Deep Cerebral Venous Sinus Thrombosis (Cvt) with Excellent Recovery in HIV Patient on Antiretroviral Therapy
Received: 05-Dec-2017 / Accepted Date: 21-Dec-2017 / Published Date: 24-Dec-2017 DOI: 10.4172/2314-7326.1000268
Abstract
Deep cerebral venous sinus thrombosis occurs in HIV patient with normal CD4 count. We report a patient who developed CVT while on reverse transcriptase inhibitors for the last four years, with low protein S level.
Introduction
Cerebral venous sinus thrombosis (CVST) is the presence of blood clot also called as acute thrombosis in the dural venous sinuses. Here the case of 40-year-old male has been described who was diagnosed with HIV and deep cerebral venous sinus thrombosis which was treated with antiretroviral therapy.
Case Presentation
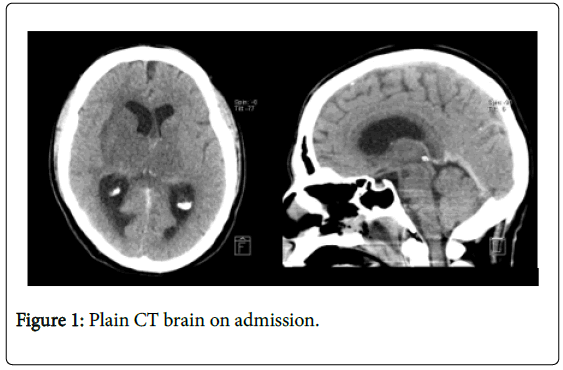
This is a 40-year-old male, diagnosed with HIV 4 years ago, on antiretroviral therapy (Efavirenz 600 mg daily and Emtricitabine/ tenofovir 200/245 mg daily). He had 5-months history of headache and mild unsteadiness, not associated with nausea or vomiting. He presented on 15th of September 2016 to a peripheral hospital with recurrent prolonged seizures. The seizures were aborted with Benzodiazepine. The patient was intubated, sedated and transferred to Neuro critical care unit at King Abdullah Medical City. Upon arrival, his neurological examination was limited due to full sedation but noted to have bilateral papilledema and no obvious localizing signs or meningeal irritation (Figure 1). Plain CT brain showed a fairly symmetrical bilateral basal ganglionic and thalamic hypodensity.
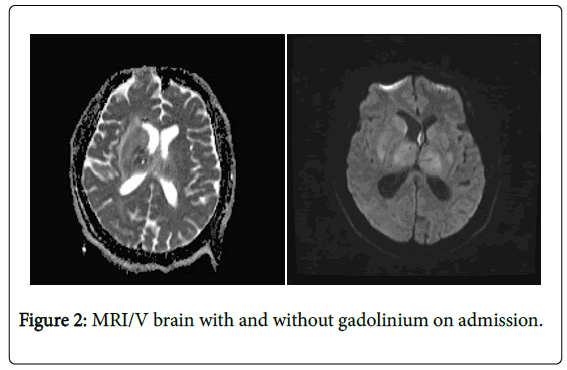
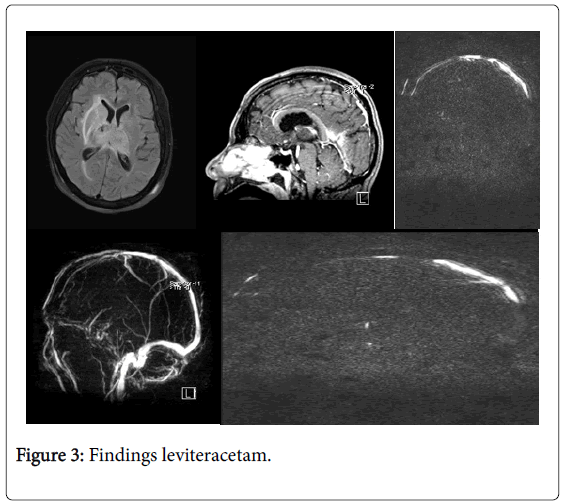
MRI brain on admission showed bilateral thalamic and basal ganglion hyperintensity on Flair, T2 and DWI, T1 showed signal hypointensity of deep cerebral veins, vein of Galen, and straight sinus, T1 post gadolinium showed filling defect of straight sinus and internal cerebral veins. Feature of obstructive hydrocephalus with dilatation of both lateral ventricles with periventricular hyperintensity secondary to the mass effect of the oedematous thalami (Figures 2 and 3).
Based on these findings leviteracetam was initiated, external ventricular drainage (EVD) was inserted, heparin IV infusion was started, and patient was taken to angio-suit for emergency thrombectomy. Thrombectomy of straight sinus thrombus was carried out with recanalization of about 80% of the straight sinus up to the vein of Galen, Heparin was eventually replaced by Warfarin.
Laboratory investigations revealed: Hb 7.9, WBC, platelets, ANCA, ANA, syphilis, anticardiolipin, anti Ro, La, B12 were all normal or negatives. Low vitamin D level of 12.9. Factor V: 121.4 (70-120), Antithrombin 3: 121 (80 -120), Protein S was low at 62 (70-140), Protein C: 148 (70-140), factor 2 Prothrombin G20210A and factor V Leiden mutation were all negative. HIV viral load was 371 copies/ml and CD4 count was 559.
The patient gradually regained his consciousness but with left side weakness. EVD was removed after a week and his muscle power on the left side improved with physiotherapy. He was discharged home on leveteracetham 1500 mg BID and Warfarin in addition to his antiretroviral therapy (Figure 4).
Discussion
Cerebral venous sinus thrombosis (CVST) is a potentially lifethreatening condition representing 0.5% of all strokes [1,2]. Though CVST were not frequently reported in HIV patients in the literature, HIV increase the risk for cerebrovascular disease. 85% of cerebral venous sinus thrombosis has prothrombotic risk factor [3]. By enlarge; CVST could be due to hypercoagulable diseases, inflammatory and infectious diseases including dental abscesses, otitis media, mastoiditis, facial infections, and endocarditis [4,5].
In HIV patients, CVST has been associated with aberrancies in factors essential in the coagulation pathway. In a study of 109 HIVinfected patients, venous and/or arterial thrombosis etiology was: protein C deficiency, elevated factor VIII concentrations, high fibrinogen concentrations, and free protein S deficiency [6]. HIV infection is also associated with an elevated level of D-dimer, along with other markers of dysregulated coagulation and fibrinolysis, which indicates that HIV infection could be associated with a pro-thrombotic state [6].
Furthermore, mechanism for the noted hypercoagulability in patients with HIV infection includes the presence of, heparin cofactor II, antithrombin. And antiphospholipid antibodies. A few studies highlighted a high prevalence of antibodies against protein S in HIV infected patients, leading to significantly low protein S activity in about 31%-76% of patients [7]. It has been noticed that protein S deficiency is not correlated with severity of HIV disease. Moreover, it seems that thrombosis is highly related to low CD4 counts [7,8], which is not the case in our patient. However, protein S level in our case is mildly low at 62 (70-140) but unfortunately protein S activity was not checked.
Konin et al. reported two cases of venous thrombosis associated with protein S deficiency in HIV patients. In the first case they reported superior mesenteric vein thrombosis in 53-year-old HIV patient with protein S deficiency. The second one was a case of cerebral venous sinus thrombosis in HIV patient who was in his third decade. Both of them were not yet on antiretroviral therapy [9].
Inspite of the fact that the absolute risk of thrombosis in patients who are not on combined antiretroviral therapy is almost 6 folds in comparison to healthy population of the same age, there is an additional risk of thrombosis in patients on HAART [10,11]. The prothrombotic effect of HAART is reported to be more common in combinations including protease inhibitors (PIs) [12,13]. Protease inhibitors based therapy promotes thrombosis by inducing platelets and endothelial dysfunction [13]. Nonetheless it is still unclear whether non-protease inhibitors are prothrombotic or not [11,14]. Our patient is on reverse transcriptase inhibitors.
Conclusion
In this HIV patient with normal CD4 count and deep cerebral venous sinus thrombosis, the underlying cause can be possibly in part related to his relatively low protein S and to his treatment with reverse transcriptase inhibitors? However, the possibility of other factors leading to CVT is still open and further case reports might help address this issue.
References
- Yadegari S, Ghorbani A, Miri SR, Abdollahi M, Rostami M (2016) Clinical features, risk factors, and outcome of cerebral venous thrombosis in Tehran, Iran. J Neurosci Rural Pract 7: 554-558.
- Ruiz-Sandoval JL, Chiquete E, Bañuelos-Becerra LJ, Torres-Anguiano C, González-Padilla C, et al. (2012) Cerebral venous thrombosis in a Mexican multicenter registry of acute cerebrovascular disease: the RENAMEVASC study. J Stroke Cerebrovasc Dis 21: 395-400.
- Modi M, Singla V, Ahluwalia J, Sharma A, Prabhakar S, et al. (2012) HIV infection presenting as cerebral venous sinus thrombosis. Am J Emerg Med 30: 517-e1.
- Stam J (2005) Thrombosis of the cerebral veins and sinuses. N Engl J Med 352: 1791-1798.
- Saadatnia M, Fatehi F, Basiri K, Mousavi SA, Mehr GK (2009) Cerebral venous sinus thrombosis risk factors. Int J Stroke 4: 111-123.
- Lijfering WM, Sprenger HG, Georg RR, Van Der Meulen PA, Van Der Meer J (2008) Relationship between progression to AIDS and thrombophilic abnormalities in HIV infection. Clin Chem 54: 1226-1233.
- Mwita JC, Baliki K, Tema L (2013). Cerebral venous sinus thrombosis in HIV-infected patients: Report of 2 cases. Pan Afr Med J 16, 4.
- Bousser MG, Russell RR (1997) Cerebral venous thrombosis. London: WB Saunders, UK. 12: 385-389.
- Konin C, Adoh M, Adoubi A, Anzouan-Kacou JB, Azagoh R, et al. (2008) Unusual venous thrombosis revealing a human immunodeficiency virus infection and a protein S deficiency. Two cases and literature review. Rev Med Interne 29: 508-511.
- Saif MW, Bona R, Greenberg B (2001) AIDS and thrombosis: Retrospective study of 131 HIV-infected patients. AIDS Patient Care STDS 15: 311-320.
- Rasmussen LD, Dybdal M, Gerstoft J, Kronborg G, Larsen CS, et al. (2011) HIV and risk of venous thromboembolism: A Danish nationwide populatio-based cohort study. HIV Medicine 12: 202-210.
- Lijfering WM, Ten Kate MK, Sprenger HV, Van Der Meer J (2006) Absolute risk of venous and arterial thrombosis in HIV-infected patients and effects of combination antiretroviral therapy. J Thromb Haemost 4: 1928-1930.
- Majluf-Cruz A, Silva-Estrada M, Sánchez-Barboza R, Montiel-Manzano G, Treviño-Pérez S, et al. (2004) Venous thrombosis among patients with AIDS. Clin Appl Thromb Hemost 10: 19-25.
- Verma R, Patil TB, Kumar N (2012) Early recanalisation of cerebral venous sinus thrombosis in an unusual case associated with severe protein S deficiency. BMJ Case Rep 2012: bcr2012006496.
Citation: Elamin I (2017) Deep Cerebral Venous Sinus Thrombosis (Cvt) with Excellent Recovery in HIV Patient on Antiretroviral Therapy. J Neuroinfect Dis 8: 268. DOI: 10.4172/2314-7326.1000268
Copyright: © 2017 Elamin I. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 5079
- [From(publication date): 0-2017 - Feb 22, 2025]
- Breakdown by view type
- HTML page views: 4411
- PDF downloads: 668