clinically it may occur in vital standing tooth giving appearance of radicular cyst. That may imapde the eruption of related teeth, resulting in a dentigerous appearance radiologically and may give rise to misconception [12].
The belief that UA arises either from pre-existing odontogenic cyst like dentigerous cyst or airsing de novo has been debatable. While Robinson and Martinez stated that the possibility of neoplastic transformation of non-neoplastic ameloblastoma though less frequent. The reason being the epithelium of odnotgenic cyst and ameloblastoma are showing common origin [11]. The fact that among all cysts, dentigerous cyst is common in pediatric patients. The occurrence of UA can be supported by this theory.
Prepathogenic mechanisms were proposed by Leider et al for evolution of UA. 1) ameloblastic transformation of reduced enamel epithelium in association with developing tooth, along with subsequent cystic development. 2) Development from neoplastic transition of non-neoplastic ameloblastic epithelium of dentigerous or other odontogenic cysts. 3) Cystic degeneration of ameloblastic islands in a solid ameloblastoma followed by fusion of multiple microcysts resulting in a unicystic lesion [13].
The treatment of ameloblastoma is controversial. In children, the treatment is complicated by three factors: 1) continuing facial growth, different bone physiology (greater percentage of cancellous bone, increased bone turnover and reactive periostium) and presence of unerupted teeth; 2) difficulty in initial diagnosis; and 3) predominance of the unicystic type of ameloblastoma [2].
Unicystic ameloblastoma is radiologically characterized by a unilocular aspect and it is less aggressive than the solid type, but has the potential for recurrence [2] But in the present case, the pathology had involved the left maxillary sinus which is evident in radiograph. And there is greater rotation of permanent tooth bud than that found with a dentigerous cyst.
The treatment of ameloblastoma varies according to type of lesion, from a conservative approach to radical resection. The rate of recurrence following radical treatment is lower than that following conservative treatment. Radical resection of an ameloblastoma in children should be avoided. Such treatment could result in deformity and dysfunction of the face, which is bound to influence both the physical and psychological development of the child later in life [14]. So all the points should be kept in mind while choosing the treatment option, and should end up with functional and aesthetic rehabilitation.
Conclusion
This case report showed how an unsuspected carious lesion led to a cystic lesion which further transformed into a rare, benign tumour i.e., an intraluminal unicystic ameloblastoma. The lesion attained a considerable size without the patient’s/ Guardian’s awareness. Such cases test the clinicians knowledge and treatment protocol options once the diagnosis is confirmed. The need of the hour for the clinician is to take into consideration, the age of the patient and also the rehabilitative or corrective procedures to establish proper functional and aesthetic restoration of occlusion. Thus, an early diagnosis and appropriate treatment strategy can prevent/decrease the morbidity associated with the same.
References
- Reddy SK, Rao GS (2011) Unicysticameloblastoma in 6 year old child and its significance. Worl J Dent 2: 363-366.
- Zhang J, Gu Z, Jiang L, Zhao J, Tian M, et al. (2010) Ameloblastoma in children and adolescents. Br J Oral MaxillofacSurg 48: 549-554.
- Bansal S, Desai RS, Shirsat P, Prasad P, Karjodkar F, et al. (2015) The occurrence and pattern of ameloblastoma in children and adolescents: an Indian institutional study of 41 years and review of the literature. Int J Oral MaxillofacSurg 44: 725-731.
- Barnes L, Eveson JW, Reichart P, Sidransky D (2005) Pathology and genetics of head and neck tumors. Lyon: IARC Presspp:1-435.
- Keszler A, Dominguez FV (1986) Ameloblastoma in childhood. J Oral MaxillofacSurg 44: 609-613.
- Ueno S, Nakamura S, Mushimoto K, Shirasu R (1986) A clinicopathologic study of ameloblastoma. J Oral MaxillofacSurg 44: 361-365.
- Reichart PA, Philipsen HP, Sonner S (1995) Ameloblastoma: biological profile of 3677 cases. Eur J Cancer B Oral Oncol 31B: 86-99.
- Olaitan AA, Adekeye EO (1996) Clinical features and management of ameloblastoma of the mandible in children and adolescents. Br J Oral MaxillofacSurg 34: 248-251.
- Robinson L, Martinez MG (1977) Unicysticameloblastoma: a prognostically distinct entity. Cancer 40: 2278-2285.
- Lau SL, Samman N (2006) Recurrence related to treatment modalities of unicysticameloblastoma: a systematic review. Int J Oral MaxillofacSurg 35: 681-690.
- Gabhane M, Kulkarni M, Mahajan A (2011) Unicysticameloblastoma of mandible: a case report. Indian J Stomatal 2: 273-276.
- Shear M, Speight PM (2008) In Dentigerous cyst: Cysts of the oral & maxillofacial regions(4th edn.). Blackwell munksgaard.
- Leider AS, Eversole LR, Barkin ME (1985) Cystic ameloblastoma. A clinicopathologic analysis. Oral Surg Oral Med Oral Pathol 60: 624-630.
- Scariot R, da Silva RV, da Silva FW Jr, da Costa DJ, Rebellato NL (2012) Conservative treatment of ameloblastoma in child: a case report. Stomatologija 14: 33-36.
Citation: Singh G, Banda NR, Patel A, Kandya A (2016) Dentigerous Cyst or Ameloblastoma in Paediatric Patient: A Diagnostic Dilemma? - A Rare Case Report. Otolaryngol (Sunnyvale) 6:227. DOI: 10.4172/2161-119X.1000227
Copyright: © 2016 Singh G, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 13053
- [From(publication date): 4-2016 - Apr 07, 2025]
- Breakdown by view type
- HTML page views: 12154
- PDF downloads: 899