Correlation Research on Professional Counselling and Hiv/Aids Treatment Default at Chiradzulu and Queen Elizabeth Hospital-a Cohort Study
Received: 01-Jun-2020 / Accepted Date: 16-Jun-2020 / Published Date: 23-Jul-2020 DOI: 10.4172/2471-9846.1000244
Abstract
Counseling provided by trained professionals can make a profound impact on the lives of individuals, families and communities. This service helps people navigate difficult life situations, to better understand the reasons why patients default from antiretroviral treatment (ART) programmes while they are being counselled, to help design interventions that improve treatment retention and ultimately, patient outcomes through professional counseling in order to promote change that improves the quality of life for not only their clients, but the public, Hampered in part by lack of empirical evidence for quality of life, which is affecting immune system exposing clients to opportunistic infections.
There is high rate of clients stopping taking the drug that assist them in suppressing an HIV Virus called Ante retroviral drugs despite available counseling services at their clinics. Therefore a research was conducted to determine the relationship between professional counseling and HIV treatment default, AIDS as a disease carries stigma because of the way it is acquired by the people .Traditionally, our society view AIDS affected people as promiscuous and tend to isolate them as bad mannered It is against this background that professional counselling needs to come in to help these people to heal psychologically. Counseling as a profession is supported by quality assurance structures , implemented by an expert group or government body , that mandate the specific knowledge and skills necessary to be a professional counsellor.
Prospective cohort study at two treatment sites in Southern Malawi, Queen Elizabeth Central Hospital) and Chiradzulu district hospital followed by qualitative interviews with patients on treatment and that had defaulted ,deductive and inductive approach had been used, deductive in the sense that the research used the existing theories and models, the study was limited to public hospitals which have well established ART clinics . The research was designed to use cross sectional explorative research. Quantitative data was collected using questionnaires, observations to achieve objectives. Counselling process was used to study the relationship of the parameters. Correlation of default rate to the practice of standard counselling to prove professionalism which is Comparison of adherence to treatment and counsellors qualification. Correlation regression analysis was done.
Respondents overwhelmingly defaulted there treatment, Counsellors were unable to conduct the proper counselling process due to the infrastructure ,no special rooms for counselling ,compromised competency of counsellors. Components had strong positive correlation between default rate and professional counselling. With a better understanding of the reasons for defaulting, interventions can be designed that improve treatment retention and ultimately, patient outcomes. This study argues for introduction of professional counseling cadres in Anteretroviral treatment Clinics of Malawi and policy changes designed to reduce the financial and time burden for follow up of lost to follow up clients , tie burden of HIV profession Counseling and reduce logistic barriers, Privacy has to be addressed and adopting extended and weekend clinic, more awareness on effects of treatment default and community sensitization in reducing stigma.
Keywords: World Health Organisation; Counseling; Couples Counseling; Hiv
Introduction
World health organisation, UNAIDS 2007, PITC Guidelines recommended that Post-test counselling is an integral component of the HIV testing process. All individuals undergoing HIV testing must be counselled when their test results are given, regardless of the test result.
Counseling is essentially a confidential dialogue between an individual/couple and a counsellor, aimed at enhancing individual's abilities to make personal decisions. Pre-test counseling, post-test counseling, adherence counseling, couples counseling, crisis counseling and grief or bereavement counseling are the types of counseling practiced in the fields of HIV/AIDS. For achieving behavioural goals, counsellors need to have empathy and inculcate verbal and non-verbal counseling skills. Correct and timely documentation helps in enhancing quality of counseling care given to the client. Counsellors’ ability to identify the cause or trigger for client's problems and empower the clients in working out a plan to resolve their crisis is essential. The actions taken by the counsellors could be continuously reviewed by the supervisors to ensure their growth as a counsellor. Skill building needs of counsellors can be identified through direct observations, exit interviews of the clients, reviewing counsellor’s notes and time-to-time evaluations.
According to National AIDS Control Programme National Institute of Health Islamabad, Pakistan various studies throughout the world suggest that HIV/AIDS counselling assists people to make informed decisions, cope better with their condition, lead more positive lives, and prevent HIV transmission. HIV/AIDS counselling is important because infection with HIV is a lifelong phenomenon and during the course of the infection, a broad range of physical, social and psychological needs and problems are likely to be experienced. The changing nature of the illness imposes a variety of psychological and emotional strains on individuals and those closest to them. HIV/ AIDS counselling is a dialogue between a client and a care provider aimed at enabling the client to cope with stress and to make personal decisions related to HIV/AIDS. The counselling process includes the evaluation of personal risk of HIV transmission and the facilitation of preventive behaviour.
HIV/AIDS counseling is a process that begins with the client's first contact either with an HIV/AIDS counseling service or with the care system for HIV-related needs. In the context of HIV/AIDS, the care system includes all health and social service facilities, both governmental and non-governmental, where individuals receive care and social support. The counseling process continues through a referral network to various community and social support agencies, according to the need of the individual and the family affected by or worried about HIV. Counseling goals are to provide psychosocial support to those whose lives have been affected by HIV and to prevent HIV infection and its transmission to other people.
East and Southern Africa is the region hardest hit by HIV. It is home to around 6.2% of the world’s population but over half (54%) of the total number of people living with HIV in the world (20.6 million people). In 2018, there were 800,000 new HIV infections, just under half of the global total. In recent years, a number of countries in the region such as Botswana, Kenya, Uganda, Malawi and Rwanda have implemented national campaigns to encourage uptake of HIV testing and counselling (HTC). In 2018, 85% of people living with HIV had knowledge about their status–a significant improvement from 77% in 2015 and higher than the global percentage in 2018 (79%).
Access to HTC has been a major barrier to testing up-take and a number of strategies have been used to address this. Provider-initiated testing remains the region’s main approach, but community-based testing is growing as it has been shown to be effective in reaching large numbers of first-time testers, diagnosing people living with HIV at earlier stages of infection, and linking those who test positive to care. Workplace and door-to-door testing, using rapid diagnostic tests, is also increasing. Though in the era of covid 1, community counseling is also becoming a big challenge, one meter distance is not giving much privacy to clients.
Avert 2020 reported Malawi’s HIV prevalence to be one of the highest in the world, with 9.2% of the adult population (aged 15-49) living with HIV.1 In 2018, an estimated one million Malawians were living with HIV and 13,000 Malawians died from AIDS-related illnesses. The Malawian HIV epidemic plays a critical role in the country’s life expectancy of 61 years for men and 67 for women.
HTC services are provided in two ways: through client-initiated HTC (also known as ‘voluntary counseling and testing’), and providerinitiated HTC. Provider-initiated testing, which is when a health worker offers an HIV test to a patient, occurs in a wide variety of settings, including healthcare facilities, mobile testing units, people’s homes and at national health events. In clinical settings, HIV testing is available in adult and paediatric inpatient wards, nutritional clinics, antenatal care, maternity and postnatal wards, outpatient departments and sexual health clinics.41In comparison, 1.8 million people accessed HTC services in total during 2014.42 This suggests HIV testing services have significantly expanded in recent years.
Most of the counseling were done by Lay workers who have had on job training, some of them they have done 6weeks training where there learn a lot of skills, Information overload is the order of the day. Avert observed that Stigma remains a key barrier to progress, particularly among men who have sex with men and sex workers. There is a need to provide professional counselling to clients/patients, guardians and community to combat stigma. The nature of the mode of spread of the condition is the one that gives stigma.
Despite these successes, treatment adherence levels in Malawi are lower than the rate of 85% recommended by the World Health Organization (WHO). In 2018, 65% of people living with HIV who had begun ART were still on it after 12 months, the lowest rate recorded since 2011.This is potentially due to the rapid expansion of the number of people on treatment. Adherence levels are lower among adolescents than adults. Recent research found that 45% of adolescents living with HIV reported missing ART in the past month. The most commonly reported reason was forgetting (more than 90%), travel from home (14%) and busy doing other things (11%). Alcohol use, violence in the home and low treatment self- efficacy were all associated with worse adherence.
In October 2019, a study was conducted in two privately owned ART facilities in Malawi to find Factors influencing adherence to antiretroviral treatment among adults accessing care from private health facilities in Malawi they found out that the main reason for defaulting from antiretroviral (ARVs) was fear of disclosing an HIV status to avert potential stigma and discrimination [1-5]. In implementing ART clinics due consideration and strategies need to be adopted to ensure that privacy and confidentiality is preserved.
Defaulter rate for Patients on Antiretroviral Treatment (ART) in Ntcheu was pegged at 40 per cent which is threatening in the attainment of 90:90:90 HIV initiatives. ART Coordinator for Ntcheu, Dave Muhasuwa disclosed on Friday, 1st July 2019 at Masimale village in the area of Traditional Authority (TA) Kwataine during a joint review of TB and HIV Global Fund Programme [6-9]. He said over 53, 0000 patients were put on ART treatment only 32,000 were accessing the drugs from various outreach points in the district.
Another study was done at Queen Elizabeth Central Hospital where they were evaluating treatment results of the paying antiretroviral therapy (ART) clinic of, a large public and teaching hospital in Blantyre, Malawi. A total of 422 (59%) of the patients who started ART since 2000 were lost to follow-up. The 176 patients enrolled in the study had good virological and excellent clinical treatment results. (Research gate) one of the reasons for non-adherence of drugs was that many patients were lost to follow up , perception would be probably they were not counselled properly.
ART adherence and tolerability
According Malawi AIDS Response Progress 2015 Report , In July 2013, Malawi’s started transitioning first line ART from stavudine / lamivudine/nevirapine (Regimen 1 A) to tenofovir /lamivudine/ efavirenz (Regimen 5A). By the end of September 2014, 513,600 (99%) of patients were on first line and 5,240 (1%) were on second line regimens; 471 (<1%) were on non-standard regimens. Of the 488, 020 adults on first line ART, 454,763 (93%) were receiving regimen 5A, 26,686 (5%) were on zidovudine /lamivudine/nevirapine (regimen 2A), while 1,925 (<1%) were on regimen 1A (“the old regimen”). Among 25,580 HIVpositive children on paediatric ART formulations, 24,401 (95%) were on zidovudine/lamivudine/nevirapine (regimen 2P) which is the new standard first line for children. The prevalence of side effects in all ART patients stabilized at ~2% which is lower than when the majority of patients were on regimen 1A. Based on pill count and self-reported missed doses, almost 91% of the patients on ART were classified as >95% adherent.
Stigma
The other reason for most of clients defaulting is the issue of stigma Stigmatization can be overt. It can manifest as aversion to interaction, avoidance, social rejection, discounting, discrediting, dehumanization, and depersonalization of others into stereotypic caricatures. Stigma can also be subtle. For example, stigma can arise as non-verbal expressions of discomfort (e.g. a lack of eye contact) that result in tense social interactions between stigmatized and non-stigmatized individuals.
Most of the clients got affected with stigma, at Chiradzulu District hospital. Most of the clients from Blantyre opt to get treatment from a far district than within Blantyre to avoid being stigmatized.
From a social psychological perspective, stigmatization may have a number of functions [10-12]. One is the function of exploitation and domination (keeping people down). People with more power may stigmatize people with less power in order to maintain inequalities between groups. Another function is social norm enforcement (keeping people in). The threat of stigmatization is thought to encourage deviants to conform to in-group norms. A final function is disease avoidance (keeping people away). From an evolutionary perspective, social exclusion of deviants protected against infectious diseases and thus contributed to survival.
Effects of HIV aids stigma
AIDS related stigma refers to prejudice, discounting, discrediting and discrimination directed at people perceived to have AIDS or HIV and at the individuals, groups and communities with which they are associated. It persists despite passage of protective legislation and disclosures by public figures that they have AIDS or are infected with HIV.
The University of Manitoba found out that stigma reduction can be classified into six broad domains. Information based approaches, Skills building interventions, Counseling interventions, Contact with stigmatized groups, Structural interventions, biomedical interventions, these can be due to personal, interpersonal, organizational, community, government and structural levels. The literature suggests that approaches combining multiple strategies have the promise for stigma reduction. A large body of research suggests that HIV/AIDS related stigma is associated with poor physical & mental health outcomes negatively affects work and family life and a barrier. Influencing individual’s decision to be tested for HIV .Impacts access to health services negatively affects adherence to treatment. The following questions were addressed .What are effective strategies to reduce stigma related to living with HIV/AIDS.
Discrimination
Given the degree of discrimination and prejudice experienced by people living with HIV/AIDS, social stigma often functions as a barrier to disclosure of one’s HIV status. Crocker, 2011 offered two interesting motivational factors in relation to disclosing one’s HIV status: ego system and ecosystem. Ego system is made up of self-serving benefits, which boosts one’s image.
In constructing desired self-images, people present themselves in a certain way to get other people to see them as having particular qualities, so they can obtain resources such as relationship partners, jobs or admissions to college. The ecosystem goals focus on supporting others by avoiding being selfish, self-centered and harmful to others.
The fear of rejection leads people to conceal a status if they have ego system goals, but not if they have ecosystem goals. When people have ego system goals, they tend to enhance self-images and obtain desired social outcomes such as acceptance.
Consequently, when stigmatized people expect rejection if they reveal their stigma, they attempt to conceal it from others. Ecosystem goals for disclosing stigmatized identities include consideration of the needs and well-being of others, in addition to the self. Instead of focusing on protecting the self, ecosystem goals focus on supporting others. People with ego system motivations might be willing to risk disapproval for the sake of creating authentic relationships with supporting others.
Mostly the gendered effect and how HIV status intersects with the power imbalance at the root of sexual assault. The tension between the need for women to protect both their medical information and their sexual integrity puts them in an awkward situation. They are discriminated in their own homes, and have fear of the husband which affects adherences to drugs.
Chiradzulu had registered 2317 patients commenced ART in 2001, By the year 2004, 230 patients had died,169 were lost to follow up and 99 had side effects, according to medicines frontiers report . The question would be if antiretroviral clinics in Malawi offer professional counselling to people living with HIV and AIDS? We answer the question by determining whether there is a relationship between default rate and professional counselling for Queen Elizabeth central Hospital and Chiradzulu District Hospital.
One out of every twenty HIV positive Malawi adults is now on ART. Two hundred seventy five thousand deaths have been averted and 1.4 million life-years have been gained, primarily among young adults in their peak productive life period. Default rate of anteretroviral is increasing affecting the mentioned statistics making clients susceptible to opportunistic infections instead of having a benefit of prolonging life they lessen the life expectancy. Most of the counsellors who are assisting clients on ARVS did not go for counseling course or had done short courses of counseling in which they learn a lot of material within a short time leading to information overload and difficult to absorb it and after the course nobody follows them ,they work without supervision . Clients are not getting enough knowledge as there is incompetence of providers on counseling issues. Patient goes with no knowledge on the benefits of ARVS hence no information on the importance of adhering to the Antiretroviral drugs, leading to increase in default rate as clients develop negative perception of ARVs due to unknown causes. It is against this background that the author is intending to find out if there is any correlation between professional counselling and default rate of Antiretroviral drugs.
The main objective was to find out if there was any correlation between Anteretroviral treatment default rate with professional counselling ,further they were other specific objectives as follows (1) to find out the default rate of Chiradzulu District Hospital and Queen Elizabeth central Hospital, (2) To find out whether clients had undergone professional counselling, (3) analysing the counselling qualification s of the counsellors.
Key points
Stigma: Can be described as a dynamic process of devaluation that significantly discredits an individual in the eyes of others. ‘Stigma’ is derived from the Greek meaning a mark or a stain.
Discrimination: Discrimination refers to any form of arbitrary distinction, exclusion, or restriction affecting a person
Immunity: Refer to the body's specific protective response to an invading foreign agent or organism
Professional counselling: Professional counseling is the process whereby specially trained individuals work with others individually ,in families and /or in groups to address and work to resolve personal and interpersonal issues by using active listening, goal setting and behaviour change and by teaching new skills and problem solving.
Methods
Data
Primary data was collected from clients at both centres and medical personnel’s ,further counsellors were interviewed , data was also collected lost to follow up clients were also interviewed. A case study design was used of queen Elizabeth Central Hospital and Chiradzulu District Hospital of different health services of essential health services, tertially and secondary level ,counselling process how clinics are conducted was a guiding tool in the use of Naturalistic observation .Regarding the limited time needed to accomplish the study cross sectional study was used the only solution for the exposure and the outcome to be assessed at the same time and relatively easy and helpful in assessing health needs. Point prevalence of default rate in relation to professional counseling was assessed at the same time because it was a non-probability random sampling. Only those patients on antiretroviral drugs were eligible to participate. The outcome of the result was determined with client satisfaction attained and the dependent variable of professional counseling proved default rate. deductive approach was adopted where the existing theories were tested ,social networking theory and social cognitive theories. A correlation research, which shall use the relationship of default rate and professional counselling, a questionnaire, observation charts, registers were some of the research tools that were used. Secondary data which was taken from journals, other empirical evidences were compared with the results. The researcher opted to use a multistrategy approach as employed by layder 1963 and Bryman referring to research that will combine quantitative and qualitative research. The researcher interviewed eight lost to follow up clients four from both centres to find out why they defaulted and how they were managed.
Analysis
The study has to find the relationship between default rate and professional counselling. The data was captured on the clients who had defaulted. Out of 24 clients of Chiradzulu District Hospital 18 clients were counselled once or twice with the follow up of the past three years they have been in care , while 6 weren’t,four were lost to follow up, out of the four only two came back to care through the mother to other care project, the other two wouldn’t be traced. Below is the table while 11clients defaulted treatment Table 1.
| Period counselled | No of respondents | Defaulted (X) | Counselled (Y) | XY | X2 | Y2 |
|---|---|---|---|---|---|---|
| Once | 6 | 2 | 5 | 10 | 4 | 25 |
| Twice | 9 | 3 | 9 | 33 | 9 | 81 |
| Three | 4 | 4 | 2 | 8 | 16 | 4 |
| Not counselled | 6 | 2 | 2 | 4 | 4 | 4 |
| Totals | 24 | 11 | 18 | 55 | 33 | 112 |
Table 1: Data from Chiradzulu Respondents.
While at Queen Elizabeth Central Hospital out of 34 clients 22 were counselled and adhered to treatment while 12clients defaulted treatment ,four lost to follow up clients were contacted whom after counselling they came back to care with the help of light house organization Table 2.
| Period counselled | No of respondents | Defaulted (X) | Counselled (Y) | XY | X2 | Y2 |
|---|---|---|---|---|---|---|
| Once | 16 | 5 | 11 | 55 | 25 | 121 |
| Twice | 6 | 2 | 4 | 8 | 4 | 16 |
| Three | 2 | 1 | 2 | 2 | 1 | 4 |
| Not counselled | 10 | 4 | 5 | 20 | 16 | 25 |
| Totals | 34 | 12 | 22 | 85 | 46 | 166 |
Table 2: Data from Queen Elizabeth Central Hospital.
Correlation analysis for chiradzulu using correlation regression formula

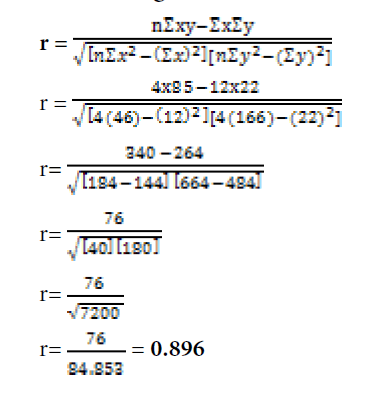
Correlation analysis for queen elizabeth central using correlation regression formula
Cohort comparison analysis of two different facilities (Chiladzulu and Queen Elizabeth Central Hospital)
Correlation Coefficient for Chiradzulu District Hospital is 0.6 and for Queen Elizabeth Central Hospital is 0.8. Both results have a strong positive correlation between default rate and professional counseling.
Results
The results showed that there is strong positive correlation between default rate and professional counselling.
Out of 24 respondent of Chiradzulu District Hospital 11 defaulted treatment representing 45% default rate. Four were lost to follow up out of the four returned to care. Out of 34 respondents from Queen Elizabeth Central Hospital 12 defaulted representing 35% of default rate.
Counsellors were unable to conduct the proper counselling process due to the infrastructure ,no special rooms for counselling ,some rooms would handle two to three counsellors at a time ,privacy was not being observed, some of the steps were missed due to a lot of clients on clinic days ,Some steps were missed unaware due to Knowledge gap.
All counsellors did not go for a formal course of counselling, almost all the counsellors has had on job training .Out of 30 medical personnel’s who were interviewed from Chiradzulu only two people had counselling expertise representing 6% They went for six weeks training, the rest had on job training. While at Queen Elizabeth Central Hospital out of 30 people 4 were trained counsellors, they were also using the Medical assistant and the nurse to assist with counseling which is representing 20%.The other observation was that there had no specific rooms favorable for individual counselling especially at Queen Elizabeth Central hospital
Discussion
Despite a lot of success stories of Malawi HIV and AIDS still faces the problems of clients defaulting Malawi still faces challenges of Anteretroviral treatment adherence ,which will delay the HIV 90 -90-90 strategic plan , The Vision of the NSP is to have a healthy and prosperous nation free from HIV and AIDS. The Mission of this NSP is to provide high-quality HIV prevention, treatment and care services for all Malawians. This 5 year strategic plan aims to meet the Ambitious 90-90-90 Treatment Targets released by UNAIDS in 2014 will result in 760,000 (73%) of the projected 1,042,000 PLHIV being virally suppressed, leading to a dramatic reduction in sexual and vertical transmission at the population level. If we have an increased default rate, it shall affect the planned outcome.
Definitely something has to be done on the strong positive correlation of the default rate and professional counselling, a lot is desired to be done on professional counselling.
Counselling is a principled relationship characterized by the application of one or more psychological theories and a recognized set of communication skills, modified by experience, intuition and other interpersonal factors, to clients’ intimate concerns, problems or aspirations [13-17]. Its predominant ethos is one of facilitation rather advice-giving or coercion. It may be of very brief or long duration, take place in an organizational or private practice setting and may or may not overlap with practical, medical and other matters of personal welfare.
According to the qualifications of the counsellors, it is so difficult to expect professional counselling from them ,this might be a reflection of most of the reasons for default rate as presented by UNAIDS, Queen Elizabeth study and Ntcheu study, most of the these studies believed default rate had increased due to stock outs of drugs, the researcher believes there are line of drugs according to the Malawi HIV /AIDS guidelines .Therefore clients would be switched to the drugs that are always in stock .
The perception is that those who have been taking drugs have also been influenced by the Social cognitive theory than counselling, clients have been counselled once, twice of three times during a period of three years of taking drugs ,the setup of the clinics would also affect what is expected to be done in counselling,
Social cognitive theory evolved from social learning theory, which was created by Albert Bandura in the early 1960s. In 1986, Bandura officially launched social cognitive theory with his book Social Foundations of Thought and Action: Social cognitive theory defines human behavior as an interaction of personal factors, behavior, and the environment. Social cognitive theory is the most frequently used paradigm in health promotion.
Bandura has identified several important constructs of social cognitive theory, including the environment, situations, behavioural capacity, outcome expectations, outcome expectancies, self-control, observational learning, self-efficacy, and emotional coping.This theory is based on the reciprocal determinism between behavior, environment, and person; their constant interactions constitute the basis for human action.
The researcher argues that the construct of the theory assisted clients to learn from fellow clients who were taking drugs and through the information they were hearing from media assisted them to adopt the behavior of adhering to drugs. On personal perspective, a person’s expectations, beliefs, self-perceptions, goals, and intentions shape and direct behavior this would come as a client is managing individual health, other clients would simply default they feel healed or they are having side effects of the drug of the drug and choose just to stop taking the drugs with no replacement or advice from the medical personnel’s.
On Environmental factors: Some clients were affected by the constructs of social influence either positive and negative way, others benefited by understanding the benefits of adhering to the anteretroviral drugs, Human expectations, beliefs, and cognitive competencies are developed and modified by social influences and physical structures within the environment. Other clients defaulted because of environmental factors like prayer stigma and family no family support.
As for the Behavioural factors: other clients had defaulted because they were newly married and ashamed to inform the partner and choosing to use herbals. A person’s behaviour will determine the aspects of the person ’ s environment to which the person is exposed, and behaviour is, in turn, modified by that environment. Therefore if people in the society are using herbal they influence peers to take them.
The other biggest challenge has been follow up of lost to follow up clients,at least further Individual counselling on follow up would bring clients back to care .According to the outcome of the interview with the providers of mother to mother care at Chiradzulu District Hospital ,who go for home visits there biggest challenge were resources, they usually go on foot ,they choose to go to nearby villages which affect those from long distances.
Joffe’s theory
Joffe had defined stigma as a social process, drawing on existing forms of social representation that are rooted in social power relations, emerging from an individual psychological blaming and othering response, a cognitive justification for an emotional reaction of fear. Stigmatizing discourse allows people to distance themselves and their self-defined in-groups from the risk of infection by blaming contraction of the illness on characteristics normally associated without groups, who are classified as deviant and ‘others’. The same way they distant themselves with the ARV drugs. I argue that in understanding default rate of ARVS due to no professional counseling can lead to stigma which come as a social process we do not need to define it in terms of discrimination to appreciate the importa4.nce of social power relations as it appears in the Social network theory. We can define stigma as a social process in which: Illness is constructed as preventable or controllable; Non adherence to treatment can be preventable by giving enough information to the client which will be controlling from stopping treatment and can be controlled with good counseling follow ups.
Certain people are thus blamed for their own infection; Self-blame may come to the patient if the patient has not yet reached acceptance of the condition and feels better to die or feels others are blaming him/her being the cause of the disease, if this is not managed well may push the patient to stop treatment.
Status loss is projected onto the ‘other’, which may (or may not) result in disadvantage to them; Others feel having the lifelong treatment makes them lose their status, they would prefer hiding them taking drugs when they see they have improved they forget that this is a lifelong treatment, stopping adhering to the drug leads to the deterioration of the condition as the virus starts replicating again.
Building on Joffe’s theory HIV /AIDS carries a lot of stigma despite position in society mostly as per researchers observation cultural believes, gender and disease process carries a lot of stigma. Mostly on those who are on Antiretroviral therapy, people define them with different names. Mostly they are being teased as taking daily units, Marking them as outcasts ‘those with HIV/AIDS’. For these reason patients, clients would choose to stop ARV’s.
Issues of psychological blaming, shame and fear comes in, this stigma leads to withdrawal and in trying to hide out the patients resolves of stopping taking drugs. Manifestation of depression, social withdrawal, school dropouts comes in. But still in other ways the stigma cannot be run away because of the nature of acquiring the disease, the author feels the only solution can be the use of professional counseling, as it will empower the client, patient to have more information on the disease process and would not be shaken with the perceptions out there to the extent of stopping the drugs. From my theories my conceptual framework will base on combating default rate with the use professional counseling, if it’s either because of not being supported through the social network theory, attitude or being stigmatized from Joffes theory.
Best practices should be put in place ,cadres of counsellors is missing in the healthy systems management structures, it has not to be undermined ,we find more non adherences, which further lead to defaulting, this makes the half-life of the anteretroviral drugs to be affected, it later makes the patient to be susceptible to opportunistic infections. The imunity decreases due to the replication of Human Immunovirus Syndrome, Adherence of the anteretroviral assists in achieving viral suppression.
Conclusion
The study aimed at finding out if there is any correlation between Anteretroviral treatment default rate with professional counselling. Upon the findings it was determined that counselling has influence on clients to adhere to anteretroviral, Peers has influence on encouraging others to adhere or not to adhere to anteretroviral. Professional counselling assist clients holistically not only promoting benefits of the drugs and managing other confounders as well which may cause clients not to adhere to drugs. In determining default rate in patients who did not have professional counseling they study concluded to have a strong positive relationship from centres.
Knowledge gap contributed to defaulting, lack of information which would have been obtained from counselling on the effects of defaulting drug on the same pressure of work affects the people care. It was also discovered that the challenges are available in both centres both had positive correlation, 35 and 45%. Register for counselled clients would have assisted to provide best care.
Finally other confounders like an issue of side effects of drugs apart from counselling contributed to the reasons of defaulting drugs. Further follow up counselling of lost to follow up clients proved effective.
References
- Aidi M (2009) Patient Retention in Treatment–Contributing Factors and Challenges in Tanzanian Patients on Antiretroviral Therapy.2009 HIV Implementers Meeting, Windhoek, Namibia.
- Billy A (2007) What does “lost to follow-up†mean for patients enrolled in a highly active antiretroviral treatment (HAART) programme in Africa? 4th IAS Conference on HIV Pathogenesis, Treatment and Prevention Abstract CDB514.
- Dahab M, Charalambous S, Hamilton R (2008) “That is why I stopped the ARTâ€: patients' and provider' perspectives on barriers to and enablers of HIV treatment adherence in a South African workplace program. BMC Public Health 18:63.
- Elias S (2018) Malawi, World Health Report, Malaria Indicator Survey 2017, National Malaria Control Programme (NMCP).
- Fetham C, Dryden W (1993) Dictionary of counselling, London: WhurrGlenn Sheppard, Ed.D.CCC, and Notebook on Ethics, Legal Issues, and standards for Counsellors.
- Kurzban R, Leary MMR (2013) Stigma, Discrimination, and Living with HIV/AIDS: A Cross-Cultural Perspective. Front Public Healh 3:242.
- McNairy ML (2013) Retention of HIV-infected children on antiretroviral treatment in HIV care and treatment programs Kenya, Mozambique, Rwanda and Tanzania. J Acquir Immune Defic Syndr 62:e70–e81.
- Feltham C, Dryden W (1993) Dictionary of counselling, 2nd edition Wiley published,
- Frost J (2019) Introduction to statistics,an intuitive Guide for Analysing Data and unlocking discoveries.
- Loubiere S (2009) HIV disclosure and unsafe sex among HIV-positive women in Cameroon. Social Science Medicine 69:885-891.
- Malamba SS (2005) Couples at risk: HIV-1 concordance and discordance among sexual partners receiving voluntary counseling and testing in Uganda. J Acquir Immune Defic Syndr 39:576-580.
- https://www.ilo.org/wcmsp5/groups/public/---ed_protect/---protrav/---ilo_aids/documents/legaldocument/wcms_250398.pdf
- Razieh TN (2012) Theories of Developmental Psychology Bandura’s Social Learning Theory & Social Cognitive Learning Theory. Theory Dev Psychol 2012:1-24.
- Tweya H (2009) Early active follow-up of art-patients who are overdue for their appointment: the ‘Back-To-Care’ project at the Lighthouse Clinic, Malawi, South Africa.
- Unge C, Södergård B, Marrone G (2010) Long-term adherence to antiretroviral treatment and program drop-out in a high-risk urban setting in sub-Saharan Africa: a prospective cohort study. PLoS One 5:e13613.
- Yu JKL, Chen SCC, Wang KY (2007) True outcomes for patients on antiretroviral therapy who are “lost to follow-up†in Malawi. Bulletin o World Health Org 85:550-554.
Citation: Singini P (2020) Correlation Research on Professional Counselling and Hiv/Aids Treatment Default at Chiradzulu and Queen Elizabeth Hospital-a Cohort Study. J Comm Pub Health Nursing 6: 244 DOI: 10.4172/2471-9846.1000244
Copyright: © 2020 Singini P, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 1886
- [From(publication date): 0-2020 - Feb 22, 2025]
- Breakdown by view type
- HTML page views: 1278
- PDF downloads: 608
