Research Article Open Access
Creating Effective Interprofessional Mentoring Relationships in Palliative Care- Lessons from Medicine, Nursing, Surgery and Social Work
Muhammad Taufeeq Wahab1, Muhammad Fadhli Bin Mohamad Ikbal1, Wu Jingting1*, Loo Teck Wee Wesley1, Ravindran Kanesvaran1,2,3 and Lalit Kumar Radha Krishna1,2,4,51Department of Medicine, Yong Loo Lin School of Medicine, Singapore
2Practice Course 2, Duke NUS Postgraduate Medical School, Singapore
3Department of Medical Oncology, National Cancer Center, Singapore
4Department of Palliative Medicine, National Cancer Center, Singapore
5Center for Biomedical Ethics, National University, Singapore
- *Corresponding Author:
- Wu Jingting
Department of Medicine
Yong Loo Lin School of Medicine
Singapore
Tel: +6597115775
E-mail: wujting@gmail.com
Received date: November 10, 2016; Accepted date: November 24, 2016; Published date: November 25, 2016
Citation: Wahab MT, Ikbal MFM, Jingting W, Wesley LTW, Kanesvaran R, et al. (2016) Creating Effective Interprofessional Mentoring Relationships in Palliative Care- Lessons from Medicine, Nursing, Surgery and Social Work. J Palliat Care Med 6:290. doi: 10.4172/2165-7386.1000290
Copyright: © 2016 Wahab MT, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Palliative Care & Medicine
Abstract
Palliative Care requires multidisciplinary teamwork to achieve its patient specific objectives. Success of this approach pivots on nurturing effective interprofessional relationships through the provision of holistic support and multidimensional training of multiprofessional Palliative Care team members. Mentoring is seen as an effective means of facilitating multiprofessional collaborations however little data exists on operationalizing an interprofessional mentoring program in Palliative Care. To address this gap and circumnavigate the context-specific nature of mentoring, we scrutinized mentoring approaches in medicine, surgery, nursing and medical social work to identify common elements of mentoring within their respective practices that will provide the basis of an interprofessional mentoring in Palliative Care. Thematic analysis of 20 reviews of undergraduate and postgraduate mentoring programs in medicine, surgery and nursing suggest that successful mentoring programs are underscored by effective nurturing and support of mentoring relationships. Successful mentoring relationships are built on strong relational ties between mentees and mentors. Delineating the key elements to effective mentoring relationships allow for the forwarding of a basic framework to enhance relational ties within interdisciplinary mentoring in Palliative Care and the proffering of an evidence-based platform for the adoption of a cognitive apprenticeship model that can guide the operationalization of a multiprofessional mentoring program in Palliative Care.
Keywords
Mentor; Medicine; Surgery; Nursing; Social work; Interprofessional education
Introduction
To achieve its goals of improving “the quality of life of patients and their families facing the problems associated with life-threatening illness, through the prevention and relief of suffering by means of early identification and impeccable assessment and treatment of pain and other problems, physical, psychosocial and spiritual Palliative Care requires that “health professionals should be educated to deliver patient-centered care as members of an interdisciplinary team” [1,2].
To facilitate this vision of patient-centered Palliative Care, care must be “delivered by intentionally created, usually relatively small work groups in health care [1,3], who are recognized by others as well as by themselves as having a collective identity and shared responsibility for a patient or group of patients” [4]. Physicians, surgeons, nurses, social workers, physiotherapists and occupational therapists who form the core of Palliative Care teams must display “the levels of cooperation, coordination and collaboration characterizing the relationships between professions in delivering patient-centered care” [4].
In most cases Palliative Care teams particularly in the Asian setting work in multidisciplinary teams, which may be seen as a ‘group of people of different healthcare disciplines, which meets together at a given time (whether physically in one place, or by video or teleconferencing) to discuss a given patient and who are each able to contribute independently to the diagnostic and treatment decisions about the patient’ as well as to elaborate upon the various biopsychosocial, spiritual and cultural determinants that may be relevant to the provision of care and support to patients and their families” [5,6].
Achieving such lofty ambitions necessitates the employment of an Interprofessional Education (IPE) approach where “students from two or more professions learn from and with each other to achieve effective collaboration and improved health outcomes” [7,8] and break down ‘professional silos’ in education and clinical care provisions to enhance collaborative and non-hierarchical relationships [9].
However whilst data suggests that IPE enables learners of various levels of experience and training from “multiple disciplines of the health care team to gain an appreciation for each other’s role within the team and perform hands-on skills while simultaneously improving teamwork” [7], the majority of IPE interventions are limited to planning sessions, presentations and training workshops. Such ‘superficial’ approaches are unlikely to support the complex, evolving, patients sensitive, context-dependent demands of “changing one’s conceptual model from disease and diagnosis to patient goals, prognosis and function” [10].
Palliative Care practitioners [10-12] have posited that mentoring could provide a means of meeting the demands of Palliative Care practice and education whilst concurrently providing career development, productivity and personal well-being for both the mentor and mentee [13]. However, whilst mentoring has enjoyed significant successes in medicine, surgery, nursing and social work, there is a dearth of data on mentoring in the context of IPE and Palliative Care. This is in part as mentoring, as a whole remains poorly defined and largely context-dependent [13-25].
This review seeks to circumnavigate the lack of a clear definition of mentoring and the absence of a universally-accepted description of mentoring practice in medicine, surgery, nursing and social work by focusing on systematic reviews, literature reviews and meta-analyses of mentoring involving undergraduates and postgraduates in clinical and academic mentoring settings.
This approach circumvents the context-dependent and goalsensitive nature of mentoring and allows for the identification of common core concepts and approaches within these specialties that will make lessons learnt translatable to mentoring in Palliative Care and form the basis for an IPE-based mentoring program. To further focus these efforts this review will be limited to mentoring relationships between mentors and mentees and focus upon discerning the characteristics, benefits and the drawbacks of mentoring within undergraduate and postgraduate medicine, surgery, nursing and social work. We have included surgical practice to provide a holistic perspective of mentoring within medical practice as a whole.
Methodology
We believe that the overview of practice trends and causal ties between mentoring approaches and their influence upon mentoring will be transferable to Palliative Care practice given the similarities of their practices. We believe that study of mentoring in nursing, medicine, social work and surgery is warranted given the central roles these specialties play in Palliative Care practice especially within the Asian setting where we aim to apply the results of this analysis to guide efforts to introduce and expand mentoring programs in Palliative Care. Single study analyses on mentoring in these specialties were deemed to be of limited use given the inherent differences in the clinical, contextual, practice and health care systems [26]. Leech et al. and Onwuegbuzie et al. [27,28] argue that use of multiple sources serves two key functions. Firstly, the authors argue that combination of data from many studies provide a better understanding of a phenomena or ‘representation’ [27-30]. Secondly, the use of data from multiple sources allows corroboration and convergence of aspects being studied improving ‘between source legitimation’ [27,28].
The absence of an a priori framework for mentoring [31] and a lack of understanding in the processes and the relationships behind the mentoring process within Palliative Care underpinned the adoption of a constructivist approach [32,33]. The Grounded Theory was employed to thematically analyze the review articles [28,34]. The process included open coding of the reviews where data was coded for and axial coding wherein similar codes were grouped together to create a theme. The individual reviewers independently determined the themes within their individual analyses and the themes were discussed in a reviewer’s meeting. Reviewers agreed upon the themes and the verified themes formed sections and subsections within the review [35]. Thematic saturation was determined by the 7th review.
Inclusion and exclusion
This review focuses on evaluating aspects of the traditional hierarchical mentoring between a senior experienced clinician and a junior clinician and/or student [20], a dyadic approach (one-to-one, senior-to-junior, face-to-face) [36] and group mentoring approaches. Excluded were peer, near-peer, leadership, family, patient, e-mentoring and youth mentoring. We also limited our attention to literature reviews, systematic reviews and meta-analyses of mentoring involving undergraduates and postgraduates in clinical, research and academic settings.
Focus was limited to mentoring in medicine, nursing and social work given that these are the most common participants of the Palliative Care multidisciplinary team in most developing nations and certainly in multicultural societies in Asia where pastoral services often play ad hoc roles in multidisciplinary teams given diverse religious beliefs and cultural sensitivity. Inclusion of surgical specialties within this review was aimed at making this process more inclusive and served to acknowledge the significant contribution that surgical mentoring has made to our understanding of mentoring as a whole.
Perspective, opinion and reflective pieces, commentaries, editorials and recommendations were excluded due to the diversity of practices described. The search was restricted to reviews in English or had English translations only. We included all study designs aimed at the personal and/or professional development of the mentee. We excluded literature reviews, systematic reviews or meta-analyses that were not exclusively focused upon adult medicine, surgery, nursing or medical social work. Other health specialties not regularly associated with adult Palliative Care such as dieticians, psychologists, chiro-practitioners, midwifery, Pediatrics, Clinical and Translational Science and Dentistry were excluded. We also excluded mentoring in Obstetrics and Gynecology given it regularly encapsulates mentoring in Obstetrics and midwifery.
We also excluded literature reviews, systematic reviews or metaanalyses on supervision, coaching, role modeling, preceptorship, sponsorship and advisor roles, given that these practices are seen as distinct from a mentoring approach.
Search and retrieval
Our literature search involved PubMed, ERIC, Cochrane Database of Systematic Reviews and Science Direct databases with the search terms: “mentor”, “mentoring”, “mentorship” “mentoring relationships” AND one of the following: “medicine”, “surgery”, “nursing” and “social work” or their combinations, to identify literature reviews, systematic reviews or meta-analyses on the mentoring of undergraduates or postgraduates in the abovementioned fields between 1st January 2000 and 31st December 2015.
Data extraction and analysis
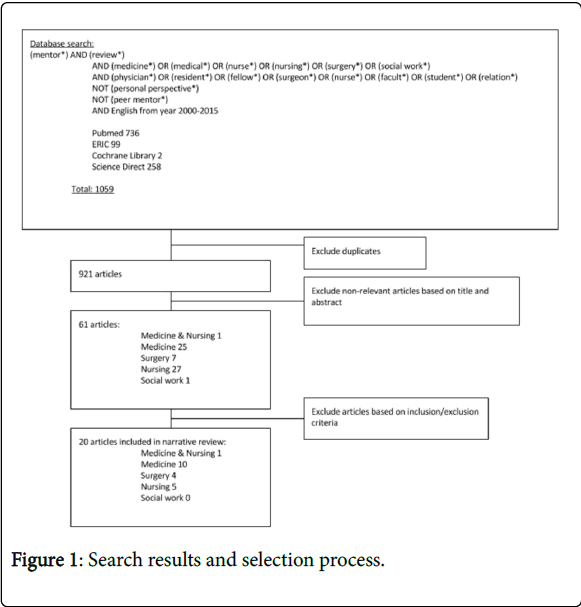
Four of the authors (MTW, WJT, MFMI, LK) carried out independent searches, scrutiny of shortlisted abstracts and reviews of all full text reviews fulfilling the inclusion criteria. Each author compiled a shortlist of papers (Figure 1). Following review of 10 full text articles the four authors unanimously agreed upon a common template to be used for the thematic analysis of the papers. Further face-to-face meeting between all 6 authors was carried out once all the authors had completed their reviews of all the full text reviews fulfilling the inclusion criteria. At this meeting the themes were discussed and agreed upon by the authors. In cases of disagreement or omissions, the authors reviewed the full text review and a unanimous decision was sought.
Results
Search results and selection process
A total of 1059 abstracts were retrieved and evaluated, 61 full-text
Of the 20 reviews included in this review, 1 review included a review of mentoring in medicine and nursing, 10 in medicine, 4 in surgery and 5 in nursing. There were no relevant reviews on mentorship in medical social work identified. articles were analyzed and 20 reviews were included in this review.
Thematic analysis revealed 6 themes including: (1) characteristics of prevailing definitions of mentoring, (2) characteristics of mentoring relationships, (3) characteristics of mentors and (4) mentees, (5) benefits of mentoring, (6) drawbacks of mentoring and finally how they all tie into painting a preferred mentoring partnership.
Components of Mentoring Relationships
Characteristics of prevailing definitions of mentoring
An analysis of the core elements within the 18 definitions of mentoring in medicine, 6 in surgery, and 12 in nursing identified in this review revealed the central importance of mentoring relationships [37-39]. Mentoring relationships are seen to display interpersonal, dynamic (or evolutionary or developmental) and reciprocal (or beneficial) features. We will discuss these features in turn.
a. Interpersonal relationship: Five medical [14,24,40-42], 1 surgical [43] and 2 nursing [44,45] reviews discussed the interpersonal qualities of mentoring relationships. In all three specialties, mentoring relationships are characterized by “personal connections” [14,44] that move beyond a “boss-employee” dynamic is critical [40,41].
Other interpersonal characteristics of mentoring relationships described in prevailing definitions of mentoring include
• Honesty and trust (4 medicine papers) [14,40-42]
• Confidentiality (3 medicine papers) [14,24,40]
• Respect (2 medicine papers, 1 surgery paper) [41,43-46]
• Open and frank communication (1 medicine paper, 2 nursing papers) [14,44,45]
• Nurturing (1 medicine paper, 1 nursing paper) [43,47] and supportive (2 medicine papers) [41,42]
b. Dynamic relationship: Three medical, 1 surgical and 2 nursing reviews described mentoring relationships as “dynamic” or “evolutionary” [41,43,44,46-47] which in turn exhibits features of flexibility and evolving practices. We discuss each feature in turn.
Flexible relationship: Two medical [14,24] and 1 surgical review [43] describe the flexible nature of mentoring relationships [24]. Changing demands upon the mentoring relationship, time constraints, evolving goals, roles and responsibilities of mentees and mentors and changing organizational factors highlight the need for mentoring relationships to adapt to ‘survive’ and continue to be relevant [24,43,46]. It also underscores the importance of the flexible nature of mentoring relationships but also that such flexibility is individualized and largely mentor and mentee dependent [14,24,43].
Stages of relationship: White et al. [41] in medicine and Dorsey et al. [47] in nursing subscribe to Kram’s 4 stages of a mentoring relationship to describe the “initiation, cultivation, separation and redefinition” [48] stages of mentoring relationships. Chen et al. [44] describe mentoring relationships as an evolution in practice from the transfer of basic clinical skills to imparting life lessons on humanistic nursing [49]. Komaratat et al. [50] suggest that there are three stages to the development of mentoring relationships which include initiation, working together and independent mentee functioning.
Sambunjak et al. and White et al. [14,41] observations of mentoring in medicine, Healy et al. [43] proposed noted that mentoring in surgery undergoes continuous cycles of change and renewal in mentoring relationships as mentees mature and develop and that this process culminates in the creation of collegial relationships between peers.
c. Beneficial relationship: Although prevailing definitions highlight the importance of “reciprocity” in mentoring relationships, nearly all the attention focuses upon the benefits accrued by the mentee [14,24,41,42,45]. Only Frei et al. [24] discussed the benefits of mentoring to mentors and mentees within medicine.
d. Other characteristics: Two papers in medicine [14,40] and 1 in nursing [51] discussed the importance of mutual interests and ideals amongst mentor and mentee. Frei et al. and Davis et al. [24,42] highlight the importance of “non-threatening” and “non-competitive” characteristics of mentoring.
Characteristics of a mentor
Seven reviews of mentoring in medicine, [14,24,41,42,52,53] 3 in surgery [38,43,54] and 6 in nursing [37,44,45,47,51,53], discussed the desired attributes of mentors. These attributes may be categorized into ‘Personal’, ‘Professional’ and ‘Undesired’ characteristics, they are collated in Table 1.
| Characteristics | Medicine | Surgery | Nursing |
|---|---|---|---|
| Personal characteristics | *Honest *Friendly and Collegial *Approachable *Patient Supportive Altruistic Understanding Responsive Nonjudgmental Reliable Calm Respectful/Courteous Committed/Dedicated |
*Honest *Friendly *Approachable Supportive Compassionate Kind, warm and non-threatening Willing to learn from themselves, mentees and others |
*Honest *Friendly and Collegial *Approachable *Patient Enthusiastic Good sense of humor Motivated Positive attitude Knowledgeable Concerned Sense of humanity |
| Professional characteristics |
Respected Senior Experienced |
- | Objective Analytical Supervisory Assessor Facilitator Academic tutor Role model |
| Undesired characteristics | Authoritative | Biased/Show favouritism | Stifling Critical Defensive |
Table 1: Characteristics of mentors
Characteristics of a mentee
Three similar categories were found in the 6 medical [14,24,40-42,52], 2 surgical [38,43] in surgery and 2 nursing [45,51] reviews that considered the characteristics of mentees, they are collated in Table 2.
| Characteristics | Medicine | Surgery | Nursing |
|---|---|---|---|
| Personal Characteristics | *Committed *Open *Proactive *Motivated/Ambitious Honest Reliable Intelligent Passion to succeed Willing to learn and reveal flaws Face their own weakness and perform self-reflection and self-critique Receptive to constructive feedback and make changes accordingly Conduct themselves in a mature and ethical manner |
*Committed *Open to learning from colleagues *Proactive responsibility Appreciate experienced senior colleagues Respect mentor’s input Voluntarily offer relevant feedback |
Conative characteristics: *motivation volition Affective characteristics: temperament emotion Independence |
| Professional Characteristics | Awareness Take responsibility for career path Reflect on clinical knowledge Learn from their mistakes Adept in synthesizing and extrapolating knowledge Mindful of mentor’s time constraints Complete assigned tasks |
- | Clinical reasoning Critically interpret data |
| Undesired Characteristics | Afraid to face: Inadequacies make necessary changes |
- | - |
Table 2: Characteristics of mentees
Benefits of mentoring
a. Benefits to mentees: Most accounts on the benefits mentoring pivot around the benefits accrued by mentee. Six postgraduate reviews in medicine [21,40,41,52-55], 24 undergraduate medical review, 3 reviews involving undergraduates and postgraduates accounts of mentoring in medicine [14,21,56] , 1 postgraduate [43] surgical review, 1 review involving postgraduates and undergraduates mentored in surgery, 3 postgraduate nurse mentoring reviews [37,44,53] and 3 undergraduate mentoring nursing reviews focused upon the benefits of mentoring for mentees [45,47,51]. These benefits are categorized according to:
• ‘Personal’ (personal life) Table 3:
| Benefits to mentees | Faculty | ||
|---|---|---|---|
| Medicine | Surgery | Nursing | |
| Personal benefits | *Career satisfaction *Psychosocial support *Increased self-confidence *Networking *Improved communication *Improved well-being *Improved socialization Career mentoring satisfaction Professionalism Sense of community Understanding institutional culture Elective advice Residency application |
*Motivation *Personal development Life mentors |
*Motivation *`Personal development *`Career satisfaction *Psychosocial support *Increased self-confidence *Networking *`Improved communication *Improved well-being *`Improved socialization Decrease anxiety and stress Personal satisfaction Empowerment Generativity Improved collegiality Improved collaboration Career dedication Reduce stress `Interpersonal skills Improved perception of organizational culture Dispel notion that a nursing professional couldn’t ask for help Sharing of ideas Increased reflection on teaching Improved responsibility for learning Enjoying a challenge Learn by turning negative experiences into learning opportunities |
Table 3: Personal benefits of mentoring to mentees
• “Professional’ (career/school performance, clinical skill, academic research/non-research skill) Table 4
| Benefits to mentees | Faculty | ||
|---|---|---|---|
| Medicine | Surgery | Nursing | |
| Professional benefits | *Career choice *Career promotion *Professional development *Professional knowledge *Staff/faculty retention *Rise in ethnic minority faculty Career-enhancing factor Career preparation Faculty productivity Financially-rewarding practice Increased compensation Develop high-quality practice Institution support Navigate academic environment Society and committee nominations Interest in research Research preparation Research skills Research productivity Research opportunity Increased time allocation for research Increased publications Academic promotions Increased grants Advancing research agenda Increased thesis completion More likely to subsequently mentor Progress in dealing with specialist literature and computers |
*Career choice | *Career promotion *Professional development *Professional knowledge *Staff retention Career competence Career performance Improved counselling skills Apply theoretical knowledge Increased evidence-based practice Internalization stage for lifelong learning Improved participation Improved exam results Increased recruitment Increased likelihood of graduation Assist role transition Instills future practices Reduced time learning new skills Reduced frequency employing trial-and-error methods Increase new research investigators *Rise in ethnic minority faculty |
Table 4: Professional benefits of mentoring to mentees
b. Benefits to mentors: The benefits of mentoring for mentors in postgraduate medicine revolve around psychosocial benefits, gaining new knowledge and skills, experience, opportunity to share knowledge and experience, satisfaction and pride in a mentee's success, giving back to the profession, gaining a new collaborator, recognition from peers, credit for academic promotion, propagation of and increased willingness to mentor. In undergraduate programs, there were increased professional recognition and accelerated research productivity for mentors [24].
One undergraduate nursing review found that mentoring enhanced a mentor’s self-worth, teaching satisfaction, career revitalization, improved leadership skills, and reignited the passion for mentoring [47].
c. Benefits to other shareholders: The benefits of mentoring in medicine and surgery for patient care include improved patient survival and outcomes [57] and reduced lengths of stay [53]. There were also lower surgical morbidities [54].
Hosting mentoring programs reduced employee turnover and medical negligence rates within the institution. Consequent institutional stability, continuity and increased minority representation enhanced the reputations of host organizations [47].
Drawbacks of mentoring
a. Drawbacks to mentees: Mentors using mentee’s work to advance their own career, mentor misuse of power and overdependence upon mentors are common concerns featured in reviews of mentoring in medicine [41,52,56], surgery [43,54] and nursing [45].
b. Drawbacks to mentors: A lack of recognition and financial compensation for mentoring efforts featured strongly in mentoring reviews in medicine [21] and nursing [45].
Discussion
Analysis of mentoring practice in nursing, medicine and surgery reveals consistent themes within mentoring practice. These include interpersonal and dynamic relationships and mentoring outcomes, which suggest that a common mentoring approach could be adopted with the multidisciplinary setting of Palliative Care. We discuss each aspect in turn.
Interpersonal relationship
Building upon the key themes identified in this review, it is evident that at the heart of a proposed IPE-based mentoring program in Palliative Care must be interpersonal relationships. This entails nurturing confidential, reciprocal, trusting personal ties between mentee, mentor and host organization within a safe mentoring environment. The impact of mentors, mentees and the host organization must be taken into account to realize the unique interpersonal relationship that must underpin this process. Consistent efforts to facilitate interpersonal relationships are evident across all the specialties review and include (1) selection of mentors with the desired characteristics, and training them to provide appropriate, timely, effective, specific and holistic support and feedback, (2) selecting mentee’s with the desired characteristics identified in this review and matching of mentees to appropriate mentors, suitable projects and effective supervision and oversight, (3) providing appropriate financial and administrative support for the program and (4) the creating and nurturing an effective mentoring environment.
Dynamic relationship
Reviews of mentoring in all 3 healthcare disciplines suggest that mentoring relationships evolve over time and with the development and strengthening of relational ties within the mentoring relationship. The ultimate goal of a maturing mentoring relationship is for friendship to blossom and the development of a collegial relationship between peers.
Facilitating this change is the host organization, which provides the resources required for mentors to support mentees over long periods of time and across different sites and creates and nurtures a viable mentoring environment for mentees and mentors to develop.
Mentoring outcomes
There is consistency in the mentoring outcomes seen across the specialties reviewed suggesting similarities in mentoring approach employed despite inherent differences in the clinical setting, context, goals and health care settings they were employed in. Homogeneity in these findings also validate the approach taken in this study to concentrate on a macroscopic perspective of mentoring evident in reviews of mentoring rather than considerations of individual reports that are mired in local health care practices and local geopolitical considerations.
It is also evident from the theme that host organizations play a critical role in mentoring. The role of host organization in facilitating and supporting mentoring relationships is critical to realizing the benefits of mentoring and in the negation of the ill effects of mentoring discussed earlier. Any IPE-based mentoring program must consider the influence of the host organization and indeed the design of the mentoring program (we have discussed these issues elsewhere).
Limitations and Further research
The primary limitations of this study is the assumption that there are commonalities in mentoring practices across the specialties and that these common approaches can be amalgamated effectively to form the basis of a mentoring approach in Palliative Care. The presence of a variety of definitions and theories of mentoring complicate the analysis of the data and compromise the conclusions detailed here. The inclusion and exclusion criteria employed here make it difficult to make accurate comparisons of review data across the disciplines. With most reviews outside North America, Europe and Australia conclusions drawn may not be adaptable to other mentoring settings. Heterogeneity in the mentoring objectives, clinical settings, healthcare systems, mentoring approaches employed, duration of mentoring relationships and mentee- and mentor-dependent factors also hinders accurate conclusions being drawn.
Finally, there is no data available to suggest that mentoring lends itself to an IPE-based mentoring approach in Palliative Care.
A Potential IPE Approach to Mentoring
Whilst the concerns raised are valid, consistencies in the desired characteristics of mentors and mentees, matching processes, consistencies in the appropriate financial and administrative support adopted by prevailing practices and consistent descriptions of effective mentoring environments across the specialties reviewed for the program evidenced in this review does suggest that an IPE framework for mentoring in Palliative Care is possible particularly when both processes pivot on building relationships. Some of the critical qualities required of mentoring, mirror established requirements for interprofessional collaboration including effective communication [58] and the building and clarification of professional roles [59]. However whilst many prevailing IPE-based training approaches such as the use of simulation [60-64], didactic lectures [62,64-66], group discussions and collaborations [60,62,64-68] as well as clinical rotations [65,68] are applicable to mentoring in Palliative Care, it is also evident that prevailing IPE approaches need to be adapted to the Palliative Care setting.
Design of more mentoring specific IPE approaches demands a ‘return to the drawing board’ and consideration of the learning theories that will guide this process. Conceptual analysis [69] suggests that IPE is built upon elements of multiple learning theories such as constructivism (learning through experiences and discussion) [70], cognitivism (organisation of information via cognitive processes) [69] and humanism (learning by self-actualisation) [71]. The cognitive apprenticeship model, which focuses upon “learning about practice” [72,73] does embrace many of the core aspects of these theories and does appear to reflect Palliative Care practice that does see junior clinicians building upon their training and enhancing it with a multidimensional perspective drawn from instruction and holistic support from various members of the multiprofessional team. Furthermore the cognitive apprenticeship model does lend itself to the Palliative Care instructional approach that sees mentors model the desired behavior and practice for their mentees and “trains the next generation of experts” [74] and independent Palliativists. Similarly multiprofessional ‘apprenticeship’ advocated by the adapted cognitive apprenticeship model will allow for multiple mentoring relationships [75] that facilitate learning, skills training and personal advice from multiple mentors from different clinical backgrounds [5,74]. Simulation and community projects can be done under the purview of mentors from a variety of backgrounds, who can then provide feedback and track progress, facilitating multiprofessional and multidimensional learning [76,77]. Similarly amalgamation of structural and administrative changes such as scheduling [72] and the incorporation of an appropriate mentoring framework will allow for the effective and holistic support of Palliative Care mentees.
Conclusion
If Palliative Care is to continue to expand and take its place within medical practice, it is evident that IPE-based mentoring is required. As with mentoring in other clinical fields such as geriatrics, rehabilitation medicine, pediatrics and oncology any effort to create an IPE-based mentoring program must pay close attention to nurturing the mentoring ties within mentoring relationships. However, it is clear that prevailing data only hints at the appropriate process to be adopted and further studies are required. This review serves then to point to the areas that require urgent attention. These include understanding of mentoring relationships and the dynamics within mentoring processes. It is evident that further studies are required not only to evaluate context-specific mentoring in Palliative Care but the learning theories that underpin it and guide its applications. It is only then can mentoring aid Palliative Care in achieving its overall goals in an effective manner.
Acknowledgements
The authors would like to dedicate this paper to Dr S Radha Krishna and Dr Deborah Watkinson whose advice and ideas were integral to the success of this study and who sadly passed away during the writing of this paper.
References
- (1988) Learning Together to Work Together for Health: Report of a WHO Study Group on Multiprofessional Education of Health Personnel: the Team Approach pp: 72.
- Stephen R, Connor MCSB (2014) Global Atlas of Palliative Care at the End of Life. Worldwide Palliative Care Alliance pp: 5.
- (2003) Committee on the Health Professions Education Summit, Board on Health Care Services, Institute of Medicine. Health Professions Education: A Bridge to Quality. National Academies Press pp: 192.
- (2011) Core Competencies for Interprofessional Collaborative Practice. Report of an expert panel. Interprofessional Education Collaborative.
- Krishna LR (2012) Best interests determination within the Singapore context. Nurs Ethics 19(6):787-799.
- (2007) Manual for Cancer Services. UK Government of Health.
- Reeves S, Scott R, Laure P, Joanne G, Della F, et al. (2013) Interprofessional education: effects on professional practice and healthcare outcomes.
- Gilbert JHV, Yan J, Hoffman SJ (2010) A WHO report: framework for action on interprofessional education and collaborative practice. J Allied Health 39: 196-197.
- Frenk J, Chen L, Bhutta ZA, Cohen J, Crisp N (2010) Health Professionals for a New Century: Transforming Education to Strengthen Health Systems in an Interdependent World. The Lancet 376: 1923-1958.
- Arnold RM (2005) Mentoring the next generation: a critical task for palliative medicine. J Palliat Med 8:696-698.
- Periyakoil VS, Von Gunten CF (2007) Mainstreaming palliative care. J Palliat Med 10: 40-42.
- Jackson V, Arnold RM (2010) Clinician educators navigating the world of academic palliative medicine. J Palliat Med 13:1139.
- Sambunjak D, Straus SE, Marusic A (2010) A systematic review of qualitative research on the meaning and characteristics of mentoring in academic medicine. J Gen Intern Med 25:72-78.
- Stamm M, Buddeberg-Fischer B (2011) The impact of mentoring during postgraduate training on doctors’ career success. Med Educ 45: 488-496.
- Zhang Y, Qian Y, Wu J, Wen F, Zhang Y (2016) The effectiveness and implementation of mentoring program for newly graduated nurses: A systematic review. Nurse Educ Today 37:136-144.
- Maramaldi P, Gardner D, Berkman B, Ireland K, D’Ambruoso S, et al. (2004) Mentoring new social work faculty:agerontological perspective. GerontolGeriatrEduc 25:89-106.
- Duffy K, Kathleen D, Belinda E (2014) Enhancing the collaborative review of NHS Education for Scotland’s mentor preparation framework. Nurs Manage 21: 24-31.
- Damaskos P, Penelope D, Gardner DS (2015) Cultivating a Culture of Mentorship in Palliative Social Work. J Soc Work End Life Palliat Care 11: 101-106.
- Chow AYM (2013) Developing Emotional Competence of Social Workers of End-of-Life and Bereavement Care. Br J Soc Work.
- Kashiwagi DT, Varkey P, Cook DA (2013) Mentoring programs for physicians in academic medicine: a systematic review. Acad Med 88: 1029-1037.
- Buddeberg-Fischer B, Barbara BF, Katja-Daniela H (2006) Formal mentoring programmes for medical students and doctors – a review of the Medline literature. Med Teach 28: 248-257.
- Wolak E, Eric W, Meghan M, Sara Q, Catherine M, Susan L (2009) Perceptions Within a Mentorship Program. Clin Nurse Spec 61-7.
- Frei E, Esther F, Martina S, Barbara BF (2010) Mentoring programs for medical students - a review of the PubMed literature 2000 - 2008. BMC Med Educ.
- Huybrecht S, Loeckx W, Quaeyhaegens Y, De Tobel D, Mistiaen W (2011) Mentoring in nursing education: perceived characteristics of mentors and the consequences of mentorship. Nurse Educ Today 31: 274-278.
- Andrews M, Chilton F (2000) Student and mentor perceptions of mentoring effectiveness. Nurse Educ Today 20: 555-562.
- Popay J, Roberts H, Sowden A, Petticrew M, Arai L, et al. (2006) Guidance on the Conduct of Narrative Synthesis in Systematic Reviews. ESRC Methods Programme.
- Leech NL, Onwuegbuzie AJ (2007) An array of qualitative data analysis tools: A call for data analysis triangulation. SchPsychol Q 22:557-584.
- Onwuegbuzie AJ, Leech NL, Collins KMT (2012) Qualitative Analysis Techniques for the Review of the Literature. The Qualitative Report 17: 1-30.
- Leech NL, Onwuegbuzie AJ (2008) Qualitative data analysis: A compendium of techniques and a framework for selection for school psychology research and beyond. SchPsychol Q 23: 587-604.
- Leech NL, Onwuegbuzie AJ (2010) Guidelines for Conducting and Reporting Mixed Research in the Field of Counseling and Beyond. J Counsel Dev 88: 61-9.
- Aagaard EM, Hauer KE (2003) A cross-sectional descriptive study of mentoring relationships formed by medical students. J Gen Intern Med 18: 298-302.
- Kennedy TJT, Lingard LA (2006) Making sense of grounded theory in medical education. Med Educ40: 101-108.
- Creswell JW (2014) Educational Research: Planning, Conducting, and Evaluating Quantitative and Qualitative Research pp: 672.
- Lingard L, Albert M, Levinson W (2008) Grounded theory, mixed methods, and action research. BMJ 7: 337-367.
- Burnard P, Gill P, Stewart K, Treasure E, Chadwick B (2008) Analysing and presenting qualitative data. Br Dent J 204: 429-432.
- Charles C, Healy AJW (1990) Mentoring Relations: A Definition to Advance Research and Practice. Educational Researcher 19: 17-21.
- Poronsky CB (2012) A literature review of mentoring for RN-to-FNP transition. J NursEduc 51: 623-631.
- Patel VM, Warren O, Ahmed K, Humphris P, Abbasi S, et al. (2011) How can we build mentorship in surgeons of the future? ANZ J Surg 81: 418-424.
- Lafleur AK, White BJ (2010) Appreciating mentorship: the benefits of being a mentor. Prof Case Manag 15: 305-311.
- Sambunjak D, Straus SE, Marusic A (2010) A systematic review of qualitative research on the meaning and characteristics of mentoring in academic medicine. J Gen Intern Med 25: 72-78.
- White HK, Buhr GT, Pinheiro SO (2009) Mentoring: a key strategy to prepare the next generation of physicians to care for an aging America. J Am GeriatrSoc 57: 1270-1277.
- Davis OC, Nakamura J (2010) A proposed model for an optimal mentoring environment for medical residents: a literature review. Acad Med 85: 1060-1066.
- Healy NA, Cantillon P, Malone C, Kerin MJ (2012) Role models and mentors in surgery. Am J Surg 204: 256-261.
- Chen CM, Lou MF (2014) The effectiveness and application of mentorship programmes for recently registered nurses: a systematic review. J NursManag 22: 433-442.
- Wilkes Z (2006) The student-mentor relationship: a review of the literature. Nurs Stand 20: 42-47.
- Sambunjak D, Straus SE, Marusic A (2010) A systematic review of qualitative research on the meaning and characteristics of mentoring in academic medicine. J Gen Intern Med 25: 72-78.
- Dorsey LE, Baker CM (2004) Mentoring undergraduate nursing students: assessing the state of the science. Nurse Educ 29: 260-265.
- Kram KE (1983) Phases of the Mentor Relationship. Acad Manage J 26: 608-625.
- Haggerty LA, Grace P (2008)Clinical wisdom: the essential foundation of “good” nursing care. J Prof Nurs 24: 235-240.
- Komaratat S, Oumtanee A (2009) Using a mentorship model to prepare newly graduated nurses for competency. J ContinEducNurs 40: 475-480.
- Jokelainen M, Turunen H, Tossavainen K, Jamookeeah D, Coco K (2011) A systematic review of mentoring nursing students in clinical placements. J ClinNurs 20: 2854-2867.
- Yeung M, Nuth J, Stiell IG (2010) Mentoring in emergency medicine: the art and the evidence. CJEM 12: 143-149.
- Abdullah G, Rossy D, Ploeg J, Davies B, Higuchi K, et al. (2014) Measuring the effectiveness of mentoring as a knowledge translation intervention for implementing empirical evidence: a systematic review. Worldviews Evid Based Nurs. 11: 284-300.
- Entezami P, Pouya E, Franzblau LE, Chung KC (2011) Mentorship in surgical training: a systematic review. Hand 7:30-36.
- Beech BM, Calles-Escandon J, Hairston KG, Langdon SE, Latham-Sadler BA, et al. (2013) Mentoring programs for underrepresented minority faculty in academic medical centers: a systematic review of the literature. Acad Med 88: 541-549.
- Sambunjak D, Straus SE, Marusi�? A (2006) Mentoring in academic medicine: a systematic review. JAMA 296: 1103-1115.
- Hay D, Khan MS, Van Poppel H, Van Cleynenbreugel B, Peabody J, et al. (2015) Current status and effectiveness of mentorship programmes in urology: a systematic review. BJU Int 116:487-494.
- Körner M, Bütof S, Müller C, Zimmermann L, Becker S, et al. (2016) Interprofessional teamwork and team interventions in chronic care: A systematic review. J Interprof Care 30: 15-28.
- Kvarnström S (2008) Difficulties in collaboration: a critical incident study of interprofessional healthcare teamwork. J Interprof Care 22: 191-203.
- Odegard PS, Robins L, Murphy N, Belza B, Brock D, et al. (2009) Interprofessional initiatives at the University of Washington. Am J Pharm Educ 73:63.
- Muller-Juge V, Cullati S, Blondon KS, Hudelson P, Maître F, et al. (2014) Interprofessional collaboration between residents and nurses in general internal medicine: a qualitative study on behaviours enhancing teamwork quality. PLoS One 9:e96160.
- Kahaleh AA, Danielson J, Franson KL, Nuffer WA, Umland EM (2015) An Interprofessional Education Panel on Development, Implementation, and Assessment Strategies. Am J Pharm Educ 79:78-80.
- Watt-Watson J, Siddall PJ, Carr E (2012) Interprofessional pain education: the road to successful pain management outcomes. Pain Manag 2: 417-420.
- Bridges DR, Davidson RA, Odegard PS, Maki IV, Tomkowiak J (2011) Interprofessional collaboration: three best practice models of interprofessional education. Med Educ Online.
- Gilligan C, Outram S, Levett-Jones T (2014) Recommendations from recent graduates in medicine, nursing and pharmacy on improving interprofessional education in university programs: a qualitative study. BMC Med Educ 18: 14-52.
- Hall LW, Zierler BK (2015) Interprofessional Education and Practice Guide No. 1: developing faculty to effectively facilitate interprofessional education. J Interprof Care 29: 3-7.
- Brennan CW, Olds DM, Dolansky M, Estrada CA, Patrician PA (2014) Learning by doing: observing an interprofessional process as an interprofessional team. J Interprof Care 28: 249-251.
- Head BA, Schapmire T, Hermann C, Earnshaw L, Faul A, Jones C, et al. (2014) The Interdisciplinary Curriculum for Oncology Palliative Care Education (iCOPE): meeting the challenge of interprofessional education. J Palliat Med 17: 1107-1114.
- Olenick M, Allen LR, Smego RA (2010) Interprofessional education: a concept analysis. Adv Med EducPract. 1: 75-84.
- Vygotsky LS, Cole M (1978) Mind in Society. Harvard University Press pp: 159.
- Maslow AH (1943) A theory of human motivation. Psychol Rev 50: 370-396.
- Burring SM (2009) Interprofessional education supplement: keys to successful implementation of interprofessional education: learning location, faculty development, and curricular themes. Am J Pharm Educpp: 4.
- Collins A, Brown JS, Newman SE (1988) Cognitive apprenticeship: Teaching the craft of reading, writing and mathematics 8: 2-10.
- Dow AW, DiazGranados D, Mazmanian PE, Retchin SM (2013) Applying organizational science to health care: a framework for collaborative practice. Acad Med 88: 952-957.
- Higgins MC, Kram KE (2001) Reconceptualizing Mentoring at Work: A Developmental Network Perspective. Academy of Management Review 26: 264-288.
- Headrick LA, Shalaby M, Baum KD, Fitzsimmons AB, Hoffman KG, et al. (2011) Exemplary care and learning sites: linking the continual improvement of learning and the continual improvement of care. Acad Med. 86: e6-e7.
- Steinert Y (2011) Commentary: Faculty development: The road less traveled. Acad Med 86: 409-411.
Relevant Topics
- Caregiver Support Programs
- End of Life Care
- End-of-Life Communication
- Ethics in Palliative
- Euthanasia
- Family Caregiver
- Geriatric Care
- Holistic Care
- Home Care
- Hospice Care
- Hospice Palliative Care
- Old Age Care
- Palliative Care
- Palliative Care and Euthanasia
- Palliative Care Drugs
- Palliative Care in Oncology
- Palliative Care Medications
- Palliative Care Nursing
- Palliative Medicare
- Palliative Neurology
- Palliative Oncology
- Palliative Psychology
- Palliative Sedation
- Palliative Surgery
- Palliative Treatment
- Pediatric Palliative Care
- Volunteer Palliative Care
Recommended Journals
- Journal of Cardiac and Pulmonary Rehabilitation
- Journal of Community & Public Health Nursing
- Journal of Community & Public Health Nursing
- Journal of Health Care and Prevention
- Journal of Health Care and Prevention
- Journal of Paediatric Medicine & Surgery
- Journal of Paediatric Medicine & Surgery
- Journal of Pain & Relief
- Palliative Care & Medicine
- Journal of Pain & Relief
- Journal of Pediatric Neurological Disorders
- Neonatal and Pediatric Medicine
- Neonatal and Pediatric Medicine
- Neuroscience and Psychiatry: Open Access
- OMICS Journal of Radiology
- The Psychiatrist: Clinical and Therapeutic Journal
Article Tools
Article Usage
- Total views: 12911
- [From(publication date):
November-2016 - Apr 05, 2025] - Breakdown by view type
- HTML page views : 11956
- PDF downloads : 955