Research Article Open Access
Deep Vein Thrombosis: The Incidence Post-PICC Line Placement
Altawan A1*, Golchian D2, Iljas J1,2, Patel B1,2 and Bazzi M1,21Heart and Vascular Department, St. Mary Mercy Hospital, Livonia, Michigan, USA
2Beaumont Health System–Oakwood, Dearborn, Michigan, USA
- *Corresponding Author:
- Anita Altawan
Heart and Vascular Department, St. Mary Mercy Hospital
Livonia, Michigan, USA
Tel: 248-720-8973
E-mail: aaltawan@yahoo.com
Received date: June 11, 2017; Accepted date: June 16, 2017; Published date: June 23, 2017
Citation: Altawan A, Golchian D, Iljas J, Patel B, Bazzi M (2017) Deep Vein Thrombosis: The Incidence Post-PICC Line Placement. OMICS J Radiol 6:264. doi: 10.4172/2167-7964.1000264
Copyright: © 2017 Altawan A, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Radiology
Abstract
Background: Peripherally Inserted Central Catheters (PICC) are being increasingly used in the hospital setting. However, there are a number of complications associated with PICCs, particularly upper extremity deep and/or superficial venous thrombosis, leading to Post-Thrombotic Syndrome (PTS), pulmonary embolism, and increased risk of Catheter-Related Infections (CRI).
Objective: To review the occurrence of deep and superficial vein thrombosis in patients who have undergone PICC placement and also to highlight the complications, epidemiology, risk factors, diagnosis, and management of PICCrelated thrombosis in patients.
Data sources and extraction: We performed article searches and obtained electronic literature from the following databases: PubMed, EMBASE, and Google scholar using key terms. We utilized St. Mary Mercy Hospital for patient data abstraction.
Summary of review: There is evidence that has shown peripherally inserted central catheters may double the risk of deep and superficial venous thrombosis compared with Centrally Inserted Venous Catheters (CIVCs). Duplex ultrasound is the preferred diagnostic imaging modality to rule-out thrombosis.
Conclusion: Medical records on 1,429 PICC-line insertion patients were reviewed. A venous duplex examination was performed on all of the patients who were noted to have complications post-procedure. The duplex was also performed on patients who manifested symptoms such as pain, swelling, and/or extremity discoloration after catheter insertion. The data abstracted concluded, 59% of symptomatic patients post-peripherally inserted central catheters tested positive for Deep Vein Thrombosis (DVT). Once there was sufficient evidence to prove deep vein thrombosis, the catheter was removed or the patient was started on anticoagulation.
Keywords
Deep Vein Thrombosis (DVT); Peripherally Inserted Central Catheters (PICC); Thrombosis; Centrally Inserted Venous Catheters (CIVCs); Upper extremity
Introduction
Peripherally Inserted Central Catheters (PICC) are non-tunneled medium-to long-term vascular access devices which are usually inserted into the deep veins of the upper extremities [1,2]. PICCs are being increasingly utilized in the Intensive Care Unit (ICU), because of the safe insertion, ease of use, lower risk of mechanical injury (such as pneumothorax and vascular injury) and perceived lower incidence of infectious complications with longer duration of use, when compared to Centrally Inserted Venous Catheters (CIVCs) [1-3]. In many hospitals, there are now dedicated vascular access teams available to undertake PICC placement [3].
Background
Deep vein thrombosis and pulmonary embolism is evolving and becoming well known to the public. They are both conditions that are recognized to have life-threatening consequences. The focus for deep vein thrombosis and pulmonary embolism has been mostly on the lower extremities. Upper extremity thrombosis is normally viewed as a more benign entity, but recent data suggested that the significance of morbidity and mortality is equal to that of the lower extremities. The prevalence of upper extremity thrombosis has increased due to the increase in usage of central venous catheters. Although, a majority of patients present with pain, swelling or prominent veins throughout the upper extremity, many patients will present as asymptomatic. While there is published medical literature for a push to increase upper extremity DVT attention, there is no consensus on the treatment methodology. Since upper extremity DVT has become more common secondary to an increase in catheter insertions, more venous duplex examinations are being performed to decrease the morbidity and mortality rates. Since patients can present asymptomatically with an indwelling catheter, it is believed that the incidence of DVT is more likely higher than what data has previously reported.
Methods
Electronic databases were searched and reviewed. The search engines utilized were PubMed, EMBASE, Google Scholar, for articles reporting on the use of peripherally inserted central catheters as well as articles on peripherally inserted central catheters related thrombosis. The following terms were used to search for articles: PICC, Peripherally Inserted Central Catheters, Deep Vein Thrombosis, DVT, PE, pulmonary embolism, thrombosis, upper extremity thrombosis, venous thromboembolism, IVC, PICC thrombosis, PICC management, PICC insertion method, vascular, vascular access and anticoagulation. Our own hospital database was reviewed as well. We abstracted data on patients with PICC-line insertions. The PICC-line specifically utilized at St. Mary Mercy Hospital is the BARD. 1,429 patients were reviewed to obtain the necessary data pertaining to this study. Patients who were selected for the review and data abstraction were from a timespan of approximately two-years, January 2, 2015 to December 30, 2016. Of the 1,429 patients reviewed and 94 venous duplex ultrasounds were performed. The patients whom required an ultrasound were noted to have complications and/or symptoms, which required the examination of the upper extremity to rule-out thrombosis.
Complications
The most common complication of upper extremity deep vein thrombosis is post-thrombotic syndrome also known as PTS. PTS present with features similar to those present in deep vein thrombosis. Patients who present with PTS typically have the pain and swelling like the thrombosis patients, but with PTS venous ulcers and skin pigmentation can be present as well from the chronic venous insufficiency due to prior blood clots in the extremity. Recurrent thrombosis and/or residual are associated with increased PTS risk. Pulmonary embolism is less common with upper extremity venous thrombosis.
Epidemiology
The incidence of PICC-related symptomatic upper extremity venous thrombosis (UVET) ranges 3% to 20% and the rate of asymptomatic thrombosis has be reported as high as 61.9% [3] (7-13). A prospective study by Itkin et al. showed an overall thrombosis rate of 71.9%, on ultrasound of upper extremity veins, in patients with 5F double-lumen PICCS [4]. In a descriptive study of 479 consecutive PICCS placed in neurocritically ill patients, the incidence rate of PICCrelated large vein thrombosis was 8.1% [5].
Bonizzoli et al. provided evidence in patients discharged from the ICU with a PICC in situ, the rate of DVT/1,000 catheter days was 7.7 and the estimated incidence rate of PICC-related thrombosis, 27.2% [6]. One prospective trial which had aimed to recruit 167 ICU patients with triple lumen 6F PICCs was stopped prematurely after recruiting only 50 patients’ due to the unacceptable number of symptomatic (20%) and asymptomatic (58%) UEVTs detected [3]. Of noted is the fact that in the above studies, large-bore PICCs (5F and 6F) were used, without taking into account the vein calibre and so these results may be biased. Although PICC lines reduce the incidence of pneumothorax, they have an incidence of upper extremity venous thrombosis similar to the centrally inserted catheters.
Risk Factors
For thrombus to form, there are three components called Virchow’s triad. The patient must present with at least one of three Virchow’s triad components: stasis, hypercoagulability, and vessel wall injury. Any intravenous catheter has the potential to cause thrombosis. This includes peripheral intravenous catheters, PICCs, tunneled and non-tunneled central catheters, port devices and pacemakers. The diameter of the catheter relative to the size of the vessel lumen can also play a major role in the risk factor of thrombus formation. A catheter which is too large for the vessel can cause blood not to flow freely around the catheter, flow becomes stagnant then thrombus formation occurs. The presence of many congenital or acquired systemic prothrombotic conditions may increase the risk for catheter-induced venous thrombosis. Prior deep or superficial vein thrombosis increases the patient’s risk for catheter-induced thrombus formation as well.
Diagnosis
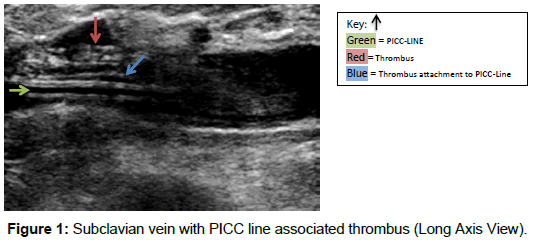
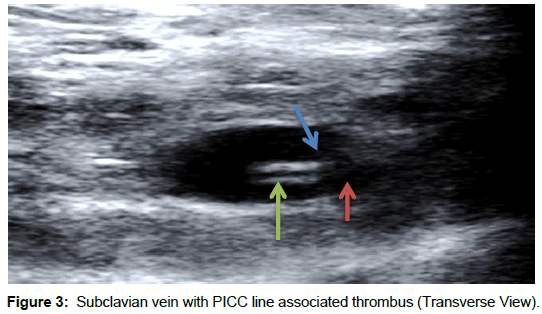
To diagnose PICC-line related thrombosis, a venous duplex must be performed on the symptomatic extremity. We utilized the Phillips IU-22 and Siemens S-2000 ultrasound equipment to perform these venous duplex examinations. When venous duplex examinations are ordered unilaterally, a comparison of the flow characteristics is performed to the contralateral internal jugular vein and subclavian vein. During duplex examinations, compression maneuvers are utilized in order to demonstrate evidence of thrombus. Typically, a venous duplex image will demonstrate a dilated, partial or non-compressible vessel with a hypoechoic spongy-texture within the vessel lumen. The acute thrombus will alter normal venous flow hemodynamics. PICCline observation on duplex, allows the physician to see a hyperechoic catheter within the vessel walls. Ultrasound is able to differentiate whether the thrombus is attached to the PICC-line and/or the vessel wall.
Venous Duplex Ultrasound
Below, are images of patients who had undergone venous duplex to rule out thrombosis (Figures 1-6)?
Prevention
There are various strategies used to reduce thrombotic complications secondary to indwelling catheters that we utilized. The use of heparinized saline solution to flush and/or lock catheters to reduce catheter occlusion has been the standard of care. Recent reviews have shown that the evidence is not reliable for the effectiveness of heparin flushing in reducing catheter occlusion. Data on the benefits of heparin-bonded catheters in reducing thrombosis are scarce, and were published more than two decades ago which makes the data less reliable. Overall, there is not enough supporting evidence that proves heparin bonding reduce catheter thrombotic complications.
Acute Management of PICC-Related Thrombosis
The goal in managing catheter-related venous thrombosis include alleviation of symptoms, minimizing risk for embolization and providing continued intravenous access as needed. For patients with PICC line related thrombosis, embolization is a major cause of morbidity and mortality. Therapy related to treating upper extremity Deep Vein Thrombosis (DVT) is directed toward preventing complications such as pulmonary embolism. Anticoagulant therapy is the general route taken for preventing pulmonary embolism in patients with lower extremity DVT. Starting patients on anticoagulation for upper extremity thrombosis should be just as effective as when treating the lower extremities. The anticoagulation treatment should begin as soon as possible, as it may help decrease the risk for embolization. Routine removal of the catheter is not recommended. In patients who have an on-going need for the catheters, it is reasonable to administer anticoagulant therapy without catheter removal. Removal is not typically necessary, provided the PICC line remains functional and well positioned. This approach has been associated with positive clinical outcome at our organization. There is no standardization for optimal duration of a PICC line while the patient undertakes anticoagulation treatment. The American College of Chest Physicians (ACCP) guidelines favor anticoagulation for up to three months if the thrombosis is symptomatic, associated with cancer, or the catheter remains in place. Still, it is important to keep in mind that there is no published data that has directly compared the one-month and threemonth anticoagulation treatments.
Conclusion
The data abstracted on 1,429 patient’s demonstrated evidence of a high thrombosis rate in the deep vein system post BARD PICC line insertion. We were able to conclude 59% of patients were positive for PICC-line associated deep vein thrombosis (acute) in the upper extremity. Upper extremity deep vein thrombosis is not a benign condition, and it has associated with a general increase in morbidity and mortality. The treatment for upper extremity deep vein thrombosis should be treated similarly to the lower extremity deep vein thrombosis in order to decrease the reoccurrence of DVT, pulmonary embolism, and post-thrombotic syndrome.
References
- Marnejon T, Angelo D, Abu AA, Gemmel D (2011) Risk factors associated with peripherally inserted central venous catheters. J Vasc Access 13: 231-238.
- Wilson TJ, Brown DL, Meurer WJ, Stetler WR, Wilkinson DA, et al. (2012) Risk factors associated with peripherally inserted central venous catheters in neurological intensive care patients. Intens Care Med 38: 272-278.
- Trerotola SO, Stavropoulos SW, Mondschein JI, Patel AA, Fishman N, et al. (2010) Triple lumen peripherally inserted central catheter in patients in the critical care unit: prospective evaluation. Radiology 256: 312-320.
- Itkin M, Mondshein JI, Stavropoulos SW, Shlansky-Goldbery RD, Soulen MC, Trerotola SO (2014) Peripherally inserted central catheter thrombosis-reverse tapered versus nontapered catheters: a randomized controlled study. J Vasc Interv Radiol 25: 85-91.
- Fletcher JJ, Stetler W, Wilson TJ (2011) The clinical significance of peripherally inserted venous catheter-related deep vein thrombosis. Neurocrit Care 15: 454-460.
- Bonizzoli M, Batacchi S, Cianchi G, Zagli G, Lapi F, et al. (2011) Peripherally inserted central venous catheters and central venous catheter-related thrombosis in post-critical patients. Intens Care Med 37: 284-289.
Relevant Topics
- Abdominal Radiology
- AI in Radiology
- Breast Imaging
- Cardiovascular Radiology
- Chest Radiology
- Clinical Radiology
- CT Imaging
- Diagnostic Radiology
- Emergency Radiology
- Fluoroscopy Radiology
- General Radiology
- Genitourinary Radiology
- Interventional Radiology Techniques
- Mammography
- Minimal Invasive surgery
- Musculoskeletal Radiology
- Neuroradiology
- Neuroradiology Advances
- Oral and Maxillofacial Radiology
- Radiography
- Radiology Imaging
- Surgical Radiology
- Tele Radiology
- Therapeutic Radiology
Recommended Journals
Article Tools
Article Usage
- Total views: 9281
- [From(publication date):
June-2017 - Mar 29, 2025] - Breakdown by view type
- HTML page views : 8348
- PDF downloads : 933