Case Report Open Access
Decreased Survival in African Patients with Triple Negative Breast Cancer
Marta Honório1, Nuno Guerra-Pereira2, Júlia Silva3, Janice Alves3, Ana Filipa3 and Sofia Braga1*
1Hospital Prof. Doutor Fernando Fonseca, José de Mello Saúde, Portugal
2Hospital Nossa Senhora do Rosário, Portugal
3University of Algarve, Portugal
- *Corresponding Author:
- Sofia Braga, MD, PhD
Hospital Prof. Doutor Fernando Fonseca, José de Mello Saúde, Portugal
Tel: +351966722731
E-mail: sofia.braga@jmellosaude.pt
Received date: May 25, 2016; Accepted date: June 25, 2016; Published date: June 29, 2016
Citation: Honório M, Guerra-Pereira N, Silva J, Alves J, Filipa A, et al. (2016) Decreased Survival in African Patients with Triple Negative Breast Cancer. J Palliat Care Med 6:270. doi:10.4172/2165-7386.1000270
Copyright: © 2016 Honorio M, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Palliative Care & Medicine
Abstract
Introduction: Triple Negative Breast Carcinomas (TNBC) are more prevalent in younger women especially those with African Ancestry, in whom the disease appears to be more aggressive. Since there are no data on Africans living in continental Europe, we sought to analyse a sample of African women from a European country and determine if, like African Americans, they have more aggressive tumor biology and poorer outcomes.
Methods: We performed a retrospective review of TNBC to compare clinical and pathological features and survival between African and non-African patients. All women presented with breast cancer (BC), between 2005 and 2014, to a single general hospital, in Portugal.
Results: A total of 144 (9.3% of the whole sample) TNBC patients were identified and amongst these, 17 were African (12%). African patients were not significantly younger than non-African patients (median age of 60 years vs 57.2 years, respectively, p=0.59). Regarding tumor size, nodal status and histologic grade at presentation, these variables were very similar between the two cohorts. Nevertheless, the prevalence of initially metastatic BC was significantly higher among the African population (41.2% vs 11%, p<0,005) and the outcome was worse for these patients (median survival: 62 vs 15 months, p<0.005).
Conclusions: Our study demonstrated that African patients more frequently presented with late stage disease and worse survival outcome than the non-African population. These findings may be explained by more aggressive tumor biology.
Keywords
Breast cancer; Estrogen; Progesterone
Introduction
Human BC represents a heterogeneous group of tumors. According to gene expression studies, there are four common molecular subgroups of BC that vary importantly with respect to clinical features, natural history and outcomes [1]. In particular, the TNBC (absence of estrogen receptor (ER), progesterone receptor (PR), and Epithelial Growth Factor Receptor 2 (HER 2) overexpression) which are associated with an overall worse prognosis compared to other breast cancer subtypes. These tumors are more likely to be poorly differentiated, of higher histological grade, associated with a higher recurrence rate and, unlike other subtypes, there are no target therapies. They account for 15-20% of all breast cancer cases, affect mainly younger women and are more prevalent in those with African Ancestry [2]. In Senegal and Nigeria TNBC account for 30% [3] and in Ghana for 82% [4] of all BC cases.
African women with BC have lower survival than British non- African female patients and their carcinomas are more likely to be triple negative (TN) and grade 3 [5]. Despite their aggressiveness and high prevalence in the female population of African ancestry, there is no data on those living in continental Europe, regarding the incidence and outcome of patients with TNBC.
Portugal has a high number of African inhabitants originated from Portuguese-speaking African countries. Since we have observed very aggressive TNBC in African patients and because data from other countries with African patients, especially African American, have confirmed these findings, we decided to determine if African patients living in a European country would have more aggressive disease and worse outcome.
To this end, we compared the clinical and pathological characteristics and the survival of TNBC in African women versus non-African women, using a consecutive sample of TNBC with a longterm follow-up from a general hospital. Our institution provides support to a very heterogeneous population in terms of socioeconomic status and race/ethnicity, serving the most densely populated area in the country, and the largest African community living in Portugal.
Materials and Methods
We selected women, of all ages and races/ethnicities, with TNBC from a consecutive sample of BC patients treated in a single institution from 2005 until 2014. Details of age at diagnosis; race/ethnicity; tumor stage, histology and grade; location of tumor metastases; unilateral or bilateral synchronous/metachronous disease; and estrogen receptor (ER), progesterone receptor (PR), and Epithelial Growth Factor Receptor 2 (HER 2) status were recorded. All data were collected from hospital’s electronic medical records, patient charts and pathology reports. Where ethnicity was undisclosed or histological, or immunohistochemistry, diagnosis was unconfirmed, patients were excluded. Molecular subtypes other than TNBC were also excluded.
Overall Survival (OS) was calculated based on the day of death or the date of last follow-up. Statistical analysis was descriptive and analysis was performed with the use of SPSS Statistics 22nd edition. Categorical variables are presented as frequencies and percentages, and continuous variables as means and standard deviations, or medians and interquartile ranges for variables with skewed distributions. Survival analysis was performed by the Kaplan Meyer method, with Log Rank test used to compare survival between groups. All reported p-values are two-tailed, with a P value of 0.05 indicating statistical significance.
Results
A total of 1552 patients with BC were identified. Of these, 144 had TNBC which represented 9.3% of the whole sample.
Of the 144 patients with TNBC, seventeen were African women (12%). The mean age at the time of the diagnosis for the TNBC population was 57.5 years. The mean age for the African patients was 60 years compared with 57.2 years for the non-African patients (– t (18) =-0.54, p=0.59).
The tumor features in the two patient cohorts were compared (Table 1).
| Tumor features | Non-African no (%) |
African no (%) |
|---|---|---|
| Tumor size | ||
| T1 | 43 (33.9%) | 6 (35.2%) |
| T2 | 50 (39.4%) | 10 (58.8%) |
| T3 | 17 (13.4%) | 1 (5.9%) |
| T4 | 8 (6.3%) | 0 |
| Unknown | 9 (7%) | |
| Total | 127 | 17 |
| Nodal status | ||
| N+ | 37 (29.1%) | 1 (5.9%) |
| N0 | 76 (59.8%) | 8 (47.1%) |
| Unknown | 14 (11%) | 8 (47.1%) |
| Total | 127 | 17 |
| Histological srade | ||
| 1 | 6 (4.7%) | 1 (5.9%) |
| 2 | 45 (35%) | 2 (12.8%) |
| 3 | 61 (48%) | 8 (47%) |
| Unknown | 15 (11.8%) | 6 (35%) |
| Total | 127 | 17 |
| Initial metastatic disease | 14 (11%) | 7 (41.2%) |
| Bilateral disease | 5 (3,9%) | 2 (11.8%) |
| Adjuvant chemotherapy | ||
| Yes | 77 (60.6%) | 6 (35.3%) |
| No | 37 (29.1%) | 10 (58.8%) |
| Unknown | 13 (10.2%) | 1 (5.9%) |
| Total | 127 | 17 |
Table 1: Clinicopathological tumor features in African and non-African triple negative breast cancer patients.
Regarding tumor size, 94.1% of the African patients presented with primary breast tumor size ≤ 5 cm compared with 73.3% of the non- African patients and 5.9% of the Africans presented with tumor size >5 cm compared with 19.7% of the non-Africans, but we could not find statistical difference (Fisher’s exact test, p=1).
Nodal involvement was present in one African patient (5.9%) but was unknown for eight patients. Five of them were initially metastatic, and three others were over 80 years old, with T1 and T2 tumors, and were treated with simple mastectomy without lymphadenectomy or sentinel lymph node assessment.
In the non-African group, 37 patients (29.1%) had nodal involvement and fourteen patients (11%) had no data available. These were initially metastatic patients, where surgery was not performed, or older patients treated with simple mastectomy without axillary staging. Seven patients were found to have bilateral disease which accounted for 4.9% of the whole sample. Regarding the histological characteristics of both lesions, 4 patients had TNBC in both breasts.
Of these, 2 were African patients who presented with synchronous tumors, and 2 were non-African and presented with metachronous lesions (time interval to contralateral cancer was 4 and 9 years). The histological grade assessment showed that 54% of the TNBC population with available data had grade 3 tumors (47% African; 48% Non-African).
The missing information in African patients pertained to those who had initially metastatic disease. In the African group, nine patients (53%) had metastatic disease. Seven of them, which represented 41.2% of the African cohort, presented with synchronous disease – one in the brain, five in the lungs and one in the skin.
And two others developed metachronous metastasis – one in the bone and the other one in the lungs. Concerning the non-African patients, there were thirty-eight metastasized patients (30%), fourteen of them (11%) ab initio – four with lung metastases, three with lymph node metastasis, two with liver metastasis, two with brain metastasis, two with bone metastasis and one with peritoneal metastasis.
The other twenty-four developed metastasis during the course of the disease – eleven with lymph node metastasis, four in the lungs, three in the bone, three in the liver and three in the skin.
The percentage of initially metastatic BC was significantly higher among the TNBC African population (Two-sided Fisher’s exact test p<0.005). Analyzing survival, 102 of the 144 patients (70.8%) are alive, seven of them are African (41.2% of the African group). Of the 42 patients who died, 6 of them died of non-BC related causes.
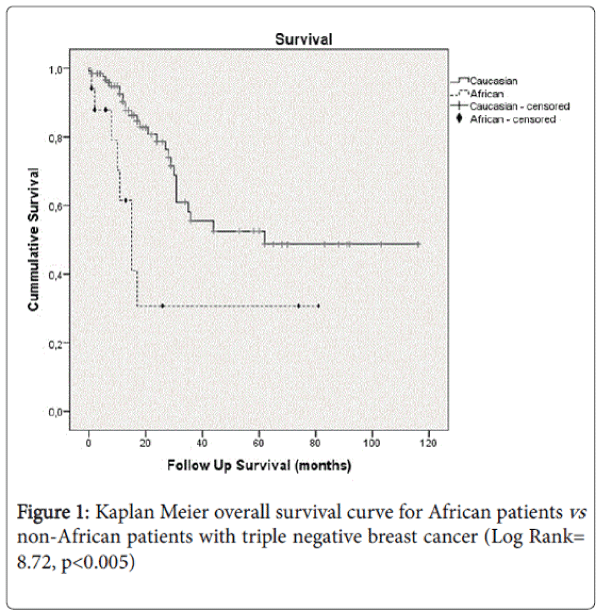
Excluding these patients, the median survival for the TNBC population was 62 months. Considering the groups, the median survival was 62 months for the non-Africans compared with 15 months for the Africans (Log Rank= 8.72, p< 0.005) (Figure 1).
Concerning the African TNBC population, ten patients have died. Two of them died of non-breast cancer related causes and eight patients died of metastatic breast cancer. Of these 8 patients, six were initially metastatic and two became so during follow-up (one had a survival of 3 months and the other one of 1 month after the diagnosis of metastatic disease). There is one patient, who had initially metastatic BC, that is still alive with a survival of 9 months.
Discussion
In the Carolina Breast Cancer Study, the percentage of patients with TNBC was 20% [6], in our dataset it was only 9.3%. Despite other series showing early age of onset of TNBC or early age of onset of breast cancer in Africans, in our analysis we were not able to show this difference. Stead LA et al. [7] have documented increased, equivalent proportions of TNBC both in younger and older African women.
In our series of patients, we were able to show that Africans with TNBC had higher prevalence of initially metastatic breast cancer when compared to non-African patients with TNBC. This finding has not before been reported in the literature. Regarding bilateral disease, we found that four of our patients with bilateral BC had TN tumors. Two of them were African with synchronous tumors at the time of diagnosis which may, in part, reflect the aggressiveness of the disease in this population.
Other series of TNBC and of BC in African patients showed that BC in Africans are more frequently poorly differentiated [8]. In our dataset we did not draw this conclusion. We have found, in the whole sample, a high prevalence of poorly differentiated carcinomas, which was around 50%.
We were not able to find differences with regard to tumor size and nodal involvement, at the time of diagnosis, between the African and non-African populations. Nevertheless, it is interesting to notice that despite this similarity more African patients presented with metastatic disease and had worse survival outcome. This, in line with other previous reports, shows that the worse prognosis in Africans may not only be due to late diagnosis but to an underlying aggressive biology [9]. The Southwest Oncology Group reported similar clinical trial data. In a retrospective analysis of a large clinical trial database, authors [10] were able to show that in stage-matched and treatment-matched patients, with adjustment to socioeconomic status, there is worse prognosis in early African American BC patients when compared to white patients.
The main limitations of our study were the very small numbers, namely only seventeen patients were African. This fact probably did not allow us to show statistical significance in certain comparisons, and hence draw some conclusions. The other limitation was the retrospective nature of this study, and probably more African patients could have been identified. The socioeconomic status was another limitation, which in this series may have been a confounding factor. In the population served by our institution, the Africans have a lower socioeconomic status which may concur to late diagnosis and noncompliance with therapy enhancing the effect of race and decreased survival in TNBC.
It is important, therefore, to target this population to raise their awareness to the risk factors of breast cancer, the importance of selfexamination and the early presentation with clinical signs. The access to the health care services should be made easier and alterations to the screening services offered to the black populations might be considered.
We may conclude that given their worse prognosis, African patients with TNBC may be considered upfront f or referral to Palliative care.
Author disclosure statement
No competing financial interests exist.
References
- Kassam F, Enright K, Dent R, Dranitsaris G, Myers J, et al. (2009) Survival outcomes for patients with metastatic triple-negative breast cancer: implications for clinical practice and trial design. Clin Breast Cancer 9: 29-33
- Peddi PF, Ellis MJ, Ma C (2012) Molecular basis of triple negative breast cancer and impications for therapy. Int J Breast Cancer 217185.
- Huo D, Ikpatt F, Khramtsov A, Dangou JM, Nanda R, et al. (2009) Population differences in breast cancer: survey in indigenous African women reveals over-representation of triple negative breast cancer. J ClinOncol 27: 4512-4521.
- Stark A, Kleer CG, Martin I, Awuah B, Nsiah-Asare A, et al. (2010) African ancestry and higher prevalence of triple-negative breast cancer. Cancer 116: 4926-4932.
- Bowen RL, Duffy SW, Ryan DA, Hart IR, Jones JL (2008) Early onset of breast cancer in a group of British black women. Br J Cancer 98: 277-281
- Carey LA, Perou CM, Livasy CA, Dressler LG, Cowan D, et al. (2006) Race, breast cancer subtypes, and survival in the Carolina breast cancer study. JAMA 295: 2492-2502.
- Stead LA, Lash TL, Sobieraj JE, Chi DD, Westrup JL, et al. (2009) Triple-Negative Breast Cancers are increased in black women regardless of age or body mass index. Breast cancer res 11: R 18.
- Morris GJ, Naidu S, Topham AK, Guiles F, Xu Y, et al. (2007) Differences in breast carcinoma characteristics in newly diagnosed African-American and Caucasian patients: a single-institution compilation compared with the national Cancer Institute’s Surveillance, Epidemiology, and End Results database. Cancer 110: 876-884.
- Newman LA, Griffith KA, Jatoi I, Simon MS, Crowe JP, Colditz GA (2006) Meta-analysis of survival in African American and white American patients with breast cancer: ethnicity compared with socioeconomic status. J ClinOncol 24: 1342: 1349.
- Albain KS, Unger JM, Crowley JJ, Coltman CA, Hershman DL (2009) Racial disparities in cancer survival among randomized clinical trials patients of the southwest oncology group. J Natl Cancer Inst 101: 984-992.
Relevant Topics
- Caregiver Support Programs
- End of Life Care
- End-of-Life Communication
- Ethics in Palliative
- Euthanasia
- Family Caregiver
- Geriatric Care
- Holistic Care
- Home Care
- Hospice Care
- Hospice Palliative Care
- Old Age Care
- Palliative Care
- Palliative Care and Euthanasia
- Palliative Care Drugs
- Palliative Care in Oncology
- Palliative Care Medications
- Palliative Care Nursing
- Palliative Medicare
- Palliative Neurology
- Palliative Oncology
- Palliative Psychology
- Palliative Sedation
- Palliative Surgery
- Palliative Treatment
- Pediatric Palliative Care
- Volunteer Palliative Care
Recommended Journals
- Journal of Cardiac and Pulmonary Rehabilitation
- Journal of Community & Public Health Nursing
- Journal of Community & Public Health Nursing
- Journal of Health Care and Prevention
- Journal of Health Care and Prevention
- Journal of Paediatric Medicine & Surgery
- Journal of Paediatric Medicine & Surgery
- Journal of Pain & Relief
- Palliative Care & Medicine
- Journal of Pain & Relief
- Journal of Pediatric Neurological Disorders
- Neonatal and Pediatric Medicine
- Neonatal and Pediatric Medicine
- Neuroscience and Psychiatry: Open Access
- OMICS Journal of Radiology
- The Psychiatrist: Clinical and Therapeutic Journal
Article Tools
Article Usage
- Total views: 11452
- [From(publication date):
July-2016 - Apr 02, 2025] - Breakdown by view type
- HTML page views : 10592
- PDF downloads : 860