Case Report Open Access
Cystic Lymphangioma of the Breast: A Case Report in an Adult Woman
Almohawes E1*, Khoumais N2, Arafah M3, Pant R2 and Al-Bahrani R41Department of Radiology, Security Force Hospital, Dammam, Saudi Arabia
2Department of Radiology, King Faisal Specialist Hospital and Research Center, Riyadh, Saudi Arabia
3Department of Pathology, College of Medicine, King Khalid University Hospital, King Saud University, Riyadh, Saudi Arabia
4Department of Radiology, Dammam Medical Complex, Dammam, Saudi Arabia
- *Corresponding Author:
- Almohawes E
Department of Radiology
Security Force Hospital
Dammam, Saudi Arabia
Tel: 00966505869914
E-mail: dralmohawes@hotmail.com
Received Date: April 04, 2017; Accepted Date: April 17, 2017; Published Date: April 24, 2017
Citation: Almohawes E, Khoumais N, Arafah M, Pant R, Al-Bahrani R (2017) Cystic Lymphangioma of the Breast: A Case Report in an Adult Woman. OMICS J Radiol 6: 259. doi: 10.4172/2167-7964.1000259
Copyright: © 2017 Almohawes E, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Radiology
Abstract
Cystic lymphangioma of the breast is a rare benign condition. We report a case of breast cystic lymphangioma diagnosed in a 39-year-old woman. It showed enlarged right breast with multiple partially circumscribed, high-density round masses on mammography, well-defined anechoic cysts with septa and no solid nodules replacing the whole breast on sonography. This lesion had a location and imaging findings typical of breast cystic lymphangioma.
Keywords
Cystic lymphangioma; Cystic hygroma; Mammography; Ultrasound
Introduction
Cystic lymphangioma, also known as cystic hygroma, is a rare benign congenital malformation of the lymphatic system [1]. It is a vascular malformation rather than a true neoplasm, and this lesion is believed to be the result from failure of the lymphatic system to connect with the venous system [2-4]. Possible etiological factors include Blockage of the lymphatic channels with resultant secondary dilatation, congenital weakness of the lymphatic wall or proliferation of lymphatic vessels [3]. It may be associated with other anatomic and/ or chromosomal abnormalities [1]. More than 90% of cystic hygroma cases are diagnosed by the age of 2 years, in more than 90% of cases the lesion is located in the neck or axilla [1,5].
It is extremely rare to occur in the breast and only few cases have been reported in the literature documenting their radiological appearance [5]. Therefore, we report an additional case with a typical clinical and radiological appearance, confirmed by histopathological analysis.
Case Presentation
A 39 years old woman, not known to have any medical problem, presented with a history of gradual increase in the size of her right breast over duration of 9 years, associated with fullness in the right axilla. Her past medical history is negative.
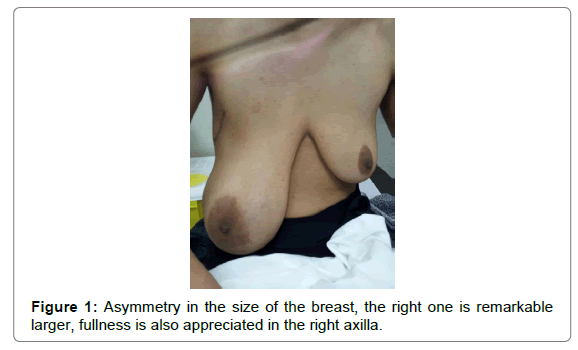
On physical examination, she had a soft non-tender mass replacing the completely right breast and extending to the axilla. No associated nipple retraction or discharge and no changes in skin color (Figure 1).
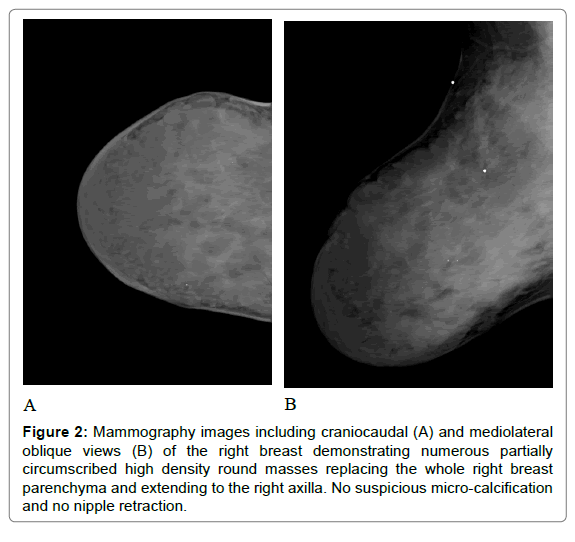
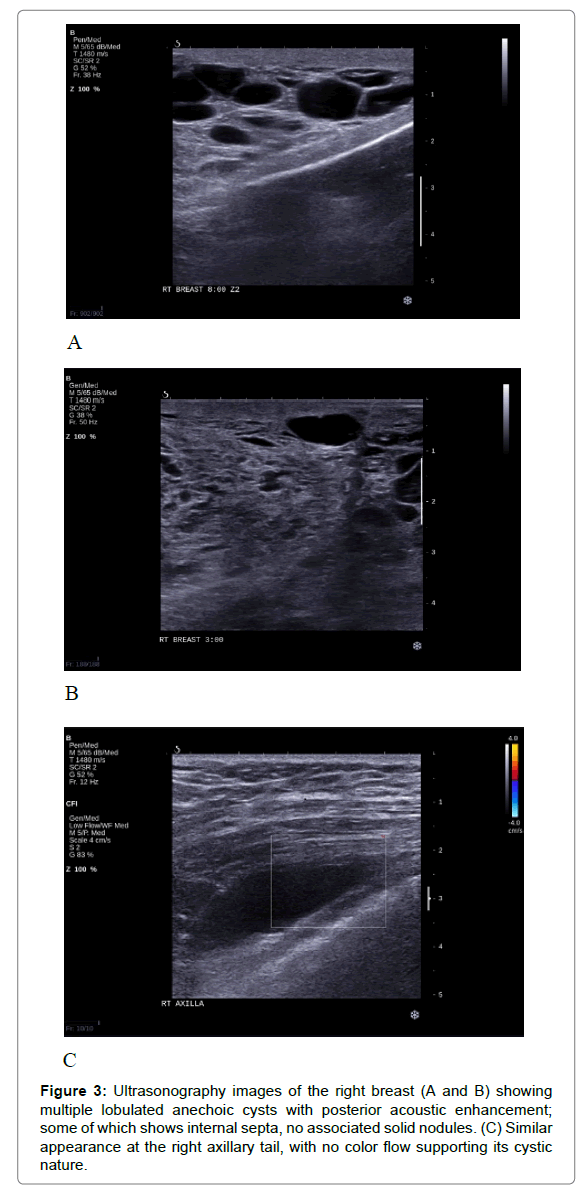
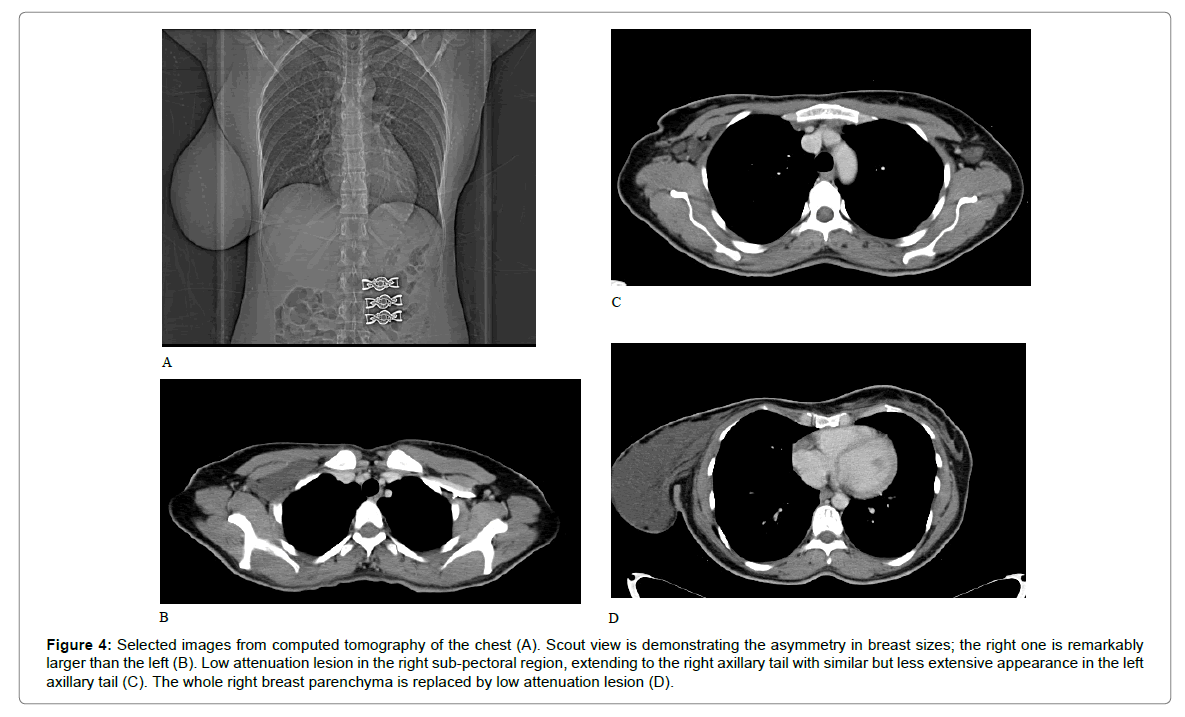
Radiological investigations were performed, including mammogram, ultrasound and CT scan. On mammography, there are numerous partially circumscribed high density round masses involving the completely right breast and extending to the axilla (Figure 2). Focal similar appearance is seen at the contralateral left axillary tail region. Sonography revealed multiple loculated anechoic cysts; some of which shows septa, no associated solid nodules (Figure 3). Complementary CT scan of the chest was performed to assess the full extension of the lesion and showed low attenuation lesion similar to fluid seen in the right sub-pectoral region, extending to the right axillary tail with similar but less extensive appearance in the left axillary tail (Figure 4).
Figure 2: Mammography images including craniocaudal (A) and mediolateral oblique views (B) of the right breast demonstrating numerous partially circumscribed high density round masses replacing the whole right breast parenchyma and extending to the right axilla. No suspicious micro-calcification and no nipple retraction.
Figure 3: Ultrasonography images of the right breast (A and B) showing multiple lobulated anechoic cysts with posterior acoustic enhancement; some of which shows internal septa, no associated solid nodules. (C) Similar appearance at the right axillary tail, with no color flow supporting its cystic nature.
Figure 4: Selected images from computed tomography of the chest (A). Scout view is demonstrating the asymmetry in breast sizes; the right one is remarkably larger than the left (B). Low attenuation lesion in the right sub-pectoral region, extending to the right axillary tail with similar but less extensive appearance in the left axillary tail (C). The whole right breast parenchyma is replaced by low attenuation lesion (D).
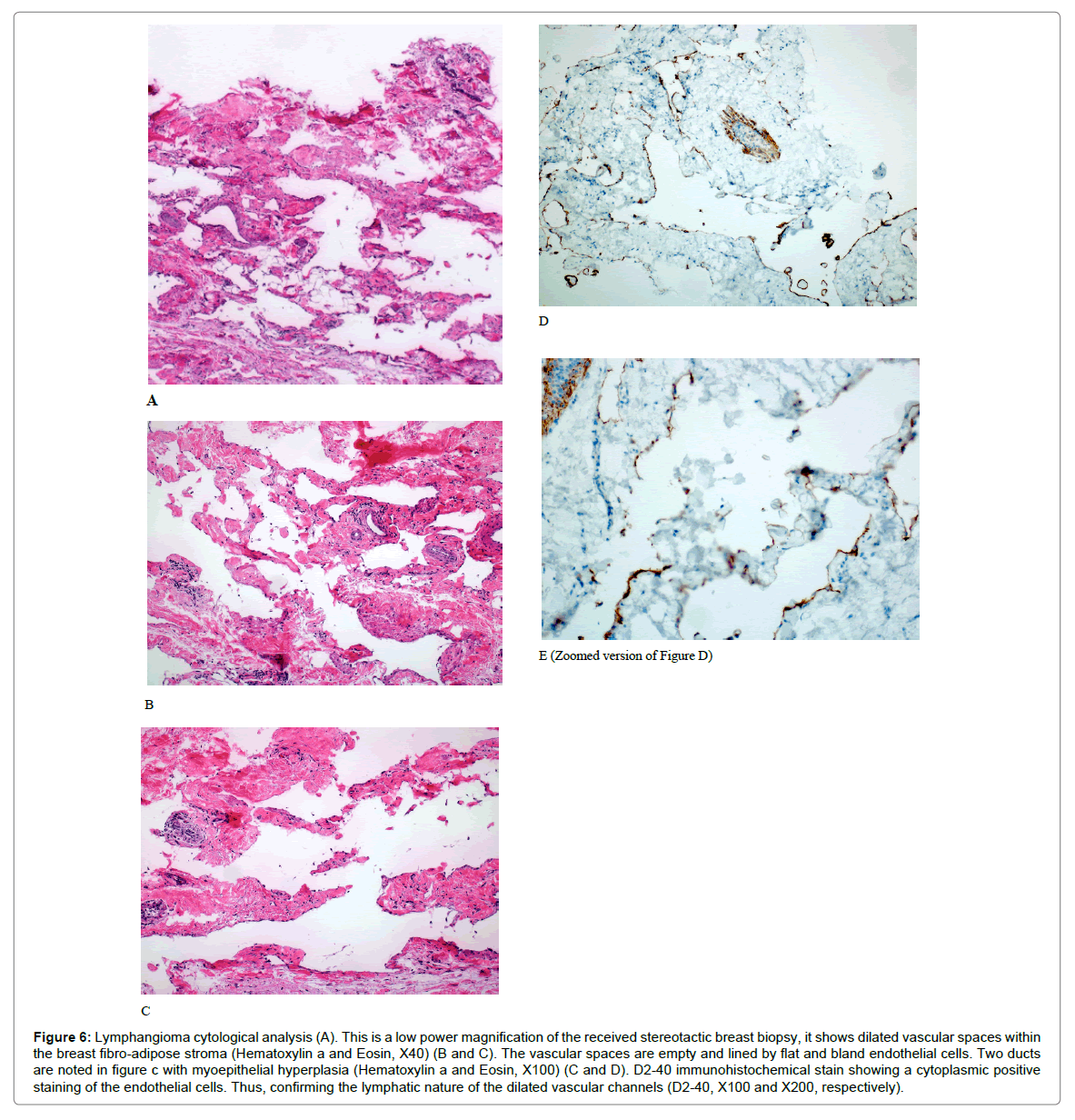
Diagnostic vacuum-assisted biopsy of this right breast mass was performed under sonographic guidance (Figure 5), without total aspiration of the lesion. Cytological examination confirmed the diagnosis of breast lymphangioma (Figure 6).
Figure 6: Lymphangioma cytological analysis (A). This is a low power magnification of the received stereotactic breast biopsy, it shows dilated vascular spaces within the breast fibro-adipose stroma (Hematoxylin a and Eosin, X40) (B and C). The vascular spaces are empty and lined by flat and bland endothelial cells. Two ducts are noted in figure c with myoepithelial hyperplasia (Hematoxylin a and Eosin, X100) (C and D). D2-40 immunohistochemical stain showing a cytoplasmic positive staining of the endothelial cells. Thus, confirming the lymphatic nature of the dilated vascular channels (D2-40, X100 and X200, respectively).
Discussion
Cystic lymphangioma of the breast in an adult woman is extremely rare, only few cases were reported in the literature. Less than 20 cases had been reported in the last 40 years [6-9]. Some authors consider lymphangioma as a true neoplasm that exert local aggressive behavior, but overall it is considered as a benign disease [7]. On the other hand, other authors believe that lymphangioma is a hamartomatous malformation resulting from the inability of the lymphatic system to communicate with the venous system. Another closely related opinion is that lymphangiomas are sequestered lymphatic tissue which had failed to communicate with the lymphatic channels [6,7]. Considering the latter described two opinions, fluid will accumulate in this abnormal lymphatic tissue, resulting in its cystic appearance [6-8]. Lymphangioma is considered mostly as a benign, slow growing disease that usually has low malignancy potential, however, malignant transformation into squamous cell carcinoma after long standing lymphangioma circumscriptum has been reported [9].
Lymphangiomas have been classified into three subtypes: Simple (or capillary), cavernous and cystic lymphangiomas [1,4-7]. Simple lymphangioma consists of several small capillary-sized, thin-walled vessels with an element of connective tissue [1,5]. Cavernous lymphangioma is composed of dilated lymphatic vessels that are surrounded by a fibrous capsule, containing lymphoid aggregates [1,5]. While cystic lymphangioma (cystic hygroma), is characterized by large cystic like spaces filled with clear lymphatic fluid, that is usually lined by flat endothelial cells with well-defined margins [1,4,5]. Cystic lymphangioma does not have capsule and the cystic lumen can be empty or filled with proteinaceous material, lymphocytes or red blood cells [1,4]. However, the distinction between cystic and cavernous lymphangioma is believed to be arbitrary, as both can co-exist in the same lesion, suggesting that a lymphangioma cyst is merely a cavernous lymphangioma of long duration, in which the cavernous spaces are large [6,7].
Considering the proposed etiology for this disease, resulting in failure of communication with the main central lymphatic ducts; explaining their tendency to occur along the lymphatic drainage routes, being directed towards the axilla [2,5,7]. Such localized lesions in the breast are usually located in the upper outer quadrant, tail of Spence or sub-areolar space [5]. However, one case report documented a rare histologically proven cystic lymphangioma in the upper inner quadrant of the breast [9]. Secondary lymphangioma developing post mastectomy and irradiation of the chest wall has been described [10,11].
The previously documented cases of breast lymphangioma in the literature showed variable sizes that range from 3 to 25 cm [7]. Lymphangioma can be diffuse and/or multi-centric (lymphangiomatosis) [1]. They can be located in the soft tissues only, or can extend to involve other locations like the bone and the viscera [1]. Around 70% of lymphangiomas occur in the neck region, 20% in the axilla, while the remaining 10% is reported in the abdominal organs, retro peritoneum, skeleton, scrotum and, very rarely, in the breast [1,7].
Lymphangioma is usually an asymptomatic smooth mass. However, rapid expansion can occur because of hemorrhage into the cyst, inflammation or trauma. Patients usually present clinically with rapidly enlarging mass that show no other local alterations. Physical examination and palpation would reveal a well-defined, painless, smooth and mobile mass [1].
Investigation is performed using radiological examinations, including mammogram, ultrasound and other cross sectional imaging if needed. On mammography, breast cystic lymphangioma show round-shaped or lobulated densities [2]. However, the mammographic findings are non-specific as many of the cases occur high in the axilla, rendering its visualization on mammogram difficult. While on sonography, it appears as a multiloculated cystic mass with variable sized septations that contain solid components arising from the cyst wall or septa [2,10]. Some authors suggest that when the lymphatic ducts in cases of lymphangioma are prominent on ultrasound, appearance can resemble duct ectasia in an accessory breast tissue, however, upon compression by the transducer, lymphatic ducts in lymphangioma will be totally collapsed while it will not be affected by compression in cases of duct ectasia related to accessory breast. In one case report, cavernous lymphangioma showed complex echoic speculated mass, mimicking malignancy, Ko et al. attributed the appearance to the tiny size of the lymphatic ducts being closely related to each other giving an appearance of a solid mass, with surrounding fibrosis and prominent fibro-collagenous stroma giving the speculated appearance [8,10].
Magnetic Resonance Imaging (MRI) is proposed to be the best modality for the diagnosis and evaluation of lymphangioma extension [8]. Cystic lymphangioma appear as multiseptated masses on MRI, usually following the signal intensity of fluid, showing low signal intensity on T1 and high signal intensity on T2, with enhancement of the septa. However, appearance of the cystic fluid content can be variable depending on the presence of hemorrhage or high proteinaceous material.
Differential diagnosis of breast lymphangioma includes simple cysts, post-surgical collection, hematoma, lymphocele, abscess and hemangioma [1].
The usual characteristic location of lymphangioma, its large size and painless progressive course helps to suggests the diagnosis and differentiate it from other differentials, however, since the radiological images does not always provide sufficient information, histopathological diagnosis by Fine Needle Aspiration (FNA) remains the mainstay of diagnosis in some cases [1].
FNA fluid aspirates will show clear, yellowish, or straw-colored fluid, with plenty of lymphocytes. However, these specimens are rarely cellular and FNA is usually not diagnostic, since it cannot evaluate the architecture of these lesions. Therefore, surgical excision with histopathological diagnosis remains the mainstay of diagnosis [9].
Primary treatment of lymphangioma is complete surgical excision. Ensuring safe margins is important to prevent recurrence; however, obtaining safe margins can be difficult because of its tendency to infiltrate the surrounding soft tissues. Recurrence probability is low if total excision s performed. Other options include percutaneous sclerosis or a combination of surgical excision and percutaneous sclerosis [8].
Conclusion
In conclusion, we presented a rare case of breast lymphangioma disease is even more rare in adults, as seen in our case. Clinical history, typical location and radiological appearance help in guiding to the correct diagnosis, however, FNA, histopathological analysis remains the mainstay of diagnosis in most cases, and the primary treatment is surgical with a high probability of recurrence if the safe margins are not removed.
References
- Torcasio A, Veneroso S, Amabile MI, Biffoni M, Martino G, et al. (2006) Cystic hygroma of the breast: A rare lesion. Tumori 92: 347.
- Chung SY, Oh KK, Kim DJ (2003) Mammographic and sonographic findings of a breast cystic lymphangioma. J Ultrasound Med 22: 307-309.
- Waqar SN, Khan H, Mekan SF, Kayani N, Raja AJ (2004) Cystic breast lymphangioma. J Pak Med Assoc 54: 531-533.
- Jang KWMSH, Jang WNSM, Jang YJJKS, Paik SS (2008) Cystic lymphangioma of the breast in an adult woman. Korean J Pathol 2008; 42: 244-246.
- Balaji R, Ramachandran K (2010) Cystic lymphangioma of the breast: magnetic resonance imaging features. Breast Care 5: 250-252.
- Vargas-Hernández VM, Tovar-Rodríguez JM, Moreno-Eutiio MA, Acosta-Altamirano G (2014) Giant cystic lymphangioma of the breast: Report of a case with 20-year follow-up and review of the literature. Circulation 82: 81-86.
- Ogun GO, Oyetunde O, Akang E (2007) Cavernous lymphangioma of the breast. World J Surg Oncol 5: 69.
- Ko KH, Kim EK, Kang HY, Youk JH (2009) Cavernous lymphangiomas of the breast mimicking breast cancer. J Ultrasound Med 28: 973-976.
- Rusdianto E, Murray M, Davis J, Caveny A (2016) Adult cystic lymphangioma in the inner quadrant of the breast-Rare location for a rare disease: A case report. Int J Surg Case Rep 20: 123-126.
- Hahn SY, Choi HY, Park SH, Jang J (2011) Lymphangioma and lymphangiectasia of the breast mimicking inflammatory breast cancer. J Ultrasound Med 30: 863-865.
- Krainick-Strobel U, Krämer B, Walz-Mattmüller R, Kaiserling E, Röhm C, et al. (2006) Massive cavernous lymphangioma of the breast and thoracic wall: Case report and literature review. Lymphology 39: 147-151.
Relevant Topics
- Abdominal Radiology
- AI in Radiology
- Breast Imaging
- Cardiovascular Radiology
- Chest Radiology
- Clinical Radiology
- CT Imaging
- Diagnostic Radiology
- Emergency Radiology
- Fluoroscopy Radiology
- General Radiology
- Genitourinary Radiology
- Interventional Radiology Techniques
- Mammography
- Minimal Invasive surgery
- Musculoskeletal Radiology
- Neuroradiology
- Neuroradiology Advances
- Oral and Maxillofacial Radiology
- Radiography
- Radiology Imaging
- Surgical Radiology
- Tele Radiology
- Therapeutic Radiology
Recommended Journals
Article Tools
Article Usage
- Total views: 5718
- [From(publication date):
April-2017 - Mar 29, 2025] - Breakdown by view type
- HTML page views : 4848
- PDF downloads : 870