Critical Care for Older Adults: Unique Considerations and Challenges
Received: 03-May-2023 / Manuscript No. JCPHN-23-98096 / Editor assigned: 05-May-2023 / PreQC No. JCPHN-23-98096 (PQ) / Reviewed: 19-May-2023 / QC No. JCPHN-23-98096 / Revised: 22-May-2023 / Manuscript No. JCPHN-23-98096 (R) / Published Date: 29-May-2023 DOI: 10.4172/2471-9846.1000416
Abstract
As the population continues to age, there has been a significant increase in the number of older adults who require critical care. Older adults have unique physiological, cognitive, and functional changes that can affect their response to critical illness and medical interventions. This article will explore the unique considerations and challenges associated with providing critical care to older adults.
Keywords
Critical care; Senior citizens; Cognitive changes; Polypharmacy
Introduction
Older adults experience several physiological changes that can affect their response to critical illness. These changes include a decreased ability to maintain homeostasis, decreased organ reserve, and decreased immune function. These changes can make older adults more susceptible to complications and longer hospital stays [1].
Methodology
Cognitive impairment: Older adults with cognitive impairment may have difficulty understanding their medical condition, communicating their symptoms, and following medical instructions. This can lead to suboptimal medical decision-making and increase the risk of adverse outcomes.
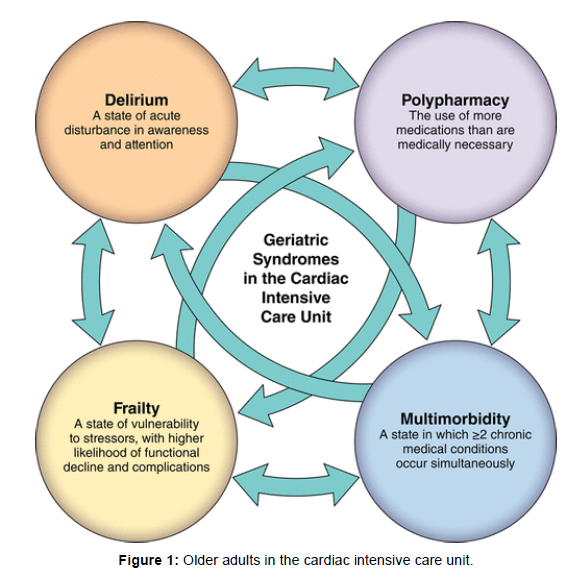
Polypharmacy: Older adults are more likely to have multiple chronic medical conditions and require multiple medications. Polypharmacy can increase the risk of adverse drug reactions, drugdrug interactions, and medication non-adherence [2, 3].
Challenges in critical care for older adults
Delirium: Older adults are at increased risk of developing delirium during critical illness. Delirium can lead to longer hospital stays, increased mortality rates, and long-term cognitive impairment.
Functional decline: Older adults may experience functional decline during hospitalization, including loss of mobility, increased dependence, and decreased ability to perform activities of daily living. This functional decline can increase the risk of long-term disability and reduce quality of life.
End-of-life care: Older adults may have different end-of-life preferences than younger adults. It is crucial to discuss end-of-life care preferences early in the hospitalization and involve the patient and their family in decision-making [4, 5].
The world's population is rapidly aging, with the number of older adults expected to reach 1.5 billion by 2050. With this demographic shift, there has been an increasing need for critical care services for older adults, particularly those with complex medical needs. In this research article, we will discuss the challenges and strategies for providing critical care to older adults.
Challenges in providing critical care to older adults
Multi-morbidity: Older adults are more likely to have multiple chronic health conditions, known as multi-morbidity, which can complicate their care in critical care settings. Managing multiple conditions simultaneously can be challenging and requires a coordinated approach among healthcare providers.
Frailty: Frailty is a condition that affects many older adults, characterized by a decline in physical function and increased vulnerability to stressors such as surgery or infection. Frailty can make critical care management more complex and increase the risk of adverse outcomes.
Cognitive impairment: Older adults with cognitive impairment, such as dementia, may struggle to understand and communicate their symptoms or make decisions about their care. This can make it difficult for healthcare providers to provide appropriate critical care management [6, 7].
Strategies for providing critical care to older adults
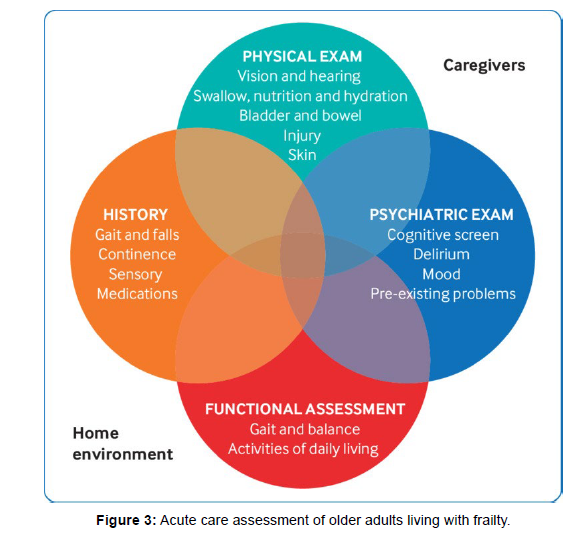
Comprehensive Geriatric Assessment (CGA): A CGA is a multidimensional assessment that evaluates an older adult's physical, functional, and cognitive status, as well as their social and environmental factors. This approach can help healthcare providers identify older adults' unique needs and tailor their critical care management accordingly.
Interdisciplinary care teams: Interdisciplinary care teams, including geriatricians, nurses, and social workers, can provide comprehensive care for older adults in critical care settings. This approach allows healthcare providers to work collaboratively to manage the complex needs of older adults.
Palliative care: Palliative care focuses on providing comfort and support to individuals with serious illnesses and their families. Incorporating palliative care into critical care management for older adults can help improve quality of life and reduce unnecessary interventions [8, 9].
Providing critical care to older adults can be complex and challenging due to the high prevalence of multi-morbidity, frailty, and cognitive impairment. However, using strategies such as CGA, interdisciplinary care teams, and palliative care can help healthcare providers tailor their management to the unique needs of older adults. By improving critical care management for older adults, we can ensure that they receive the best possible care and improve their health outcomes (Figure 1).
As the global population continues to age, the need for critical care services for older adults is increasing. Older adults are more likely to experience acute and chronic health conditions that require intensive medical intervention and support. However, critical care for older adults presents unique challenges due to age-related changes in physiology, multiple comorbidities, and social factors. In this research article, we will discuss the challenges and strategies for critical care of older adults [10, 11].
Challenges in critical care of older adults
Age-Related changes: Older adults undergo several physiological changes that can affect their response to critical care interventions. For instance, decreased respiratory and cardiovascular reserve, decreased renal function, and altered pharmacokinetics can impact the effectiveness and safety of critical care interventions.
Multiple comorbidities: Older adults often have multiple comorbidities, which can complicate the management of critical illness. The presence of comorbidities can make it difficult to identify and treat the underlying cause of critical illness and may require the coordination of multiple specialists to provide comprehensive care (Figure 2).
Social factors: Older adults may face social challenges such as limited social support, financial constraints, and lack of transportation, which can impact their ability to access critical care services. These social factors can also influence treatment decisions, making it difficult to provide appropriate care [12, 13].
Strategies for critical care of older adults
Comprehensive geriatric assessment: Comprehensive geriatric assessment is a process that evaluates the medical, functional, and social status of older adults. This assessment can help identify comorbidities,social challenges, and functional impairments that can impact critical care management. This assessment can also help identify potential risks of adverse events and inform the development of an individualized care plan.
Multidisciplinary team approach: Critical care of older adults requires a multidisciplinary team approach, which includes physicians, nurses, pharmacists, social workers, and other specialists. This approach ensures comprehensive care, including medical management, rehabilitation, and social support.
Palliative Care: Palliative care is an approach that focuses on improving the quality of life for patients with serious illnesses. Palliative care can be integrated into critical care management to address symptom management, psychological support, and end-of-life care [14, 15].
Critical care of older adults presents unique challenges due to age-related changes, multiple comorbidities, and social factors. The strategies outlined above, including comprehensive geriatric assessment, a multidisciplinary team approach, and palliative care, can help address these challenges and improve critical care outcomes for older adults. As the population continues to age, it is essential to prioritize the development of effective strategies for critical care of older adults. By doing so, we can ensure that all individuals, regardless of age, receive high-quality critical care when needed.
Critical care is an important aspect of healthcare that involves the management of life-threatening illnesses and injuries. As the population continues to age, the need for critical care services for older adults is increasing. Older adults are more likely to experience acute and chronic health conditions that require intensive medical intervention and support. However, critical care for older adults presents unique challenges due to age-related changes in physiology, multiple comorbidities, and social factors. In this research article, we will discuss the challenges and strategies for critical care of older adults [s].
Older adults undergo several physiological changes that can affect their response to critical care interventions. For instance, decreased respiratory and cardiovascular reserve, decreased renal function, and altered pharmacokinetics can impact the effectiveness and safety of critical care interventions. Additionally, older adults are more susceptible to delirium, a common complication of critical illness that can lead to adverse outcomes such as prolonged hospitalization and increased mortality. Older adults often have multiple comorbidities, which can complicate the management of critical illness. The presence of comorbidities can make it difficult to identify and treat the underlying cause of critical illness and may require the coordination of multiple specialists to provide comprehensive care. Additionally, older adults with multiple comorbidities may require more intensive monitoring and supportive care during critical illness, which can further complicate their management [17].
Older adults may face social challenges such as limited social support, financial constraints, and lack of transportation, which can impact their ability to access critical care services. These social factors can also influence treatment decisions, making it difficult to provide appropriate care. For example, older adults with limited social support may be at risk of prolonged hospitalization due to lack of resources for discharge planning.
Patients admitted to the intensive care unit (ICU) are critically ill and require specialized care. The complexity of care required in the ICU setting can present unique challenges for healthcare professionals. This article provides an overview of best practices in critical care of ICU patients, as well as current challenges in providing optimal care.
A literature review was conducted to identify best practices in critical care of ICU patients. Articles were selected based on their relevance to the topic and their inclusion of practical recommendations for improving care. Current challenges were identified through an analysis of recent publications and expert opinions in the field.
Use of evidence-based protocols: ICU patients should be managed using evidence-based protocols that have been shown to improve patient outcomes.
Early recognition and treatment of sepsis: Prompt recognition and treatment of sepsis can improve patient outcomes and reduce mortality rates.
Management of pain and sedation: ICU patients frequently experience pain and discomfort. The use of appropriate pain management and sedation protocols can improve patient comfort and reduce the risk of delirium.
Prevention of ventilator-associated pneumonia (VAP): Strategies to prevent VAP include proper hand hygiene, oral care, and implementation of a ventilator bundle.
Prevention of ICU-acquired weakness (ICU-AW): Early mobilization and rehabilitation can help prevent ICU-AW and improve patient outcomes.
Staffing shortages: Many ICUs face staffing shortages, which can limit the ability to provide optimal care.
Burnout and moral distress: Healthcare professionals working in the ICU are at risk of burnout and moral distress, which can impact patient care.
Cost of critical care: The cost of critical care can be high, and access to care may be limited for some patients.
Limited access to specialized care: Some patients may require specialized care that is not available in their local ICU.
The best practices identified in this article can help improve patient outcomes in the ICU setting. However, current challenges such as staffing shortages, burnout, and limited access to specialized care can impact the quality of care provided. Addressing these challenges will require a multi-faceted approach that includes strategies to improve staffing levels, reduce burnout, and increase access to specialized care. Providing optimal care for ICU patients requires a commitment to evidence-based protocols and a focus on addressing current challenges in the field. While there are no easy solutions to the challenges facing critical care, ongoing efforts to improve care will benefit patients and healthcare professionals alike.
The intensive care unit (ICU) provides advanced medical care to critically ill patients who require close monitoring, life support, and specialized treatment. Critical care in ICU patients has evolved significantly over the years, with the development of new technologies and medical practices. Despite this, critical care of ICU patients remains a complex and challenging process. This research article aims to provide an overview of the current practices in critical care of ICU patients and explore potential future directions for improving patient outcomes [18].
Current practices
The current standard of care for ICU patients includes frequent monitoring of vital signs, continuous administration of life support measures, and use of evidence-based medical interventions. Advanced technologies such as mechanical ventilation, extracorporeal membrane oxygenation (ECMO), and continuous renal replacement therapy (CRRT) are commonly used in ICU settings. In addition, multidisciplinary teams including physicians, nurses, respiratory therapists, and pharmacists collaborate to provide coordinated care for ICU patients. The use of evidence-based guidelines and protocols is also a key component of current critical care practices in ICU patients.
Despite the advances in critical care practices, ICU patients face a number of challenges that can impact their outcomes. One of the biggest challenges is the risk of healthcare-associated infections, which can lead to increased morbidity and mortality. Other challenges include the risk of delirium, pressure ulcers, and adverse drug reactions. In addition, ICU patients often experience emotional distress and psychological trauma as a result of their critical illness and prolonged hospitalization [19].
Future directions
To address these challenges and improve outcomes for ICU patients, several future directions have been proposed. These include the use of precision medicine approaches to tailor treatment to individual patients, the implementation of telemedicine and remote monitoring technologies to improve patient access to critical care, and the use of multidisciplinary teams with specialized training in critical care. Other potential directions include the use of advanced technologies such as artificial intelligence and machine learning to identify patient risk factors and predict outcomes, as well as the development of alternative models of care delivery such as ICU-at-home programs (Figure 3).
Critical care of ICU patients is a complex and challenging process that requires a multidisciplinary approach and the use of evidencebased practices. While current critical care practices have advanced significantly, there are still challenges that need to be addressed to improve patient outcomes. By exploring potential future directions such as precision medicine, telemedicine, and advanced technologies, we can continue to advance critical care practices and improve outcomes for ICU patients [20].
Conclusion
Providing critical care to older adults requires a comprehensive approach that addresses their unique physiological, cognitive, and functional changes. Healthcare providers must be aware of the
challenges associated with providing critical care to older adults and take steps to minimize the risk of adverse outcomes. By recognizing the unique considerations and challenges associated with critical care for older adults, healthcare providers can provide high-quality care that improves health outcomes and enhances quality of life.
References
- Batty CJ, Tiet P, Bachelder EM, Ainslie KM (2018) Drug Delivery for Cancer Immunotherapy and Vaccines. Pharm. Nanotechnol 6:232-244.
- Keam SJ (2020) Trastuzumab Deruxtecan: First Approval Drugs. 80:501-508.
- Lipson EJ, Drake CG (2011) Ipilimumab: An Anti-CTLA-4 Antibody for Metastatic Melanoma. Clin Cancer Res 17:6958-6962.
- Wei SC, Duffy CR, Allison JP (2018) Fundamental Mechanisms of Immune Checkpoint Blockade Therapy. Cancer Discov 8:1069–1086.
- Markham A, Duggan S (2018) Cemiplimab: First Global Approval Drugs. 78:1841-1846.
- Zhang F, Qi X, Wang X, Wei D, Wu J, et al. (2017) Structural Basis of the Therapeutic Anti-PD-L1 Antibody Atezolizumab. Oncotarget 8:90215-90224.
- Lee HT, Lee JY., Lim H, Lee SH., Moon YJ ,et al.(2017) Molecular Mechanism of PD-1/PD-L1 Blockade via Anti-PD-L1 Antibodies Atezolizumab and Durvalumab. Sci Rep 7:5532.
- Ahmad A (2020). CAR-T Cell Therapy. Int J Mol Sci 21:4303.
- Stein-Merlob AF, Rothberg MV, Holman P, Yang EH (2021). Immunotherapy-Associated Cardiotoxicity of Immune Checkpoint Inhibitors and Chimeric Antigen Receptor T Cell Therapy: Diagnostic and Management Challenges and Strategies. Curr Cardiol Rep 23:11.
- Van den Bulk J, Verdegaal EM, de Miranda NF (2018). Cancer Immunotherapy: Broadening the Scope of Targetable Tumours. Open Biol 8:180037.
- Adler CH (1999) Differential diagnosis of Parkinson’s disease. Med Clin North Am 83:349–367.
- Alam M, Schmidt WJ (2002) Rotenone destroys dopaminergic neurons and induces parkinsonian symptoms in rats. Behav Brain Res 136:317-324.
- Ansari RA, Husain K, Gupta PK (1987) Endosulfan toxicity influence on biogenic amines of rat brain. J Environ Biol 8:229-236.
- Bagetta G, Corasaniti MT, Iannone M, Nisticò G, Stephenson JD (1992) Production of limbic motor seizures and brain damage by systemic and intracerebral injections of paraquat in rats. Pharmacol Toxicol 71:443-448.
- Barlow BK, Thiruchelvam MJ, Bennice L, Cory-Slechta DA, Ballatori N, et al.(2003) Increased synaptosomal dopamine content and brain concentration of paraquat produced by selective dithiocarbamates. J Neurochem 85:1075-1086.
- Behari M, Srivastava AK, Das RR, Pandey RM (2001) Risk factors of Parkinson’s disease in Indian patients. J Neurol Sci 190:49-55.
- Betarbet R, Sherer TB, Di Monte DA, Greenamyre JT (2002) Mechanistic approaches to Parkinson’s disease pathogenesis. Brain Pathol 12:499-510.
- Betarbet R, Sherer TB, MacKenzie G, Garcia-Osuna M, Panov AV, et al. (2000) Chronic systemic pesticide exposure reproduces features of Parkinson’s disease. Nat Neurosci 3:1301-1306.
- Bloomquist JR, Kirby ML, Castagnoli K, Miller GW (1999). Effects of heptachlor exposure on neurochemical biomarkers of parkinsonism. In: Progress in Neuropharmacology and Neurotoxicology of Pesticides and Drugs Cambridge, UK: Royal Society of Chemistry 195-203.
- Butterfield PG, Valanis BG, Spencer PS, Lindeman CA, Nutt JG (1993) Environmental antecedents of young-onset Parkinson’s disease. Neurology 43:1150-1158.
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Citation: Gomez C (2023) Critical Care for Older Adults: Unique Considerationsand Challenges. J Comm Pub Health Nursing, 9: 416. DOI: 10.4172/2471-9846.1000416
Copyright: © 2023 Gomez C. This is an open-access article distributed under theterms of the Creative Commons Attribution License, which permits unrestricteduse, distribution, and reproduction in any medium, provided the original author andsource are credited.
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 1277
- [From(publication date): 0-2023 - Mar 12, 2025]
- Breakdown by view type
- HTML page views: 1179
- PDF downloads: 98