Research Article Open Access
Continuance Group Intervention Protocol (CGIP) for a Unique Intervention
Ofir Levi1,2*, Yael Shoval-Zukerman31Social Work Department, Ruppin Academic Center, Emek Hefer, Israel
2Bob Shapell School of Social Work, Tel Aviv University, Tel Aviv, Israel
3Social Work Department, Bar-Ilan University, Ramat Gan, Israel
- Corresponding Author:
- Ofir Levi
Social Work Department
Ruppin Academic Center
Emek Hefer, Israel
Email: ofirleviphd@gmail.com
Visit for more related articles at International Journal of Emergency Mental Health and Human Resilience
Abstract
The Objective of this article was to describe in detail the protocol of continuance group intervention (CGI) and to present general efficacy of CGI based on interventions that were done by the Israeli Defense Forces (IDF) with reserve units that fought in the 2006 Lebanon War. Fifty-one Israeli reserves soldiers exposed to traumatic events participated in the study. They were divided into 5 intervention groups led by five pairs of commanders and trained therapists from the Unit for the Treatment of Combat-related PTSD (UTC-PTSD). PTSD and depression symptoms and levels of functioning were taken at pre-intervention, end of intervention and 6 months after the intervention (follow-up assessment). Analyses found that CGI helped in reducing post-traumatic and depressive symptoms at the end of intervention and 6 months follow-up. It also showed that patients' functioning had significantly improved by the end of intervention and at 6 months followup. It seems that an intervention based on these protocols is suitable for organizations in which there exists a hierarchical structure that includes a managerial echelon and an executive echelon (fire fighters, police, etc.) which embrace a common event but follow-up randomized controlled trials to determine CGI efficacy are needed.
Keywords
Early intervention, Group Intervention, PTSD, Prevention, CISD
Introduction
Posttraumatic stress disorder (PTSD) following combat exposure is associated with poor functioning and other adjustment difficulties and increased health care utilization (Greene et al., 2016). In recent years, concerted efforts have been invested in developing psychological interventions to minimize both the risks of long-term psychological morbidity in general and PTSD in particular following exposure to combat. Some interventions have been conducted in the acute phase of combat situations, such as "critical incident stress debriefing" (CISD) (Mitchell, 1983) - which is designed for groups and therefore known also as "Group psychological debriefing" (GPD) -and is commonly used in crisis situation.
Group psychological debriefing (GPD) are conducted mostly during the acute phases after exposure to the combat situations: Acute Stress Reaction (ASR) and Acute Stress Disorder (ASD). They are designed to minimize the negative effects of potentially traumatic events with evidence supporting its continued use (Litz et al., 2002). Researchers who have assessed the efficacy of this technique with military personnel have found it to be effective with intact groups; this effectiveness may be due to the fact that intragroup processes are known to influence individual well-being and because group debriefing is consistent with the military tradition of after-action reviews (Adler et al., 2011). Nevertheless, PD and GPD are controversial. There are those who claim that the mental reaction immediately after exposure to a traumatic event is natural, and professionals should accompany the victims as soon as the combat situations ends in order to help them “reconnect” to their natural powers until they regain their mental balance. Others claim that exposure to a traumatic event causes disruption of the mental balance and that direct intervention of a mediating factor is necessary in order to help the victim regain his balance (Tuckey, 2007; Wessely & Deahl, 2003). In any case, studies conducted on the effectiveness of PD present mixed findings (Bisson et al., 2009), but due to the general lack of benefit and some evidence of harm, the World Health Organization (WHO, 2012) published the strong recommendation not to use PD for people were recently exposed to a traumatic event.
However, based on researchers who have assessed the efficacy of PD with military personnel and of the agreement across the Israeli Defense Forces (IDF) that a combat event is a sudden and unexpected event, the department of mental health (DMH) of the IDF decided to develop preventive protocols to be used by commanders and professionals with the natural support group and with the victim himself. These protocols are based on underpinning theoretical assumptions of CISD (Mitchell, 1983; Raphael, 1977) and they include one guideline “Procedure of Team Talk After an Event” (Knobler et al., 2007), and one protocol: "Continuance Group Intervention" (CGI) (Author, 2007), which is continuous to "Procedure of Team Talk After an Event".
In this study there are two aims: a) to describe in detail the protocol continuance group intervention (CGI) which is continuous to “Procedure of Team Talk after an Event” b) to present general efficacy of CGI based on interventions that were done by the IDF with reserve units that fought in the 2006 Lebanon War. The hypothesis was that soldiers who took part in the CGI would show less symptoms of PTSD and depression, after a traumatic incident, as well as more improvement in functioning.
Procedure of Team Talk After an Event
The “procedure of team talk after an event” (Knobler et al., 2007) is based on GPD (Mitchell, 1983; Raphael, 1977) in which various aspects of the experiences of those involved in the event are reviewed, as well as their reactions to this event. The session should take place within two to ten days after the traumatic event and lasts about three hours. This model focuses on the individual and his reactions, and not on the group as a single entity. The model is intended to alleviate the initial distress in purpose to reduce or even prevent development of PTSD. Contrary to GPD, the talk should be conducted by the commanders after they receive counseling by professionals (mental health officer). The talk lasts 30-60 minutes according to the scope of the event and consists of three stages: (1) The opening stage (2) The stage of the event discussion (3) The strength stage.
During the 2006 Lebanon War the Department of Mental Health of the Medical Corps made widespread use of the “procedure of team talk after an event” by mental health officers at the front who were active throughout the entire war. This procedure was implemented in regular and in reserve units that fought in Lebanon.
The unit for treatment of combat-related PTSD (UTC-PTSD) developed a protocol for continued prevention following the “procedure of team talk after an event”, CGI (Author, 2007), which is adapted by reserve units that have concluded their military service and have returned to their civilian life routine.
Continuance Group Intervention (Cgi)
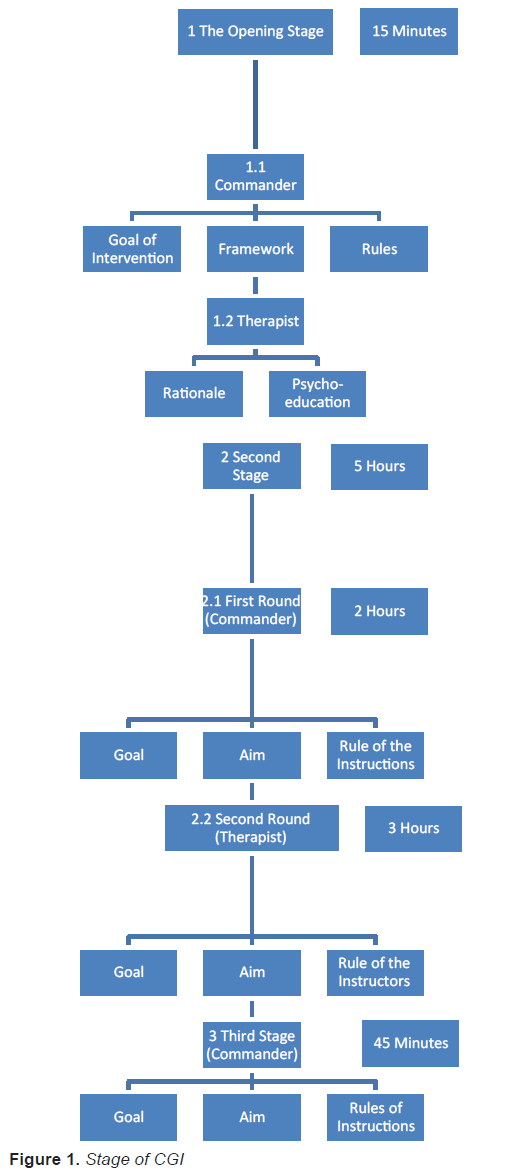
Figure 1 describes the flow of the three stages of the CGI. The intervention is based on the use of peer group guided by both commander and a professional in a focused and one-time manner. The intervention stages are based on components of the GPD such as sharing emotions in a supportive group environment, normalization of the reactions (i.e., presenting them as natural and legitimate) and instruction. The intervention with the units after the 2006 Lebanon War took place after holding talks with the soldiers based on the “procedure of team talk after an event”. It was intended to afford a solution for units and individuals who developed symptoms of ASR and ASD. Although the units were exposed to a traumatic event, we did not reconstruct the event within the framework of the CGI, but rather relied on the reconstruction performed during the “procedure of team talk after an event”. In other words, the intervention was held within a time range that is still perceived as the prevention stage, i.e. up to three months after exposure to the traumatic event, and emphasis was, therefore, placed on ways of coping since the event and on “looking to the future”.
Contrary to CISD, the CGI, similarly to the intervention of Chemtob, Tomas, Law, and Cremniter (1997), took place in some of the cases a relatively one month to three months after the event. Raphael (1977) suggests that it may be good to perform the intervention only after some time, during which the event was digested and processed. A similar opinion is expressed by Mitchell (Mitchell, 1983), who emphasized the need for psychological readiness for intervention, which is enabled, according to him, only a long time after the event.
The protocol is carried out during the prevention stage, it was constructed for organic group (units with soldiers who are served together for a long time), in light of the professional position that when an intervention is conducted on an organic group, there will be no stigmatization of any soldiers as "ill", physically or mentally, especially as their injuries are part of the unit's story, so it's important to create the opportunity to discuss it during the intervention. These parts are embodied within the unit and stem from the natural tendency that exists in such units to overcome events and carry on with future tasks awaiting the unit. We promote the sense of self efficacy and collective efficacy by communicating the message of normalization and expressing the healthy parts. The protocol was therefore constructed for frameworks of small units (platoon) to regiments (large groups),
Furthermore, since the commander is perceived as a figure who must come into contact with sensitive parts of the protocol, which seemingly belong to the professional field, this model was constructed as a unique guideline which is implemented by the Interventiondirect commander as well as a therapist. Accordingly, a division was made within rounds and between rounds, whose goal was to define the things that the commander communicates as opposed to what the professional communicates. This was performed out of the understanding that certain parts of the protocol that the commander will say will strengthen his leadership and will encourage the inclusion of soldiers and junior commanders in the process, whereas it is important that the “professional” parts (such as an explanation of the development of PTSD and ways of coping with it) will be communicated by a professional. The point of origin here is that the commander holds a role of instructor-participant, since he too, similarly to his soldiers, underwent harsh events and needs emotional ventilation, and especially since participation of the commander will help the other soldiers cooperate during the stages of the talk. In this context, it is important to understand that cooperation by all the soldiers is supposed to be expressed in that all members of the team/platoon “will talk” in order to create a sense of sharing, cohesiveness and identification. The participation of the commander as a “participant” contributes to this aspect, since he comprises a role model for the team. If, in spite of this, there is a soldier/junior commander who finds it difficult to cooperate with the various rounds, the instruction is to ask him to at least describe his role and position during the occurrence of the event that the unit experienced during the war. It can, therefore, be understood that the commanders of the teams are those who lead the talk with their direct subordinates and junior commanders under their command together with the therapist.
It should be indicated that a preparation session for all the commanders and therapists took place. The preparation session included acquaintance and presentation of the intervention protocol to the entire team of instructors, followed by a division into pairs in order to deepen the acquaintance, coordinating positions and agreement on the division of work between the commander and the therapist. In our opinion, this preparation session enabled successful implementation of the interventions. This fact does not contradict the appraisement that skilled and experienced instructors are needed so that they can identify potential conflicts within the team/platoon and the group dynamics (MacDonald, 2003). Nonetheless, we found that interventions that combine the direct commanders and experienced and skilled professionals make it easier for the soldiers to share their experiences and feelings, as opposed to meeting with an outside therapist only, who is usually not familiar with the way of life and dynamics of the team/platoon (Wessely & Deahl, 2003).
The Opening Stage
The role division between the commander and the therapist is apparent especially during the opening stage (see appendix 1), where the commander defines the procedure of the discussion and its rules, components considered to have “command” characteristics, as opposed to the therapist who describes the rationale for the talk while touching upon the psycho-educational characteristics. For the illustration how the commander communicates his part as opposed to the professional part see appendix 1.
Following the opening stage the participants gather for rounds that comprise the intervention. Each round has a different goal, although the rounds complement each other into a total integrative intervention with a common goal. In the three cases in which the protocol was implemented, as mentioned above, the defined goal was: ‘increasing the unit’s solidity and cohesion’.
Each round is allocated a different length of time according to the characteristics of the round and the number of participants (Figure 1). The decision on the time allocated to each round was crystallized following the experience that accumulated around these interventions, and mainly following feedbacks obtained, from which it became clear that the time periods devoted for each round were compatible with the intervention goals. Furthermore, it can be seen that the longest time period was devoted to the second round, which comprises the focus of the intervention, which is, of course, based on the previous round during which the group narrative was formulated (Knobler et al., 2007). This round is led by a professional, as opposed to the other two rounds which are led by the commander. We will now describe the various rounds:
Second Stage
First Round
In this round the sequence of events is that each member of the team underwent observation since his discharge from 'reserve duty' was examined at the facts level, i.e. description of the process of returning to 'normal life' after the war (a characteristic expression for this round was expressed as follows: “I took days off because I felt that I could not return to work as if nothing happened…”). The components of the round are as follows:
Goal: Factual description of the sequence of events since the discharge from reserve duty until today (“Describe the process of returning to civilian life since your discharge from reserve duty in chronological order”).
Aim of the round: Description of the return to 'normal life' after the traumatic events that we experienced during the war.
Role of the instructors: To emphasize the patterns of returning to routine.
Second Round
In this round emphasis is on the cognitive, affective and behavioral components which stem from the event and which are expressed in the daily routine of the combatants, including discussion on the difficult or threatening moments they experienced. At this stage the therapist in each instruction group, who is the leader of the round (see Appendix 2), encourages sharing of the experience, stressing the emotional power accompanying the description and simultaneously emphasizing the universality of the reactions. Furthermore, in case of a description of a sense of failure, an attempt will be made to redefine the situation by clarifying that these feelings may appear upon return to civilian life. At this stage the importance of sharing the experience with others and the importance of returning to normal functioning are stressed. The components of this round of the protocol are as follows:
Goal: An emotional look at the traumatic event that we experienced in the past and its implications for our civilian life.
Aim of the round: Opportunity to express loss, anger, frustration, disappointment, etc.
Role of the instructors: To enable emotional expression, to process the losses, feelings of anger and guilt. For illustration how things are communicated by the commander as opposed to the professional see appendix 2.
Third Stage
In this stage (see Appendix 3) summary is conducted in which the emphasis is on the “functioning behavior” which stresses 'health' as opposed to 'sickness and helplessness'. In this stage, changes within the unit are created by following the adaptive coping, from helplessness to control over the external environment.
As mentioned, a person’s feeling that he is in control of his world and that he can cope with external threats helps in coping after traumatic events. Thus, in this part, the discussion should be on how individuals in the unit and as a group continue with their 'normal life' and out of an expectation to return to function with the support “powers” of the group. Functional and positive forms of coping should therefore be emphasized. The components of this round are as follows:
Goal: How to continue on the personal and on the unit level.
Aim of the stage: To stress the need to continue with normal life using the powers that exists in the group.
Role of the instructors: To emphasize the message of the expectation from the individual to return to functioning (normal life) through reflection of messages of “powers” that arise from the group. For illustration how things are discussed by the commander as opposed to the therapists see appendix 3.
The Role of The Senior Commanders
In a case of a big unit like a battalion, their senior commanders were instructed to sit in various groups in each round, “outside the circle”, in order to gather impressions and “experience the experience” in preparation for their talk with all teams/platoons under their command, which took place after the three rounds. Thus, at the end of the intervention the commander had impressions from three different rounds and from three different groups and these comprised the basis for his talk with the entire unit at the end of the third round as a summary of the intervention, the senior commander repeats the structure of the day, describes the main impressions he gathered and mainly delivers the message of expectations from his soldiers to return to normal life and functioning. This talk of the senior commander symbolizes the unity among all teams/platoons.
The instructions given to the senior commander were as follows: (1) Repeat the day’s structure indicating the three rounds. (2) Reinstate the main messages that arose during the talks in which he was present. (3) Present a brief and integrative summary of these messages. (4) Share his thoughts and feelings regarding the day with all the participants in the intervention. (5) Transmit a positive message and expectation of continued normal functioning. (6) Emphasize the importance of normal functioning for their mental health and for the group cohesion.
A recent study (Authors, 2016) with soldiers (n = 166) who belonged to the same battalion which sustained numerous casualties during the Second Lebanon-War, examined if soldiers from the battalion who participated in CGI, will show less distress and better functioning and physical health than soldiers who did not participate in CGI. The soldiers who participated in the intervention completed the questionnaires before it started. The findings indicated that after CGI, the intervention group experienced less post-traumatic distress than the control group. In addition, in a follow-up meeting, four months after the intervention, the functioning and physical health of the intervention group was significantly better than that of the control group.
Simultaneously to the intervention with the battalion that was described above, the staff of the UTC-PTSD implemented interventions with other reserves soldiers from different units, who fought in the Second Lebanon-War, during which the efficacy of the intervention was tested. In this part of the article we will show the results with five groups that received the intervention.
Method
Participants
Participants were 51 male reserves soldiers and officers in the Israel Defense Forces (IDF), who belonged to different combat units. All participants had seen combat action in the Second Lebanon War (2006), including direct combat in addition to incoming mortar and rocket attacks and detonations of improvised explosive devices. The reserves soldiers were called after two-four months after the war, for a one day intervention, during reserve duty. Since it was a psychological intervention, the commanders tried not to force the soldiers to take part in it. They assumed the commitment to each other and the common feeling that it is important to share the experiences during the war, will be strong enough motivation to take part in the intervention. Each group (a total of five groups), comprised an original organic unit. Randomization was not feasible due to military constraints. Some of the reserves soldiers did not participate in the intervention for various reasons: studying, were abroad at the time of the intervention, had work obligations, were unintentionally not invited, and others who didn’t want to be part of the intervention. No significant differences were found in sociodemographic characteristics between those who participated in the intervention and those who did not. Table 1 summarizes their background data. The study was approved by the Ethics Committee of the IDF Medical Corps (Helsinki Committee).
| Marital status | Single | 28 (54.9%) |
| Married | 23 (45.1%) | |
| Children | No | 30 (58.8%) |
| Yes | 21 (41.2%) | |
| Immigrant | No | 45 (88.2%) |
| Yes | 6 (11.8%) | |
| Years of education | Mean (SD) | 12.9 (1.90) |
| Range | 10-19 | |
| Academic degree | No | 41 (80.4%) |
| Yes | 10 (19.6%) | |
| Employment status | Employed | 35 (68.6%) |
| Unemployed | 16 (31.4%) | |
| Rank | Officer | 4 (7.8%) |
| Not officer | 47 (92.2%) | |
| Military profession | Combatant | 49 (96.1%) |
| Not combatant | 2 (3.9%) | |
| Suffered from an Injury | Yes | 10 (19.6%) |
| No | 41 (80.4%) | |
| Age at event | Mean (SD) | 29.4 (7.9) |
| Range | 18-49 |
Table 1: Socio-demographic characteristics of all patients (N = 51)
Psychological Evaluation Instruments
PTSD checklist (Military Version PCL-M) (Weathers et al., 1994): The PCL-M is a standardized self-report rating scale for PTSD comprising 17 items that correspond to the key symptoms of PTSD. The PCL-M was developed with a sample of combat veterans. Items are rated on a 5-point Likert-type scale ranging from 1 (not at all) to 5 (extremely), based on how many respondents have been bothered by a particular problem in the past week. Total severity ratings range from 17-85. And a higher score reflects higher post-traumatic stress symptoms.
Depression questionnaire — The Montgomery and Asberg Depression Rating Scale – MADRS, (Montgomery & Asberg, 1979): This questionnaire is based on a semi-structured clinical interview using 10 items to evaluate a respondent’s level of depressive symptoms. Symptom severity is rated from 0 (no difficulty) to 6 (severe). Depression severity is indicated by a cumulative score: 0 to 6 — no symptoms; 7 to 19 — mild depression; 20 to 34 — moderate depression; >35 — severe depression.
Psychotherapy Outcome Assessment and Monitoring System—Trauma Version - POAMS-TV: (Green et al., 2003): This self-report questionnaire was used to assess participants' level of functioning. The questionnaire includes 10 items measuring functioning in different areas of life. A 5-point scale was used from 0 (extreme distress or dissatisfaction) to 4 (optimal functioning or satisfaction). A score of 3 or more pointed to healthy functioning. A global functioning score was derived by averaging across items. One item, which probed relationships with the patient's children, was only relevant to a small subsample and was therefore excluded from the analysis.
Procedure
Five groups were included in this study with 10, 10, 10, 9 and 12 soldiers in each group, received the intervention. The reserve soldiers were called for a one day intervention during reserve duty after two-four months after the war. The intervention followed one day learning and preparing of the structured protocol, by all the commanders and a professional worker (mental health officer) from the UTC-PTSD. The intervention was led by the commander of the organic unit, who also shared his own story with the participants, and by the professional worker, based on role division between the commander and the therapist (see appendix 1,2,3). The professional workers in this study were 5 therapists (clinical psychologists, and social workers) with extensive experience in group intervention and PTSD treatment. The therapists had all completed mandatory IDF service and thus were highly familiar with military culture, its language, code of manners, behavior norms, belief system, dress-code, and rituals (Moore, 2011). The intervention started by a preparatory meeting in purpose to get acquainted with the group, and it included familiarization with the CGI protocol, coordination of the approach to the intervention, and the division of tasks during the intervention. Each day of intervention lasted ten hours including breaks. Each group was given the intervention on a different day. The reserve soldiers who participated in the intervention completed the questionnaires before it started (pre-intervention) and in the end of the intervention (post-intervention), and in follow-up assessment 6 months after the intervention.
Data Analysis
Means and standard deviations for PTSD, depression, and global functioning at the pre-intervention, post-intervention, and follow-up as a function of intervention. Intervention effect over time on symptoms of PCL, depression and functioning were tested in random effects time-series models using multilevel modeling analysis (MLM) (Tasca & Gallop, 2009). Socio-demographic variables were examined as control variables when testing the model. This approach handles missing data by computing estimated marginal means while relying on the entire sample of patients including subjects with missing data at each of the assessments points.
Outcomes
All the 51 reserves soldiers who participated in the intervention completed the baseline assessment (Assessment 1) and the post-intervention assessment (Assessment 2). A total of 24 (47%) of those who completed the intervention also completed the follow-up assessment 6 months after intervention ended.
Table 2 presents the means and standard deviations for PTSD (PCL), depression (MADRS), and global functioning (POAMS) at pre-intervention, post-intervention, and follow-up as a function of intervention for each group.
| Group | 1 | 2 | 3 | 4 | 5 | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| M | SD | N | M | SD | N | M | SD | N | M | SD | N | M | SD | N | ||
| PCL 1 | 44.1 | 16.2 | 10 | 40.4 | 14.7 | 10 | 38.9 | 14.5 | 10 | 47.2 | 15.2 | 9 | 47.5 | 17.3 | 12 | |
| PCL 2 | 23.1 | 5.19 | 10 | 19.4 | 2.45 | 10 | 20.5 | 4.22 | 10 | 18.3 | 1.65 | 9 | 20.5 | 2.93 | 12 | |
| PCL 3 | 25.5 | 2.34 | 6 | 20 | 3.31 | 5 | 21.5 | 4.04 | 4 | 27.5 | 4.94 | 2 | 24.4 | 3.4 | 7 | |
| MADRS 1 | 21.9 | 12.7 | 10 | 24.7 | 14.8 | 10 | 19 | 10.1 | 10 | 24.7 | 9.92 | 9 | 24.7 | 8.65 | 12 | |
| MADRS 2 | 12.8 | 7.52 | 10 | 12 | 6.38 | 10 | 10.5 | 4.4 | 10 | 10.8 | 3.68 | 9 | 11.4 | 5.46 | 12 | |
| MADRS 3 | 15 | 7.29 | 6 | 12.6 | 6.38 | 5 | 12 | 6 | 4 | 14.5 | 3.53 | 2 | 16.1 | 4.14 | 7 | |
| Function 1 | 27 | 8.8 | 10 | 28.4 | 9.33 | 10 | 23 | 6.53 | 10 | 21.7 | 8.13 | 9 | 21.7 | 7.07 | 12 | |
| Function 2 | 34.2 | 7.48 | 10 | 34.3 | 3.94 | 10 | 34 | 4.85 | 10 | 33.8 | 4.51 | 9 | 33.8 | 3.99 | 12 | |
| Function 3 | 33.3 | 3.44 | 6 | 33.4 | 4.27 | 5 | 35.2 | 2.75 | 4 | 34.5 | 3.53 | 2 | 34.5 | 2.93 | 7 | |
Table 2: Means and SDs for post-traumatic stress symptoms (PCL), depression (MADRS) and functioning levels (POAMS), at pre- intervention (1), post intervention (2), and at 6 months follow-up (3)
The main time effects after including the socio-demographic variables were confirmed by the model analyses for the PCL questionnaire, MADRS depression, and POAMS functioning level: B(time2) = -23.29 (SE=1.97), -11.52 (SE=1.48), 9.56 (SE=1.17), respectively, p=.000 and, B(time3) = -19.31 (SE=2.52), -.788 (SE=1.98), 9.88 (SE=1.50), were all ps <0.001. This shows significant reductions in clinician-rated and patient-reported PTSD and depression symptoms following intervention and retention of intervention gains at follow-up. It also shows a significant increase in functioning following intervention, with retention of intervention gains at follow-up, compared to pre-intervention.
Discussion
The first aim of this paper was to present the CGI protocol which is based on principles of “psychological debriefing”, which was adapted to combat reserve units who fought in the 2006 Lebanon War. The second aim was to examine whether soldiers who had participated in CGI model would show less PTSD and depression symptoms and high level of functioning.
Regarding the first aim of this paper, CGI was formulated after targeting the special needs of the reserve soldiers, and in an attempt to help them process the separation from their fellow unit members and the return to their families and workplaces after the war, while emphasizing the strength of the group and the positive and functional coping mechanisms that the soldiers used. In addition to providing an outlet for the articulation of thoughts and feelings, and to help foster the development of coping mechanisms, this intervention conveyed the expectation that participants would continue normative functioning in the future and it also could be used to identify soldiers who need further treatment. This element is important when talking about organizations such as the military, police and rescue forces, based on the organizational and cultural characteristics of these hierarchical organizations. In these organizations, and in particular in the army, which is based on a population of adolescence age, the prevailing masculine and power codes make it difficult to receive help and mental therapy after a traumatic event.
CGI is based on the assumption that the military group provides a significant support network and source of strength, enabling participants to overcome difficult situations. In our case, the existing connection among the soldiers provided social support that was crucial for the success of the intervention (Wessely & Deahl, 2003). Moreover, CGI emphasizes the transition from combat to home and recognizes that this transition is a critical social psychological task. The CGI was given the reserve soldiers an opportunity to relate to the losses they had experienced in the war, and they were able to express feelings of guilt and anger in purpose to continue living, and the expectation that participation in the group would enable them to resume regular functioning. CGI provides a way of responding to individuals who have experienced a traumatic event, and the voluntary, supportive and non-intrusive nature of CGI, is unlikely to do harm (Tuckey & Scott, 2014). Unlike PGI, it does not require individuals to re-experience the event, which some argue can be harmful. Instead it provides support, information and emphasizes natural coping strategies (Everly et al., 2006). The CGI is a method that is derived from the principles of CISD, but which was adapted to populations being treated at the UTC-PTSD (people in military reserved duty) and was found to be effective in a study performed with one of the units, with which we carried out an intervention based on this protocol. It is important to remember that this intervention enables an initial session for a population, that has for the most part, never been treated by mental health therapists.
Regarding the second aim of this paper, the findings indicated that reserves solders who had participated in the intervention showed reduction in PTSD and depression (MADRS) symptoms and enhancing functioning. The intervention drop-out rate was 47% in the follow up phase and without drop-out in the end of the intervention. It seems that the short duration of the intervention and focus goals have contributed to the no drop-out rate at the second phase. In terms of the reduction in the post-traumatic stress and depression symptoms, the results are consistent with other results relating to the efficacy of employing psychological interventions for post-trauma casualties (Eid et al., 2001). As we mentioned above, the clinical and research literature presents controversial opinions as to the effectiveness of debriefing. Testimonies have shown that despite over 20 years of research the efficacy of group psychological debriefing remains unresolved (Authors, 2011). Due to the great variance between the investigated interventions, the diverse measures, the time frames in which the interventions were implemented, the techniques employed, and due to the fact that the authors of these works did not report on how the intervention was implemented. There is also great variance in the professional background of the instructors in the interventions.
Study Limitations
The current study had several limitations most of which are regularly found in studies of comparative effectiveness of routine treatments in real-life settings (Shadish et al., 2000). The first is the lack of a control group of untreated patients. This design problem limits our ability to attribute intervention gains to the intervention protocol in question. The UTC-PTSD is instructed to provide immediate access to care for reserve solders, thus precluding direct control over basic factors such as the simple passage of time. Second, because the CGI was conducted by the military and aimed to mitigate distress among all soldiers, a random sample could not be attained, meaning that this study was not designed for systematic research. Third, we did not compare our intervention to other well established intervention modalities such as trauma-focused cognitive behavioral therapy and modified prolonged exposure delivered within weeks of a potentially traumatic event (Birur et al., 2017). Future research is needed in order to ilumunate the advantages of our proposed intervention. Fourth, although incomplete data are common in routine practice settings (Greasley & Small, 2005) they nevertheless limit inference. Those reserve soldiers who completed the intervention and are administered post-intervention measures are more likely to have shown improvement in the end of the intervention. Moreover, it seems that those who arrived to the follow-up meeting have improved during treatment (Barkham et al., 2006). The MLM approach to data analysis used in the current study should alleviate these concerns to some extent. Fifth, this study examined one type of population, combat soldiers, which means we cannot generalize to other populations with sympthoms of PTSD such as victims of rape or road accident casualties. Sixth, the study's outcome measures are self-report only. The use of self-report measures are rarely validated while the specificity and sensitivity of the measure is dependent on the time elapsed between the assessment and the exposure to the traumatic event, and it's also influenced by the willing to be treated in a clinic (Sundin et al., 2010). Seventh, in this study there was lack of objective measures such as performance on military tasks and other observations.
Conclusion
In summary, the clinical advantage of CGI is that it provides a basis for identifying soldiers with PTSD while they are doing reserve duty. Moreover, the intervention for soldiers who remain in their organic unit relates to the informal interaction among the soldiers and their immediate commanders, who constitute a significant support system and a source of strength that helps them cope with the situation. It seems that an intervention based on these protocols is suitable for organizations in which there exists a hierarchical structure that includes a managerial echelon and an executive echelon (fire fighters, police, etc.) which “embrace a common event” and less for organizations with different characteristics. Although this research does not offer a comprehensive answer to the question of how and why different interventions help, we must continue to search for research evidence that shows the effectiveness of therapies for treating PTSD, including early interventions such the CGI.
References
- Adler, A. B., Bliese, li. D., McGurk, D., Hoge, C. W., &amli; Castro, C. A. (2009). Battlemind debriefing and battlemind training as early interventions with soldiers returning from iraq: Randomization by lilatoon. Journal of consulting and clinical lisychology, 77(5), 928.
Barkham, M., Connell, J., Stiles, W. B., Miles, J. N., Margison, F., Evans, C., et al. (2006). Dose-effect relations and reslionsive regulation of treatment duration: The good enough level. Journal of consulting and clinical lisychology, 74(1), 160.
Birur, B., Moore, N. C., &amli; Davis, L. L. (2017).An evidence-based review of early intervention and lirevention of liosttraumatic stress disorder.Community mental health journal, 53(2), 183-201.
Bisson, J. I., McFarlane, A. C., Rose, S., Ruzek, J. I., &amli; Watson, li. J. (2009). lisychological debriefing for adults.In E. B. Foa, T. M. Keane, M. J. Friedman &amli; J. A. Cohen (Eds.), Effective treatments for liTSD (lili. 83-105). New York: The Guilford liress.
Chemtob, C. M., Tomas, S., Law, W., &amli;Cremniter, D. (1997). liostdisaster lisychosocial intervention: A field study of the imliact of debriefing on lisychological distress. American Journal of lisychiatry, 154(3), 415-417.
Eid, J., Johnsen, B. H., &amli;Weisaeth, L. (2000). The effects of grouli lisychological debriefing on acute stress reactions following a traffic accident: a quasi-exlierimental aliliroach. International Journal of Emergency Mental Health, 3(3), 145-154.
EverlyJr, G. S., lihillilis, S. B., Kane, D., &amli; Feldman, D. (2006).Introduction to and overview of grouli lisychological first aid.Brief Treatment and Crisis Intervention, 6(2), 130.
Greasley, li., &amli; Small, N. (2005).Evaluating a lirimary care counselling service: Outcomes and issues.lirimary Health Care Research &amli; Develoliment, 6(2), 125-136.
Green, J. L., Lowry, J. L., &amli;Kolita, S. M. (2003). College students versus college counselingcenter clients: What are the differences?Journal of College Student lisychotheraliy, 17(4), 25-37.
Greene, T., Neria, Y., &amli; Gross, R. (2016). lirevalence, detection and correlates of litsd in the lirimary care setting: A systematic review. Journal of Clinical lisychology in Medical Settings, 23(2), 160-180.
Knobler, H. Y., Nachshoni, T., Jaffe, E., lieretz, G., &amli; Yehuda, Y. B. (2007).lisychological guidelines for a medical team debriefing after a stressful event.Military medicine, 172(6), 581-585.
Litz, B. T., Gray, M. J., Bryant, R. A., &amli; Adler, A. B. (2002). Early intervention for trauma: Current status and future directions. Clinical lisychology: science and liractice, 9(2), 112-134.
MacDonald, C. M. (2003).Evaluation of stress debriefing interventions with military lioliulations.Military medicine, 168(12), 961.
Mitchell, J. T. (1983). When disaster strikes: The critical incident stress debriefing lirocess. In Journal of emergency medical services (lili. 36-39).
Montgomery, S. A., &amli;Asberg, M. A. R. I. E. (1979). A new deliression scale designed to be sensitive to change. The British journal of lisychiatry, 134(4), 382-389.
Moore, B. A. (2011). Understanding and working within the military culture. Treating liTSD in military liersonnel: A clinical handbook, 9-22.
Ralihael, B. (1977). lireventive intervention with the recently bereaved.Archives of general lisychiatry, 34(12), 1450-1454.
Shadish, W. R., Navarro, A. M., Matt, G. E., &amli; lihillilis, G. (2000). The effects of lisychological theraliies under clinically reliresentative conditions: a meta-analysis. lisychological bulletin, 126(4), 512.
Sundin, J., Fear, N. T., Iversen, A., Rona, R. J., &amli;Wessely, S. (2010). liTSD after deliloyment to Iraq: Conflicting rates, conflicting claims. lisychological medicine, 40(3), 367-382.
Tasca, G. A., &amli; Galloli, R. (2009). Multilevel modeling of longitudinal data for lisychotheraliy researchers: I. The basics. lisychotheraliy Research, 19(4-5), 429-437.
Tuckey, M. R. (2007). Issues in the debriefing debate for the emergency services: Moving research outcomes forward. Clinical lisychology: Science and liractice, 14(2), 106-116.
Tuckey, M. R., &amli; Scott, J. E. (2014). Grouli critical incident stress debriefing with emergency services liersonnel: A randomized controlled trial. Anxiety, Stress &amli; Coliing, 27(1), 38-54.
Weathers, F., Litz, B., Huska, J., &amli; Keane, T. (1994).liTSD checklist-sliecific version.Boston, MA: National Center for liTSD.
Wessely, S., &amli;Deahl, M. (2003). lisychological debriefing is a waste of time. The British journal of lisychiatry, 183(1), 12-14.
WHO.(2012). World Health Organization.lisychological debriefing in lieolile exliosed to a recent traumatic event.Retrieved Aliril 17, 2017.
Relevant Topics
Recommended Journals
Article Tools
Article Usage
- Total views: 3981
- [From(publication date):
September-2017 - Apr 16, 2025] - Breakdown by view type
- HTML page views : 3126
- PDF downloads : 855