Co-Occurring Conditions among Young Adults who Stutter
Received: 03-Apr-2023 / Manuscript No. jspt-23-94151 / Editor assigned: 05-Apr-2023 / PreQC No. jspt-23-94151(PQ) / Reviewed: 19-Apr-2023 / QC No. jspt-23-94151 / Revised: 24-Apr-2023 / Manuscript No. jspt-23-94151(R) / Accepted Date: 29-Apr-2023 / Published Date: 01-May-2023 DOI: 10.4175/2472-5005.1000181
Abstract
Population-based studies allow inferences to be made about large segments of the population. However, a limitation to many population-based studies is that they rely on secondhand reports. This study examined the incidence of five nonspeech- language co-occurring conditions to stuttering that have been self-reported, using a nationally representative sample of young adults (ages 24-32 years) including some conditions that relatively few studies have explored. Analyses of the association between stuttering and self-reported asthma, attention-deficit disorder/attention-deficit hyperactivity disorder (ADD/ADHD), anxiety, depression, and epilepsy diagnosis were conducted using the National Longitudinal Study of Adolescent to Adult Health. First the incidence of each condition among respondents with and without stuttering was evaluated. Second, logistic regression was used to evaluate the relationship between stuttering and each condition, controlling for demographic and parental attributes. Among reports from young adults, stuttering was associated with increased odds of experiencing the following examined conditions asthma, ADD/ADHD, anxiety, and depression. The increased odds of these conditions among people who stutter were significant after controlling for personal characteristics. This study reinforces and extends similar previous findings by showing increased odds of these co-occurring conditions among self-reports from young adults who stutter. While the mechanism(s) linking these conditions to stuttering remains unclear, clinicians and researchers should be aware of these co-occurring conditions and their potential influence on outcomes.
Keywords
Stuttering; Co-occurring conditions; Adults
Introduction
Stuttering is an involuntary communication disorder whose overt behaviors are commonly characterized by sound or word repetitions, sound prolongations, audible or inaudible postural fixations, and aberrant body movements [1]. While listeners recognize these behaviors as symptoms of stuttering, the processes of speech production for people who stutter (PWS) include a range of less observable behaviors. For example, PWS anticipate moments of stuttering [2]. This anticipation of stuttering can occur in the moment of speaking or well before linguistic units have been selected [3]. While anticipation of stuttering does not necessarily effectuate a negative response, this experience can ultimately lead to avoidances of sounds, words, people, places, or situations [2,4]. Collectively, negative thoughts, feelings, or behaviors as responses to the presence of stuttering [1] can lead to the reality of impacted well-being [5]. Beyond the struggles that stuttering directly induces, subgroups of PWS are left to overcome the challenges posed by co-occurring conditions.
Beyond reports of co-occurring speech/language related disorders [6-8], previous studies have provided evidence of co-occurring, non-speech related disorders and delays, which have profiled the rate of learning and/or reading disabilities, autism, attention-deficit hyperactivity disorder (ADHD), seizures, sleep issues, allergies, asthma, executive functioning impairments, emotional and social issues, among others [6-15]. However, gaps remain in the literature due to a variety of factors including limited reports of some co-occurring conditions leading to inconclusive findings, a heavy reliance on speech-language pathologists’ (SLP) or parental reported data, and many studies with a primary focus on co-occurring conditions among children who stutter (CWS). For example, while previous research has found a relationship between the broad category of speech disorders and asthma [16,17], less research has focused solely on the connectedness of asthma and stuttering. Recent findings using two separate large datasets suggesting a relationship between asthma and stuttering [13,18] indicate a need to further explore the association between these two conditions.
Additionally, previous studies examining the relationship between ADHD and stuttering have primarily analyzed samples of children [12,19,20]. While less focus has been given to adults who stutter and ADHD, a recent study found a relatively high percentage of adults who stutter experience characteristics of ADHD [21]. Tichenor et al. (2021) concluded their paper highlighting the need for continued research on the overlap between stuttering and ADHD.
Knowledge of these co-occurring conditions can directly influence clinical approaches and has the potential of steering guidance given to caregivers, teachers, and others involved in the well-being of PWS. In the case of asthma, beyond the clinical reports of negatively impacting direct treatment of stuttering [22], adults with asthma are more likely to suffer from obstructive sleep apnea [23]. Recent reports of sleep issues among PWS necessitate the identification of conditions that may further put individuals at risk of less than adequate sleep [24,25]. Additionally, SLPs working with individuals with ADHD should be aware of the impacts of attentional issues on self-monitoring and implementation or revisions of speech motor plans during therapy approaches that target speech modifications, where these added barriers may result in increased time to meet desired goals [19].
Few studies have examined the incidence of these conditions via self-reports from adults who stutter (AWS) resulting in a lack of clarity as to which co-occurring conditions persist into adulthood and which conditions take divergent paths and resolve during childhood. Additional insights are possible through utilization of patient reported data, particularly when inferences can be made to the population based on analyses of that data [26]. To our knowledge, few studies have targeted young adults in the 24-to-32-year age range using a nationally representative sample of self-reported data. Gerlach et al. (2018) reported on elevated ADHD and learning disability among PWS in the same dataset as being used for the current project. However, their analysis focused on labor market outcomes among PWS and did not extend beyond the descriptive level for those two variables. This study fills a gap in the existing literature by exploring the incidence of coexisting conditions, self-reported by PWS and people who do not stutter (PWNS). This analysis will add to previous findings, which showed increased incidence of non-speech related conditions primarily via secondary reports, by examining self-reported data of young adults with stuttering. Self-reported data decreases interpretation bias introduced in secondhand reports and incorporates a comprehensive individual perspective that is missing in electronic health records (EHR) [27,28]. Addressing these issues, using self-reported measures, among a sample of young adults precludes the possibility that the presence of coexisting conditions is influenced by secondhand reports.
Method
Study sample
To appropriately address the incidence of stuttering and other conditions in self-reports from young adults, this study utilized data from the National Longitudinal Study of Adolescent to Adult Health (ADD Health)-a nationally-representative, longitudinal panel of the US population containing self-reported information on social, economic, psychological, and physical well-being as well as contextual information on the family, neighborhood, community, school, friendships, peer groups, and romantic relationships. ADD Health followed a sample of 12,105 adolescents in 7th to 12th grade during the 1994-1995 school years (ages 12 to 17) with four in-home interviews occurring at irregular intervals. Wave I was collected in 1994/95 when participants were 12 to 17 years old. Waves II and III were collected in 1996 and 2001/02, respectively. This study utilizes Wave IV which was collected in 2008 when respondents were 24 to 32 years old. While each wave consisted of a slightly different questionnaire with a different focus, Wave IV Section 6: Illness, Medications, and Physical Disabilities included detailed information on participants’ medical diagnoses and condition status. For additional information on the ADD Health survey and sampling process, see http://www.cpc.unc.edu/projects/ addhealth/design.
ADD Health has been used extensively to study a variety of topics related to stuttering and characteristics of PWS. Studies concerning labor market outcomes [29,30], aggressive behavior [31], sleep patterns [32,25], depression and suicidal ideation [24], and esophagusmuscularis tissue variation [33] among PWS used these data to generate robust findings and unique differences between those who do and do not stutter. However, to date, no research has used ADD Health to evaluate differences in the prevalence of asthma, ADD/ADHD, anxiety, depression, and epilepsy.
Identification of stuttering
The survey item regarding stuttering was only included in ADD Health Waves III and IV. In these waves, respondents were asked the question ‘Do you have a problem with stuttering or stammering?’ To identify individuals with stuttering and to ensure that individuals did not misidentify themselves as a PWS, individuals in this study were only classified as a PWS if they reported ‘yes’ to the survey question regarding stuttering in both waves. This classification scheme resulted in 261 PWS (unweighted), which represents 1.8 percent of the sample. Descriptive statistics for key variables of PWS and PWNS are provided in Table 1.
Demographic characteristics
Demographic characteristics include respondents’ sex, age, race, and ethnicity. The sample was 47% male and over 25% minority race/ ethnicity. Differences were present in the composition of people who do and do not stutter as a function of race. Specifically, Hispanics and African Americans, comprised roughly 14% and 29% of PWS, respectively, compared to comprising roughly 11% and 14% of PWNS, (African American: χ2=18.66, p<0.0001; Hispanic: χ2=4.88, p=0.003), respectively. Stuttering was also more prevalent among males than females who made up 60% of PWS, (χ2=19.44, p=0.002). Average age was 28 (sd=0.12) years with little difference between PWS and PWNS, (t=0.94, p=0.35).
Income
Respondents provided an estimate of their personal, pre-tax earnings which included wages or salaries, including tips, bonuses, and overtime pay, and income from self-employment. Average earnings were $35,766.34 (sd=$45,526.51) per year for PWNS. PWS earned significantly less with annual earnings reported at $29,182.14 (sd=$65,168.91) (t=15.47, p<0.0001). In the regression model, income was included in logarithmic form to account for potential socioeconomic differences.
Parental characteristics
Nearly all parents of PWNS (96%) were married compared to only 90% of parents of PWS-a statistically significant difference (χ2= 9.6, p=0.002). Education is represented by a set of discrete values ranging from one to nine. These values represent the number of years of postsecondary education. On average, parents of PWNS (5.6, sd=0.10) had greater educational attainment than parents of PWS (4.7, sd=0.26), a statistically significant difference (χ2= 20.8, p=0.013).
Co-Occurring conditions
Section 6 of the Wave IV ask respondents whether a doctor, nurse, or other health care provider has ever diagnosed him/her with a condition, which included the following five conditions: asthma, ADD/ ADHD, anxiety, depression, and epilepsy. Conditions in this section were selected since they were self-reported, maintained a uniform questioning framework, and presented clear criteria for diagnosis.
Analysis
All analyses were performed using SAS 9.4 (Cary, NC) proc survey logistic. The ADD Health study design used a clustered sample in which the clusters were sampled with unequal probability. While reducing the cost of data collection, this design complicates the statistical analysis because the observations are no longer independent and identically distributed. To analyze the data correctly requires the use of special survey software packages specifically designed to handle observations that are not independent and identically distributed.
The proc survey logistic procedure estimated the logistic regression model taking the survey design and data collection methods into account. In addition to survey procedures that accounted for sampling variation, estimates were also weighted. The ADD Health sampling weights were designed to turn the sample of adolescents interviewed into the representative population we intended to study. Unless appropriate adjustments are made for sample selection and participation, estimates from analyses using the ADD Health data can be biased when any factor used as a basis for selection as a participant in the study also influences the outcome of interest. To obtain unbiased estimates, it is important to account for the sampling design by using analytical methods designed to handle clustered data collected from respondents with unequal probability of selection.
By using these sampling weights and model specifications that account for regional stratification and the clustering of adolescents within schools, analysis produced unbiased estimates of population parameters and standard errors. Regression analysis tested for differences in the incidence of co-occurring conditions in PWS and PWNS, controlling for age, race, sex, parental attributes, and income. Five logistic regressions (one for each condition) were run using the same empirical specification to evaluate each condition individually. The regression modeled a binomial outcome coded as 0 or 1 to indicate whether each respondent reported the condition of interest. The model was used to obtain the odds ratio which indicates the relative likelihood of the dependent variables, adjusting for the independent variables.
Results
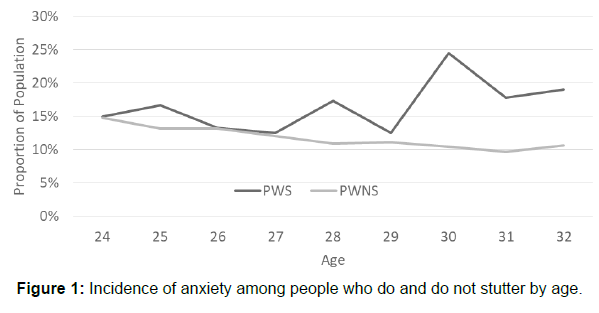
PWS had a higher proportion of asthma (15.7% vs. 14.3%), ADD/ ADHD (10% vs. 4.5%), anxiety (16.1% vs 11.2%), depression (25.3% vs. 14.6%), and epilepsy (2.3% vs. 1.2%) compared to PWNS (Table 1). However, differences in the portion of the populations with these conditions were only statistically significant for ADD/ADHD (χ2=2.5, p<0.001), anxiety (χ2=6.1, p=0.01), and depression (χ2=23.3, p<0.001) (Table 2). The disparity in anxiety incidence between PWS and PWNS is depicted in Figure 1.
| N | Mean | Std Dev | ||||
|---|---|---|---|---|---|---|
| Age | 10373 | 28.30001 | 0.119095 | |||
| logIncome | 9267 | 10.16558 | 0.027136 | |||
| Parent Education | 8997 | 5.517258 | 0.097751 | |||
| N | Percent | |||||
| Male | 10372 | 0.467087 | ||||
| Stutter | 9707 | 0.018332 | ||||
| Hispanic | 10339 | 0.11003 | ||||
| African American | 10357 | 0.145996 | ||||
| Parent Married | 9027 | 0.959855 | ||||
| Asthma | 2096 | 14.31 | ||||
| Depression | 2164 | 14.77 | ||||
| Anxiety | 1655 | 11.3 | ||||
| Epilepsy | 180 | 1.23 | ||||
| Stutter=0 | Stutter=1 | |||||
| N | Mean | Std Dev | N | Mean | Std Dev | |
| Age | 9552 | 28.30024 | 0.118645 | 155 | 28.6287 | 0.234956 |
| logIncome | 8547 | 10.19072 | 0.024855 | 134 | 9.862164 | 0.133098 |
| Parent Education | 8271 | 5.574082 | 0.096761 | 144 | 4.739442 | 0.255435 |
| N | Percent | N | Percent | |||
| Male | 9551 | 0.45818 | 155 | 0.598926 | ||
| Hispanic | 9523 | 0.106683 | 154 | 0.143098 | ||
| African American | 9537 | 0.140972 | 155 | 0.283934 | ||
| Parent Married | 8302 | 0.963178 | 143 | 0.898188 | ||
| Asthma | 2055 | 14.28 | 41 | 15.71 | ||
| Depression | 2098 | 14.58 | 66 | 25.29 | ||
| Anxiety | 1613 | 11.21 | 42 | 16.09 | ||
| Epilepsy | 174 | 1.21 | 6 | 2.3 | ||
| ADD/ADHD | 646 | 4.49 | 26 | 9.96 | ||
Table 1: Descriptive statistics of key covariates by stuttering status.
| Chi-Square | p-Value | |
|---|---|---|
| Asthma | 0.424 | 0.515 |
| Depression | 23.3251 | <.0001 |
| Anxiety | 6.0903 | 0.0136 |
| Epilepsy | 2.5061 | 0.1134 |
| ADD/ADHD | 17.5297 | <.0001 |
| *=Calculated using cross sectional sampling weights | ||
Table 2: Chi-square test of differential between young adults who do and do not stutter.
Logistic regression results modeled the probability of reporting the condition accounting for demographic and parental differences (Table 3). In the results from these regression models, a positive coefficient represented a higher log-odds ratio of the given characteristic for the respective parameter. For ease of interpretation, odds ratios were provided which quantify the relative probability of the condition given the independent characteristic. Income was significant for asthma, ADD/ADHD, anxiety, depression, and epilepsy. While there were some small differences in the racial/ethnic probability of these conditions, most demographic and parental characteristics were insignificant.
Stuttering had a statistically significant association with asthma (OR=2.1, CI= 1.04-4.27), ADD/ADHD (OR=2.3, CI=0.94-5.77), anxiety (OR=1.7, CI=0.90-3.34), and depression (OR=2.2, CI=1.19- 3.9) at the 95% level. Odds ratios represented the likelihood of PWS having been diagnosed with a given condition relative to PWNS. Ratios less than one indicated that PWS had a lower probability of having the condition. Odds ratios in Table 3 indicated that PWS had a higher likelihood of having asthma, ADD/ADHD, anxiety, and depression compared to PWNS.
| Dependent Variable | Asthma | Depression | Anxiety | Epilepsy | ADD/ADHD | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Not Diagnosed | 6380 | 6374 | 6645 | 7397 | 7146 | |||||||||||||
| Diagnosed with Condition | 1092 | 1098 | 827 | 75 | 326 | |||||||||||||
| Model Fit Statistics | ||||||||||||||||||
| AIC | 9666580 | 9798548 | 8540427 | 1235289 | 4454718 | |||||||||||||
| SC | 9666594 | 9798562 | 8540442 | 1235303 | 4454733 | |||||||||||||
| -2 Log L | 9666578 | 9798546 | 8540425 | 1235287 | 4454716 | |||||||||||||
| Parameter | Std Err | Odds Ratio | Std Err | Odds Ratio | Std Err | Odds Ratio | Std Err | Odds Ratio | Std Err | Odds Ratio | ||||||||
| Intercept | 0.316 | 0.802 | 1.290 | 0.797 | 0.579 | 1.041 | 1.803 | 3.554 | 0.006 | 1.353 | ||||||||
| Male | -0.285 | 0.113 | 0.752 | -0.954 | 0.088 | 0.385 | -0.884 | 0.094 | 0.413 | -0.063 | 0.299 | 0.939 | 0.978 | 0.156 | 2.659 | |||
| Stutter | 0.744 | 0.358 | 2.104 | 0.769 | 0.301 | 2.156 | 0.550 | 0.332 | 1.734 | 0.120 | 0.990 | 1.128 | 0.847 | 0.457 | 2.334 | |||
| Hispanic | 0.056 | 0.169 | 1.057 | -0.131 | 0.192 | 0.877 | -0.482 | 0.189 | 0.618 | -0.925 | 0.731 | 0.397 | -0.841 | 0.316 | 0.431 | |||
| African American | 0.035 | 0.112 | 1.036 | -0.834 | 0.166 | 0.434 | -1.373 | 0.173 | 0.253 | 0.249 | 0.477 | 1.283 | -1.192 | 0.389 | 0.304 | |||
| log Income | -0.108 | 0.043 | 0.897 | -0.220 | 0.043 | 0.803 | -0.143 | 0.042 | 0.867 | -0.280 | 0.098 | 0.756 | -0.365 | 0.057 | 0.694 | |||
| Parent Education | 0.036 | 0.020 | 1.036 | 0.024 | 0.023 | 1.024 | -0.031 | 0.021 | 0.969 | 0.022 | 0.087 | 1.022 | 0.132 | 0.036 | 1.141 | |||
| Parent Married | 0.077 | 0.209 | 1.080 | -0.265 | 0.242 | 0.767 | -0.367 | 0.287 | 0.693 | -0.310 | 0.757 | 0.733 | 0.489 | 0.600 | 1.630 | |||
| Age | -0.040 | 0.025 | 0.961 | -0.007 | 0.024 | 0.993 | -0.002 | 0.029 | 0.998 | -0.123 | 0.094 | 0.885 | -0.036 | 0.038 | 0.965 | |||
| *=Denotes Significant at 95% Level; **=Cross Sectional Sampling Weights Applied; ***=Data Source: Longitudinal Survey of Adolescent to Adult Health | ||||||||||||||||||
Table 3: Logistic regression of co-occurring conditions in young adults who do and do not stutter.
Discussion
This study examined the incidence of five self-reported conditions among PWS and PWNS. Findings suggest that PWS have increased odds of experiencing asthma, ADD/ADHD, anxiety, and depression. Previous analyses have examined similar conditions among CWS; however, this study extends those findings by examining co-occurrences that were self-reported by those in young adulthood.
Conditions with a significantly different representation between people who do and do not stutter
Asthma
Previous studies have helped to uncover a relationship between the broad classification of speech disorders and asthma [16,17]. Studies on the relationship between stuttering and asthma are minimal, although this possible association was considered years ago as part of the Iowa studies [34]. In Study III of the ‘Iowa studies’, 150 controls and 150 of those in the experimental group were asked, ‘What illnesses did the child have (more than one month before) the onset of stuttering?’ [35]. With regard to asthma, differences were minimal between the two groups—only 3 males in the control group and 4 males in the experimental group indicated that asthma was present. Study III also asked, ‘What other illnesses has the child had since one month after onset of stuttering?’, where 6 males in the control group indicated ‘asthma’ as compared to 2 males in the experimental group [35]. While these findings did not indicate an association between stuttering and asthma, methodological limitations may contribute to differences in findings in the Iowa studies and results from more recent investigations. Ajdacic-Gross et al., (2018) found increased odds of asthma in a sample of over four thousand Swiss adults [18]. Additionally, Briley and Merlo (2020) [13] found asthma to be more prevalent among CWS in a sample from the National Health Interview Survey, including roughly 10,000 children. The literature also includes anecdotal evidence of asthma being a condition that acts as a barrier to optimal outcomes [22] along with speculation that the relationship between asthma and stuttering may related to the timely coordination (or lack thereof) of respiration and phonation [36]. The association between stuttering and asthma requires further investigation and would likely benefit from interdisciplinary collaborations including sleep specialists, allergists, and pulmonologists.
ADD/ADHD
Findings from the current study revealed that roughly 10% of the sample of PWS self-reported a diagnosis from a doctor of ADD/ADHD, compared to roughly 4.5% of PWNS. In previous analyses, CWS have exhibited significantly higher rates of ADHD compared to CWNS [12]. Odds of having ADHD/ADD were greater among the sample of 3–17-year-old CWS, and odds were also greater at each age range (3-5 years, 6-10 years, and 11-17 years), after controlling for sex, race, parent education, and family income. Similarly, Boulet et al. (2009) [10] reported a considerably higher rate (43.1%) of ADHD/ADD among CWS using 1997-2005 NHIS datasets. More recently, in Tichenor et al.’s (2021) [21] sample of 254 adults, they noted a discrepancy between the percentage of those PWS who reported having a formal diagnosis of ADHD (7.5%) and those symptomatic of ADHD (23.6%).
Results of a higher incidence of ADD/ADHD in the current study represent an increase from Blood et al.’s (2009) and Arndt and Healy’s (2001) findings of 5.6% and 3.6%, respectively, of CWS also experiencing ADHD/ADD. Higher rates of ADHD/ADD from recent reports compared to those observed in studies from 2001 and 2009 are not surprising, as overall diagnoses of ADHD have increased as a function of time [28]. Of note, while Pruett, et al. (2021) did not find significant differences between those who stutter and matched controls, the percentage of stuttering cases in their sample also reporting ADHD (roughly 8.6%) was relatively close to what was found in the current sample. Another consideration is their analysis of electronic health records for a single University health center was limited by comorbidities that were documented in EHRs during the observation window.
Past studies showing a relationship between stuttering and ADHD suggested genetic commonalities [37] with common neurological involvement [38-40]. Regarding stuttering’s relationship to the basal ganglia, Alm (2004) [38] discussed Seeman et al.’s (1987) [41] postmortem data on D1 dopamine receptor and D2 dopamine receptor density in the putamen from 244 children and adults. In Seeman et al.’s (1987) sample, male children exhibited a smaller D1/D2 ratio. It is suggested that this imbalance in D1- and D2-receptors results in dysfunction between inhibition and facilitation of movement. The age at which the D1/D2 ratio reverses course and begins to increase follows the age at which most children recover from stuttering [38]. Alm (2004) concluded this to be a possible mechanism that accounts for sex differences in rates of stuttering and in natural recovery in many CWS [42]. In the context of the current study, these associations are important due to stuttering’s relationship with the dopaminergic system, which is also involved in ADHD [43]. Additionally, stuttering and ADHD share characteristics of occurring more frequently in males and being exacerbated by stress [20]. Of interest are questions related to the neurobiological similarities and differences in all combinations of male and female children, including those who do and do not stutter and those with and without ADHD. Future studies addressing these questions might provide critical pathophysiological evidence, contributing to etiological research.
Clinically, identification of co-occurring ADHD in PWS prompts additional considerations for SLPs since over two-thirds of individuals with ADHD suffer from at least one co-existing condition and up to half of children with ADHD also suffer from a learning disorder [44]. For example, in the presence of a suspected learning disorder rooted in reading difficulty, it should be determined if deficits in reading outcomes are a result of a true delay or if stuttering behaviors are mirroring difficulties in decoding (Blood et al., 2003). That is, are breaks in speech resulting from reduced reading fluency or in stuttering induced breaks in the forward flow of speech. Determination of the presence of ADHD may also result in divergent clinical approaches. For example, deficits in reading ability may prompt usage of sentence formulation tasks over reading passages as stimuli used in therapy when learning/practicing behavioral techniques. If the determination is that the reader’s behaviors are resulting from stuttering and not reading difficulty, then a clinical approach may be to use passages with increased linguistic complexity as the PWS’ work towards implement motoric adaptations while taxing the system with complex stimuli. The complex interactions of symptoms described above are not limited to stuttering and reading difficulty and the association between stuttering and the common coexisting conditions of ADHD should be considered in this context. Clinical awareness of high rates of co-occurring ADHD among PWS is imperative given that differences in attributes of ADHD call for varying clinical approaches [20], and the presence of ADHD symptoms may necessitate longer durations of intervention when reduction of observable behaviors of stuttering is included as an outcome measure [19]. Ultimately, any behavioral adaptation (e.g., cancellations, prolonged speech, preparatory sets, etc.) [45] can be negatively influenced by ADHD, where distractibility or lack of attention creates a barrier to learning and implementation of these behavioral changes. While ADD/ADHD among PWS is biological in nature, the higher incidence of anxiety among young AWS in the present sample is more likely a result of stuttering instead of being a true co-occurring disorder [46].
Anxiety/panic disorders and depression
Findings of increased anxiety among those in the current sample were consistent with other studies indicating that anxiety is more prevalent among all ages of PWS [46-50]. Previous findings merged with current results suggest that PWS are at risk of developing anxiety early in life and potentially having it persist into adulthood. The anxiety experienced by both children and young AWS is likely generated from both internal and external contributors and relates to both the reaction they receive from others and the feelings they experience when communicating [51,52]. Anxiety may be undue and a result of false perceptions of how others would perceive or respond stuttering. Additionally, anticipation of stuttering can lead to anxiety [2, 49,53]. In both children and adults who stutter, anxiety can be a precursor to avoidance behaviors [54,55].
Importantly, anxiety in PWS is not dependent on severity of stuttering’s observable behaviors [48]. Furthermore, evidence that anxiety exists in childhood and adulthood among PWS indicates that these common difficulties often go unnoticed or untreated, increasing the likelihood that these issues worsen in severity, impede social development, negatively impact labor market outcomes, and interfere with social function [56-58]. The current findings concerning adults echo findings from studies showing issues of social and emotional wellbeing among CWS [59]. Therefore, early identification and treatment of anxiety among PWS is critical. While unhealthy thoughts, feelings, and/ or reactions to stuttering may, at times, not receive equal consideration to more overt symptomatology, these unobservable behaviors could potentially be detrimental to long-term social, emotional, and behavioral well-being. Fear of social situations and negative peer evaluation contribute to social anxieties [60,61], and comprehensive treatment during the developmental years could reduce these negative impacts in young adults, thus improving long term quality of life for PWS. Treating SLPs should consider the full range of impact of stuttering on the individual [62], and healthcare providers treating young PWS should carefully screen for and address all pertinent issues to prevent persistence and/or exacerbation as PWS age. This type of comprehensive treatment goes beyond traditional behavioral therapies and aids in addressing the full impact of stuttering [63]. Once a client has learned to modify speech patterns to work through moments of stuttering, an approach to directly work towards reducing anxiety is exposure therapy [64]. Another critical aspect of treatment in CWS or young AWS who still live with their parents is parental involvement [65], and this is especially important for PWS who are susceptible to feelings of anxiety in social situations.
While commonly co-occurring, anxiety and depression represent two separate constructs [66]. Anxiety includes negative cognitive, behavioral, and physiological reactions in response to a threat [67]. Depression involves a range of symptomatology that impacts feelings, thoughts; lasts at least two weeks; and results in a change in prior functioning [68]. Stein et al. (2001) reported that social anxiety disorder early in life is a predictor of depression later in life [69]. While data cannot be used to determine causality of reported depression in the current sample, it is not difficult to imagine a scenario where the anxieties induced by the ubiquitous nature of stuttering (not necessarily observable stuttering behaviors) could lead to depression in an untreated PWS. Efforts to thwart this negative outcome include teaching new responses to moments of stuttering and anticipated moments of stuttering, which result in the PWS approaching situations that were once avoided. Outcomes of such an approach include increased social participation, along with strengthening and reinforcing self-efficacy [70-73].
Comprehensively addressing these issues in younger clients will most likely aid optimal outcomes for PWS. As described by previous research, these issues of social and emotional well-being among PWS could be compounded by learning, attentional, or other coexisting conditions [74,11]. However, the simultaneous co-occurrence of stuttering and ADD/ADHD, anxiety disorders, makes it difficult to disentangle the individual effects and trajectories throughout the life course. Awareness of these and other co-existing conditions could assist with identification and treatment thus reducing their incidence and impact in adulthood.
Additional noteworthy finding
While the intended purpose of this study was to examine differences in profiles between people who do and do stutter, our analyses uncovered additional findings that deserve mention. First, stuttering occurred more commonly among African Americans and Hispanics. Few studies have explored the influence of race/ethnicity on the presence of stuttering, and for those that have; there are conflicting results [12,75,76]. Recognizing these inconsistencies, Briley and Ellis (2020) [77] utilized 6 years of data from the National Health Interview Survey (NHIS) to explore differences in the presence of stuttering between racial and ethnic groups. Using White children as the reference group, African American children, but not Hispanic children, had greater odds of experiencing stuttering, and these finding were consistent across all regions of the United States, with the exception of the Northeast. While the authors acknowledged that their study could not determine causality, they speculated that a potential contributor could be differences in environmental influences as a function of race and residence.
Limitations
Despite compelling evidence of the co-occurrence between stuttering and other developmental conditions, this study faced several limitations. First, all ADD Health data used in the analysis was selfreported. While self-reported data has several advantages compared to secondhand reports, it is also subject to recall, social desirability, and question order bias. Additionally, it is possible that some respondents based an affirmative answer to the stuttering question based on overt symptomatology or some other incomplete or inaccurate definition. Therefore, it is possible that results on the presence of stuttering could be both an over- or under-representation. Second, the five conditions examined were chosen based on their suspected association with stuttering – having been examined in previous studies rather than examining a battery of conditions. It should be noted that two conditions that had previously been associated with stuttering were ultimately excluded from the current study. One of the items that was excluded probed snoring, which asked, ‘based on what you have noticed or what others have told you, are there times when you snore or you stop breathing during your sleep?’ Recently, Merlo et al. (2022) examined the same dataset as the current study and found that PWS are at greater odds of reporting affirmatively. Due to its recent inclusion in a separate study, this variable was not included in the current study. The other excluded item asked respondents, ‘have you had active seasonal allergies (hay fever) in last four weeks?’ Although PWS in the current study were at greater odds of having seasonal allergies, the limitations of only asking about the prior four weeks prevents adequate comparisons to previous studies that examined allergies among PWS. Since answers could be biased by the month/season in which the survey was administered, variations could exist in sample sizes reporting allergies, obscured differences between the sample and the population means, and increased standard errors of estimates. Third, analysis only examined the likelihood of having been diagnosed with a given condition. The severity and duration of persistence were not considered. Furthermore, no controls for treatment of stuttering or co-occurring conditions were available in the data. Respondents may have been receiving treatment or have previously been treated for stuttering or any of the conditions examined. Fourth, results indicated a significant correlation between diagnosis and income. In the United States, individuals with higher income are more likely to receive regular healthcare which subsequently increases the likelihood of diagnosis. Lower healthcare utilization could result in a higher incidence of undiagnosed conditions among lower income households. Higher health services utilization by households with higher income, increased the probability of diagnosis. Households with lower income and lower healthcare utilization may have had a higher incidence of undiagnosed, therefore unreported, cases. Finally, like all large-scale surveys, questions can be skipped, or responses can be deemed invalid. Skipped or invalid responses were partially responsible for the response variation among these conditions. Variation in responses and survey patterns could have contributed to variation in findings between surveys.
Conclusion
Despite these limitations, these findings indicate the complexity of issues among all individuals who stutter. Data reported here indicate that, the odds of self-reporting asthma, ADD/ADHD, anxiety, and depression differs significantly between those who do and do not stutter. While these findings could raise awareness of additional risks among PWS, determinations regarding treatment should be made by providers on the individual level. Additional research is needed to determine the nature, impact, and trajectory of these co-occurring conditions over the life course.
Data availability statement: Due to legal restrictions, supporting data is not available.
The ADD Health data that we used, specifically the extensive restricted-use data, can only be obtained with approval of the Carolina Population Center (https://addhealth.cpc.unc.edu/data/).
Acknowledgement
Not applicable.
Conflict of Interest
The authors report there are no competing interests to declare.
References
- Tichenor SE, Yaruss JS (2019) Group experiences and individual differences in stuttering. J Speech Lang Hear Res 62:4335-4350.
- Jackson ES, Yaruss JS, Quesal RW, Terranova V, Whalen DH (2015) Responses of adults who stutter to the anticipation of stuttering. J Fluency Disord 45:38-51.
- Crichton-Smith I (2002) Communicating in the real world: Accounts from people who stammer. J Fluency Disord 27:333-352.
- Petrunik M, Shearing CD (1983) Fragile facades: Stuttering and the strategic manipulation of awareness. Social Prob 31:125-138.
- Craig A, Blumgart E, Tran Y (2009) The impact of stuttering on the quality of life in adults who stutter. J Fluency Disord 34:61-71.
- Arndt J, Healey EC (2001) Concomitant disorders in school-age children who stutter. Lang Speech Hear Serv Sch 32:68-78.
- Blood GW, Ridenour VJ, Qualls CD, Hammer CS (2003) Co-occurring disorders in children who stutter. J Commun Disord 36:427-448.
- Ntourou K, Conture EG, Lipsey MW (2011) Language abilities of children who stutter: A meta-analytical review. Am J Speech Lang Pathol 20:163-179.
- Blood GW, Blood I, Kreiger J, O'Connor S, Qualls CD (2009) Double jeopardy for children who stutter: race and coexisting disorders. Commun Disord Quart 30:131-141.
- Boulet SL, Boyle CA, Schieve LA (2009) Health care use and health and functional impact of developmental disabilities among US children, 1997-2005. Arch Pediatr Adolesc Med 163:19-26.
- Briley PM, O’Brien K, Ellis C (2019) Behavioral, emotional, and social well-being in children who stutter: evidence from the National Health Interview Survey. J Dev Phys Disab 31:39-53.
- Briley PM, Ellis Jr C (2018) The coexistence of disabling conditions in children who stutter: Evidence from the national health interview survey. J Speech Lang Hear Res 61:2895-2905.
- Briley PM, Merlo S (2020) Presence of allergies and their impact on sleep in children who stutter. Perspect ASHA SIGs 5:1454-1466.
- Choo AL, Smith SA, Li H (2020) Associations between stuttering, comorbid conditions and executive function in children: a population-based study. BMC psychol 8:1-19.
- Merlo S, Briley PM (2019) Sleep problems in children who stutter: Evidence from population data. J Commun Disord 82:935.
- Keating D, Turrell G, Ozanne A (2001) Childhood speech disorders: reported prevalence, comorbidity and socioeconomic profile. J Paediatr Child Health 37:431-436.
- Strom MA, Silverberg JI (2016) Asthma, hay fever, and food allergy are associated with caregiver‐reported speech disorders in US children. Pediatr Allergy Immunol 27:604-611.
- Ajdacic-Gross V, Bechtiger L, Rodgers S, Mülle, M, Kawohl W, et al. (2018) Subtypes of stuttering determined by latent class analysis in two Swiss epidemiological surveys. PloS one 13:8450.
- Druker K, Hennessey N, Mazzucchelli T, Beilby J (2019) Elevated attention deficit hyperactivity disorder symptoms in children who stutter. J Fluency Disord 59:80-90.
- Donaher J, Richels C (2012) Traits of attention deficit/hyperactivity disorder in school-age children who stutter. J Fluency Disord 37:242-252.
- Tichenor SE, Johnson CA, Yaruss JS (2021) A preliminary investigation of attention-deficit/hyperactivity disorder characteristics in adults who stutter. J Speech Lang Hear Res 64:839-853.
- Daly DA, Simon CA, Burnett-Stolnack M (1995) Helping adolescents who stutter focus on fluency. Lang Speech Hear Serv Sch 26:162-168.
- Teodorescu M, Polomis DA, Hall SV, Teodorescu MC, Gangnon RE, et al. (2010) Association of obstructive sleep apnea risk with asthma control in adults. Chest 138:543-550.
- Briley PM, Gerlach H, Jacobs MM (2021) Relationships between stuttering, depression, and suicidal ideation in young adults: Accounting for gender differences. J Fluency Disord 67:105820.
- Merlo S, Jacobs MM, Briley PM (2022) Symptoms of Obstructive Sleep Apnea in Young Adults Who Stutter. Perspect ASHA SIGs 7:1391-1404.
- Raghavan R, Camarata S, White K, Barbaresi W, Parish S, et al. (2018) Population health in pediatric speech and language disorders: Available data sources and a research agenda for the field. J Speech Lang Hear Res 61:1279-1291.
- Pruett DG, Shaw DM, Chen HH, Petty LE, Polikowsky HG, et al. (2021) Identifying developmental stuttering and associated comorbidities in electronic health records and creating a phenome risk classifier. J Fluency Disord 68:105847.
- Visser SN, Danielson ML, Bitsko RH, Holbrook JR, Kogan MD et al. (2014) Trends in the parent-report of health care provider-diagnosed and medicated attention-deficit/hyperactivity disorder: United States, 2003–2011. J Am Acad Child Adolesc Psychiatry 53:34-46.
- Gerlach H, Totty E, Subramanian A, Zebrowski P (2018) Stuttering and labor market outcomes in the United States. J Speech Lang Hear Res 61:1649-1663.
- Rees DI, Sabia JJ (2014) The kid's speech: The effect of stuttering on human capital acquisition. Econ Educ Rev 38:76-88.
- Rima D, Malikova S, Aratuly K, Bazilova A, Beaver KM (2021) Examining the Association between Stuttering and Psychopathic Personality Traits, Nonviolent Crime, and Violent Crime. J Aggress Maltreat Trauma 30:193-206.
- Jacobs MM, Merlo S, Briley PM (2021) Sleep duration, insomnia, and stuttering: The relationship in adolescents and young adults. J Commun Disord 91:6106.
- Polikowsky HG, Shaw DM, Petty LE, Chen HH, Pruett DG, et al. (2022) Population-based genetic effects for developmental stuttering. HGG Adv 3:73.
- Bloodstein O (1995) A Handbook on Stuttering. 5th ed. Delmar Learning, New York.
- Johnson W (1959) The onset of stuttering: Research findings and implications. University of Minnesota Press.
- Freeman F (1999) Going out on a limb. Hypothesis regarding the nature and treatment of stuttering. Minnesota State University, Mankato.
- Comings DE, Wu S, Chiu C, Ring RH, Gade R, et al. (1996) Polygenic inheritance of Tourette syndrome, stuttering, attention deficit hyperactivity, conduct, and oppositional defiant disorder: The additive and subtractive effect of the three dopaminergic genes-DRD2, DβH, and DAT1. Am J Med Genet 67:264-288.
- Alm PA (2004) Stuttering and the basal ganglia circuits: A critical review of possible relations. J Commun Disord 37:325-369.
- Ratcliff-Baird B (2002) ADHD and stuttering: Similar EEG profiles suggest neurotherapy as an adjunct to traditional speech therapies. J Neurother 5:5-22.
- Piispala J, Kallio M, Bloigu R, Jansson-Verkasalo E (2016) Delayed N2 response in Go condition in a visual Go/Nogo ERP study in children who stutter. J Fluency Disord 48:16-26.
- Seeman P, Bzowej NH, Guan HC, Bergeron C, Becker LE, et al. (1987) Human brain dopamine receptors in children and aging adults. Synapse 1:399-404.
- Yairi E, Ambrose N (2013) Epidemiology of stuttering: 21st century advances. J Fluency Disord 38:66-87.
- Ribases M, Ramos-Quiroga JA, Herva SA, Sánchez-Mora C, Bosch R, et al. (2012) Candidate system analysis in ADHD: evaluation of nine genes involved in dopaminergic neurotransmission identifies association with DRD1. World J Biol Psychiatry 13:281-292.
- National Resource Center on ADHD-A Program of CHADD (2015) ADHD and Coexisting Disorder. CHADD
- Blomgren M (2010) Stuttering treatment for adults: an update on contemporary approaches. Semin Speech Lang 31:272-282.
- Craig A, Tran Y (2014) Trait and social anxiety in adults with chronic stuttering: Conclusions following meta-analysis. J Fluency Disord 40:35-43.
- Blumgart E, Tran Y, Craig A (2010) Social anxiety disorder in adults who stutter. Depress Anxiety 27:687-692.
- Mulcahy K, Hennessey N, Beilby J, Byrnes M (2008) Social anxiety and the severity and typography of stuttering in adolescents.J Fluency Disord 33:306-319.
- Iverach L, Jones M, McLellan LF, Lyneham HJ, Menzies RG, et al. (2016) Prevalence of anxiety disorders among children who stutter. J Fluency Disord 49:13-28.
- Iverach L, Rapee RM (2014) Social anxiety disorder and stuttering: Current status and future directions. J Fluency Disord 40:69-82.
- Guitar B (2019) Stuttering: An Integrated Approach to its Nature and Treatment. Wolters Kluwer.
- Langevin M, Packman A, Onslow M (2009) Peer responses to stuttering in the preschool setting.Am J Speech Lang Pathol 218:264-276.
- Tichenor S, Yaruss JS (2020) Repetitive negative thinking, temperament, and adverse impact in adults who stutter. Am J Speech Lang Pathol 29:201-215.
- Lau SR, Beilby JM, Byrnes ML, Hennessey NW (2012) Parenting styles and attachment in school-aged children who stutter. J Commun Disord 45:98-110.
- Lowe R, Helgadottir F, Menzies R, Heard R, O'Brian S, et al. (2017) Safety behaviors and stuttering. J Speech Lang Hear Res 60:1246-1253.
- Adriaensens S, Beyers W, Struyf E (2015) Impact of stuttering severity on adolescents’ domain-specific and general self-esteem through cognitive and emotional mediating processes. J Commun Disord 58:43-57.
- Iimura D, Miyamoto S (2022) The influence of stuttering and co-occurring disorders on job difficulties among adults who stutter. Speech Lang Hear 25:235-244.
- Iverach L, Jones M, Lowe R, O’Brian S, Menzies RG, et al. (2018) Comparison of adults who stutter with and without social anxiety disorder. J Fluency Disord 56:55-68.
- McAllister J (2016) Behavioural, emotional and social development of children who stutter.J Fluency Disord 50:23-32.
- Blood GW, Blood IM (2016) Long-term consequences of childhood bullying in adults who stutter: Social anxiety, fear of negative evaluation, self-esteem, and satisfaction with life. J Fluency Disord 50:72-84.
- Iverach L, Rapee RM, Wong QJ, Lowe R (2017) Maintenance of social anxiety in stuttering: a cognitive-behavioral model. Am J Speech Lang Pathol 26:540-556.
- Briley PM (2018) Issues in assessment of children who stutter: A survey of speech-language pathologists in the state of North Carolina. Clin Arch Commun Disord 3: 95-103.
- Menzies R, O’Brian S, Packman A, Jones M, Helgadóttir FD, et al. (2019) Supplementing stuttering treatment with online cognitive behavior therapy: An experimental trial. J Commun Disord 80:81-91.
- Menzies RG, Onslow M, Packman A, O’Brian S (2009) Cognitive behavior therapy for adults who stutter: A tutorial for speech-language pathologists. J Fluency Disord 34:187-200.
- Caughter S, Crofts V (2018) Nurturing a resilient mindset in school-aged children who stutter. Am J Speech Lang Pathol 27:111-123.
- Anxiety & Depression Association of America. (2022) What is Depression?
- Arroll B, Kendrick T (2018) Definition of Anxiety. Primary Care Mental Health 20:125-37.
- American Psychiatric Association (2022) What is Depression?
- Stein MB, Fuetsch M, Müller N, Höfler M, Lieb R, et al. (2001) Social anxiety disorder and the risk of depression: a prospective community study of adolescents and young adults. Arch Gen Psychiatry 58:251-256.
- Beilby JM, Byrnes ML, Yaruss JS (2012) Acceptance and commitment therapy for adults who stutter: Psychosocial adjustment and speech fluency. J Fluency Disord 37:289-299.
- Craig A (1998) Relapse following treatment for stuttering: A critical review and correlative data. J Fluency Disord 23:1-30.
- Helgadóttir FD, Menzies RG, Onslow M, Packman A, O’Brian S (2014) A standalone Internet cognitive behavior therapy treatment for social anxiety in adults who stutter: CBTpsych. J Fluency Disord 41:47-54.
- Menzies RG, O’Brian S, Onslow M, Packman A, St Clare T, et al. (2008) An experimental clinical trial of a cognitive-behavior therapy package for chronic stuttering. J Speech Lang Hear Res 51:1451-1464.
- Blood GW, Blood IM, Maloney K, Meyer C, Qualls CD (2007) Anxiety levels in adolescents who stutter. J Commun Disord 40:452-469.
- Boyle CA, Boulet S, Schieve LA, Cohen RA, Blumberg SJ, et al. (2011) Trends in the prevalence of developmental disabilities in US children, 1997-2008. Pediatrics 127:1034-1042.
- Proctor A, Yairi E, Duff MC, Zhang J (2008) Prevalence of stuttering in African American preschoolers. J Speech Lang Hear Res 64:839-853.
- Briley PM, Ellis C (2020) The influence of ethnicity and residence on presence of stuttering in children. J National Black Assoc Speech-Lang Hear 15:21-30.
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Citation: Jacobs M, Briley P (2023) Co-Occurring Conditions among Young Adults who Stutter. J Speech Pathol Ther 8: 181. DOI: 10.4175/2472-5005.1000181
Copyright: © 2023 Jacobs M, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Select your language of interest to view the total content in your interested language
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 2461
- [From(publication date): 0-2023 - Oct 01, 2025]
- Breakdown by view type
- HTML page views: 2137
- PDF downloads: 324