Research Article Open Access
Decompressive Craniectomy and Partial Temporal Lobectomy for Herpes Simplex Virus Encephalitis with Refractory Intracranial Hypertension in an Adolescent
Stephen Ray1,2, Anand Iyer1, Conor Mallucci3, Tom Solomon2,4 and Rachel Kneen1,2*
1Littlewoods Neurosciences Unit, Alder Hey Children’s NHS Foundation Trust, UK.
2Institute of Infection and Global Health, University of Liverpool, UK.
3Department of Paediatric Neurosurgery, Alder Hey Children‘s NHS Foundation Trust, UK.
4Walton Centre for Neurology and Neurosurgery NHS Foundation Trust, UK.
- *Corresponding Author:
- Dr Rachel Kneen
Littlewood Neurosciences Unit
Alder Hey Children’s NHS Foundation Trust
Eaton Road, Liverpool, L12 2AP, UK
Tel: 01512525163
E-mail: rachel.kneen@liverpool.ac.uk
Received March 17, 2015; Accepted April 28, 2015; Published April 30, 2015
Citation: Ray S, Iyer A, Mallucci C, Solomon T, Kneen R (2015) Decompressive Craniectomy and Partial Temporal Lobectomy for Herpes Simplex Virus Encephalitis with Refractory Intracranial Hypertension in an Adolescent. J Neuroinfect Dis 6:174. doi: 10.4172/2314-7326.1000174
Copyright: © 2015 Ray S, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Neuroinfectious Diseases
Abstract
Herpes simplex virus (HSV) encephalitis is an uncommon, but potentially devastating brain infection with significant morbidity and mortality. Some patients develop a brainstem herniation syndrome because the virus has a predilection for the temporal lobes despite prompt treatment with the antiviral drug aciclovir. We report a case of HSV encephalitis in an adolescent who developed severe cerebral oedema and subfalcine herniation which was refractory to medical management. He underwent a decompressive craniectomy with partial right temporal lobectomy. He made a rapid recovery with no physical deficits though he has some residual neuropsychological problems similar to those reported following HSV encephalitis previously.
Neurosurgical intervention appears to be uncommon in HSV encephalitis: to our knowledge only four other children are reported to have had a similar procedure. We describe our case in detail and provide a full review of the literature surrounding neurosurgical intervention in severe HSV encephalitis.
Keywords
Herpes simplex encephalitis; Raised intracranial pressure; Temporal lobectomy; Craniectomy
Introduction
Viral encephalitis is relatively uncommon, with a reported incidence of 1.5 cases/100,000 in England [1]. Herpes simplex virus (HSV) is the most common viral cause of encephalitis, accounting for approximately 50% of cases [1,2]. Therefore, a typical district general hospital in the UK might expect to see approximately 1-2 children with HSV encephalitis per year [3]. The introduction of successful medical treatment with the antiviral drug aciclovir, led to a reduction in mortality, but it still remains high at 10-30% [2,4,5]. One cause of death is brainstem herniation: HSV typically affects the temporal lobes (often with asymmetry) which can lead to brain oedema and subsequent shift of brain compartments [3]. Prompt medical treatment is associated with a better prognosis, but problems with recognition and diagnosis of HSV encephalitis are common and often lead to delayed diagnosis [5]. Treating clinicians should be aware of the risks of brain compartment shift, monitor patients carefully for clinical signs suggesting this, and involve intensive care and potentially neurosurgical colleagues early in these cases. Aggressive neuroprotective strategies and timely neurosurgical intervention to relieve raised intracranial pressure (ICP) can be life-saving in these cases.
We report a case of a 13-year-old boy with HSV encephalitis, who developed refractory cerebral oedema in the right temporal lobe and in whom decompressive craniectomy with partial temporal lobectomy was lifesaving. His overall outcome was good and did not appear to have been affected by the development of the brainstem herniation syndrome.
Case Report
A 13-year-old, right-handed boy presented with a two-day history of vomiting, fever, lethargy and abdominal pain. He subsequently had two brief left sided clonic seizures with secondary generalization. On examination, he was encephalopathic with a Glasgow Coma Scale (GCS) of 11 out of 15 (eyes 3, motor 5 and verbal 3). There were no focal neurological signs and the rest of the physical examination was normal. An initial non-axial brain computed tomography (CT) scan was normal and he was commenced on cefotaxime for suspected bacterial meningitis. Blood investigations revealed a neutrophilia, but the rest of the investigations were unremarkable.
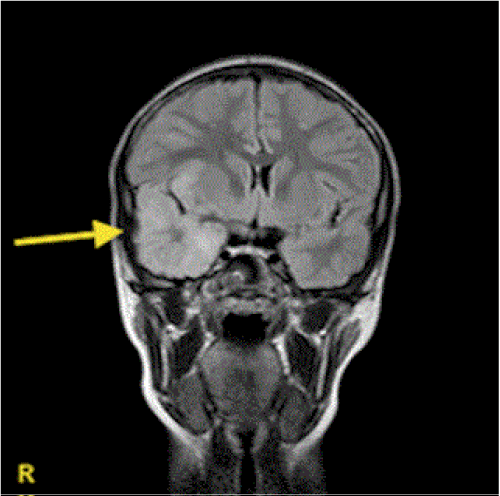
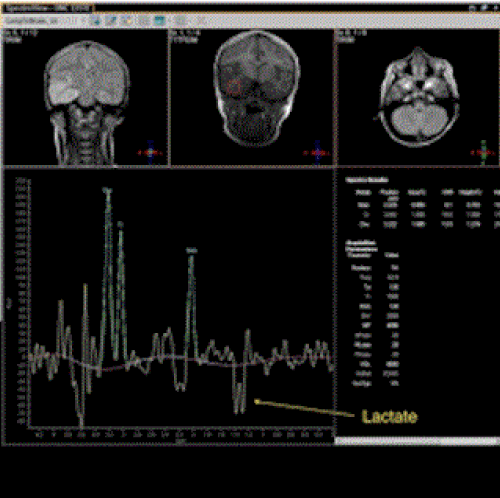
Over the next day his GCS fluctuated between 10 and 14, but on day 3 of admission, his condition deteriorated with a further brief left sided clonic seizure. He was noted to have developed a left hemiparesis with deteriorating level of consciousness. Magnetic resonance imaging (MRI) of the brain showed hyperintense T2 signal with restricted diffusion on diffusion weighted imaging (DWI) in the right temporal lobe (Figure 1). Magnetic resonance spectroscopy (MRS) showed reduced N-acetylaspartate (NAA) peak and a prominent lactate doublet (Figure 2). A lumbar puncture (LP) revealed 78 white cells/mm3 (12 neutrophils/ mm3, 66 monocytes/mm3, 10 red blood cells/mm3), an elevated protein level of 0.64 g/l, and normal glucose of 3.3 mmol/l (plasma glucose 5 mmol/l). Subsequently the polymerase chain reaction (PCR) for HSV type 1 DNA was positive confirming the diagnosis of HSV encephalitis.
On day two of admission, 360 milligrams (mg) (10 mg/kg) of intravenous (IV) aciclovir was commenced, four times daily, to treat suspected HSV encephalitis. Despite this, the patient remained encephalopathic (GCS 10 to 12) until day 7 when he deteriorated acutely with deepening coma (GCS 5), hypertension, bradycardia and the development of a right fixed dilated pupil and absent deep tendon reflexes in the lower limbs; features consistent with tentorial herniation. An urgent CT scan of the brain showed extensive infarct of the right temporal lobe with significant midline shift. Intensive care support was initiated, along with medical management of raised.
On day two of admission, 360 miligrams (mg) (10 mg/kg) of intravenous (IV) aciclovir was commenced, four times daily, to treat suspected HSV encephalitis. Despite this, the patient remained encephalopathic (GCS 10 to 12) until day 7 when he deteriorated acutely with deepening coma (GCS 5), hypertension, bradycardia and the development of a right fixed dilated pupil and absent deep tendon reflexes in the lower limbs; features consistent with tentorial herniation. An urgent CT scan of the brain showed extensive infarct of the right temporal lobe with significant midline shift. Intensive care support was initiated, along with medical management of raised ICP on day 7, which included a 34 gram (1 gram/kg) stat dose of IV mannitol, 4 mg of IV dexamethasone (twice daily) and full maintenance IV hypertonic saline, 2.7%.
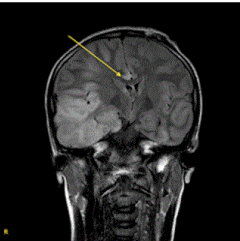
At this point, his prognosis was considered to be poor and neurosurgical intervention was considered; however the outcome of any surgical treatment was uncertain and few cases had been reported in the literature for reference (Table 1). A decision was made to undertake another MRI brain scan (intraoperative scanner in the theatre suite) to assess the extent of the inflammation, particularly to assess if there was mainly unilateral involvement. In addition we planned ICP monitoring with drainage of cerebrospinal fluid (CSF) to reduce pressure as a first step. An external ventricular drain plus intraparenchymal pressure transducer was inserted. The initial intracranial pressure was 52 mm CSF; it decreased to 32 mm after CSF drainage, but did not reduce further. At this stage the intraoperative MRI of his brain (Figure 3) demonstrated persistence of the midline shift due to cerebral oedema involving the right temporal lobe. After careful consideration by the full team, and discussion with the patient’s family, consent was given for a decompressive craniectomy with partial resection of the right temporal lobe to reduce the tentorial herniation.
| References (year) | Patient age (years) | Clinical presentation (as described in the report) |
Neuroimaging | Neurosurgical intervention | Glasgow Outcome Score*, Comments |
|---|---|---|---|---|---|
| Ebel (12) (1998) | 0.8 | Somnolence, L clonic seizure, L hemiparesis |
R temporal lobe haemorrhagic conversion & transtentorial herniation | R craniotomy & anterior temporal lobectomy | 5 |
| Sanchez-Carpintero (13) | 6 | Fever, encephalopathy, L clonic seizures, L hemiparesis |
Initial CT scan normal, MRI 2 days later showed extensive necrotic haemorrhagic lesions of the R temporal lobe with midline shift & uncal herniation |
R craniotomy, duraplasty & R anterior temporal lobectomy |
4, Mild verbal and visual explicit memory impairments. Attention deficit disorder |
| (2008) | 9 | Fever, vomiting, status epilepticus, unreactive R pupil, L hemiplegia |
CT - Oedematous R temporal lobe with haemorrhagic changes & uncal herniation |
R craniotomy & temporal lobectomy | 4, L superior quadrantonopia |
| 13 | Fever, headache, vomiting, neck stiffness, L focal seizures | CT – R temporal lobe hypodensity with mass effect |
R temporoparietal craniectomy | 5 | |
| Kannu (14) (2004) | 16 | Headache, vomiting, encephalopathy, L hemiparesis, diplopia |
CT - R temporal frontal low signal | Decompressive craniectomy | 5 |
| Gonzalez Rabelino (15) (2008) | 14 | Fever, headache, lethargy, seizure, L arm drift |
CT - Low attenuation in R temporal lobe with mass effect & enhancement |
R craniotomy & temporal lobectomy | 5 |
| 32 | Headaches, vomiting, seizures, third nerve palsy, encephalopathy | CT - High & low attenuation lesion in R temporal lobe with midline shift & ring enhancement |
R craniotomy & temporal lobectomy | 5 | |
| Gonzalez Rabelino (15) (2008) | 15 | Fever, headache, vomiting & R focal seizures |
L temporal & parietal lobe oedema with partially haemorrhagic conversion & midline shift | L craniectomy & duraplasty | 5 |
| Counsell (16) (1994) | 21 | Fever, malaise, headache, vomiting, encephalopathy, papilloedema, L hemiparesis |
Lesion in R temporal region on carotid angiogram & abnormal EEG in R temporal lobe region |
R craniotomy | 5 |
| Counsell (16) (1994) | 21 | Fever, headache, myalgia, seizures, anisosocria | CT - Large hyperdense lesion R temporoparietal region with R temporal uncal herniation |
R craniotomy | 4, Seizures, mild aphasia, mild frontal lobe syndrome |
| Bayram (17) | 23 | Hemiparesis, encephalopathy | Unknown | Decompressive craniotomy & duraplasty | 5 |
| (2008) | 61 | Hemiparesis, encephalopathy | Unknown | Decompressive craniotomy & duraplasty | 5 |
| 25 | Comatose, flexion posturing | R hemispheric oedema | R craniectomy & duraplasty | 5 | |
| Laha (18) (1976) | 25 | Obtunded | R frontotemporal lobe oedema, transtentorial herniation | R craniectomy & duraplasty | 5 |
| Mellado (19) (2003) | 42 | Early headaches, later anisocoria, comatose | R temporal lobe oedema, haemorrhagic conversion | R craniectomy, duraplasty & evacuation of R temporal lobe |
4, Minor neurocognitive deficits |
| Stula (20) (1992) | 37 | Headache, encephalopathy, dysarthria, R hand weakness, unable to stand, later anisocoria |
CT - Hyperintense R temporal lobe, massive cerebral oedema, midline shift, transtentorial herniation, compression of brainstem |
R craniectomy & temporal lobectomy | 5 |
| Stula (20) (1992) | 37 | Early headaches, memory loss and personality change, later anisocoria, encephalopathy | L temporal lobe oedema, haemorrhagic conversion & brainstem compression | L craniectomy, duraplasty & L anterior temporal lobectomy |
5 |
| 48 | Early severe headaches, later R hemiparesis & anisocoria |
L temporal lobe oedema, haemorrhagic conversion | L craniectomy, duraplasty & L temporal lobectomy |
4, Stutter | |
| Schwab (21) (1997) | 38 | Fever, myalgia, encephalopathy | MRI - Diffuse hyperintensity of R frontotemporal region |
R craniectomy | 5 |
| 60 | Fever, headache, neck stiffness, encephalopathy, focal seizure | CT - Mesial temporal lobe involvement with haemorrhage | Decompressive craniectomy & haemorrhagic evacuation of temporal lobe | 5 | |
| Taferner (22) | 66 | Fever, encephalopathy, branchiofacial palsy, facial apraxia | CT - Extensive R temporal lesion with uncal herniation, midline shift & gross cerebral oedema |
R craniectomy & duraplasty |
4, Poor short term recall and mildly abnormal gait |
| (2001) | U, Adult | Fever, headache, worsening encephalopathy | Unknown | Decompressive hemicraniectomy, anterior temporal lobectomy & dural augmentation | 5 |
| U, Adult | Fever, headache, worsening encephalopathy | Unknown | Decompressive hemicraniectomy, anterior temporal lobectomy & dural augmentation | 5 |
Table 1: Summary of case reports with neurosurgical intervention in severe HSV encephalitis. R: Right, L: Left, U: Unknown, CT: Computed Tomography, MRI: Magnetic Resonance Imaging.*GOS – Glasgow Outcome score – a 5-level score given to victims of traumatic brain injury during recovery to categorize their outcome (28)1. Dead 2. Vegetative State (meaning the patient is unresponsive, but alive; a “vegetable” in lay language) 3. Severely Disabled (conscious but the patient requires others for daily support due to disability) 4. Moderately Disabled (the patient is independent but disabled) 5. Good Recovery (the patient has resumed most normal activities but may have minor residual problem).
Neurosurgical Intervention
A generous right temporoparietal craniectomy was performed to expose the swollen temporal lobe. On opening the dura, largely necrotic swollen temporal lobe herniated out and a limited lobectomy was performed until the brain was slack and pulsatile. The dura was left open, with a layer of dural substitute laid over the defect to allow for any potential swelling. The bone flap was not fixed but allowed to float freely over the decompression to allow for any further swelling.
Following surgery, the ICP was stable around 11 mm CSF and a postoperative CT scan showed resolution of the midline shift. The patient made a rapid recovery without any further interventions. Polymerase chain reaction of the CSF taken at repeat LP after 21 days of aciclovir remained positive therefore treatment with aciclovir was continued for a further two weeks (total of five weeks). Analysis of the CSF at the end of this extended treatment period was negative for HSV PCR.
Outcome
He had no residual motor deficits, but did display a range of behavioral and cognitive vulnerabilities in the early stages of rehabilitation. When assessed at 9 months he continued to demonstrate vulnerabilities in memory and executive functioning, struggling with planning, sequencing and novel problem solving tasks. He also presented with increased anxiety and obsessive-compulsive symptoms. He received an intensive period of neurological, psychological and educational rehabilitation and is now independently studying for his fitness exams at college.
Discussion
Herpes simplex virus (HSV) encephalitis is a rare but potentially fatal infection of the brain. The management has improved considerably in recent years: improved diagnostic tests (viral PCR of the CSF), and modern neuroimaging techniques (especially Diffusion Weighted Imaging (DWI)) have facilitated a more rapid diagnosis. Antiviral treatment (aciclovir) and advanced neurointensive care and rehabilitation have improved outcome. Despite this, the mortality is still reported to be 10-30% with deaths usually occurring from brain herniation syndromes [5]. Focal involvement of the temporal lobe is common in HSV encephalitis and leads to raised ICP. Patients should be monitored carefully for signs of raised ICP and incipient brain herniation syndromes, and some may require invasive ICP monitoring if they have a low coma score or need intensive seizure management.
The gold standard for diagnosing HSV encephalitis is detecting HSV DNA via PCR of the CSF. This investigation has a sensitivity and specificity of between 75-85% and 60-90% respectively [3,5]. However, it can take several days for these tests to become available. In addition, if an LP is undertaken early in the disease, there may be no white cells in the CSF, which may also be negative for HSV at that stage [3,6,7]. Therefore, integration of clinical findings with imaging might help in diagnosing HSV encephalitis early in the absence of definitive CSF results. Newer MRI sequences such as DWI have been shown to be more sensitive than standard MRI sequences [8-10]. Diffusion Weighted Imaging is particularly sensitive in detecting the extent of disease during the early stages. Restricted diffusion is seen in areas of cytotoxic oedema which is often due to tissue hypoxia. In this case, we also noted an exaggerated lactate peak on the MRS which is an indicator of anaerobic glycolysis [11]. The restricted diffusion and raised lactate in this case are nonspecific findings but an indicator of the severity of disease.
Neurosurgical intervention in HSV encephalitis is rare. Decompressive craniectomy is a lifesaving intervention for the control of intractably raised ICP for a variety of neurological disorders such as head trauma, space-occupying hemispheric infarction and subdural hematoma. Clearly there are potential complications of offering craniotomy and partial temporal lobectomy including infection and hemorrhage amongst others. Therefore one would only propose offering this surgical intervention in herpes simplex encephalitis in the context of failed medical treatment resulting in life threatening raised ICP, with impending ischemia, brainstem shift and ultimately death.
Table 1 [12-28] provides a list of English and non-English language articles reporting HSV encephalitis with neurosurgical intervention to date. One English case and two non-English cases were omitted due to inadequate detail regarding clinical presentation, investigation and outcome. Sixteen adults (median age 38 years) and seven children (median age 10 years) underwent a neurosurgical intervention, predominantly decompressive craniectomy. The presenting features for all these cases were typical for HSV encephalitis and the reason for neurosurgical intervention was progression of encephalopathy and anisocoria in some cases, however there were no specific presenting features that would predict the need for neurosurgical intervention. To our knowledge, only four children [12-14,16] and eight adults [16,22-24,26,28] are reported to have undergone a temporal lobectomy for treatment of raised ICP in HSV encephalitis. It is probable that there have been more cases worldwide that are unreported. Temporal lobectomy reduces intracranial pressure, removes the focal necrotic-haemorrhagic brain tissue and the accompanying inflammation, and probably helps prevent gliotic scarring [13]. This may also prevent symptomatic longterm epilepsy, which is reported in 15-44% of survivors after HSV encephalitis in adults [3]. The outcome in most cases reported in Table 1 appears to have been favorable with minor neurocognitive deficits reported. However, details of formal neuropsychological tests are not given. It is also possible that in unreported cases there has been a more unfavorable outcome than described in our review.
In conclusion, decompressive craniectomy and partial temporal lobectomy for a patient with HSV encephalitis and a brain stem herniation syndrome can be a lifesaving treatment. Our patient had some neuropsychiatric sequalae but this is also reported in medically managed HSV encephalitis and is unlikely to be directly related to surgical intervention.
Acknowledgements
We acknowledge Dr. Shivaram Avula and Andrew Healey for their helpful comments on the radiology aspects; Victoria Gray for her helpful comments on the neuropsychological outcomes and Matthew Grant for his help with the literature search.
References
- Granerod J, Ambrose HE, Davies NW, Clewley JP, Walsh AL, et al. (2010) Causes of encephalitis and differences in their clinical presentations in England: a multicentre, population-based prospective study. The Lancet Infectious diseases 10: 835-44.
- Davison KL, Crowcroft NS, Ramsay ME, Brown DW, Andrews NJ (2003) Viral encephalitis in England, 1989-1998: what did we miss? Emerg Infect Dis 9: 234-240.
- Kneen R, Michael BD, Menson E, Mehta B, Easton A, et al (2006) Management of suspected viral encephalitis in children - Association of British Neurologists and British Paediatric Allergy, Immunology and Infection Group national guidelines. J fect 64: 449-77.
- Whitley RJ (2006) Herpes simplex encephalitis: adolescents and adults. Antiviral Res 71: 141-148.
- Thompson C, Kneen R, Riordan A, Kelly D, Pollard AJ (2012) Encephalitis in children. Arch Dis Child 97: 150-161.
- Raschilas F, Wolff M, Delatour F, Chaffaut C, De Broucker T, et al. (2002) Outcome of and prognostic factors for herpes simplex encephalitis in adult patients: results of a multicenter study. Clin Infect Dis 35: 254-260.
- Steiner I, Budka H, Chaudhuri A, Koskiniemi M, Sainio K, et al. (2005) Viral encephalitis: a review of diagnostic methods and guidelines for management. Eur J Neurol 12: 331-343.
- Sener RN (2001) Herpes simplex encephalitis: diffusion MR imaging findings. Comput Med Imaging Graph 25: 391-397.
- McCabe K, Tyler K, Tanabe J (2003) Diffusion-weighted MRI abnormalities as a clue to the diagnosis of herpes simplex encephalitis. Neurology 61: 1015-1016.
- Küker W, Nägele T, Schmidt F, Heckl S, Herrlinger U (2004) Diffusion-weighted MRI in herpes simplex encephalitis: a report of three cases. Neuroradiology 46: 122-125.
- Sämann PG, Schlegel J, Müller G, Prantl F, Emminger C, et al. (2003) Serial proton MR spectroscopy and diffusion imaging findings in HIV-related herpes simplex encephalitis. AJNR Am J Neuroradiol 24: 2015-2019.
- Ebel H, Kuchta J, Balogh A, Klug N (1999) Operative treatment of tentorial herniation in herpes encephalitis. Childs NervSyst 15: 84-86.
- Sánchez-Carpintero R, Aguilera S, Idoate M, Bejarano B (2008) Temporal lobectomy in acute complicated herpes simplex encephalitis: technical case report. Neurosurgery 62: E1174-1175.
- Kannu P, Pinnock R (2004) Uncommon complication of herpes simplex encephalitis. J Paediatr Child Health 40: 711-713.
- González Rabelino GA, Fons C, Rey A, Roussos I, Campistol J (2008) Craniectomy in herpetic encephalitis. PediatrNeurol 39: 201-203.
- Counsell CE, Taylor R, Whittle IR (1994) Focal necrotising herpes simplex encephalitis: a report of two cases with good clinical and neuropsychological outcomes. J NeurolNeurosurg Psychiatry 57: 1115-1117.
- Bayram N, Ciftdogan DY, Karapinar B, Ozgiray E, Polat M, et al. (2008) A case of herpes simplex encephalitis revealed by decompressive craniectomy. Eur J Pediatr 167: 821-822.
- Laha RK, Saunders FW, Huestis WS (1976) Herpes simplex encephalitis: treatment with surgical decompression and cytosine arabinoside. Can Med Assoc J 115: 236-237.
- Mellado P, Castillo L, Andresen M, Campos M, Perez C, et al. (2003) Decompressive craniectomy in a patient with herpetic encephalitis associated to refractory intracranial hypertension. Rev Med Chil 131: 1434-8.
- Stula D, Lyrer P (1992) [Severe herpes simplex encephalitis: course 15 years following decompressive craniotomy]. Schweiz Med Wochenschr 122: 1137-1140.
- Schwab S, Jünger E, Spranger M, Dörfler A, Albert F, et al. (1997) Craniectomy: an aggressive treatment approach in severe encephalitis. Neurology 48: 412-417.
- Taferner E, Pfausler B, Kofler A, Spiss H, Engelhardt K, et al. (2001) Craniectomy in severe, life-threatening encephalitis: a report on outcome and long-term prognosis of four cases. Intensive Care Med 27: 1426-1428.
- Midi I, Tuncer N, Midi A, Mollahasanoglu A, Konya D, et al. (2007) Effects of decompressive surgery on prognosis and cognitive deficits in herpes simplex encephalitis. BehavNeurol 18: 245-249.
- Yan HJ (2002) Herpes simplex encephalitis: the role of surgical decompression. SurgNeurol 57: 20-24.
- Pili-Floury S, Valentin L, Blasco G, Godard J, Samain E (2009) Late refractory intracranial hypertension treated by decompressive craniectomy in severe herpetic encephalitis. Ann FrAnesthReanim 28: 709-10.
- Di Rienzo A, Iacoangeli M, Rychlicki F, Veccia S, Scerrati M (2008) Decompressive craniectomy for medically refractory intracranial hypertension due to meningoencephalitis: report of three patients. ActaNeurochir (Wien) 150: 1057-65.
- Maraite N, Mataigne F, Pieri V, Dang T, Diederich NJ (2009) Early decompressive hemicraniectomy in fulminant herpes simplex encephalitis. Bull SocSci Med Grand Duche Luxemb2: 131-3.
- Adamo MA, Deshaies EM (2008) Emergency decompressive craniectomy for fulminating infectious encephalitis. J Neurosurg 108: 174-176.
Relevant Topics
- Bacteria Induced Neuropathies
- Blood-brain barrier
- Brain Infection
- Cerebral Spinal Fluid
- Encephalitis
- Fungal Infection
- Infectious Disease in Children
- Neuro-HIV and Bacterial Infection
- Neuro-Infections Induced Autoimmune Disorders
- Neurocystercercosis
- Neurocysticercosis
- Neuroepidemiology
- Neuroinfectious Agents
- Neuroinflammation
- Neurosyphilis
- Neurotropic viruses
- Neurovirology
- Rare Infectious Disease
- Toxoplasmosis
- Viral Infection
Recommended Journals
Article Tools
Article Usage
- Total views: 15885
- [From(publication date):
May-2015 - Apr 05, 2025] - Breakdown by view type
- HTML page views : 11247
- PDF downloads : 4638