Case Report Open Access
Decalcification does not Affect Immunohistochemical Stain of HBME-1 on Papillary Thyroid Carcinoma
Shuting Bai1*, Luis Chiriboga2, Keith Heller3, Kepal N Patel3 and Virginia A LiVolsi41Department of Pathology, Tisch Hopsital, New York University Langone Medical Center, USA
2Experimental Pathology Core Lab, New York University Langone Medical Center, USA
3Devision of Endocrine Surgery, Department of Surgery, New York University Langone Medical Center, USA
4Department of Pathology, Hospital of University of Pennsylvania, USA
- *Corresponding Author:
- Shuting Bai, MD, PhD
Department of Pathology
New York University Langone Medical Center, USA
Tel: 212-263-0956
Fax: 212-263-7916
Email: Shuting.bai@nyumc.org
Received date: July 18, 2014; Accepted date: September 09, 2014; Published date: September 12, 2014
Citation: Bai S, Chiriboga L, Heller K, Patel KN, LiVolsi VA (2014) Decalcification does not Affect Immunohistochemical Stain of HBME-1 on Papillary Thyroid Carcinoma. J Clin Exp Pathol 4:188. doi: 10.4172/2161-0681.1000188
Copyright: © 2014 Bai S, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Clinical & Experimental Pathology
Introduction
Thyroid carcinoma is the most common endocrine malignancy and 80% of all thyroid malignancies are papillary thyroid carcinoma [1]. The diagnosis of papillary thyroid carcinoma is based on architectural features combined with nuclear features, including nuclear clearing, overlapping, grooves and pseudoinclusions [2,3]. It is always challenging in our everyday practice to distinguish folicualr variant papillary thyroid carcinoma (FVPTC), one of the subtypes of PTC, from cellular adenomatous nodules. Nuclear clearing in benign thyroid lesion, such as in Hashimoto’s disease may lead pathologists to misdiagnose papillary thyroid carcinoma. In an unusual condition, it may also be difficult for differentiating papillary hyperplastic nodules from papillary thyroid carcinoma.
HBME1 is a monoclonal antibody which was originally developed as a mesothelioma marker and directed against the microvillous surface of mesothelial cells [4]. Subsequently, it was applied to the diagnosis of malignant thyroid conditions. Several studies demonstrated that HBME-1 is a sensitive marker for papillary thyroid carcinoma [5-9].
Calcification of thyroid carcinoma and benign thyroid lesions are common [10-15]. In practice, decalcification process must be performed for surgical pathological slides formation to evaluate the nature of the calcified lesion. Decalcification has been demonstrated to affect the identification of markers by immunohistochemistry [16-18]. More importantly, nuclei of thyroid follicular cells close to calcified areas can appear to have (?) nuclear clearing or even nuclear grooves. As an important marker for diagnosing PTC, the effect of decalcification in HBME-1 staining for papillary thyroid carcinoma has not been elucidated. For this purpose, we performed immnuhistochemical stains for HBME-1 in calcified PTCs by using calcified benign thyroid lesions as controls and concluded that decalcification does not affect HBME-1 stain for PTCs.
Methods
The surgical pathology files from two participating institutions (Tisch Hopsital, New York University Langone Medical Center and the Hospital of University of Pennsylvania) were searched for cases on thyroid resection specimens that contained in the gross description and/or diagnosis with key word “decalcification” from 2008 to 2012. Twenty-six cases were recruited, including seventeen cases of papillary thyroid carcinoma, eight cases of nodular hyperplasia, and one case of follicular carcinoma. Hematoxylin and eosin slides from all cases were reviewed to confirm the diagnosis. Clinical information was obtained by reviewing the charts.
Immunohistochemical stain for HBME-1 was performed for all the cases:
Immunohistochemistry was performed on 4 micron formalin fixed, paraffin embedded papillary thyroid carcinomas using mouse anti-human mesothelial cell, tissue culture supernatant clone HBME-1 (Dako Carpentaria, CA USA). In brief, sections were deparaffinized in xylene (3 changes), rehydrated through graded alcohols (3 changes 100% ethanol, 3 changes 95% ethanol) and rinsed in distilled water. Heat induced epitope retrieval was performed in a 1200-Watt microwave oven at 100% power in 10 mM sodium citrate buffer, pH 6.0 for 10 minutes. Sections were allowed to cool for 30 minutes and then rinsed in distilled water. Antibody incubation and detection were carried out at 40°C on a NexES instrument (Ventana Medical Systems Tucson, Arizona USA) using Ventana’s reagent buffer and detection kits unless otherwise noted. Endogenous peroxidase activity was blocked with hydrogen peroxide. Anti-HBME-1 was diluted 1:100 in Dulbecco’s Phosphate Buffered Saline, (Life Technologies Grand Island, New York USA) and incubated overnight at room temperature. Primary antibody was detected with iView biotinylated goat anti-mouse followed by application of streptavidin-horseradish-peroxidase conjugate. The complex was visualized with 3,3-diaminobenzidene and enhanced with copper sulfate. Slides were washed in distilled water, counterstained with hematoxylin, dehydrated and mounted with permanent media. Appropriate positive and negative controls were included with the study sections.
Results
Most papillary thyroid carcinomas with calcification stain for HBME-1:
With appropriate controls seventeen papillary thyroid carcinoma with calcification were stained with HBME-1. Sixteen cases were positive for membraneous staining of the tumor cells with this antibody except for one case that was negative. Interestingly, noncalcified carcinoma blocks were available for six PTC cases. Five positive cases showed positive labeling for HBME-1 in the noncalcified carcinoma. The noncalcified carcinoma from the negative case was negative.
All non-papillary thyroid carcinoma cases are negative for HBME-1 staining:
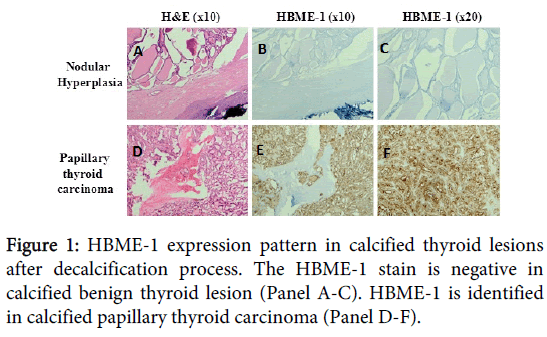
Eight cases of calcified nodular goitre and one case of follicular carcinoma were stained with HBME-1 by using the same condition of PTC in this study. All these non-PTC cases were negative for HBME-1 staining (Figure 1).
Discussion
Papillary thyroid carcinoma is the most common thyroid malignant tumors [1]. Calcification within the thyroid gland is a common finding both on thyroid imaging and thyroid histopathologic findings. Several reports in the literature have noted that calcification seems to be more common in malignant thyroid nodules than benign thyroid nodules [12-14]. Most of the calcified benign thyroid lesion was in multinodular goiters [14].
The use of immunohistochemical markers, such as HBME-1, CK19, CD15, and Galectin 3, has been proven in many histological studies to distinguish PTC from its mimics [5,7,19-21]. HBME-1 was noted as one of the most sensitive and specific markers for PTCs [7,8].
For severely calcified thyroid lesions, decalcification has to be performed to evaluate the nature of the lesion. Decalcification of the tissue has variable effects on immunohistochemical stains [19-21]. To elucidate the effect of decalcification on HBME-1 staining on PTCs and its mimics, we searched surgical pathological cases in two institutions and identified sixteen calcified PTCs, one calcified follicular carcinoma, and eight cases of thyroid multinodular hyperplasia.
All cases were stained for HBME-1 immunohistochemically on decalcified samples. All PTC cases were positive for HBME-1 labeling except one case. Interestingly, noncalcified carcinoma samples were available for six PTC cases. Five positive cases showed positive labeling for HBME-1 in the noncalcified carcinoma. The noncalcified carcinoma from the negative case was negative. All benign thyroid lesions and the case of follicular carcinoma were negative for HBME-1 staining. These results indicate decalcification does not have significant effect on immunohistochemical staining of HBME-1 for thyroid lesions. HBME-1 stain can be used in practice to distinguish difficult calcified cases between papillary thyroid carcinoma and benign thyroid lesions.
References
- LiVolsi VA (2011) Papillary thyroid carcinoma: an update. Mod Pathol 24 Suppl 2: S1-9.
- Hapke MR, Dehner LP (1979) The optically clear nucleus. A reliable sign of papillary carcinoma of the thyroid? Am J Surg Pathol 3: 31-38.
- Baloch ZW, LiVolsi VA, Asa SL, Rosai J, Merino MJ, et al. (2008) Diagnostic terminology and morphologic criteria for cytologic diagnosis of thyroid lesions: a synopsis of the National Cancer Institute Thyroid Fine-Needle Aspiration State of the Science Conference. Diagn Cytopathol 36: 425-437.
- Mase T, Funahashi H, Koshikawa T, Imai T, Nara Y, et al. (2003) HBME-1 immunostaining in thyroid tumors especially in follicular neoplasm. Endocr J 50: 173-177.
- Cheung CC, Ezzat S, Freeman JL, Rosen IB, Asa SL (2001) Immunohistochemical diagnosis of papillary thyroid carcinoma. Mod Pathol 14: 338-342.
- Papotti M, Rodriguez J, De Pompa R, Bartolazzi A, Rosai J (2005) Galectin-3 and HBME-1 expression in well-differentiated thyroid tumors with follicular architecture of uncertain malignant potential. Mod Pathol 18: 541-546.
- Nasr MR, Mukhopadhyay S, Zhang S, Katzenstein AL (2006) Immunohistochemical markers in diagnosis of papillary thyroid carcinoma: Utility of HBME1 combined with CK19 immunostaining. Mod Pathol 19: 1631-1637.
- Scognamiglio T, Hyjek E, Kao J, Chen YT (2006) Diagnostic usefulness of HBME1, galectin-3, CK19, and CITED1 and evaluation of their expression in encapsulated lesions with questionable features of papillary thyroid carcinoma. Am J Clin Pathol 126: 700-708.
- Fischer S, Asa SL (2008) Application of immunohistochemistry to thyroid neoplasms. Arch Pathol Lab Med 132: 359-372.
- Komolafe F (1981) Radiological patterns and significance of thyroid calcification. Clin Radiol 32: 571-575.
- Katz JF, Kane RA, Reyes J, Clarke MP, Hill TC (1984) Thyroid nodules: sonographic-pathologic correlation. Radiology 151: 741-745.
- Hayashi N, Tamaki N, Yamamoto K, Senda M, Yonekura Y, et al. (1986) Real-time ultrasonography of thyroid nodules. Acta Radiol Diagn (Stockh) 27: 403-408.
- Watters DA, Ahuja AT, Evans RM, Chick W, King WW, et al. (1992) Role of ultrasound in the management of thyroid nodules. Am J Surg 164: 654-657.
- Khoo ML, Asa SL, Witterick IJ, Freeman JL (2002) Thyroid calcification and its association with thyroid carcinoma. Head Neck 24: 651-655.
- Yoon DY, Lee JW, Chang SK, Choi CS, Yun EJ, et al. (2007) Peripheral calcification in thyroid nodules: ultrasonographic features and prediction of malignancy. J Ultrasound Med 26: 1349-1355.
- Matthews JB (1982) Influence of decalcification on immunohistochemical staining of formalin-fixed paraffin-embedded tissue. J Clin Pathol 35: 1392-1394.
- Mullink H, Henzen-Logmans SC, Tadema TM, Mol JJ, Meijer CJ (1985) Influence of fixation and decalcification on the immunohistochemical staining of cell-specific markers in paraffin-embedded human bone biopsies. J Histochem Cytochem 33: 1103-1109.
- Mukai K, Yoshimura S, Anzai M (1986) Effects of decalcification on immunoperoxidase staining. Am J Surg Pathol 10: 413-419.
- Miettinen M, Kärkkäinen P (1996) Differential reactivity of HBME-1 and CD15 antibodies in benign and malignant thyroid tumours. Preferential reactivity with malignant tumours. Virchows Arch 429: 213-219.
- Sack MJ, Astengo-Osuna C, Lin BT, Battifora H, LiVolsi VA (1997) HBME-1 immunostaining in thyroid fine-needle aspirations: a useful marker in the diagnosis of carcinoma. Mod Pathol 10: 668-674.
- Prasad ML, Huang Y, Pellegata NS, de la Chapelle A, Kloos RT (2004) Hashimoto's thyroiditis with papillary thyroid carcinoma (PTC)-like nuclear alterations express molecular markers of PTC. Histopathology 45: 39-46.
Relevant Topics
Recommended Journals
Article Tools
Article Usage
- Total views: 14471
- [From(publication date):
November-2014 - Dec 19, 2024] - Breakdown by view type
- HTML page views : 10046
- PDF downloads : 4425