De Bukes Syndrome - Tetrology of Fallot with Absent Left Pulmonary Artery
Received: 25-Jan-2016 / Accepted Date: 26-Feb-2016 / Published Date: 03-Jan-1970
Abstract
De Bucket syndrome - TOF with unilateral absence of a pulmonary artery (UAPA) is a rare condition with an estimated prevalence of 1 in 200,000 young adults. Most commonly, UAPA occurs in conjunction with cardiovascular abnormalities such as tetralogy of Fallot (TOF) coarctation of the aorta, VSD, subvalvular aortic stenosis, transposition of the great arteries (plus VSD or pulmonary stenosis), Taussig-Bing malformation and coarctation, congenitally corrected transposition and pulmonary stenosis, scimitar syndrome. Patients with isolated UAPA can remain asymptomatic into late adulthood but usually report symptoms such as dyspnea or chest pain or suffer from hemoptysis or recurrent infections. Diagnosis can be difficult due to the rarity of the condition and its nonspecific presentation. We present a case of a 5month old child who presented with TOF with Right pulmonary artery stenosis and absent left pulmonary artery, with typical findings on chest radiograph, angiographic features and treatment discussed.
Keywords: Tetrology of fallot; Right pulmonary artery; Left pulmonary artery; Balloon dilatation
77960Introduction
De Buckes syndrome – TOF with unilateral absence of a pulmonary artery (UAPA) is a rare condition with an estimated prevalence of 1 in 200,000 young adults [1]. Most commonly, UAPA occurs in conjunction with cardiovascular abnormalities such as tetralogy of Fallot (TOF) coarctation of the aorta, VSD, subvalvular aortic stenosis, transposition of the great arteries (plus VSD or pulmonary stenosis), Taussig-Bing malformation and coarctation, congenitally corrected transposition and pulmonary stenosis, scimitar syndrome. Patients with isolated UAPA can remain asymptomatic into late adulthood but usually report symptoms such as dyspnea or chest pain or suffer from hemoptysis or recurrent infections. Diagnosis can be difficult due to the rarity of the condition and its nonspecific presentation [2]. We present a case of a 5month old child who presented with TOF with Right pulmonary artery stenosis and absent left pulmonary artery, with typical findings on chest radiograph, angiographic features and treatment discussed.
Case Report
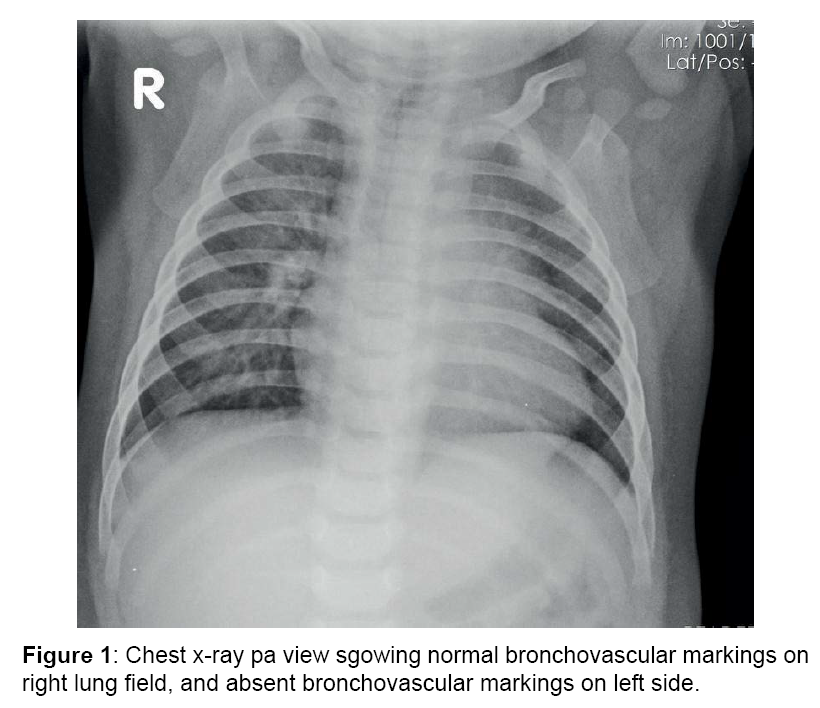
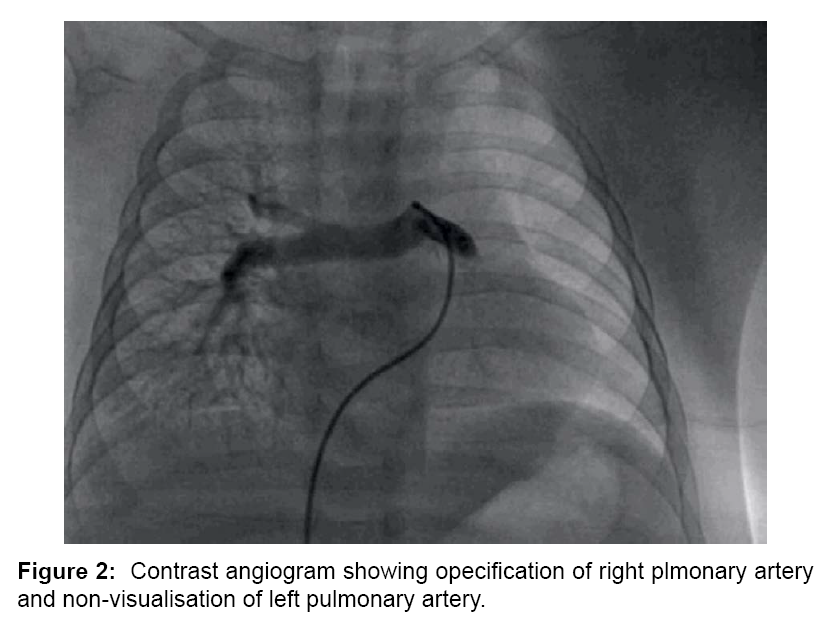
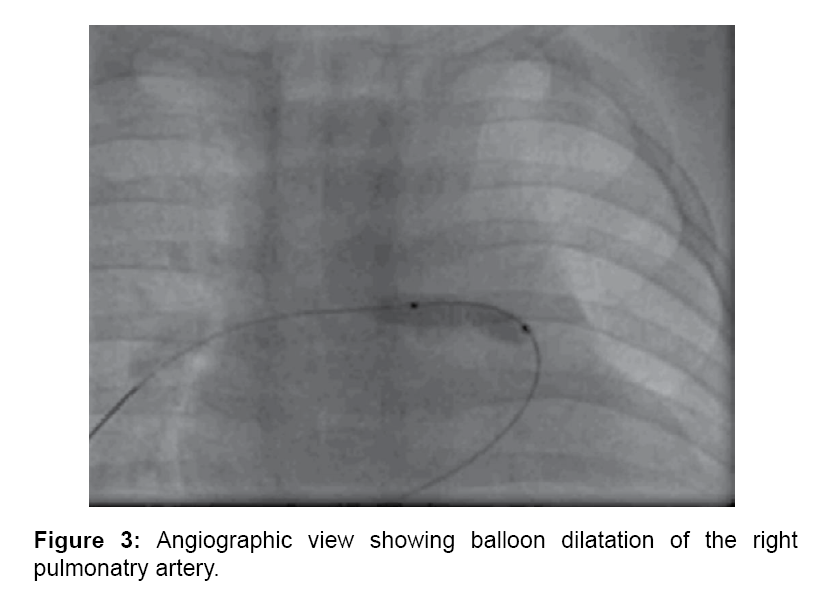
A five months old male child was referred to Sri Jayadeva Institute of Cardiovascular Science and research for cardiac evaluation. He was born to non-consanginous parents with normal pregnancy and normal delivery. He presented with history of incessant feeding and cyanosis while feeding and crying. On physical examination, the patient had cyanosis with SpO2 of 67%. There was no respiratory distress at rest. His weight was 3 kgs (just below the 5th percentile for his age). Heart rate was 104 beats/minute and blood pressure was 100/55 mmHg. Cardiovascular examination revealed normal peripheral pulses, the second heart sound was single and Grade 3/6 Ejection systolic murmer. The electrocardiogram showed sinus rhythm, right axis deviation and right ventricular (RV) hypertrophy. Chest X-ray (Figure 1) showed mild cardiomegaly, with normal bronchovascular markings on right side and absent bronchovascular markings on left side. A 2-dimensional echocardiography and Doppler study confirmed the diagnoses of TOF with right pulmonary artery stenosis and non-vislaisation of left pulmonary artery, peak systolic gradient of 70 mmHg across the RV outflow tract (RVOT). The aortic arch was left sided and no patent ductus arteriosus was seen. At cardiac catheterization, RV systolic pressure was at systemic level and there was a peak systolic gradient of 77 mmHg across RVOT. The main PA pressure was 23/10 mmHg. The pulmonary flow to systemic flow (Qp/Qs) was 0.83. The catheter could not enter the site of LPA. PA angiography failed to show a LPA (Figure 2). Angiography following pulmonary vein wedge injection in the left lung failed to show LPA, confirming its absence. Aortography failed to show a patent ductus arteriosus, collaterals supplying the distal segment of LPA or anomalous origin of the LPA. The diagnosis of TOF with right pulmonary artery stenosis and absent LPA was established. Since the child was symptomatic, pulmonary artery balloon dilatation of right pulmonary artery (Figure 3) was done which decreased the gradient across the RVOT with temperory relief of symptoms. The child was later referred to cardiothoracic surgeon for definitive intracardiac repair.
Discussion
UAPA is a rare condition, with an estimated prevalence of 1 in 200,000 young adults [3]. Most commonly, UAPA occurs in conjunction with cardiovascular abnormalities such as tetralogy of Fallot or cardiac septal defects, but it can also occur in an isolated manner [3,4]. Isolated UAPA involves the right lung in about two thirds of cases [1]. Due to embryologic relationships, UAPA commonly occurs on the side of the chest opposite the aortic arch (although that was not the case in our patient) [5]. The exact embryologic cause of UAPA is a matter of debate and is likely different in left- vs. right-sided UAPA. In both cases, however, altered development of a sixth aortic arch segment is thought to result in a ductal origin to a pulmonary artery that leads to the proximal interruption of that vessel when the ductal tissue regresses at the time of birth [5]. Distal intrapulmonary branches of the affected artery usually remain intact and can be supplied by collateral vessels from bronchial, intercostal, internal mammary, subdiaphragmatic, subclavian, or even coronary arteries [6,7]. Patients with isolated UAPA can present in a variety of ways. A 2002 review of 108 cases of UAPA revealed a median age of presentation of 14 years [1]. The combination of chest pain, pleural effusion, and recurrent infections was present in 37% of patients, while dyspnea or exercise intolerance was present in 40% of patients. Pulmonary hypertension was found in 44% of patients that were tested for the disorder. Hemoptysis occurred in about 20% of patients, and high-altitude pulmonary edema was seen in approximately 10% of patients [1]. Seven deaths were noted in the case series and included mortality from massive pulmonary hemorrhage, right heart failure, respiratory failure, pulmonary hypertension, and high-altitude pulmonary edema. Only 14 of 108 patients with isolated UAPA were asymptomatic at the time of their diagnosis and throughout variable followup [1]. In addition, poor blood flow to the affected lung may result in alveolar hypocapnia, leading to secondary bronchoconstriction and mucous trapping [6]. Chronic infection can lead to bronchiectasis in some patients [2,6]. Hemoptysis is a potentially serious complication of UAPA. Hemoptysis appears to be caused by large collateral circulations that subject venous systems to unusually high pressures. While hemoptysis can be chronic and self-limited, cases of massive hemoptysis have been reported in the literature [6-8].
Diagnosing UAPA can be difficult, but important clues are present in chest radiographs. The chest radiograph of patients with UAPA typically shows asymmetric lung fields, with an ipsilateral small hemithorax holding a hyperlucent lung [2,3]. When suspicious findings are noted on a chest radiograph, the diagnosis of UAPA can be definitively made by CT, magnetic resonance imaging (MRI), or transthoracic echocardiogram. On cross-sectional imaging, the absent pulmonary artery will typically terminate within 1 cm of its expected origin from the main pulmonary artery [3]. Other findings that may be noted on CT or MRI include intact peripheral branches of the pulmonary artery, variable collateral circulation, mosaic parenchymal changes, and bronchiectasis secondary to recurrent infections [2,3,6].
Transthoracic echocardiogram can also be used to diagnose UAPA and is advantageous because the examiner can look for coexisting cardiac malformations at the same time. Angiography is considered the gold standard for the diagnosis of UAPA but is invasive and typically unnecessary, unless it is being used as a preoperative test for a studying hemodynamic parameters and also for palliative treatment. There is currently no consensus concerning treatment of patients with UAPA. Some authors have recommended using serial echocardiography to monitor asymptomatic adults for the development of pulmonary hypertension [9]. Patients who develop pulmonary hypertension can be treated medically with vasodilator therapy [1,10]. Alternatively, revascularization of peripheral branches of the affected pulmonary artery to the pulmonary hilum can be attempted, and there are reports of successful revascularization procedures, mostly in the pediatric population [2,11-13].
Conclusion
Agenesis of the left pulmonary artery is a rare anomaly and the patient may remain asymptomatic till adulthood. Imaging plays a major role in the diagnosis and detecting the associated findings in heart and lungs. For patients who present with a unilateral small hemithorax, recurrent chest infections and an abnormal chest X-ray, a UAPA anomaly should be considered in the differential diagnosis. An early diagnosis can avert serious complications.
References
- Â Ten Harkel AD, Blom NA, Ottenkamp J (2002)Isolated unilateral absence of a pulmonary artery: a case report and review of the literature. Chest 122: 1471-1477.
- Â Griffin N, Mansfield L, Redmond KC, Dusmet M, Goldstraw P, et al. (2007)Imaging features of isolated unilateral pulmonary artery agenesis presenting in adulthood: a review of four cases. Clin Radiol 62: 238-244.
- Bouros D, Pare P, Panagou P, Tsintiris K, Siafakas N, et al. (1995)Â The varied manifestation of pulmonary artery agenesis in adulthood. Chest 108: 670-676.
- Presbitero P, Bull C, Haworth SG, de Leval MR (1984)Absent or occult pulmonary artery. Br Heart J 52: 178-185.
- Pfefferkorn JR, Löser H, Pech G, Toussaint R, Hilgenberg F, et al. (1982) Absent pulmonary artery. A hint to its embryogenesis. Pediatr Cardiol 3: 283-286.
- Kadir IS, Thekudan J, Dheodar A, Jones MT, Carroll KB, et al. (2002)Congenital unilateral pulmonary artery agenesis and aspergilloma. Ann Thorac Surg 74: 2169-2171.
- Bockeria LA, Makhachev OA, Khiriev TK, Abramyan MA (2011) Congenital isolated unilateral absence of pulmonary artery and variants of collateral blood supply of the ipsilateral lung. Interact Cardiovasc Thorac Surg 12: 509-510.
- Reñé M, Sans J, Dominguez J, Sancho C, Valldeperas J, et al. (1995)Unilateral pulmonary artery agenesis presenting with hemoptysis: treatment by embolization of systemic collaterals. Cardiovasc Intervent Radiol 18: 251-254.
- Bekoe S, Pellegrini RV, DiMarco RF , Grant KJ, Woelfel GF, et al.(1993)Pneumonectomy for unremitting hemoptysis in unilateral absence of pulmonary artery.Ann Thorac Surg 55: 1553-1554.
- Turner DR, Vincent JA, Epstein ML (2000)Isolated right pulmonary artery discontinuity. Images Paediatr Cardiol 4: 24-30.
- Shostak E, Sarwar A (2009) A 50-year-old woman with dyspnea, lower extremity edema, and volume loss of the right hemithorax. Chest 136: 628-632.
- Welch K, Hanley F, Johnston T, Cailes C, Shah MJ, et al.(2005) Isolated unilateral absence of right proximal pulmonary artery: surgical repair and follow-up. Ann Thorac Surg 79: 1399-1402.
- Toews WH, Pappas G (1983)Surgical management of absent right pulmonary artery with associated pulmonary hypertension. Chest 84: 497-499
Citation: Madhu KJ, Kumar S, Vijayalakshmi IB, Chitra Manjunath CN (2016) De Bukes Syndrome - Tetrology of Fallot with Absent Left Pulmonary Artery. Cardiovasc Ther 1: 105.
Copyright: © 2016 Madhu KJ, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Open Access Journals
Article Usage
- Total views: 13985
- [From(publication date): 2-2016 - Dec 22, 2024]
- Breakdown by view type
- HTML page views: 13133
- PDF downloads: 852