Cutaneous Lupus Lesions with Squamous Cell Carcinoma: Diligence in Interpretation
Received: 29-Jun-2021 / Accepted Date: 13-Jul-2021 / Published Date: 20-Jul-2021
Abstract
Discoid Lupus Erythematosus (DLE) is the most common subtype of Cutaneous Lupus Erythematosus (CLE). There are two types of Discoid LE Hypertrophic and Atrophic type. Malignant transformation of Discoid LE is few and far between.
The first case study is a 35-year-old female, known case of Systemic Lupus Erythematosus (SLE) with seizure and polyarthritis presented with an ulcer over the lip for 8 months. Edge wedge biopsy of the lesion was done, and a diagnosis of hypertrophic lupus erythematosus was rendered. The second case report is about A 50-year-old female with a hypopigmented patch measuring 8 × 4 cm present with a raised warty like lesion with black discoloration measuring 3 × 3 cm present over the patch over the right shoulder. Punch biopsy was diagnosed as Discoid lupus erythematosus. Microscopy of wide local excision however turned out to be squamous cell carcinoma in a background of DLE in both the patients.
We report two cases of Lupus Erythematosus which is associated with squamous cell carcinoma in the same lesion and the need of careful diligence whilst reporting the diagnosis.
Keywords: Squamous cell carcinoma; Discoid lupus erythematosus; Pseudoepitheliomatous hyperplasia
Introduction
Lupus Erythematosus is a disease with clinical features ranging from an isolated cutaneous eruption to fatal systemic illness. Cutaneous forms of lupus erythematosus represent an important subcategory of the diseases as they occur two to three times more commonly than systemic lupus and hence represent an important subcategory of the disease.
Cutaneous lupus erythematosus can be divided into chronic or discoid, acute, or systemic, and subacute forms. Discoid Lupus Erythematosus (DLE) is one of the most common cutaneous manifestations of SLE. Recent population-based studies estimates that it occurs in approximately 12.4% to 15.0% of incident SLE cases and in approximately 16.6% to 24.3% of prevalent cases with male: female ratio is 1:3 [1]. Malignant transformation is a rare complication of this condition. Incidence of SCC over DLE in the Indian population is found to be 0.98% to 3.4% with a male-to-female ratio of 1.6:1 [2].
We report two cases of Squamous Cell Carcinoma (SCC) developing over lesions of disseminated DLE. The scarcity of reports of this complication in literature as well as its overlapping histological features and different treatment protocol validates the need for this case report.
Case Presentation
Case report-1
A 35-year-old female, known case of SLE with seizure and polyarthritis presented with an ulcer over the lip for 8 months.
On examination, a single ulceroproliferative lesion with well-defined margins over the lower lip which was hard in consistency was present. Floor of the ulcer was indurated with congested buccal mucosa.
Erythrocyte sedimentation rate was normal. A steady decline in gamma glutamyl transferase was observed on follow up showing the regressive pattern with previous corticosteroid therapy.
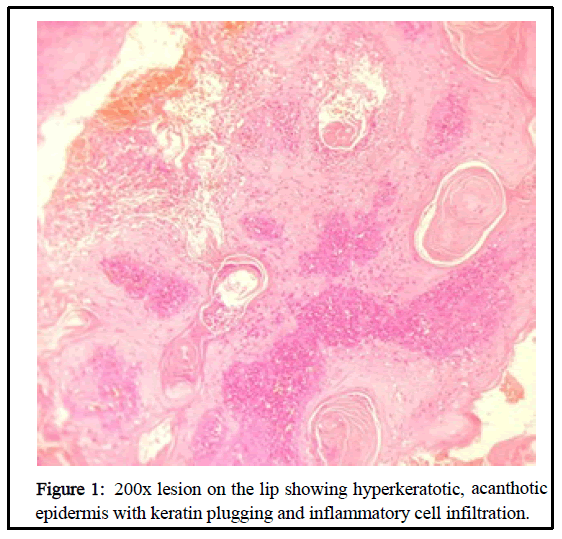
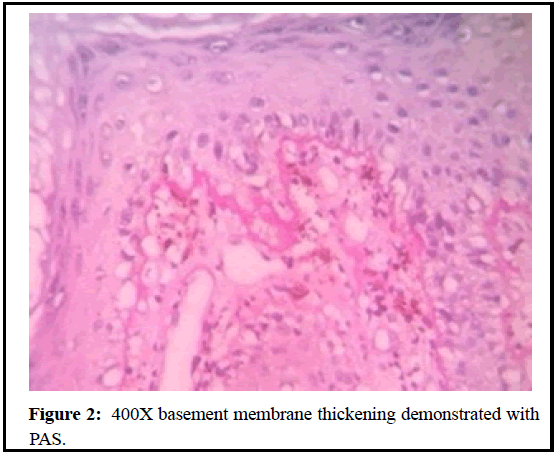
Edge wedge biopsy of the lesion was done and sent for HPE. Biopsy revealed a hyperplastic, hyperkeratotic and papillomatous epidermis and follicular plugging overlying fibro collagenous dermis was observed in Figure 1. Superficial dermis and epidermo-dermal junction showed lympho plasmocytic infiltrate admixed with pigment laden cells. PAS was done and basement membrane thickening was observed in Figure 2.
Based on these features, a diagnosis of hypertrophic lupus erythematosus was rendered, and excision of the lesion was recommended.
Excision biopsy specimen of the resected ulcerated growth from the lower lip on the mucocutaneous junction measuring 1.5 × 1 cm, along with a whitish nodule measuring 0.5 cm in diameter at the base was also sent for histopathological examination.
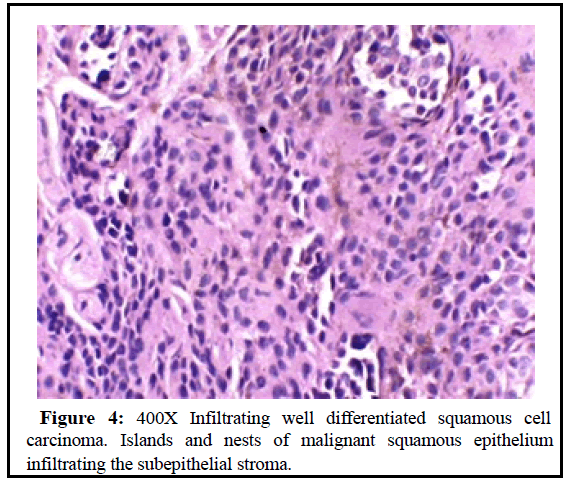
Histopathology revealed hyperkeratotic, parakeratotic, acanthotic and papillomatous stratified squamous epithelium with irregular down growth enclosing cellular keratin pearls with tiny islands and nests of squamous cells infiltrating the subepithelial stroma. A dense lymphoplasmacytic infiltrate surrounded the tumor islands. Some of the islands showed hyperchromatic, pleomorphic nuclei and mitotic figures.
Based on these features a diagnosis of infiltrating well differentiated squamous cell carcinoma was made.
Case report-2
A 50-year-old female came with complaints of discoloration over right shoulder for 2 years which started as a small patch and progressed to attain a size of 8 × 4 cm. The lesion was associated with pain for one week. Similar lesion was present over the lip 4 years back for which the patient had underwent excision.
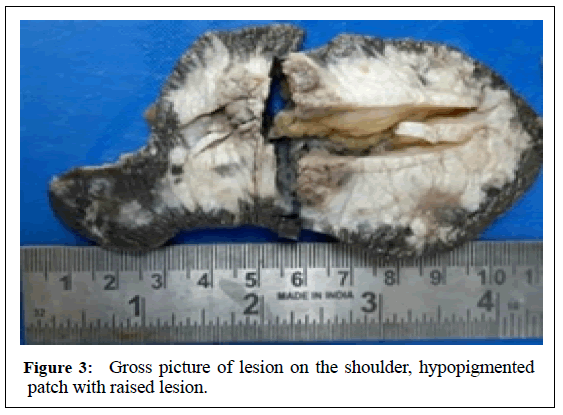
On local examination, a hypopigmented patch measuring 8 × 4 cm was present over the right shoulder with a raised warty like lesion with black discoloration measuring 3 × 3 cm present over the patch was observed in Figure 3.
Punch biopsy was done and sent for HPE. Histopathology showed hyperkeratotic, focally parakeratotic and acanthotic epidermis with irregular down growth overlying dense inflammatory cell infiltration in the dermo-epidermal junction. There was basal cell vacuolar degeneration and tiny islands of squamous epithelium extending into dermis.
Deeper sections showed follicular plugging, squamatization of basal layer, civatte bodies with lymphoplasmacytic infiltrate in the superficial dermis, mid dermis and surrounding adnexal structures. Hence, we reported the diagnosis as Discoid lupus erythematosus.
Excision of the discolored patch with nodular growth was done and was submitted for suspicion of Squamous cell carcinoma and margins clearance. Frozen section was done to look for invasion in the margins of the tumor to give appropriate clearance.
Wide local excision was done and 12 × 6 × 1.5 cm of skin with subcutaneous and raised lesion 5 × 3.5 cm with 4.2 cm from posterior margin, 5 cm from anterior margin, 0.8 cm from medial margin, 0.5 cm from deep resected margin and 0.5 cm from lateral margin clearance.
On microscopy, tumor with lateral and medial margins showed hyperkeratotic, acanthotic and papillomatous epidermis with irregular down growth enclosing keratin cysts overlying islands and nests of malignant squamous epithelium infiltrating the subepithelial stroma, up to the subcutaneous fat. Dense inflammatory cell infiltrate was seen surrounding the tumor islands was observed in Figure 4.
Anterior, posterior, and deep resected margins were free of tumor. Lateral resected margin from the tumor showed tiny fragments of tumor in the fibro collagenous dermis. Medial resected margin from the tumor showed hyperplastic stratified squamous epithelium with dysplastic changes overlying fibro collagenous dermis.
The final diagnosis was given as infiltrating well differentiated squamous cell carcinoma confirming the findings of frozen section.
Results and Discussion
Squamous cell carcinomas arising in chronic lupus are rarely reported. We are reporting two cases of squamous cell carcinoma (SCC) developing over lesions of DLE which could not be confirmed by small incisional biopsy due to several overlap of features which simulate each other and caused dilemma in establishing the diagnosis of the presence of SCC to initiate appropriate surgical and medical therapy. The paucity of the cases of this complication in literature necessitates its mention.
Characteristic lesions of DLE consist of well demarcated, erythematous slightly infiltrated discoid plaques. Early and active DLE lesions usually display surrounding erythema; old lesions often appear atrophic epidermis or epidermal hyperplasia. Occasionally, lesions may show verrucous epidermal hyperplasia especially at their periphery. In our case study, one patient had a verrucous lesion in the lip, and another had a large, discolored patch in right side of neck with a well-defined verrucous lesion present within it.
The characteristic microscopic DLE changes are Hyperkeratosis, acanthosis and degeneration of basal layer, apoptotic keratinocytes and marked thickening of Basement membrane. In well-established lesions marked follicular plugging and dense interface infiltrates of lymphocytes and plasma cells extending into perifollicular zones is characteristic. Pseudoepitheliomatous hyperplasia may also be present to complicate the picture more in some instances.
Genetic deficiencies of the complement components including C2, C3, C4 and C5 as well as the C1 esterase inhibitor are associated with DLE. This can be demonstrated by Immunoflorescent studies.
Hypertrophic DLE mimics squamous cell carcinoma frequently [3,4]. SCC followed by Basal Cell Carcinoma (BCC) is the most worrisome complications of chronic cutaneous lupus erythematosus (CCLE). The incidence was found to be 3.3% among 120 white patients with CCLE [5].
Squamous cell carcinoma is a malignant neoplasm arising from epithelial keratinocytes of skin and mucous membrane. Due to mutation in p53 tumor suppressor gene, there will be defect in apoptosis of keratinocytes that have sustained UV-radiation-induced DNA damage which ultimately led to SCC.
The time interval between development of DLE and SCC has varied from four to twenty years [6-8]. Precipitating factors for SCC are age more than 40 years, sun/ultraviolet ray exposure, male sex, less skin pigmentation, and chronic inflammatory processes.
Chronic sun exposed skin lesions of Squamous cell carcinoma usually arise in skin damaged by actinic rays. The most common sites involved are scalp followed by the lips.
Squamous cell carcinoma that has not penetrated basement membrane are termed in-situ. They are sharply defined red, scaling plaques. Advanced invasive lesions show nodular masses variable keratin production appreciated grossly as hyperkeratotic scale and may ulcerate. Squamous cell carcinoma also presents as nodular masses with variable keratin production and can have hyperkeratotic scales and ulceration and can be independent of DLE.
SCC arising from DLE lesions has worse outcomes in terms of metastasis, recurrence, and death when comparing it to conventional squamous cell cancer of the skin [9].
The overlapping microscopic features which have be to be vigilantly analyzed include pseudoepitheliomatous hyperplasia, acantholysis and lymphocytic infiltration was shown in Figure 5.
Pseudoepitheliomatous hyperplasia represents florid proliferation of epidermis, and it can simulate well differentiated SCC. Besides DLE/ SLE, it is also seen in non-inflammatory conditions which may be due to infective aetiology such as chronic granulomatous disorders like tuberculous verrucae cutis, lupus vulgaris and fungal infections like chromoblastomycosis.
The characteristic histology includes columns of prickle cell down growths into the dermis in an irregular and contiguous fashion. Maturation of central portion causes pearl formation similar in SCC but lacks individual cell atypia. When these columns are penetrated by lymphocytes, hypertrophic SLE like picture emerges.
Another feature shared with Hypertrophic SLE is acantholysis in SCC (Acantholytic SCC). In SLE, acantholysis is mostly limited to basal layer. In SCC, it is evident in tumor cell nests and seem to fall into empty spaces in the central portion of nests, but nuclear atypia and mitosis can be appreciated. Focal keratin formation can also be seen.
The third feature is the interphase infiltrate of lymphoplasmacytoid cells. They are seen in well-established lesions of hypertrophic SLE, and this can extend into perifollicular zones in late lesions. Lymphocytic infiltration is also seen in SCC, more so in verrucous type, which is characterized by squamous epithelial proliferation hyperkeratosis with papillomatosis, hyper granulosis and acantholysis. Rete ridges are bulbous in bull dozing fashion and proliferate downwards into deep dermis with pushing margins. Cellular atypia is minimal if present.
The long-term prognosis of such cases is varied. SCC arising in DLE is regarded as a locally aggressive but low-grade carcinoma with recurrences with reported local recurrences in about 20% and metastasis in 30% cases [5].
In both the case reports of DLE, biopsy specimens were inadequate to confirm the presence of Squamous cell carcinoma. It raises the concern and need for diligent histopathologic interpretation to prevent missing a malignancy such as SCC. The need for deep biopsy from the edge of the growth as well as from raised lesions within areas of DLE/SLE is vital to exclude squamous cell carcinoma.
To summarize, DLE/hypertrophic SLE shares some features with SCC especially in situ lesions and with pseudoepitheliomatous hyperplasia associated with some chronic inflammatory conditions. It gives the pathologist a challenging time, as each disease must be reported separately to enable appropriate therapy.
Development of SCC in chronic cases of DLE/SLE needs extra caution to identify the malignancy. The most important diagnostic clue lies within the tumor cells which display pleomorphism and hyperchromasia in addition to hyperplasia seen in other conditions.
Due to the elevated risk of recurrence along with high chances for recurrence and metastasis and finally the hassle in obtaining a histopathological confirmation, the biopsy study needs diligence as the treatment of SCC is usually superficial resection with clear margins.
Conclusion
We are reporting two rare cases of Squamous cell carcinoma developing over Lupus Erythematosus lesions. A scrupulous clinical and histopathological search for SCC and other malignancies in all patients who have had Discoid Lupus Erythematosus for 5 years or more should be performed routinely by practitioners, including repeat biopsies and close follow-up for any worsening lesions, but the ultimate responsibility for accurate diagnosis lies with the pathologist in these life-threatening situations.
References
- Izmirly P, Buyon J, Belmont HM, Sahl S, Wan I (2019) Population-based prevalence and incidence estimates of primary discoid lupus erythematosus from the Manhattan Lupus Surveillance Program. Lupus Sci Med 6: 1.
- Fernandes MS, Girisha BS, Viswanathan N, Sripathi H, Noronha TM (2015) Discoid lupus erythematosus with squamous cell carcinoma: A case report and review of the literature in Indian patients. Lupus 24: 1562-1566.
- Perniciaro C, Randle HW, Perry HO (1995) Hypertrophic discoid lupus erythematosus resembling squamous cell carcinoma. Dermatol Surg 21: 255-257.
- Sulica VI, Kao GF (1988) Squamous-cell carcinoma of the scalp arising in lesions of discoid lupus erythematosus. Am J Dermatopathol 10: 137-141.
- Millard LG, Barker DJ (1978) Development of squamous cell carcinoma in chronic discoid lupus erythematosus. Clin Exp Dermatol 3: 161-166.
- Kar BR, Nair V, Ebenezer G, Job CK (2004) Squamous cell carcinoma of the scalp arising from chronic cutaneous lupus erythematosus: report of two Indian patients. Indian J Dermatol Venereol Leprol 70: 236-238.
- Nair VL, Chacko M (1991) Disseminated discoid lupus erythematosus with squamous cell carcinoma. Indian J Dermatol Venereol Leprol 57: 196-197.
- Pandhi RK, Gupta R, Kumar SA, Bhutani LK (1984) Discoid lupus erythematosus in Northern India. Ind J Dermatol Venereol Leprol 50: 97-99.
- Tao J, Zhang X, Guo N (2012) Squamous cell carcinoma complicating discoid lupus erythematosus in Chinese patients: review of the literature, 1964–2010,â€. J Am Acad Dermatol 66: 695-696.
Citation: Lilly M, Kaushika, Gali V (2021) Cutaneous Lupus Lesions with Squamous Cell Carcinoma: Diligence in Interpretation. J Clin Exp Pathol 11: 392.
Copyright: © 2021 Lilly M, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Recommended Journals
Open Access Journals
Article Usage
- Total views: 2199
- [From(publication date): 0-2021 - Dec 20, 2024]
- Breakdown by view type
- HTML page views: 1724
- PDF downloads: 475