Research Article Open Access
Correlates of Psychosocial Health-related Quality of Life Measures for Normal Weight and Obese Children Participating in an Active Play Program
Angelo Belcastro*, Donna Mohseni Mofidi, Yasamin Ahmadi and Asal MoghaddaszadehDepartment of Health Science, Pediatric Exercise Science Laboratory, School of Kinesiology and Health Science, York University, Toronto Ontario, Canada
- *Corresponding Author:
- Angelo Belcastro
Department of Health Science
School of Kinesiology and Health Sciences, Faculty of Health
York University, 4700 Keele Street, Toronto
ON, M3J 1P3, Canada
Tel: (416) 736 5403
E-mail: anbelcas@yorku.ca
Received Date: August 12, 2015 Accepted Date: August 31, 2015 Published Date: September 04, 2015
Citation: Belcastro A, Mofidi DM, Ahmadi Y, Moghaddaszadeh A (2015) Correlates of Psychosocial Health-related Quality of Life Measures for Normal Weight and Obese Children Participating in an Active Play Program. J Child Adolesc Behav 3:242. doi:10.4172/2375-4494.1000242
Copyright: © 2015 Belcastro A et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Child and Adolescent Behavior
Abstract
Objective: The purpose of this investigation was to examine changes in quality of life indicators from normal weight (NW) and overweight (OW) children to a play-based fun physical activity (PA) intervention. Methods: Children (n=33) were assessed prior to and following an eight-week (4 d/wk; 55 min/d) active play program. Children were assessed by the PedsQL survey for psychosocial function and perception of physical function, PA enjoyment and PA participation. Results: These were related to changes in body composition, cardiovascular measures and physical activity participation. OW children showed a reduction in waist circumference (1 mm) and sum of skinfold (12 mm) (p<0.05), in contrast to NW group (p>0.05). NW and OW groups experienced similar reductions in blood pressure (p<0.05). The changes in body composition (body mass waist circumference and sum of skinfolds) were related (r from -0.36 to -0.51) with psychosocial function for NW and OW children (p<0.05). In contrast the cardiovascular measures were related to changes in the OW group for blood pressures and heart rate. Conclusions: In summary NW children had a less pronounced response for cardiovascular measures to playbased PA when compared to the OW group. Nonetheless both groups benefitted in terms of improvements in body fat (waist circumference; sum of Skinfolds). Therefore active play PA programs, in contrast to training programs, are effective in mediating obesity and beneficial to physical health regardless of a child’s weight or risk status
Keywords
Children’s quality of life; Weight status; Physical activity; Active play
Introduction
Higher levels of perceived health-related quality of life (HRQL) profiles and improved cardiovascular health/fitness [1] have been associated with greater physical activity (PA) participation among children and adolescents [2]. The relationships between PA and both health and psychological well-being have been reported to yield positive benefits for children and adolescents [3]. One correlate of children’s PA is weight status, compared to normal weight, children adolescents show less PA participation and manifest a lower healthrelated quality of life, thereby increasing their risk for developing chronic disease [1]. Indeed, this is a positive correlation between excess weight in childhood and growing challenges with physical and emotional health [1,4]. Studies indicate that incorporating aerobicexercise as a means of treatment for individuals diagnosed with depression results in improvement in depression and decreases relapse rates than individuals only on medication [5]. What is unclear is the extent to which short-term, PA intervention programs promote positive benefits for cardiovascular health, self-esteem and depressive symptoms in obese children [1,4,6]. Also unknown is the effectiveness of a PA intervention program to improve emotional and psychosocial factors related to quality-of-life variables in relation to changes in health variables.
This is not a trivial matter since only a small percentage of children meet recommended PA guidelines. The 2009 to 2011 Canadian Health Measures Survey indicates for children between the ages of 5 and 17 that 31.5% are classified as either overweight or obese [7]. To overcome such a large deficit in children’s PA participation, it has been suggested that active play [8,9] may be an appropriate format to improve PA participation and also promote positive benefits for health and psychological wellbeing of children and adolescents. Minimal literature exists as to the impact of quantified play-based PA participation and health and psychological outcomes in children and adolescents. However, Canadian PA guidelines promote children and youth (ages 5 to 17 yrs) to participate in 60 min/day of vigorous physical [10]. A study using sixty overweight and obese children and adolescents were randomly assigned them to either an intervention group or a control group. The intervention group was required to do 60 min of guided PA twice a week for five months. While this extent of PA does not meet Canadian PA guidelines, the study can be used as a less extensive representation of the ideal. As expected, the overweight and obese individuals reduced in overall percentage body fat by 1.8%, while the control group decreased by 0.9%. As indicated the children who participated in two days of 60 min PA reduced their percentage body fat on average by 2.0% [11]. This suggests that PA is effective in lowering or reversing obesity in children [3,6]. The purpose of this investigation was to examine changes in various health variables and psychological well-being indicators of children who participated in an eight-week guided active play program. The specific questions addressed were to: 1) assess whether normal and overweight children respond differently to a PA play-based intervention program and 2) correlate health-related quality of life measures with changes in health/ fitness variables in children with different weight profiles. It is hypothesised that the outcomes will be the same for both obese and normal weight children.
Methods
Participants
Prior to data collection, the Human Participant Research Ethics Committee at York University granted approval. This study was conducted in accordance with Canada’s Tri-Council Policy for the Ethical Conduct of Research Involving Humans. Written consent was obtained from parents/guardians of the children involved with this study. Children also provided their own verbal assent to participate. Children (n=33) included males and females (55% and 45% respectively), with ages ranging from 7 to 12 years. These children were recruited to participate in this study from a local community centre children’s PA. The 33 participants that took part in the program Children (and their parents/guardians) wishing to participate in the study were given an information and orientation session prior to the commencing sessions.
Study design
Children (n=33) participated in an eight-week PA program (4 d/wk; 55 ± 3 min/d), which consisting of five or six randomly assigned, selfpaced (unregulated), age appropriate games from a directory [8]. In addition to the 55 minutes of activity, a warm-up period and a water break (half way through the session) were included. The opportunity for children’s self-paced activity was delivered in a guided/facilitated active play program, which involves experienced Kinesiology Undergraduate majors serving as positive role models and encouraging children to participate in a ratio of five-children for oneundergraduate student. At no time are the children forced and/or ridiculed for not participating; their engagement in the games is completely under their control. This is an attempt to provide the opportunity to cooperate and socialize with peers while having fun and being active. All activity sessions were conducted in a temperature controlled 20 ± 1°C gymnasium.
Measurement of physical activity
PA was quantified by accelerometry (Actigraph GT3X+) during the hour long active play program and expressed as vector for ten-second epochs [12]. The ACC data were transformed using a linear regression equation (y=0.0045x+0.9912) (R2=0.99) to predict metabolic equivalents, which was generated on from all participants. Briefly the ACC calibration was accomplished with a treadmill protocol of rest, 4, 6 and 8 km/h (0% grade) treadmill activity (8) using a CosMed2 oxygen collection system for VO2 determination. Cutoffs for activity levels were; 0 – 2 METs classified as sedentary, 3 – 3.9 METs classified as light activity, 4-5.9 METs classified as moderate and <6 METs classified as vigorous.
Measurements of psychosocial well-being and attractiveness to physical activity
The Pediatric Quality of Life Inventory (Peds-QL) was used to assess psychological well-being or health-related quality of life prior to and after completing the intervention. Scores for psychosocial functioning and perceived physical functioning were used as described by Varni et al. [13], with moderate to very good Pearson’s correlation and intra-class correlation coefficients for children between the ages 4-12 years. The questions were read to the child, who were then asked to circle whichever answer felt the most appropriate regardless of child’s age and level of comfort in reading. The Children’s Attraction of Physical Activity (CAPA) was administered to the children [14]. The CAPA scale is built upon psychological characteristics found to influence children’s attraction to physical activity. It consists of five factors; liking and feelings toward vigorous exercise, liking of games/ sports, importance of exercise related to health, peer acceptance in games/sports, and fun of physical exertion. There are four items for the first four factors listed and five items to determine feelings toward physical exertion. The CAPA instrument was developed based upon findings in focus groups comprising of children in grade 3–4; the survey has be found to produce reliable and valid results for children ages 8–10 with an alpha value >0.60 on all five sub-groups [14].
Procedures
Standing height was measured using a standiometer. Without shoes, children were asked to stand erect with feet together ensuring their heels, buttocks, back and head were in contact with the standiometer. Height was recorded to the nearest 0.5 cm. Wearing light clothing and standing in sock feet, weight was measured using an electronic scale to the nearest 0.1 kg. Body mass index (BMI) was calculated as weight divided by height (BMI = kg/m2). Waist circumference measurements were taken to the nearest 0.1 cm. Children were identified as high risk for pediatric obesity and cardiovascular disease when their waist circumference measurements fell at a value greater than the 75th percentile for their age and sex, based on the rationale that waist circumference is a direct indicator of visceral adiposity and related risk of weight-related co-morbidities. Recent waist circumference measurements of representative samples of North American children were used as references [15,16]. Upon arrival and after resting for a minimum of five minutes, heart rate was measured while the child sat in a chair with their right arm resting on a table. Manual palpation of the right carotid or radial artery occurred for 15 seconds. Blood pressure was measured on the child’s right arm using a manual sphygmomanometer and an appropriately sized cuff. Systolic blood pressure was recorded as the first audible Korotkoff sound and diastolic blood pressure was determined by the fifth Korotkoff sound.
Data analyses
Descriptive statistics were calculated for all measures and are expressed in means and standard deviations (mean ± s). All statistical analyses were conducted using the Statistical Package for Social Science (SPSS) software (v22). Statistical significance was accepted as (p ≤ 0.05) and two-tailed tests were used. Levene’s test was used to determine the homogeneity of variance and independent t-tests were conducted to compare differences between groups. When groups had unequal variances Mann-Whitney U tests pre and post scores were used to determine significance levels. Correlations (Pearson r) between body composition and cardiovascular measures and HRQL’s perception of physical function, psychosocial function and physical activity (PA) enjoyment or attractiveness parameters were performed (SSPS v22).
Results
The 33 participants that took part in the program included males and females (55% and 45% respectively). The mean age was 10±0.3 years. Eleven or 33% of the children were identified as overweight (OW) or at increased risk for obesity and cardio-metabolic issues based on their waist circumference measurements. The mean age was similar for both the overweight and normal groups (p>0.05). The baseline comparison of overweight and normal groups is summarized in Table 1. The overweight groups weighed on average 21 kg (± 0.3) more than the normal group, had a waist circumference 19 cm (± 0.1) greater and had an average sum of skin folds 86mm greater than the normal groups. The average diastolic and systolic blood pressure and resting heart rate was comparatively higher in the overweight group by 7 mmHg, 5 mmHg and 5 bpm (± 0.5) respectively. A statistically significant difference was not seen in quality of life scores between the two groups, except that the overweight children scored an average of 9% higher on their perception of physical functioning than normal weight children. They also rated themselves slightly higher (3%) on emotional functioning and lower on psychosocial functioning (6%) and physical activity enjoyment/attractiveness (6%).
| Parameter | Normal Weight | Overweight | Total |
|---|---|---|---|
| Children (n) | 22 | 11 | 33 |
| Age, years (sd) | 10.2(±0.3) | 10.3(± 0.4) | 10.3(±0.2) |
| Body Composition and Cardiovascular Parameters | |||
| Body Mass, kg (sd) | 36 (±2) | 57 (±3)* | 43 (± 2) |
| Waist Circumference, cm (sd) | 61 (± 1) | 80 (±2)* | 67 (±2) |
| Sum of Skinfolds, mm (sd) | 61 (±6) | 147 (± 12)* | 90 (±9) |
| Resting BP Systolic, mmHg (sd) | 99 (±3) | 106 (±3)* | 101 (±2) |
| Resting BP Diastolic, mmHg (sd) | 65 (±2) | 70 (±4)* | 67 (±2) |
| Resting Heart Rate, bpm (sd) | 77 (±2) | 82 (±4) | 79 (±3) |
| Quality of Life Parameters - expressed as percent (sd) | |||
| Perception of Physical Function | 76 (±3) | 85 (±4)* | 79 (±3) |
| Psychosocial Function | 74 (±3) | 66 (±6)* | 71 (±3) |
| Physical Activity Attractiveness | 73 (±3) | 67 (±4)* | 71 (±3) |
Table 1: Characteristics of children participating in an eight-week guided active play summer program. Body composition, cardiovascular and Health-Related Quality of Life measures are reported prior to program. Data are expressed as means ± sd and the level of statistical significance (p<0.05) reported with an asterisk (*) for Normal Weight versus Overweight Groups.
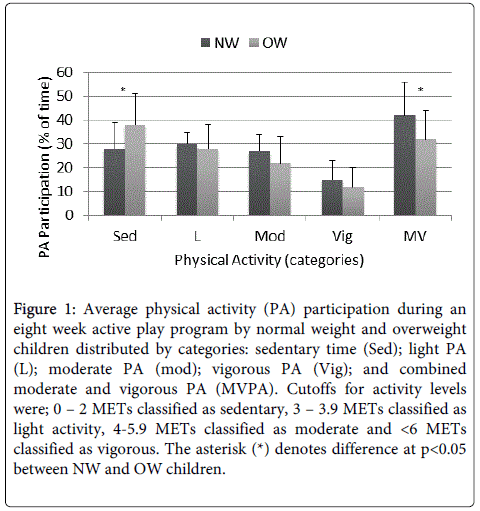
Normal weight children participating in the eight-week PA program completed on average 3456 ± 209 counts/min (vector magnitude), which was greater than the PA participation noted for obese children attending the program (2733 ± 467 counts/min) (p<0.05). Overall the average percentage of time spent in sedentary (S), light (L), moderate (M), vigorous (V) and M-V intensities were 28% ± 11%, 30% ± 5%, 27% ± 7%, 15% ± 8%, 42% ± 14%; 38% ± 13%, 28% ± 10%, 22% ± 11%, 12% ± 8%, and 32% ± 12%; for the NW versus OW groups, respectively. The average %MVPA elicited throughout the eight-week program is in Figure 1.
Figure 1: Average physical activity (PA) participation during an eight week active play program by normal weight and overweight children distributed by categories: sedentary time (Sed); light PA (L); moderate PA (mod); vigorous PA (Vig); and combined moderate and vigorous PA (MVPA). Cutoffs for activity levels were; 0 âÂ?Â? 2 METs classified as sedentary, 3 âÂ?Â? 3.9 METs classified as light activity, 4-5.9 METs classified as moderate and <6 METs classified as vigorous. The asterisk (*) denotes difference at p<0.05 between NW and OW children.
Overall, children had slight decreases in waist circumference and blood pressure, and a minor increase in resting heart rate post intervention (Table 2) (p>0.05). The overweight group gained an average body mass of 1 ± 0.4 kg, 1 ± 0.9 cm in waist circumference and lost on average 12 ± 7 mm for the sum of skinfold measurements (Table 2) (p>0,05). The normal weight group did not significantly change in any health/fitness parameter (Table 2). Both groups had lower systolic blood pressure after the intervention compared to baseline.
| Parameter | Post-Pre Intervention Mean Difference (±SD) | ||
|---|---|---|---|
| Normal Weight (n=22) | Overweight (n=11) |
Total (n=33) |
|
| Weight (kg) | -1 (±0.8) | 1 (±0.4) | 0 (±1) |
| Waist Circumference (cm) | -1 (±2) | 1 (±0.9) | -1 (±2) |
| Sum of Skinfolds (mm) | 6 (±2) | -12 (±7) | 0 (± 3) |
| Resting BP Systolic (mmHg) | -4 (±4) | -7 (±3) | -5 ± (3) |
| Resting BP Diastolic (mmHg) | -2 (±4) | -6 (±4) | -3 (±3) |
| Resting Heart Rate (bpm) | 1 (±2) | 1 (±3) | 1 (±3) |
Table 2: Impact of an active play childrenâÂ?Â?s program (i.e. the difference between post and pre-intervention) for body composition,cardiovascular and Health-Related Quality of Life measures by normal weight and overweight children.
The relationships between changes in health/fitness variables and health-related quality of life parameters seen after the guided active play program are depicted in Tables 3 and 4. The perception of physical functioning for normal weight children was not related to 5 out of the 6 fitness variables measured; body mass showed a modest but significant impact on the pre-post differences (r=-0.32) (p<0.05). Psychosocial functioning was related to body mass changes and waist circumference (Table 3) (p<0.05). None of the pre vs post difference scores for cardiovascular variables were related to either physical or psychosocial function in normal weight children (Table 4) (p>0.05). The perception of physical functioning for obese children was not related to 5 out of the 6 variables measured; only body mass showed a modest but significant impact on the pre-post differences (r=.28) (p<0.05). Psychosocial functioning was also significantly related to pre-post difference scores for all variables except heart rate (Tables 3 and 4) (p<0.05).
| Correlation Coefficients (r value) | ||||||
|---|---|---|---|---|---|---|
| Quality of Life Parameter | Weight (kg) |
Waist circumference (cm) | Sum of Skinfolds (mm) |
|||
| NW n=22 | OW n=11 |
NW n=22 | OW n=11 |
NW n=22 | OW n=11 |
|
| Physical Functioning (%) | -0.32* | 0.28* | -0.12 | 0.14 | 0.04 | -0.16 |
| Psychosocial Functioning (%) | 0.40* | 0.36* | 0.22* | 0.40* | 0.04 | -0.51* |
| PA Enjoyment Attractivenss (%) | -0.34* | -0.30* | -0.06 | -0.29* | 0.15 | 0.28* |
Table 3: Relationships (Peasron r) between baseline HRQL measures and difference in body composition measures for normal weight (NW) and overweight (OW) children. Statistical comparisons were at an alpha level of 0.05 and significant differences represented as an asterisk (*) for NW vs. OW groups.
| Correlation Coefficients (r value) | ||||||
|---|---|---|---|---|---|---|
| Quality of Life Parameter | Systolic BP (mmHg) |
Diastolic BP (mmHg) |
Heart Rate (bpm) |
|||
| NW n=22 | OW n=11 | NW n=22 | OW n=11 | NW n=22 |
OW n=11 |
|
| Physical Functioning (%) | -0.18 | 0.03 | -0.05 | -0.40* | 0.13 | 0.44* |
| Psychosocial Functioning (%) | 0.01 | 0.36* | 0.11 | 0.32* | -0.15 | 0.19 |
| PA Enjoyment Attractiveness (%) | -0.03 | 0.03 | -0.01 | 0.26* | 0.19 | 0.41* |
Table 4: Relationships (Pearson r) between baseline HRQL measures and difference in cardiovascular measures for normal weight (NW) and overweight (OW) children. Statistical comparisons were at an alpha level of 0.05 and significant differences represented as an asterisk
(*) for NW vs. OW groups.
Interestingly, the attractiveness to PA assessment for obese children showed significant relationships to the pre-post difference scores for body mass, waist circumference, sum of skinfolds, diastolic blood pressure and heart rate (Tables 3 and 4) (p<0.05). In contrast for the normal weight children were only the body mass differences were different (p<0.05).
Discussion
The first question addressed in this investigation was whether normal and overweight children respond differently to a play-based, fun PA intervention program in regard to physical and psychosocial characteristics. Overweight children responded very strongly to the PA intervention and thus it was considered effective in improving their health status, particularly in reducing waist circumference and skinfold measurement (by 12 mm on average). These changes may reduce the risk for obesity and chronic disease. Since waist circumference is an established indicator of central obesity and is positivity correlated with cardiovascular disease, type 2 diabetes mellitus and premature death [17]. The normal weight group maintained their existing health status except for an increase in skinfold measurement (6mm average). These results indicate that moderate intensity intervention programs decrease total body and visceral body fat in overweight but not normal weight children. It has been noted that 30 to 60 min of moderate activity, 3 to 7 days per week results in a reduction of total body and visceral adiposity in overweight children while not influencing percentage body fat in normal children [18]. The latter may be more active in general and require more vigorous amounts of PA to see beneficial effects on adiposity [18,19]. More importantly, growing children of healthy weight do not have the same need to lower their adiposity levels as overweight children do, and thus maintenance of their current fitness or adipose status would be considered ideal. Both normal weight and overweight children in the current study experienced reductions in blood pressure which would suggest that the intervention was effective in improving their level of fitness. Thus, it was concluded that normal weight children had a less pronounced response to the intervention program when compared to the overweight group, though both benefitted in terms of improvements in cardiorespiratory fitness. These findings suggest that play-based, fun PA intervention programs are effective in mediating obesity and chronic disease risk factors in susceptible individuals but can be beneficial to physical and emotional health regardless of a child’s weight or risk status.
The second pertinent question examined how health-related quality of life influenced the response in both groups in relation to play-based PA intervention. Higher physical functioning in normal and obese adolescents is associated with increased engagement in vigorous PA regardless of their age or gender [20]. The children with a higher baseline score for physical functioning lost more fat and experienced greater improvements in cardiovascular fitness overall and in the normal weight group but not in the overweight group. Higher physical functioning scores may reflect a discrepancy between perceived and real fitness abilities in overweight children.
Psychosocial functioning includes emotional, social and school functioning domains. Active children tend to score higher on social functioning than their less active peers, possibly due to the link between sport participation and increased social desirability and reinforcement [2]. In addition PA has a positive correlation to concentration and memory, in reference to school functioning domains [18]. The moderate correlation between psychosocial functioning scores and increasingly lower skinfold measurements in the overweight group suggest that intervention environments may be beneficial for this group. However, as seen in Table 1 such an intervention structure may not be beneficial to normal weight youth, for whom already have a higher psychosocial functioning.
Greater self-perceptions of gratification and attractiveness to PA are associated with higher PA and fitness scores in youth [20]. However, in the present investigation higher self-attractiveness scores were associated with decreases in general and cardiorespiratory fitness in the participants overall. The relation according to weight status was unclear, as higher scores were associated with adverse increases in certain fitness variables and beneficial decreases for other in both groups. These results may be due to the influence of gender, since girls and boys in particular differ in their self-perception of attractiveness [20]. In the present investigation, the small sample size made it difficult to further break down the study population by gender. This is a limitation in the present study since most of the associations seen were weak due to the small sample size. However, the results of the study are unique/relevant since the PA intervention allowed for children’s self-directed play-based, fun activities within a positive environment using undergraduate students as role models. Finally physical functioning was associated with fitness improvements following a PA intervention in normal weight youth, whereas psychosocial variables may be directly relevant for interventions targeting overweight youth. The influence of self-perceived attractiveness is unclear and research which controls for gender-based effects is needed. In conclusion, an active play based PA intervention is accompanied by sufficient moderate-to-vigorous PA to improve body composition and cardiovascular fitness for overweight children. The health-related quality of life (HRQL) measures, in particular psychosocial functioning and PA enjoyment, correlate very well with changes in cardiovascular measures suggesting that active play environment is beneficial for improving health and fitness measures in overweight children. In contrast the impact and magnitude of change reported for normal weight children is less following an active play intervention even though PA participation is greater. Therefore active play PA programs, in contrast to training programs, are effective in mediating obesity and beneficial to physical health for overweight children despite a lower psychosocial status and/or greater weight or health risk status.
Author’s Contribution
AB and AM designed and supervised the project. AM was involved in the physical activity and fitness data collection. YA and DMM collected the quality of life data and performed the HRQL data analysis. All four prepared the manuscript with AB having a lead role.
Acknowledgements
We would like to thank Driftwood Community Recreation Centre, the children and their parents/ guardians, and the Faculty of Health Research Grants program for their financial support. Thanks to Dr. Rebecca Gunter for pre-reading and early advise on the manuscript.
Disclosure Statement
No conflict of interest exists for the authors, and/or author's employer or sponsor. No professional relationship with other organizations or with the people working at the Driftwood Recreation. Community Centre such that they may exert an influence on that author's research.
References
- Kelly NR, Masseo SE, Evans RK, Stern M, Thacker LF, et al. (2011) Physical activity, fitness and psychosocial functioning of obese adolescents. Mental Health and Physical Activity 4:31-37.
- Gopinath B, Hardy LL, Baur LA, Burlutsky G, Mitchell P (2012) Physical activity and sedentary behaviors and health-related quality of life in adolescents. Pediatrics 130: 167-174.
- De Bourdeaudhuij I, Lefevre J, Deforche B, Wijndaele K, Matton L, et al. (2005) Physical activity and psychosocial correlates in normal weight and overweight 11 to 19 year olds. Obes Res 13: 1097-1105.
- Calfas KJ and Taylor WC (1994) Effects of physical activity on psychological variables in adolescents. Pediatric Exercise Science 6:406-423.
- Babyak M, Blumenthal JA, Herman S, KhatriP, Doraiswamy M, et al. (2000) Exercise treatment for major depression: Maintenance of therapeutic benefit at 10 months. Psychosom Med 62:633-638.
- Pradinuk M, Chanoine JP, Goldman RD (2011) Obesity and physical activity in children. Can Fam Physician 57: 779-782.
- Roberts KC, Shields M, de Groh M, Aziz A, Gilbert JA (2012) Overweight and obesity in children and adolescents: results from the 2009 to 2011 Canadian Health Measures Survey. Health Rep 23: 37-41.
- Belcastro AN, Morrison KS, Hicks E, Matta H (2012) Cardiorespiratory and metabolic responses associated with children's physical activity during self-paced games. Can J PhysiolPharmacol 90: 1269-1276.
- Active Healthy Kids Canada (2009) The active healthy kids Canada report card on physical activity for children and youth.
- Tremblay MS, Warburton DE, Janssen I, Paterson DH, Latimer AE, et al. (2011) New Canadian physical activity guidelines. ApplPhysiolNutrMetab 36: 36-46.
- Berntsen S, Mowinckel P, Carlsen KH, LødrupCarlsen KC, PollestadKolsgaard ML, et al. (2010) Obese children playing towards an active lifestyle. Int J PediatrObes 5: 64-71.
- Bonomi AG, Goris AH, Yin B, Westerterp KR (2009) Detection of type, duration, and intensity of physical activity using an accelerometer. Med Sci Sports Exerc 41: 1770-1777.
- Varni JW, Seid M, Kurtin PS (2001) PedsQL 4.0: reliability and validity of the Pediatric Quality of Life Inventory version 4.0 generic core scales in healthy and patient populations. Med Care 39: 800-812.
- Brustad R (1993) Who will go out and play? Parental and psychological influences on children's attraction to physical activity. Pediatric Exercise Science 5: 210-210.
- Cook S, Auinger P, Huang TT (2009) Growth curves for cardio-metabolic risk factors in children and adolescents. J Pediatr 155: S6.
- Fernandez JR, Redden DT, Petrobelli A, Allison DB (2004) Waist circumference percentiles in nationally representative samples of African-American, European –American and Mexican-American children and adolescents. JPediatr 6: 439-444.
- Katzmarzyk PT, Srinivasan SR, Chen W, Malina RM, Bouchard C, et al. (2004) Body mass index, waist circumference, and clustering of cardiovascular disease risk factors in a biracial sample of children and adolescents. Pediatrics 114: 198-205.
- Strong WB, Malina RM, Blimkie CJ, Daniels SR, Dishman RK, et al. (2005) Evidence based physical activity for school-age youth. J Pediatr 146: 732-737.
- Tsao Y (2008) Using guided play to enhance children's conversation, creativity and competence in literacy. Education 128:515-20.
- Raudsepp L, Liblik R,Hannus A (2002) Children’s and adolescents’ physical self-perceptions as related to moderate to vigorous physical activity and physical fitness. PediatrExer Sci 14: 97-106.
Relevant Topics
- Adolescent Anxiety
- Adult Psychology
- Adult Sexual Behavior
- Anger Management
- Autism
- Behaviour
- Child Anxiety
- Child Health
- Child Mental Health
- Child Psychology
- Children Behavior
- Children Development
- Counselling
- Depression Disorders
- Digital Media Impact
- Eating disorder
- Mental Health Interventions
- Neuroscience
- Obeys Children
- Parental Care
- Risky Behavior
- Social-Emotional Learning (SEL)
- Societal Influence
- Trauma-Informed Care
Recommended Journals
Article Tools
Article Usage
- Total views: 15005
- [From(publication date):
October-2015 - Apr 07, 2025] - Breakdown by view type
- HTML page views : 10394
- PDF downloads : 4611