Commentary Open Access
Cryptococcal Meningitis with Cerebral Herniation
1Division of Intensive Care Medicine, Chi Mei Medical Center, Tainan City, Taiwan
2Department of Medicine, Taipei Medical University, Taipei City, Taiwan
- *Corresponding Author:
- Wen-Liang Yu
Department of Intensive Care Medicine
Chi Mei Medical Center, 901 Chung Hwa Rd.
710 Tainan City, Taiwan
Tel: +886-6-2812811
Fax: +886-6-2833351
E-mail: Yuleon_md@yahoo.com.twa
Received date: July 28, 2016; Accepted date: August 15, 2016; Published date: August 17, 2016
Citation: Yu WL (2016) Cryptococcal Meningitis with Cerebral Herniation. J Neuroinfect Dis 7:222. doi:10.4172/2314-7326.1000222
Copyright: © 2016 Yu WL. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use,distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Neuroinfectious Diseases
Commentary
Cryptococcus neoformans (C. neoformans var. grubii and C. neoformans var. neoformans ) and C. gattii are responsible for most cases of cryptococcal meningitis worldwide [1]. The disease of cryptococcal meningitis has been well documented in patients with acquired immune deficiency syndrome (AIDS) and it may also occur in human immunodeficiency virus (HIV)-negative patients even with apparently normal immune systems [2,3]. The median age of 38.5 years at presentation in the non-HIV patients is similar to that in the HIV population (median age, 36 years) [2,4]. Chinese population seems to be more vulnerable than other ethnic groups to cryptococcal meningitis in the previously healthy patients [5]. However, the diagnosis is easily delayed and the disease manifestations may be more severe in cryptococcal meningitis of the immunocompetent patients than in immunocompromised patients [4]. The most common underlying condition in Chinese patients with cryptococcal meningitis is corticosteroid use [4], which has sometime been added illegally to traditional herb drug medication.
Moreover, it has been shown that mutative genotype coding for mannose-binding lectin (MBL) deficiency is associated with cryptococcal meningitis in HIV-uninfected Chinese patients, particularly in immunocompetent patients [6]. As the levels of MBL fluctuate with MBL gene polymorphism in systemic lupus erythematosus (SLE) patients [7] and a general hypomethylated state of T and B lymphocyte genes has been observed in SLE patients with inhibited DNA methyl transferases (DNMTs) efficacy [8,9], aberrant DNA methylation patterns might directly lead to the abnormal expression of MBL and perhaps cause cryptococcal meningitis in humans. Therefore, study the stability of enzymes that required for the establishment and maintenance of DNA methylation, including DNMTs and some histone methyltransferases [10-12], might be a new direction for the early recognition of patients who are at risk for cryptococcal meningitis.
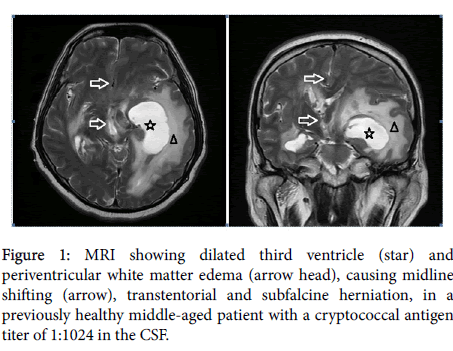
Morbidities of cryptococcal meningitis are high, with seizures, cranial nerves palsies, obstructive hydrocephalus, increased intracranial pressure (IICP), cerebral edema and herniation (Figure 1). In a retrospective review of 154 non-HIV-infected patients with cryptococcal meningitis in China, the morbidities included seizures (28.6%), cranial nerves palsies (51.5%) and cerebral herniation (19.5%), with attributable and one-year overall mortality rates of 19.6% and 28.7%, respectively [4]. Patients with delayed diagnosis of cryptococcal meningitis experience more brain herniation, coma, seizures, hydrocephalus and more surgical shunt procedures [4]. Delay in the diagnosis of hydrocephalus may be accompanied with IICP and could thereby cause a deterioration of consciousness [13].
Clinical manifestations may include nausea, vomiting, severe frontal headaches, neck stiffness, dizziness, impaired balance, oscillopsia, blindness, paraparesis, unsteadiness of gait and somnolence [14]. Radiographic image of the brain with computed tomography (CT) or magnetic resonance image (MRI) plays an important role in detection of the central nervous system (CNS) morbidities. Brain CT may show normal appearance, severe cerebral edema, hydrocephalus or tonsillar herniation. Besides, MRI is superior to CT in detecting CNS abnormalities, such as leptomeningeal enhancement and ventriculitis, in patients with cryptococcal meningitis [15]. In a recent retrospective review of immunocompetent patients with cryptococcal meningitis, multiple intraparenchymal lesions were more common than leptomeningeal enhancement in the brain MRI radiographs [16]. The cryotococcal fungi could be isolated in the cerebrospinal fluid (CSF), leptomeninges and parenchyma of the brain [17]. Cryptococcus antigen titer is usually positive in the CSF and/or serum. Nevertheless, it could happen that Cryptococcus antigen is positive in the serum but negative in the CSF [18].
Treatment of cryptococcal meningitis remains a challenge. Three most important managements have been highlighted: (1) induction therapy for meningococcal encephalitis with antifungal agents followed by suppressive regimens using fluconazole; (2) the use of lipid formulations of amphotericin B regimens in patients with renal impairment; and (3) early recognition and management of IICP [19,20]. Prompt relief of hydrocephalus is useful for the patients who show rapid deterioration of consciousness or signs of cerebral herniation. Lumbar puncture may have to be initiated or repeated sooner in managing IICP or if physicians have a concern about potential microbiologic failure [19]. Permanent ventriculoperitoneal (VP) shunt placement is a safe and effective way of therapy [13,21-24], even in the status of IICP (>500 mm CSF) without evidence of hydrocephalus [20]. Besides, premedication with antifungal drugs before surgical procedure is unnecessary [24].
Delay in the diagnosis or treatment of patients with hydrocephalus is associated with poor outcome [4]. Control of intracranial pressure could be one of the most important determinants of outcome [21-24]. Patients with hydrocephalus whose Glasgow coma scale >9 had been shown to have better outcome following permanent shunt placement [21]. However, the duration of disturbance of consciousness or change of mentality before shunting is critical in determination of the outcome of the treatment [24].
In conclusion, cryptococcal meningitis with hydrocephalus and cerebral herniation may be refractory to antifungal therapy and VP shunting. As sequential changes of brain abnormalities may occur any time throughout the disease course, further imaging study is important in followed up of patients with poor consciousness and responsiveness to treatment although treatment is undergoing and several image studies have already been performed.
References
- Mitchell TG, Perfect JR (1995)Cryptococcosis in the era of AIDS âÂ?Â?100years after the discovery of Cryptococcus neoformans.ClinMicrobiolRev 8: 515âÂ?Â?548.
- Pappas PG, Perfect JR, Cloud GA, Larsen RA, Pankey GA, et al. (2001) Cryptococcosis in humanimmunodeficiency virus-negative patients in the era of effective azoletherapy. Clin Infect Dis 33: 690-699.
- Lu CH, Chang HW, Chuang YC (1999) The prognostic factors of cryptococcalmeningitis in HIV-negative patients. J Hospital Infect 42:313-320.
- Zhu LP, Wu JQ, Xu B, Ou XT, Zhang QQ, et al. (2010)Cryptococcal meningitis in non-HIV-infected patients in a Chinese tertiary care hospital, 1997-2007. Med Mycol 48:570-579.
- Richardson PM, Mohandas A, Arumugasamy N (1976) Cerebral cryptococcosisin Malaysia. J NeurolNeurosurg Psychiatry 39: 330-337.
- Ou XT, Wu JQ, Zhu LP, Guan M, Xu B, et al. (2011) Genotypes coding for mannose-binding lectin deficiency correlated with cryptococcal meningitis in HIV-uninfected Chinese patients. J Infect Dis203: 1686-1691.
- Takahashi R, Tsutsumi A, Ohtani K, Muraki Y, Goto D, et al. (2005) Association of mannose binding lectin (MBL) gene polymorphism and serum MBL concentration with characteristics and progression of systemic lupus erythematosus. Ann Rheum Dis64: 311-314.
- Renaudineau Y, Youinou P (2011) Epigenetics and autoimmunity, with special emphasis on methylation. Keio J Med60:10-16.
- Zouali M (2011) Epigenetics in lupus. Ann N Y AcadSci1217: 154-165.
- Li E, Bestor TH, Jaenisch R (1992) Targeted mutation of the DNA methyltransferase gene results in embryonic lethality. Cell69: 915-926.
- Okano M, Bell DW, Haber DA, Li E (1999) DNA methyltransferases Dnmt3a and Dnmt3b are essential for de novo methylation and mammalian development. Cell 99: 247-257.
- Zhang T, Termanis A, ÃÂ?zkan B, Bao XX, Culley J, et al. (2016) G9a/GLP Complex maintains imprinted DNA methylation in embryonic stem cells. Cell Rep15: 77-85.
- Park MK, Hospenthal DR, Bennett JE (1999) Treatment of hydrocephalus secondary to cryptococcal meningitis by use of shunting. Clin Infect Dis 28:629-633.
- Lane H, Browne L, Delanty N, Neill SO, Thornton J, et al. (2005) July 2004: 40-year-old man with headaches and dyspnea. Brain Pathol15: 89-90, 95.
- Patronas NJ, Makariou EV (1993) MRI of choroidal plexus involvement in intracranial cryptococcosis. J Comput Assist Tomogr17:547-550.
- Tan ZR, Long XY, Li GL, Zhou JX, Long L (2016) Spectrum of neuroimaging findings in cryptococcal meningitis in immunocompetent patients in China âÂ?Â? A series of 18 cases. J Neurological Sci 368: 132âÂ?Â?137.
- Terada T (2010) Cryptococcosis in the central nervous system in a 36-year-old Japanese man: an autopsy study. Tohoku J Exp Med222:33-37.
- Garcia-Santibanez RC, Gill V, Yancovitz S, Pyburn D (2015)Neuroinvasivecryptococcosis in an immunocompetent patient with a negative spinal fluid cryptococcus antigen. Case Rep Infect Dis2015: 857539.
- Perfect JR, Dismukes WE, Dromer F, Goldman DL, Graybill JR,et al. (2010) Clinical practice guidelines for the management of cryptococcal disease: 2010 update by the Infectious Diseases Society of America. Clin Infect Dis 50:291-322.
- Dismukes WE, Cloud G, Gallis HA, Kerkering TM, Medoff G, et al. (1987) Treatment of cryptococcal meningitis with combination amphotericin B and flucytosine for four as compared with six weeks. N Engl J Med 317:334-341.
- Woodworth GF, McGirt MJ, Williams MA, Rigamonti D (2005) The use of ventriculoperitoneal shunts for uncontrollable intracranial hypertension without ventriculomegally secondary to HIV-associated cryptococcal meningitis. SurgNeurol 63: 529-531.
- Graybill JR, Sobel J, Saag M, Van Der Horst C, Powderly W, et al. (2000) Diagnosis and management of increased intracranial pressure in patients with AIDS and cryptococcal meningitis. The NIAID Mycoses Study Group and AIDS Cooperative Treatment Groups. Clin Infect Dis 30:47-54.
- Liliang PC, Liang CL, Chang WN, Chen HJ, Su TM, et al. (2003) Shunt surgery for hydrocephalus complicating cryptococcal meningitis in human immunodeficiency virusâÂ?Â?negative patients. Clin Infect Dis37: 673-678.
- Tang LM (1990)Ventriculoperitoneal shunt in cryptococcal meningitis with hydrocephalus. SurgNeurol33:314-319.
Relevant Topics
- Bacteria Induced Neuropathies
- Blood-brain barrier
- Brain Infection
- Cerebral Spinal Fluid
- Encephalitis
- Fungal Infection
- Infectious Disease in Children
- Neuro-HIV and Bacterial Infection
- Neuro-Infections Induced Autoimmune Disorders
- Neurocystercercosis
- Neurocysticercosis
- Neuroepidemiology
- Neuroinfectious Agents
- Neuroinflammation
- Neurosyphilis
- Neurotropic viruses
- Neurovirology
- Rare Infectious Disease
- Toxoplasmosis
- Viral Infection
Recommended Journals
Article Tools
Article Usage
- Total views: 13339
- [From(publication date):
September-2016 - Apr 04, 2025] - Breakdown by view type
- HTML page views : 12332
- PDF downloads : 1007