COVID-19: Spleen Involvement or Coincidence
Received: 02-Feb-2021 / Accepted Date: 16-Feb-2021 / Published Date: 23-Feb-2021 DOI: 10.4172/2165-7386.s1.10001
Abstract
A 62-year-old man presented a history of fever, cough, left thoracic pain, left hypochondrium discomfort, asthenia and anorexia for the past week. He had lost 6 Kg in the past month. His TAP CT revealed extensive densification of the left lung lower lobe and a spleen enlargement of 22 cm in its longitudinal axis. He presented anaemia, lymphopenia, elevated CRP and LDH. He had a SARS-CoV-2 positive test, Streptococcus pneumoniae positive urinary serology and blood culture. 20 days later he repeated his TAP CT showing pneumonia imaging evolution and a 21 cm spleen longitudinal axis and one month later he repeated an abdominal US revealing a 17.7 cm diameter spleen. HBV, HCV, HIV, EBV and CMV serologies were negative. Bone marrow immunophenotyping suggested splenic marginal zone lymphoma.
Keywords: Splenomegaly; Spleen; Lymphoma; COVID-19
Abbreviations
ARDS: Acute Respiratory Distress Syndrome; CM: Centimeter; CMV: Cytomegalovirus; COVID-19: Coronavirus Disease 2019; CRP: C-Reactive Protein; CT: Computed Tomography; EBV: Epstein-Barr Virus; ER: Emergency Room; G-CSF: Granulocyte-Colony Stimulating Factor; HBV: Hepatitis B Virus; HCV: Hepatitis C Virus; HIV: Human Immunodeficiency Virus; KG: Kilogram; LDH: Lactic Dehydrogenase; SARSCoV2: Severe Acute Respiratory Syndrome Coronavirus 2; SMZL: Splenic Marginal Zone Lymphoma; TAP: Thoracoabdominopelvic; US: Ultrasound
Learning Points
• Splenomegaly is a common finding in multiple diseases mostly associated with haematologic disorders and viral infections.
• SMZL is a low-grade B-lymphoma characterized mostly for nonspecific symptoms, cytopenia and splenomegaly with good prognosis when detected and treated early.
• COVID-19 global pandemic patients mostly present respiratory symptoms leading to severe pneumonia and ARDS, although there are other organs directly involved by SARS-CoV-2 described in literature. Spleen involvement has been suggested recently in the literature.
Introduction
Since December 2019, there has been an outbreak of a novel coronavirus (SARS-CoV-2) worldwide-COVID-19 infection. Although COVID-19 global pandemic patients present mainly respiratory symptoms, there are extra pulmonary manifestations directly caused by SARS-CoV-2. Spleen involvement has been suggested recently in the literature, also due to thrombotic phenomena caused by SARS-CoV-2 infection pro-inflammatory state.
This clinical case enhances spleen involvement in these patients.
Case Description
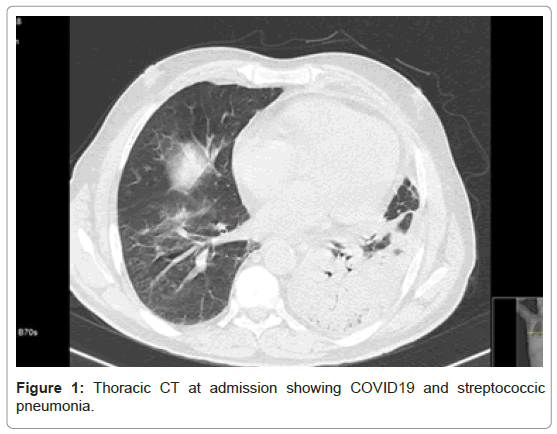
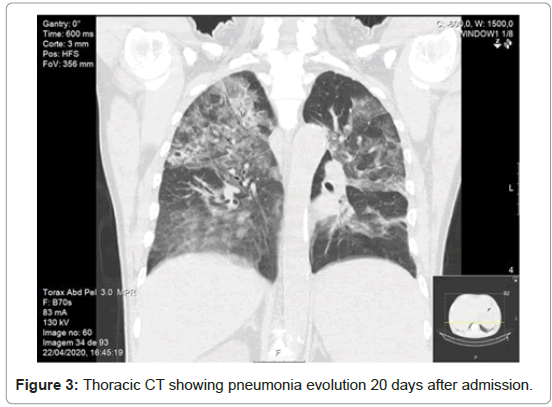
TA 62-year-old man presented at the ER on 1st April 2020 with a history of fever, cough, left thoracic pleuritic pain, left hypochondrium discomfort, asthenia and anorexia for the past week and a 6 kg loss in the past month. He presented a left hypochondrium mass almost reaching his umbilicus. He performed a TAP CT revealing an extensive densification in the lower lobe of the left lung (Figure 1) and a spleen enlargement of approximately 22 cm in its longitudinal axis (Figure 2). He presented microcytic and hypochromic anaemia (Haemoglobin 10.3 g/dL), lymphopenia (700 lymphocytes), elevated c-reactive protein (251 mg/L) and LDH (253 UI/L). He presented a SARS-CoV-2 positive test, Streptococcus pneumoniae positive urinary serology and blood culture. He started on Amoxicillin-Clavulanate, Hydroxychloroquine and Lopinavir/Ritonavir for 10 days with good clinical response. After treatment, the patient repeated a TAP CT showing pneumonia imaging progression with bilateral multilobed ground glass and crazy-paving pattern and a 21 cm spleen longitudinal axis (Figure 3). At the 20th day, the patient presented recurring fever, cough, purulent sputum and respiratory insufficiency, initiated broad-spectrum antibiotics, steroids and oxygen supplementation for nosocomial pneumonia suspicion and resolved after 7 days.
One month after diagnosis he repeated an abdominal ultrasound revealing a slightly smaller spleen with 17.7 cm of diameter.
Blood smear did not reveal alterations. HBV, HCV and HIV serologies, EBV and CMV were negative. A bone marrow puncture could only be performed after the patient presented a SARS-CoV-2 negative test, which only happened on the 50th day after admission. Bone marrow immunophenotyping revealed a monoclonal B population, compatible with a B lymphoproliferative disease with small size cells (IgM+, IgG+, lambda light chain+, CD19+, CD20+, CD5-, CD10-, CD23-, FMC7+, CD79b+, CD11c-, CD25-, CD103-, CD9-) suggesting a splenic marginal zone lymphoma.
He was discharged on the 58th day presenting 9.8 g/dL of hemoglobin, 6000 leucocytes and 107000 platelets and was oriented to Hematology consultation in the next week.
Discussion
Splenomegaly is a common finding in multiple diseases. The most common aetiologies include haematologic and liver disorders (approximately 1/3 each) and infection in approximately ¼ [1].
SMZL constitutes <1% of all non-Hodgkin lymphomas and up to 25% of low grade B cell neoplasms in splenectomy specimens and it usually occurs at a median age of 65 to 70 years with no gender predominance [2]. It usually expresses surface immunoglobulin, B cell antigens (CD19, CD20, CD22), BCL2. It doesn’t express CD10, CD25, or CD103 and CD5 is usually negative. Clinical features in SMZL patients are splenomegaly, lymphocytosis and cytopenia, which are often related to hypersplenism. Almost every patient experience left hypochondrium discomfort due to moderate to massive splenomegaly [2]. The relative 5-year overall survival rate was high in approximately 80% [2].
The COVID-19 viral outbreak was first reported in Wuhan, China in December 2019 and successively spread worldwide as a global pandemic. It is mostly associated with respiratory symptoms that may lead to severe pneumonia and ARDS, although it can affect other target organs as acute cardiac, kidney and liver injury, cardiac arrhythmias, rhabdomyolysis, coagulopathy and shock [3]. COVID-19 initial CT includes bilateral multilobed ground-glass opacification with peripheral or posterior distribution mainly in the lower lobes [4]. Follow-up CT usually presents increasing ground-glass number and size opacifications, multifocal consolidative opacities, septal thickening and crazy-paving pattern development [4]. Greatest severity of CT findings is visible around day 10 after the symptom onset and clinical and imaging improvement usually occur after week 2 of the disease [4]. The patient was admitted in the first phase of COVID-19 outbreak and since then, multiple scientific evidence has been released changing COVID-19 treatment options. Nowadays, latest evidence suggests that a steroid is associated with lower mortality [5].
Both SMZL and COVID-19 usually present with nonspecific symptoms as anorexia, asthenia, fatigue, myalgias, fever, cytopenia and elevation of inflammatory markers [2,3].
Although there is very scarce data regarding spleen involvement in COVID-19, it is suggested that the spleen may be one of the target organs directly involved by SARS-CoV-2 virus, decreasing significantly the number of peripheral blood lymphocytes and the patient’s immune function [6].
To our knowledge, steroids are also included in chemotherapy treatment options of marginal lymphomas [7], which could explain the reduction of the spleen length during hospitalization.
Conclusion
This case is particularly interesting because it showed that the spleen can be one of the target organs directly involved by the SARS-CoV- 2 virus and also because diagnosing the underlying hematologic disease allowed early treatment and prevention of disease progression.
References
- O'Reilly RA (1998) Splenomegaly in 2,505 patients at a large university medical center from 1913 to 1995, 1963 to 1995: 449 patients. West J Med 169:88.
- Liu L, Wang H, Chen Y, Rustveld L, Liu G, et al. (2013) Splenic marginal zone lymphoma: A population-based study on the 2001-2008 incidence and survival in the United States. Leuk Lymphoma 54:1380-1386.
- Berlin DA, Gulick RM, Martinez FJ (2020) Severe covid-19. N Engl J Med.
- Salehi S, Abedi A, Balakrishnan S, Gholamrezanezhad A (2020) Coronavirus disease 2019 (COVID-19): A systematic review of imaging findings in 919 patients. Am J Roentgenol 215:87-93.
- Horby P, Lim WS, Emberson JR (2020) RECOVERY collaborative group (2020) dexamethasone in hospitalized patients with Covid-19: Preliminary report. N Engl J Med.
- X Xu, Chang XN, Pan HX, Su H, Huang B, et al. (2020) Pathological changes of the spleen in ten patients with Coronavirus disease 2019 (COVID-19) by postmortem needle autopsy 49:576-582.
- Zucca E, Arcaini L, Buske C, Johnson PW, Ponzoni M, et al. (2020) Marginal zone lymphomas: ESMO clinical practice guidelines for diagnosis, treatment and follow-up. Ann Oncol 31:17-29.
Citation: Costa M, Formigo M, Bessa I, Sarmento H, Cotter J (2021) COVID-19: Spleen Involvement or Coincidence. J Infect Dis Ther S1: 001. DOI: 10.4172/2165-7386.s1.10001
Copyright: © 2021 Costa M, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 4184
- [From(publication date): 0-2021 - Apr 03, 2025]
- Breakdown by view type
- HTML page views: 3413
- PDF downloads: 771