Review Article Open Access
Cryptococcosis: An Emerging Airborne Mycosis of Global Concern
Mahendra Pal1* and Pratibha Dave22
1Veterinary Public Health (UNDP), Addis Ababa University, Ethiopia.
2Welfare Hospital and Research Centre, Bharauch-392001, Gujarat, India.
- *Corresponding Author:
- Mahendra Pal
Ex-Professor of Veterinary Public Health (UNDP)
Addis Ababa University, Ethiopia
Tel: +251 114 338 450
E-mail: palmahendra2@gmail.com
Received Date: May 05, 2016; Accepted Date: June 16, 2016; Published Date: June 25, 2016
Citation: Pal M, Dave P (2016) Cryptococcosis: An Emerging Airborne Mycosis of Global Concern. Air Water Borne Diseases 5:127. doi:10.4172/2167- 7719.1000127
Copyright: © 2016 Pal M, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Air & Water Borne Diseases
Abstract
Cryptococcosis, an emerging highly infectious respiratory mycosis, is mainly caused by Cryptococcus neoformans and Cryptococcus gattii, which exist as saprobe in the environment. Currently, nine molecular types, five in C.neoformans and four in C. gattii are identified. The disease occurs in sporadic and epidemic form resulting into significant morbidity and mortality, especially in immunocompromised patients. Globally, cryptococcosis causes about 625,000 deaths annually. The clinical manifestation of pulmonary cryptococcosis includes cough, weight loss, sputum, chest pain, dysponea, fever, headache, and hemoptysis. The demonstration of pathogen both by direct microscopy in India ink and its isolation on Pal sunflower seed medium is still considered as gold standard to confirm an unequivocal diagnosis of cryptococcosis. The morphology of isolates can be easily studied in “Narayan” stain. The fluconazole, being a less toxic drug, is recommended for the management of pulmonary cryptococcosis. It is emphasized to undertake molecular characterization of Cryptococcus isolates to know the genotypes prevalent in different regions of the world. Since many laboratory in poor resource countries do not have facilities to undertake biochemical test, it is therefore, advised to use easily available, very sensitive, highly specific and low cost “Pal sunflower seed medium” to make an early diagnosis to save the life of patients from this enigmatic mycosis. Further research work on pathogenesis, epidemiology, and chemotherapy may be rewarding.
Keywords
Airborne; Cryptococcosis; Fungus; Narayan stain; Pal sunflower seed medium; Public health; Saprobe
Introduction
Airborne can be defined as any disease that is caused by microbe such as viruses, bacteria, fungi, and are transmitted through the air. Indoor air pollution has been widely recognized as a serious health problem. Airborne diseases are of considerable importance as they result in high morbidity and morbidity. Many common infections, which can spread by airborne transmission include anthrax, aspergillosis, chlamydiosis, coccidiodomycosis, cryptococcosis, influenza, histoplasmosis, nocardiosis, Q fever, tuberculosis, etc. [1]. Among these, cryptococcosis (Busse Buschke’s disease, European blastomycosis, Torulosis) is one of the major respiratory mycotic diseases, which has emerged as a leading cause of life threatening infection, especially in immunocompromised hosts [2,3]. The recorded history of cryptococcosis goes back to year 1894 when Sanfelice recovered the yeast like fungus from peach juice in Italy, and he named it as Saccharomyces neoformans. In the same year, Busse [4] isolated the yeast from a sarcoma like lesion of tibia of a woman from Germany. Emmons is credited to report the first isolation of Cryptococcus neoformans from the soil and pigeon droppings in 1951, and 1955, respectively. Later, this observation was confirmed by many regions of the world including India [5-9]. Environmental isolations of C. gattii from wood, bark, leaves, and plant debris of Eucalyptus tree were described by Ellis and Pfeiffer [10]. The first record of association of C. neoformans with mastitis in a goat and buffalo was established by Pal, respectively [11]. The disease in humans and animals is caused mainly by Cryptococcus neoformans and Cryptococcus gattii [9].
Cryptococcosis is an enigmatic fungal disease of medical importance, which has been is reported from many countries of the world including India [11-13]. The infection is mainly acquired by inhalation of the infected dust loaded with organisms. However, accidental inoculation of fungus into skin following traumatic injury can also result infection [11]. The fungus from the lungs can disseminate to other organs including the brain, skin, skeleton system, and urinary tract [8]. The first record of pulmonary cryptococcosis in man was described in 1924 by Sheppe. Littman [14] from USA reported the first case of primary cryptococcal meningitis in a physician following direct exposure to a library air-conditioner laden with pigeon excreta containing Cryptococcus neoformans. In India, the first case of human cryptococcosis involving the lungs and brain of a 15-year-old white girl was published by Reeves et al. [15]. The disease can occur in various forms, such as pulmonary, meningoencephalitis, visearal, osseous, mucocutaneous, and cutaneous [7,11]. The ubiquitous presence of the organisms in the saprobic environment can become an important source of cryptococcal infections to humans as well as animals. Radiography reveals nodules, cavitation, and pulmonary infiltrates. Mycological, immunological, histopathological, and molecular techniques are employed to confirm the diagnosis of disease [8]. Fluconazole is the mainstay in the treatment of pulmonary cryptococcosis. However, majority of immunocompetent asymptomatic patients with pulmonary cryptococcosis may undergo spontaneous remission [16]. The present communication delineates the growing significance of cryptococcosis as an emerging mycosis of global significance.
Etiological Agents
The genus Cryptococcus is classified in the Kingdom- Fungi, Phylum-Basidiomycota, Class-Tremellomycetes, and Order- Tremellales. It includes at least 37 different species, of which two species namely, C.neoformans and C.gattii are recognized as important human and animal pathogens [17,18]. Rarely, other species of Cryptoccoccus such as C.albidus and C.laurentii are also reported to be of medical significance [9]. The pathogen is Gram- positive, non-acid fast, nonmotile, aerobic, capsulated, and saprobic basidiomycetous yeast, which exists in two mating types: “alpha” and “a” [8]. Cryptococcus neoformans is an anamorph (asexual) fungus, and its teleomorph (sexual) state is known as Fillobasidiella neoformans (serotypes A and D) and Fillobasidiella bacillispora (serotype B and C). The sexual state of C. neoformans was described for the first time by Kwon-Chung [19]. Cryptococcus neoformans is isolated from soil, pigeon droppings, bat guano, poultry faeces, excreta of other avians (parrot, canary, budgerigar, Munia bird, lorikeet), wooden avian nests and perches, empty wooden cages, and fruits and vegetables [20-23,6,8,9]. However, avian droppings particularly, the pigeon excreta is the most important niche for C. neoformans [9]. The natural reservoir of C. gattii seems to be plant materials, as it has been frequently recovered from many species of trees [10,13,9].
Clinical Spectrum
The clinical presentation of cryptococcosis varies from asymptomatic pulmonary colonization to severe pneumonia with respiratory failure and meningitis. The patients exhibit the signs of cough, sputum, fever, pleuritic chest pain, shortness of breath, chest tightness, fatigue, discomfort, malaise, sweating, haemoptysis, tachycardia,hypoxia, and weight loss [24-29,13]. The frequency of occurrence of clinical signs and symptoms observed in pulmonary cryptococcosis in AIDS patients are presented in Table 1. Miliary pulmonary cryptococcosis can also in HIV positive patients [30]. Acute respiratory failure may develop in one third of non-AIDS patients with pulmonary cryptococcosis.Pulmonary involvement in non-AIDS patients has been reported in 10 to 29 % in which the disease was diagnosed [25]. In immunocompromised patients, complications of pulmonary cryptococcosis may have pleural effusion, and meningoencephalitis. Pulmonary cryptococcosis in immunocompetent individuals remains as asymptomatic, where the yeast can be localized in the tracheobronchial tree or can cause pulmonary disease [31]. The presence of acute respiratory failure with cryptococcosis is a grave prognostic sign, and can represent a marker of systemic disease. Hence, it is pertinent to mention that in high risk patients, pulmonary cryptococcosis should be considered in the differential diagnosis of acute respiratory failure [25].
| Symptom | Frequency of occurrence |
|---|---|
| Cough | 89-95 % |
| Weight loss | 60-68% |
| Fever | 48-53% |
| Dyspone | 43-47% |
| Thoracic pain | 26-31% |
| Headache | 11-14% |
| Haemoptysis | 11-14% |
Source: Pal and Dave [11]
Table 1: Signs and symptoms observed in primary pulmonary cryptococcosis in 36 AIDS patients.
Epidemiology
In recent years, cryptococcosis has emerged an important life threatening fungal disease in immunocompromised individuals, particularly affected with AIDS. Disease is mostly reported to occur in sporadic form; however, few outbreaks are also encountered. Cryptococcosis once considered as sleeping giant has become an awakening giant after the epidemics of AIDS [3]. There is a dramatic increase in the incidence of cryptococcosis in post AIDS era. It is estimated that C. neoformans causes about one million new cases of meningoencephalitis in AIDS patients globally every year [32]. A comprehensive study conducted by Banerjee [33] at All India Institute of Medical Sciences, New Delhi, India during1992-2004 reported an increase rate from 20 to 49% of cryptococcosis in AIDS patients. Cryptococcosis has been reported in humans and a wide variety of animals from developed as well as developing nations of the world [7,8]. A plethora of risk factors such as HIV/AIDS, cancer, diabetes mellitus, organ transplant, corticosteroid therapy, tuberculosis, sarcoidosis, leukemia, emphysema, asthma, rheumatic diseases, leprosy, liver cirrhosis, systemic lupus erythematous, malnutrition, pregnancy, and advancing age can predispose the persons to cryptococcosis [8,13]. Surprisingly, C. neoformans predominantly infects the immunocompromised hosts whereas C. gatti frequently attacks the immunocompetent subjects [18]. The disease is observed in both sexes, with more cases in males, and in all age groups but rare in children [13]. Autopsy studies in South Africa and Uganda has shown a very high rate of pulmonary misdiagnosis. More than 95% of patients with pulmonary cryptococcosis were misdiagnosed, and among them, over 50% were treated for pulmonary tuberculosis [27,29,34]. The dust in the home environment can carry the pathogen, and hence, the subsequent exposure to the susceptible individual may produce the infection. Certain occupational groups such as bird fanciers, pigeon breeders, zoo workers, veterinarians, and persons engaged in the cleaning of old monuments, historical buildings, and avian habitats have a greater risk of acquiring the infection. It is pertinent to mention that over 80% of patients with pulmonary cryptococcosis reveal a history of environmental exposure, mainly to pigeon droppings [29]. Cases of pulmonary cryptococcosis in pigeon handler and per bird keeper are reported from India and other countries [35,12]. It is mentioned that HIV negative persons (30-70%) suffer from respiratory cryptococcocal infections more frequently, as compared to AIDS patients (2%), who develop disseminated cryptococcosis [36,37]. Epidemiological studies indicate that persons infected with C. gattii commonly suffer from pulmonary disease, while those affected with C.neoformans present with meningoencephalitis [18]. In immunocompromised patients, pulmonary cryptococcosis can be severe and rapidly progressive causing grave prognosis [31]. A study conducted in Uganda showed 11% prevalence of pulmonary cryptococcosis among HIV infected patients hospitalized with pneumonia who underwent bronchoscopy. It is advised to undertake detailed study to determine the growing role of Cryptococcus species in the pneumonia. Environmental studies revealed that an increased concentration of C. gattii can occur when colonized trees are clipped or felled [13]. The recovery of C. neoformans by the use of highly sensitive and specific Pal sunflower seed medium from old and dry pigeon droppings repeatedly obtained from a dark and humid covered site not exposed to direct sunlight after 20 years of its first isolation indicates the longest survival of this yeast in nature [3]. Similarly, persistence recovery of C. neoformans from empty wooden canary cages kept unused since last eight months in a dark room of a building in Antwerp, Belgium is an important observation and warrants additional studies to elucidate the role of various woods, trees, and other plant substrates to elucidate the ecology of both species of Cryptococcus [38].
Diagnosis
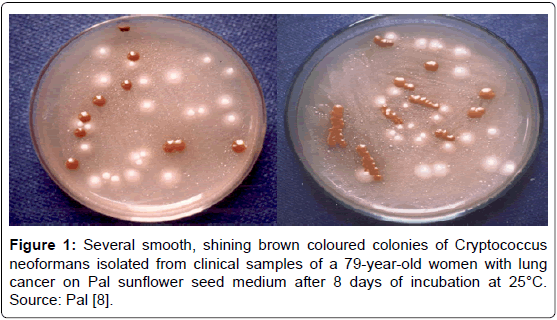
In the absence of characteristic signs, the laboratory help is imperative to establish an unequivocal diagnosis of pulmonary cryptococcosis. On computed tomography, pulmonary cryptococcosis may present as solitary or multiple masses, dense consolidation, glass coloured interstitial opacities, and pleural effussions [30]. The diagnosis of pulmonary cryptococcosis requires both direct demonstration of the pathogen in clinical sample and its isolation in pure and luxuriant growth on mycological medium. Clinical specimens such as sputum, oropharyngeal washings, bronchoalveolar lavage (BAL), and lung biopsy should be examined for the pathogen both by direct microscopy in India ink/nigrosin mount or KOH, and by culture on Pal sunflower seed medium. This medium was developed by Pal [8], and later, it was simplified to make it a very cheap differential medium for an early laboratory diagnosis so that it can be widely employed by limited resource nations. It contained 45 g of pulverized sunflower seed, 20 g agar, 500 mg chloramphenicol, and 1000 ml of distilled water [8]. On Pal sunflower seed medium, both species produce light to dark brown pigmented colonies within 2 to 3 days (Figure 1). Hitherto, there is no organism, which can impart brown colour on Pal sunflower seed medium. Therefore, this brown colour effect on this medium helps in early identification of the pathogen [39]. It is advised that cycloheximide (actidione) should not be added in the medium as it inhibits the growth of C. neofirmans. The morphology of the yeast can be easily studied in Narayan stain, which contains 6.0 ml of dimethyl sulfoxide (DMSO), 0.5 ml of 3% aqueous solution of methylene blue, and 4.0 ml of glycerine [40]. Animal pathogenicity test is performed in Swiss albino mice by injecting the culture of organism by various routes (Pal, 2005). Both varieties can be differentiated by inoculating the culture of organism on canavanine glycine bromothymol blue agar [7,8]. In vitro sexual compatibility experiment to know the mating types can be done on modified Pal sunflower seed medium, which was developed by Pal at Institute of Tropical Medicine, Antwerp. The fungus can also be demonstrated in biopsied and autopsied tissues by several hisopathological techniques such as periodic acid Schiff (PAS), Mayer’s mucicarmine ,Gomori methanamine silver nitrate (GMS) [11,8]. Latext agglutination test can detect polysaccharide capsule antigen in the serum and CSF. Although high titer is suggestive of severe infection, negative titer does not rule out the disease [37]. It is mentioned that false positive results have been found with latext agglutination test and India ink smears [7]. The comparative efficacy of various laboratory techniques for the diagnosis of cryptococcosis is given in Table 2. Molecular tests are useful to study the epidemiology of disease. Pulmonary cryptococcosis should be differentiated from tuberculosis, nocardiosis, aspergillosis, and other respiratory diseases.
| Technique | Specimen (CSF) | Percent positive |
|---|---|---|
| Direct microscopy in India ink or Nigrosin stain | 27*/31 | 87.0 |
| Culture on Pal’s medium at 30°C | 29/31 | 93.5 |
| L. A. for cryptococcal antigen | 28/31 | 90.3 |
Numerator denotes number of CSF specimens positive and denominator number of samples examined. Source: Pa [8].
Table 2: Comparison of different techniques for the diagnosis of cryptococcal infection.
Treatment
A number of antifungal drugs like amphotericin B, flucytosine, ketoconazole, fluconazole, and itraconazole are used for the management of cryptococcosis. All patients who are symptomatic should be treated. Duration of treatment depends on the severity of disease. Mild to moderate disease limited to the respiratory system can be treated orally by fluconazole (400 mg daily for 6 to 12 months) both in immunocompromised and immunocompetent hosts [36]. However, severe pulmonary cryptococcosis can be treated with a high dose of oral fluconazole 1200 mg once daily for 14 days, then 600-800 mg once daily for 8 weeks. Then, 200 mg fluconazole orally once daily for 6-12 weeks is recommended as maintenance dose [29]. It is important to mention that before the start of therapy, CSF should be cultured on Pal sunflower seed medium to rule out the possibility of meningeal involvement. Pulmonary cryptococcosis either asymptomatic or with symptoms can resolve without treatment in immunocompetent individuals [2]. Despite current therapy with antifungal drugs, patients continue to die of the cryptococcal infections. As prostate gland in male patients serve as reservoir of C. neoformans, a negative culture of urine on Pal sunflower seed medium indicates effective therapy [8]. It is important to mention that physician should enquire from the patient about the environmental and occupational exposure to avian excreta.
Therefore, research should be directed to understand the mechanisms of host invasion by the pathogen. This may be useful for developing better treatment regimes to reduce the morbidity and mortality among patients suffering from disease.
Control
Since the causative agents occur as saprobe in the environment and no commercial vaccine is available, it is not feasible to eliminate the disease from this globe. However, the susceptible subjects, especially suffering from AIDS must avoid the visit to avian habitats or dusty environment. The persons working in zoological gardens, old monuments, historical buildings, bird hospitals, wild life habitats, pet bird shops, pigeon breeding farms, wood cutting factories, etc. are advised to use face mask to prevent the inhalation of pathogen [8,3]. Decontamination of the avian excreta and habitats can be achieved by spraying 5% solution of formalin. It is emphasized to develop a potent, safe and cheap vaccine, which can be used in high risk people to control this life threatening mycosis.
Conclusion
Respiratory tract is the principal portal of entry of the fungus, which occurs widely in the environment. Inhalation of pathogen from the saprobic reservoirs such as avian droppings, wood can cause infection in the susceptible host. The role of avians and mammals, which may carry the pathogenic species of Cryptococcus, and spread of the yeasts and basidiospores in the environment need to be elucidated. It is emphasized that comprehensive epidemiological studies should be conducted to determine the incidence of pulmonary cryptococcosis both in immunocompetent as well as immunocompromised hosts. It is emphasized that early diagnosis is very important to institute antifungal therapy for averting the fatal consequences of this emerging life threatening mycosis. The discovery of safe, effective, and cheap antifungal drugs, which can be easily affordable by the poor resource counties, will be a boon to the medical field, as the incidence of cryptococcosis and other mycoses are increasing, especially in immunocompromised individuals. It is advised that multidisciplinary approach is pertinent to understand the dynamics of cryptococcal infection.
Acknowledgment
The authors wish to thank Indian Council of Agricultural Research, New Delhi, India to permit us to utilize few data from the book entitled “ Veterinary and Medical Mycology” authored by Prof.Mahendra Pal. Thanks are also due to Kushagra for helping in computer work.
References
- Pal M (2007a) Zoonoses. (2ndedtn)Satyam Publishers Jaipur India.
- Huston SM,Mody CH (2009) Cryptococcosis: An emerging respiratory mycosis. Clinical Chest Medicine 30: 253-264.
- Pal M, Tesfaye S, Dave P (2014) Cryptococcosis: An enigmatic mycosis of humans and animals. Journal of Occupational and Environmental Science 3: 53-60.
- Busse O (1894) Uberpearasitarezelleinschlusse und ihrezuchtung. Zentrablat Bacteriology 16: 175-180.
- Littman ML (1959) Cryptococcosis (Torulosis): Current concepts and therapy. American Journal of Medicine 27: 976-998.
- Pal M, Onda C, Hasegawa A (1990) Isolation of saprophytic Cryptococcus neoformans. Japanese Journal of Veterinary Science 52:1171-1174.
- Kwon Chung KJ and Bennett JE (1992) Medical Mycology. 1st Edition, Lea and Febiger, Philadelphia USA.
- Pal M (2007b) Veterinary and Medical Mycology. (1stedtn) Indian Council of Agricultural Research, New Delhi, India
- Pal M (2015) First record of isolation of Cryptococcus neoformans from pigeon droppings in Djibouti. Molecular Microbiology Research5: 1-3.
- Ellis DH, Pfeiffer TJ(1990) Natural habitat of Cryptococcus neoformans var. gattii. Journal of Clinical Microbiology 28:1642-1644.
- Dave P, Pal M (2015) Primary cutaneous mycosis in an immunocompetent parrot keeper due to Cryptococcus neoformans. Molecular Microbiology Research 5: 1-3.
- Pal M (1993) Pulmonary mycosis in a pigeon handler due to Cryptococcus neoformans var. neoformans.2nd International Conference on Cryptococcus and Cyptococcosis. Milan Italy : 119.
- MacDougall L, Fyfe M, Romney M, Starr M, Galanis E (2011) Risk factors for Cryptococcus gatti infection, British Columbia, Canada. Emerging Infectious Diseases 17: 193-199.
- Sheppe WM (1924) Torula infection in man. American Journal of Medical Science 167: 91-93.
- Reeves DL, Butt EM, Hamnack RW (1941) Torula infection of the lungs and central nervous system: report of six cases with three autopsies. Archieves of Internal Medicine 68: 57-79.
- Emmons CW (1955) Saprophyic sources of Cryptococcus neoformans associated with the pigeon (Columbia livia). American Journal of Hygiene 62: 227-232.
- Gupta G, Fries BC (2010) Variability of phenotypic traits in Cryptococcus varieties and species and the resulting implications for pathogenesis. Future Microbiology 5: 775-787.
- Pal M (2014) Cryptococcus gattii: An emerging global mycotic pathogen of humans and animals. Journal of Mycological Research 52: 1-6.
- Kwon-Chung KJ (1975) A new genus Filobasiediella ,the perfect state of Cryptococcus neoformans. Mycologia 67: 1197-1200.
- Pal M (1978) Saprobic reservoirs of Cryptococcus neoformans. Indian Journal of Public Health22: 327-328.
- Pal M,Mehrotra BS (1985) Studies on the isolation of Cryptococcus neoformans from fruits and vegetables. Mycosen 28: 200-205.
- Pal M (1986) Studies on the epidemiology of cryptococcosis. Post Doctorate Dissertation .Institute of Tropical Medicine Antwerp Belgium.
- Pal M(1989) Cryptococcus neoformansvarneoformans and munia birds. Mycoses 32: 250-252.
- Nunez M, Peacock JE Jr, Chin R Jr(2000) Pulmonary cryptococcosis in the immunocompetent host: Therapy with fluconazole: a report of four cases and review of literature. Chest 118: 527-534.
- Vilchez RA, Linden P, Lacomis J, Costello P, Fung J et al. (2001) Acute respiratory failure associated with pulmonary cryptococcosis in non-AIDS patients. Chest 119: 1865-1869.
- ChuHQ, LiHP,HeGJ (2004) Analysis of 23 cases of pulmonary cryptococcosis. Chinese Medical Journal 117: 1425-1427.
- Wong ML, Back P, Candy G, Nelson G, Murray J(2007)Cryptococcal pneumonia in African miners at autopsy. International Journal of Tuberculosis and Lung Disease 11: 528-533.
- Javis JN, Harrison TS(2008) Pulmonary cryptococcosis. Seminar Respiratory Critical Care Medicine 29: 141-150.
- Gunda DW, Bakshi FA, Rambay P, Klinzo SB(2015) Pulmonary cryptococcosis presenting as acute severe respiratory disease in a newly diagnosed HIV patient in Tanzania: a case report. Clinical Case Reports 3: 749-752.
- Zink SE, Leug AN, Frost M, Berry GJ, Muller NL (2002) Pulmonary cryptococcosis: CT and radiologic findings. Journal of Computed Assisted Tomography 26: 330-334.
- Nadrous HF, Antonias VS, Terrell CL, Ryu JH(2003) Pulmonary cryptococcosis in nonimmunocompromised patient. Chest 124: 2143-2147.
- Park JB,Wannemuehler KA, Marston BJ,Govender N, Pappas PG, et al. (2009) Estimation of the current burden of cryptococcal meningitis among persons living with HIV/AIDS.AIDS 23: 525-530.
- Banerjee U (2005) Progress in the diagnosis of opportunistic infections in HIV/AIDS. Indian Journal of Medical Research 121: 395-406.
- Yoo SD, Warodia, W, Davis JL, Cattamanchi A, Boon SD, et al. (2010) The prevalence and clinical course of HIV associated pulmonary cryptococcosis in Uganda. Journal of Acquired Immune Deficiency Syndrome 54: 269-74.
- Nosanhchuk JD, Shohan S, Fries BC, Shapiro DS, Levitz SM, et al. (2000) Evidence of zoonotic transmission of Cryptococcus neoformans from a pet cockatoo to an immunocompromised patient. Annals of Internal Medicine 132: 205-308
- ChayaKulkeerre M, Perfect JR (2006)Cryptococcosis. Infectious Disease Clinic of North America 20: 507-544.
- Shirley RM, Baddley JW(2009)Cryptococcal lung disease. Current Opinion in Pulmonary Medicine 15: 254-260.
- Pal M(1995) Natural occurrence of Cryptococcus neoformansvar.neoformans in wooden canary cages. RevistaIberoamericana de Micologia 12: 93-94.
- Pal M (1997) Use of Pal’s sunflower seed medium for an early diagnosis of cryptococcosis. The Antiseptic95: 175.
- Pal M (2004) Efficacy of Narayan stain for morphological studies of moulds,yeasts and algae. RevistaIberoamericana de Micologia 21: 219.
Relevant Topics
Recommended Journals
Article Tools
Article Usage
- Total views: 13486
- [From(publication date):
September-2016 - Apr 02, 2025] - Breakdown by view type
- HTML page views : 12525
- PDF downloads : 961