Case Report Open Access
Delayed Presentation of Short Bowel Syndrome Complicated with Severe Degree of Nutritional Deficiencies, Nephrocalcinosis and Distal Renal Tubular Acidosis
Tharuka Herath* and Aruna KulatungaNational Hospital, Colombo, Sri lanka
- *Corresponding Author:
- Tharuka Herath
National Hospital of Sri Lanka
Medicine no: 80, Mable Coore Mawatha
Primrose Garden, Kandy Central, 20000, Sri Lanka
Tel: 091775144886
E-mail: tharukaherath11@gmail.com
Receiving date: November 20, 2016; Accepted date: January 23, 2017; Published date: January 30, 2017
Citation: Herath T, Kulatunga A (2017) Delayed Presentation of Short Bowel Syndrome Complicated with Severe Degree of Nutritional Deficiencies, Nephrocalcinosis and Distal Renal Tubular Acidosis. J Gastrointest Dig Syst 7:484. doi: 10.4172/2161-069X.1000484
Copyright: © 2016 Herath T, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Gastrointestinal & Digestive System
Abstract
Background: Short bowel syndrome (SBS) is a malabsorptive state due to functional or anatomic loss of extensive segments of small intestine which can lead to nutritional deficiencies and metabolic disarrangements. Here we describe a young patient with short bowel presenting with severe nutritional deficiencies, nephrocalcinosis and distal renal tubular acidosis. Nephrocalcinosis and distal renal tubular acidosis are closely associated and each can lead to the other. There are only rare case reports of short bowel syndrome complicated with nephrocalcinosis and distal RTA and severe degree of metabolic derangement with nutritional deficiencies. And this case highlights the importance of early management of short bowel syndrome in order to prevent long-term complications. Case presentation: A forty two-year-old Sri Lankan male patient who had undergone appendectomy at the age of nineteen years, which was complicated by bowel gangrene and about 240 cm of small bowel was resected. Later he presented with recurrent urolithiasis and urinary tract infections and ten years after the surgery imaging revealed bilateral nephrocalcinosis and obstructive uropathy. Distal Renal tubular acidosis (RTA) was diagnosed at the same time. He also had osteomalacia, proximal myopathy, multiple vitamin deficiencies, mixed deficiency anemia. He was started on calcium, iron supplements, parenteral B12, vitamin D injections and alkali therapy to achieve a normal serum bicarbonate concentration. His calcium and Vitamin D supplementation is currently being monitored with serum calcium, 25-hydroxyvitamin D, serum alkaline phosphatase, serum PTH and urinary calcium/creatinine ratio. Conclusion: Patients with extensive small bowel resection are at risk for nutrient, mineral, and vitamin deficiencies because of the loss of absorptive surface. It can also be complicated with nephrocalcinosis and distal RTA which is rare in short bowel syndrome. It is therefore important to identify patients at risk of short bowel syndrome and institute an early management, follow up plan to prevent complications.
Keywords
Short bowel syndrome; Nephrocalcinosis; Nutritional deficiencies
Background
Short bowel syndrome (SBS) is a malabsorptive state due to functional or anatomic loss of extensive segments of small intestine which can cause nutritional deficiencies and metabolic disarrangements. Here we describe a patient with short bowel syndrome following resection of gangrenous bowel presenting with anemia, osteomalacia, recurrent urolithiasis, urinary tract infections and nephrocalcinosis due to hyperoxaluria. He also had distal renal tubular acidosis (RTA) which inturn caused by nephrocalcinosis and obstructive uropathy. Nephrocalcinosis and distal renal tubular acidosis are closely associated and each can lead to the other since nephrocalcinosis itself frequently causes defects in distal acidification. There are only very rare case reports of short bowel syndrome complicated with nephrocalcinosis and distal RTA with severe degree of nutritional deficiency.
Case Presentation
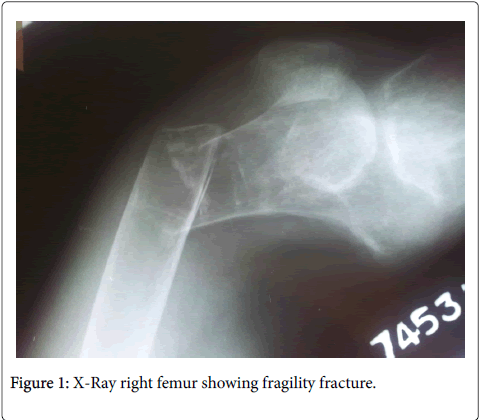
A forty two-year-old Sri Lankan male patient presented with dysuria, frequency and urgency with fever for one week with progressive proximal muscle weakness of fifteen years duration. At the age of nineteen years he had undergone appendectomy, which was complicated by bowel gangrene, and about 230 cm to 240 cm of small bowel was resected. After which he defaulted follow up because he was feeling well except for intermittent episodes of loose stools and fat intolerance with steatorrhoea. Five years later he presented with ureteric colic and was diagnosed to have a left ureteric calculus after which suffered from recurrent urolithiasis and urinary tract infections (UTI). He had undergone several urological procedures. Ten years later he was investigated and X-ray KUB and an ultrasound of KUB done at that time showed bilateral nephrocalcinosis with ureteric stones and obstructive uropathy. At the same time distal renal tubular acidosis (RTA) was diagnosed with plasma and urinary pH values and with a low plasma HCO3-. He also complained of progressive proximal muscle wasting and weakness with bone pain for the last fifteen years and had a fragility fracture of right femur (Figure 1). His growth was stunted and was also found to have a mixed deficiency anemia. He has not attended medical clinics regularly and so was not followed up properly till this admission.
On examination his height was 145 cm and weighted 45 kg with a BMI of 21.4. He was pale but did not have angular stomatitis, glossitis, bitot spots or gum bleeding. His cardiovascular, respiratory and abdominal examination was normal. Cranial nerve examination was also normal with normal fundoscopy. However he had both upper and lower limb proximal muscle wasting and weakness of grade 4 with preserved reflexes. His Heamoglobin was progressively decreasing with a rising MCV. Ten years after the surgery his Hb was 10.1 g/dl with a MCV of 89 fl and at this presentation (after 22 years later from the surgery), Hb was 6.8 g/dl with a MCV of 105 fl. White cell count and platelet count were normal throughout. Blood picture showed hypochromic microcytic RBC as well as normochromic normocytic RBC with oval macrocytes, pencil shaped cells and hyper-segmented neutrophils suggesting a mixed deficiency anemia which was confirmed bio chemically (Table 1). Liver functions were normal with a marginally low albumin and globulin (Table 2).
| Serum iron 51.9 μg/dl (59-156) | T.I.B.C. 249 (291-430) |
| Transferrin saturation 20.8% (20% -50%) | Ferritin 225 ng/ml (28-365 ). |
| Serum B12 111.5 pg/ml (223 -915) | Red cell folate 240ng/ml (252-813) |
Table 1: Mixed deficiency anemia, Serum iron studies, B12 levels and Folic acid levels.
| Albumin of 34 g/L (36-48) | Globulin of 14 g/L ( 22-40 ) |
| AST 18 U/L (10-35 ) | ALT 30 U/L ( 10-40 ) |
| Total bilirubin 13 μmol/L (5-21 ) | INR 1.4 |
| Amylase 70 U/L ( 22-80 ) |
Table 2: Liver function tests.
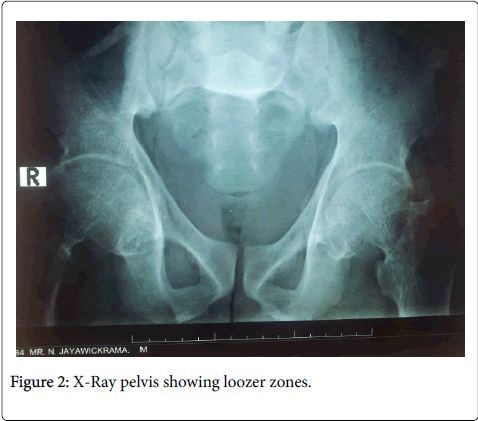
Serum creatinine was progressively rising with 84 μmol/l 10 years after the surgery and now, 22 years later, 257 μmol/l. Serum calcium and phosphate were normal with progressively rising serum Alkaline phosphatase and parathyroid hormone (PTH) (Table 3). Serum vitamin D (25 hydroxy) was low at 10.56 ng/ml (<20 deficient) X-ray pelvis revealed Looser zones (Figure 2).
| Time following surgery | 10 years | 14 years | 20 years | 22 years |
| Serum ionized Calcium (1.12 -1.32) | 1.20 | 1.0 | 1.2 | 1.14 |
| Serum Phosphate mg/dl (2.5-4.3) | 2.99 | 2.8 | 2.9 | 2.1 |
| Serum Alkaline phosphatase μmol/l (100-360) | 399 | 494 | 718 | 694 |
| Intact PTH (14-72) pg/ml | 92.6 | Not analyzed | Not analyzed | 349 |
Table 3: Serum ionized calcium, phosphate, alkaline phosphatase and intact PTH.
Serum potassium was low initially (3.3, 3.7 and 3.4 mmol/l) prior to starting potassium replacement and replaced to a level of 4.4 mmol/l. Other ions were within normal range with serum sodium 138 mmol/l and serum Chloride 110 mmol/l. Urine sodium was 62.2 mmol/l (14-144), urine potassium 14.4 mmol/l (13-62) and urine Chloride 58.0 mmol/l (55-125). Arterial pH showed acidosis with pH values of 7.3, 7.28, 7.32 with the urine pH persistently above 5.5 (6, 5.7, 5.8) Serum HCO3- was low (14.3, 8.6, 16.3 mmol/l). Lactic acid level was normal. These values were when the serum creatinine was within the normal range.
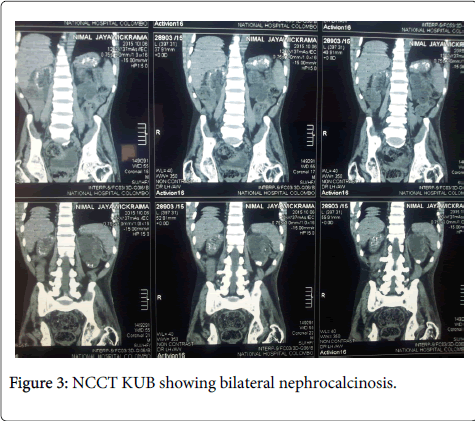
X ray KUB and CT IVU showed multiple areas of calcifications in the right kidney and lower pole calcification of the left kidney suggestive of nephrocalcinosis (Figure 3). Several ultrasound scans have been done during the past, which confirmed urolithiasis and obstructive uropathy. A recent scan showed a contracted right kidney (6 cm) with multiple renal cortical calcifications and a small left kidney (7.7 cm) with hydronephrosis and upper hydroureter with lower pole calcifications. Twenty-four hour urinary excretion of calcium was 68.08 mg (100-300) ten years after surgery with a phosphate excretion of 357.88 mg (500-1500).
On this admission urine calcium/creatinine ratio was 0.19 (0.04-0.45) Serum uric levels were elevated 9.4, 7.6, 8.0 mg/dl (3.5-7.2) at ten years, twenty years and twenty two years after surgery respectively. Urinalysis was negative for glucose but his 24-hour protein excretion was 175 mg. 24-hour urine oxalate, urine citrate and uric acid values were not done due to financial difficulties.
Renal stone analysis was positive for calcium, oxalate and cysteine and negative for uric acid, ammonia, magnesium, phosphate and carbonate.
ESR was normal. Sigmoidoscopy performed was normal and biopsy revealed nonspecific colitis only. ANA, Rheumatoid factor, C-ANCA and P-ANCA were negative. TSH 1.58 mIU/l (0.3-4.2) Fasting blood sugar and lipid profile were normal. HIV 1 and 2 and VDRL were negative.
Discussion
The short bowel syndrome (SBS) is a malabsorptive state of both macronutrients and micronutrients inadequate to maintain his or her nutrient and hydration status without intravenous or enteral supplementation that may follow massive resection of the small intestine [1] SBS in adults usually results from surgical resection of bowel for Crohn's disease, malignancy, radiation, vascular insufficiency and in infants and small children it can be due to necrotizing enterocolitis and congenital intestinal anomalies such as atresia or gastroschisis. Adult small intestine is approximately 480 cm and adults with residual small intestine of less than 180 cm are at risk for developing SBS and its complications and those who have less than 60 cm of small intestine (but with a colon) are more likely to be dependent on parental nutrition [2]. In our patient about 240 cm of the small bowel had been resected as a complication of appendicitis after which he was largely lost to follow up until he developed complications of SBS.
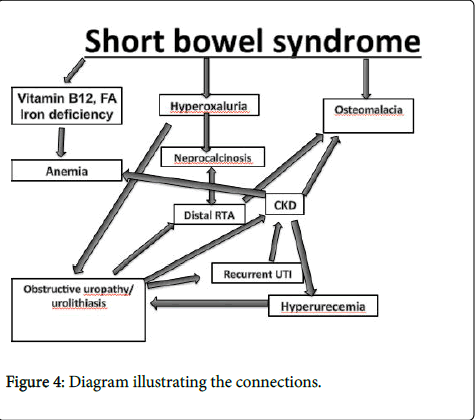
Chronic complications of short bowel syndrome include malabsorptive nutritional abnormalities including metabolic bone disease, mixed deficiency anemia, small bowel bacterial overgrowth, D-lactic acidosis, cholelithiasis, enteric hyperoxaluria and its complications and complications related to parenteral nutrition such as central line sepsis, catheter breakage and liver and biliary disease associated with parenteral nutrition [3]. Here, we discuss a patient with SBS who has mixed deficiency anemia, osteomalacia and bone disesase. He also had hyperoxaluria causing recurrent urolithiasis with obstructive uropathy and recurrent urinary tract infections leading to chronic kidney disease (CKD) with nephrocalcinosis and distal renal tubular acidosis (RTA). He has defaulted follow up so when he presented to us he had severe degree of metabolic complications of SBS which can be explained by using basic physiology and biochemistry.
Distal (type 1) RTA is characterized by an impaired capacity of hydrogen ion secretion in the collecting tubules manifested as an abnormally high urine pH (5.5 or higher) with systemic metabolic acidosis with a low plasma bicarbonate concentration, hyperchloremic normal anion gap [4] and hypokalemia which may be severe enough to produce muscle weakness [5]. Hypercalciuria occurs due to effects of chronic acidosis on both bone resorption and the renal tubular reabsorption of calcium. Hypocitraturia and hypercalciuria cause urolithiasis, nephrocalcinosis and recurrent urinary tract infections [6]. Our patient had a normal anion gap hyperchloremic metabolic acidosis with low plasma bicarbonate with values below 10 mmol/l with high urine pH (5.5 or higher) and hypokalemia which confirmed distal RTA. Other causes which can cause acidosis in these patients are D-lactic acidosis and chronic kidney disease (this will too be of a high anion gap and in our patient when the acidosis was detected he had a normal serum creatnine). Chronic diarrhoea, which can be a complication of SBS, can cause chronic normal anion gap metabolic acidosis, hypokalemia, and elevation of urine pH which mimic distal RTA. However, here the excretion of NH4, usually with Cl, increases the urine Cl concentration and cause negative urinary anion gap (UAG) with a range between -20 and -50 meq/L. In our patient urinary anion gap was {UAG (in meq/l or mmol/l) = Urine (Na+K- Cl)} 62.2+14.4-58.0 = +18.6 mmol/l. This positive UAG is consistent with low or normal NH4 excretion compatible with distal renal tubular acidosis. Our patient also did not have significant diarrhoea to cause acidosis. Since urinary tract infections with urea splitting organisms may increase the urine pH because urea is converted to ammonia and bicarbonate, these tests were done when urinary tract infection was not present. This therefore confirms distal RTA in our patient as the cause for metabolic acidosis. He initially was hypokalemic but later with development of chronic kidney disease and with potassium supplementation, potassium rose to normal levels.
In our patient we believe distal RTA to be due to nephrocalcinosis and obstructive uropathy. Nephrocalcinosis and distal renal tubular acidosis are closely associated and each can lead to the other since nephrocalcinosis itself frequently causes defects in distal acidification [7]. The reported prevalence of nephrocalcinosis in patients with distal RTA ranges from 60 to 80 percent. Another complication in patients with SBS is hyperoxaluria. This is due to fat malabsorption leading to binding of free calcium to fatty acids in the intestinal lumen making free oxalate available for absorption and increased colonic permeability to small molecules such as oxalate induced by exposure of the colon to nonabsorbed bile salts [8]. This leads to recurrent calcium oxalate stone formation and nephrocalcinosis. So we believe our patient develop nephrocalcinosis secondary to hyperoxalruia and later contributed by distal RTA. He had urolithiasis due to hyperoxaluria, hypercalciuria and hypocitrateuria [9] caused by distal RTA, and hyperuricemia caused by CKD. His urine stone analysis was positive for calcium, oxalate. Urolithiasis and hypocitraturia secondary to distal RTA led to recurrent urinary tract infections. In here we were unable to confirm hyperuricemia, hyperoxaluria and hypocitraturia by measuring twenty-four hour urinary studies due to financial difficulties.
Our patient had osteomalacia with bone pain, muscle pain, bone tenderness, a fragility fracture and proximal muscle weakness. In this case osteomalacia is due to impaired vitamin D absorption, impaired calcium absorption, CKD (reduced formation of 1,25- dihydroxyvitamin D, metabolic acidosis) and distal RTA (causing metabolic acidosis and hypercalciuria). Here the serum calcium was almost normal due to secondary hyperparathyrodism and metabolic acidosis causing bone resorption and release of calcium. But increased serum alkaline phosphatase (elevated in 95 to 100 percent), PTH (elevated in 100 percent) and low 25-hydroxyvitamin D <15 ng/ml (low in 100 percent) and looser zones in X-ray confirmed the diagnosis. Hypercalciuria is defined as urinary excretion in excess of 200 mg of calcium per 24 hours or Urinary calcium excretion greater than 4 mg/kg per 24 hours. In our patient 24 hour urinary calcium excretion was normal (68.08 mg of calcium per twenty four) because of osteomalacia leading to secondary hyper parathyroidism causing reduced urinary calcium (Parathyroid hormone acts at both cortical thick ascending limb of the loop of Henle and distal convoluted tubule in the distal tubule to stimulate calcium reabsorption) [10] balancing out with distal RTA causing increased calcium excretion [11]. We believe that he developed CKD due to recurrent urolithiaisis leading to obstructive uropathy and recurrent UTI.
If the SBS was suspected early and properly followed up the complications can be minimized. But our patient had malnutrition for long years leading to mixed deficieny anemia and severe osteomalacia even leading to fragility fractures. He had iron deficiency, Vitamin B12 and folic acid deficiency due to loss of absorptive surface area contributing to anemia. Patients with this much of severe complications due to SBS are rare these days because they are detected early and managed.
Our patient was started on calcium, iron supplements and parenteral B12 and Vitamin D injections and alkali therapy to achieve a relatively normal serum bicarbonate concentration. Repeated arterial blood gas (ABG) showed pH of 7.4 with serum bicarbonate of 24 mmol/l. His calcium and Vitamin D supplementation is monitored with serum calcium, 25-hydroxyvitamin D, serum alkaline phosphatase, serum PTH and urinary calcium/creatinine ratio. Measures were taken not to over replace since it will cause hypercalciuria which will worsen the urolithiasis.
Conclusion
Patients with extensive small bowel resection are at risk for nutrient, mineral, and vitamin deficiencies because of the loss of absorptive surface. It is also complicated with nephrocalcinosis and distal RTA which is rare in short bowel syndrome although the mechanism can be readily explained by biochemistry and physiology (Figure 4).
It is therefore important to identify patients at risk of short bowel syndrome and institute an early management follow up plan to prevent complications like nutritional deficiencies, metabolic derangements and bone disease, irreversible renal damage.
Consent to publish
Written informed consent was obtained from the patient for publication of this case report and any accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
Competing Interests
The authors declare that they have no competing interests.
Acknowledgement
This case report was supported by ward doctors in acquisition, analyzing and interpretation of data. We are thankful to the patient’s relatives for the support given in providing data.
References
- O'Keefe SJ, Buchman AL, Fishbein TM,Jeejeebhoy KN, Jeppesen PB, et al. (2006) Short bowel syndrome and intestinal failure: consensus definitions and overview. ClinGastroenterolHepatol4:6-10.
- Thompson JS, Rochling FA, Weseman RA, Mercer DF (2012) Current management of short bowel syndrome. SurgClin North Am 91: 493-510.
- Ekema G, Milianti S, Boroni G (2009) Total parenteral nutrition in patients with short bowel syndrome. Minerva Pediatr61:283-291.
- Rodríguez Soriano J (2002) Renal tubular acidosis: the clinical entity. J Am SocNephrol13:2160.-2170.
- Batlle D, Moorthi KM, Schlueter W, Kurtzman N (2006) Distal renal tubular acidosis and the potassium enigma. SeminNephrol26:471-478.
- Brenner RJ, Spring DB, Sebastian A,McSherry EM, Genant HK, et al. (1982) Incidence of radiographically evident bone disease, nephrocalcinosis, and nephrolithiasis in various types of renal tubular acidosis. N Engl J Med 307:217-221.
- Choi JS, Kim CS, Park JW, Bae EH, Ma SK, et al. (2011) Incomplete Distal Renal Tubular Acidosis with Nephrocalcinosis. Chonnam Med J 47: 170-172.
- Obialo CI, Clayman RV, Matts JP, Fitch LL, Buchwald H, et al (1991) Pathogenesis of nephrolithiasis post-partial ileal bypass surgery: case-control study. The POSCH Group. Kidney Int 39:1249-1254.
- Norman ME, Feldman NI, Cohn RM, Roth KS, McCurdy DK, et al. (1978)Urinary citrate excretion in the diagnosis of distal renal tubular acidosis. J Pediatr; 92:394-400.
- Gesek FA, Friedman PA (1979) On the mechanism of parathyroid hormone stimulation of calcium uptake by mouse distal convoluted tubule cells. J Clin Invest 90:749-758.
- Bleich HL, Moore MJ, Lemann J Jr, Adams ND, Gray RW (1979) Urinary calcium excretion in human beings. N Engl J Med 301:535-541.
Relevant Topics
- Constipation
- Digestive Enzymes
- Endoscopy
- Epigastric Pain
- Gall Bladder
- Gastric Cancer
- Gastrointestinal Bleeding
- Gastrointestinal Hormones
- Gastrointestinal Infections
- Gastrointestinal Inflammation
- Gastrointestinal Pathology
- Gastrointestinal Pharmacology
- Gastrointestinal Radiology
- Gastrointestinal Surgery
- Gastrointestinal Tuberculosis
- GIST Sarcoma
- Intestinal Blockage
- Pancreas
- Salivary Glands
- Stomach Bloating
- Stomach Cramps
- Stomach Disorders
- Stomach Ulcer
Recommended Journals
Article Tools
Article Usage
- Total views: 4779
- [From(publication date):
February-2017 - Jul 11, 2025] - Breakdown by view type
- HTML page views : 3860
- PDF downloads : 919