Research Article Open Access
Considering Mindfulness Training for Obesity-Related Eating Behaviors in Children and Adolescents: A Conceptual Review
Gillian A O’Reilly* and David S Black
Department of Preventive Medicine, Keck School of Medicine, University of Southern California, USA
- *Corresponding Author:
- Gillian A O’Reilly
Department of Preventive Medicine
Keck School of Medicine
University of Southern California
Tel: 949-463-4007
E-mail: goreilly@usc.edu
Received Date: April 17, 2015; Accepted Date: May 08, 2015; Published Date: May 15, 2015
Citation: O’Reilly GA, Black DS (2015) Considering Mindfulness Training for Obesity-Related Eating Behaviors in Children and Adolescents: A Conceptual Review. J Child Adolesc Behav 3:207. doi:10.4172/2375-4494.1000207
Copyright: © 2015 O’Reilly GA et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Child and Adolescent Behavior
Abstract
Obesity in children and adolescents is a major public health problem in the United States. Obesity-related eating behaviors are an important contributing factor to this issue. Youth in the United Stated tend to have unhealthful dietary intake and poor eating habits, such as consumption of large portion sizes, fruit, vegetable, and dietary fiber intake below dietary recommendations, and sugar intake above dietary recommendations. Emotional eating, external eating, and binge eating, behaviors that are linked with excess weight gain, have also been found to occur in youth. Eating behaviors established during the early years of life tend to persist into adulthood, so forming healthful eating habits and relationships with food early in life are important for the current and future health of children and adolescents. However, numerous factors including parenting practices, the food environment at home and outside of the home, and food advertising impart competing influences on eating behaviors in youth. It is essential to arm children and adolescents with skills that help them make healthful dietary choices and develop healthful eating styles in the face of influences that may impede healthful behaviors. Mindfulness training may be a promising approach. A recent systematic literature review by our research group found that mindfulness training programs can improve obesity-related eating behaviors in adults. Research has also shown that mindfulness training can be successfully implemented in child and adolescent populations with promise for improving stress-related and neurocognitive outcomes. The aim of this brief conceptual review is to provide an overview of obesity-related eating behaviors in children and adolescents and suggest how mindfulness training might hold promise as an intervention approach and a way of being to support healthful eating behaviors in the early years of human development.
Keywords
Mindfulness; Attention training; Obesity; Children; Adolescents; Review
Introduction
Obesity-related eating behaviors are a significant public health concern for youth in the United States and worldwide. There are a variety of problematic eating behaviors that lead to excess weight gain in children and adolescents. One of the most important of these is poor dietary intake. Overall, daily total energy intake by children and adolescents has increased in the past 30 years by as much as 150 to 300 calories per day [1]. This can be attributed at least partly to an increase in portion sizes [2] and a shift in dietary patterns away from consumption of low-calorie, nutrient-rich foods toward energy-dense, nutrient-poor foods [3]. Youth aged 2 years and older should consume balanced diets that consist predominantly of low-calorie, nutrientdense foods such as fruits, vegetables, and high-fiber whole grains [3]. However, most youth do not meet dietary recommendations [4]. Several studies have demonstrated that the majority of children and adolescents in the U.S. and other countries have inadequate intake of fruits and vegetables [5-9]. Evidence also shows that typical fiber intake by children and adolescents does not meet recommendations. In a recent study of a nationally representative sample of American youth, more than 60% had average daily fiber consumption that was less than the recommended amount [10]. These types of dietary patterns may result in increased dietary energy density and, along with other poor dietary habits, represents a risk factor for excess weight gain and obesity [6,11,12].
Dietary guidelines also recommend that youth limit consumption of energy-dense, nutrient-poor foods such as those high in added sugars [3]. However, sugar consumption among children and adolescents is a major problem. Studies have shown that children and adolescents consume an excess of energy-dense, nutrient-poor foods that are high in added sugar and precipitate excess weight gain. According to the 2010 Dietary Guidelines for Americans, intake of discretionary calories, such as those from added sugars, should be limited to 5-15% of daily caloric intake [4]. However, recent estimates have found that calories from added sugars represent as much as 16% of the total daily energy intake for children and adolescents [13]. Sugar-sweetened beverage (SSB) consumption is a major contributor to daily added sugar intake in youth, especially among adolescents [3,14]. One study of SSB intake in youth that examined the 2009-2010 National Health and Nutrition Examination Survey (NHANES) data found that SSBs contributed approximately 8% of daily energy intake among children and adolescents [15]. This is a particularly alarming problem because excess consumption of SSBs has been associated with displacement of nutrient-rich foods [14]. Unhealthful dietary patterns may be explained by the increase in availability of processed, nutrientpoor foods that has occurred over the past several decades, as well as increased availability of convenience foods [3]. Poor dietary intake may also be partially driven or exacerbated by maladaptive eating behaviors.
Several studies have found that some children and adolescents engage in maladaptive eating styles that precipitate weight gain including emotional eating [16-20] external eating [16,20] binge eating [21-24] and eating in response to cravings [25]. Emotional eating, defined as eating in response to emotional arousal [26] and binge eating, defined as a loss of control over eating, have been postulated by escape theory [27] and affect regulation models [28,29] to be maladaptive coping mechanisms for emotional distress and negative self-assessments [30]. Emotional eating and binge eating can also be explained by the psychosomatic theory, which hypothesizes that eating in response to emotional arousal may be due to an inability to differentiate between physical hunger cues and emotional cues [30,31]. External eating, defined as eating in response to food-related cues, such as the sight, smell, and taste of food [32] has been postulated by externality theory to be due to a heightened sensitivity to such external food cues [30,33]. Clearly, the problem of obesity-related eating behaviors in youth is a large, multi-faceted problem.
Consequences of Obesity-related Eating Behaviors to Health and Well-being
Weight gain is caused by an accumulation of positive energy balance over time [34]. Positive energy balance occurs when energy intake exceeds energy expenditure [34,35]. Growing evidence supports that poor dietary patterns and maladaptive eating styles are linked with weight gain due to their contributions to excess energy intake and thus [36] positive energy balance. A recent meta-analysis and systematic review that examined results from sixty randomized controlled trials and prospective cohort studies concluded that in both adults and youth, increased intake of dietary sugars was associated with increased body weight, while reduced dietary sugar intake was associated with decreased body weight [37]. Contrary to dietary sugar intake, consumption of dietary fiber, fruits, and vegetables has been found to be protective against overweight and obesity. Findings from epidemiologic studies indicate that dietary fiber, fruit, and vegetable intake are associated with lower body mass, and findings from intervention studies show that dietary fiber intake leads to weight loss [38-40]. This evidence suggests that that poor dietary patterns and problem eating behaviors can increase risk for overweight and obesity. Indeed, overweight and obesity are major health issues among children and adolescents in the U.S. Although there has been recent evidence of a plateau in the growth of overweight and obesity among youth [41-46] the prevalence is nonetheless alarmingly high. According to the latest available National Health and Nutrition Examination Survey (NHANES) data, 31.8% of youth aged 2-19 years in this country are overweight or obese [47] of those, 16.9% meet body mass index (BMI) criteria for obesity [47]. Despite public health efforts on multiple fronts, overweight and obesity prevalence in the general population is proving to be difficult to reduce.
The need to address obesity-related eating behaviors in children and adolescents is highlighted by evidence that poor dietary behaviors, overweight, and obesity during youth are associated with detrimental consequences for health during youth and into adulthood. Poor dietary intake, overweight, and obesity increase risk for chronic diseases including metabolic syndrome, type 2 diabetes [48,49] hypertension [50,51] nonalcoholic fatty liver disease [52,53] and cardiovascular disease [54-56]. Such diseases, which were known only to occur in adults in the past, have now become common among children and adolescents because of the rise of overweight and obesity in youth [57,58]. Studies have also shown that obesity increases risk for certain types of cancer, including pancreatic cancer, colon cancer, and breast cancer [59,60]. Further, excess adiposity is associated with a substantial increase in risk for mortality; relative risk for death increases across the body mass index (BMI) range of overweight and is even higher for obese individuals [61]. This indicates that overweight and obesity represent a serious health issue across the lifespan and highlights the need for effective interventions to combat overweight and obesity, especially early in life.
Overweight and obesity are also critical health issues during youth because of consequences that can impede development and well-being. Low health-related quality of life has been found to be associated with overweight and obesity across age groups [62-64]. Risk for mood disorders such as major depression, bipolar disorder, anxiety, and substance use disorders is higher for obese compared to normal weight youth and adults [56,65-68]. Poor self-esteem and adverse impacts on academic performance are more prevalent among overweight and obese adolescents compared to normal weight adolescents [63]. Such consequences hinder educational attainment and lifetime earnings [69,70] underscoring life-long, adverse impact of overweight and obesity on overall well-being. Growing evidence indicates that being overweight or obese during youth increases the risk for psychological and physical health issues in adulthood. For example, the longitudinal Northern Finland 1966 Birth Cohort Study, which followed participants from ages 14 to 31, found that individuals who were obese at 14 years old were more likely to have physician-diagnosed depression at 31 years old [71]. Participants in the Bogalusa Heart Study who were overweight or obese as adolescents had greater cardiovascular risk factors as young adults, including adverse levels of systolic and diastolic blood pressure, cholesterol, insulin, and glucose, compared to participants who were normal weight as adolescents [72]. One study that examined the association between childhood obesity and cardiovascular morbidity in a 57-year follow-up cohort study using the Carnegie Survey of Family Diet and Health found greater risk for heart disease and cardiovascular mortality for those who were overweight or obese as youth compared to those who were normal weight as youth [73]. Clearly, it is necessary to determine how to prevent and reduce excess adiposity during the critical developmental periods of childhood and adolescence.
The Challenge of establishing healthful eating behaviors in children and adolescents
Childhood and adolescence are critical periods for establishing lifelong weight-related behaviors [74,75] as dietary habits, overweight, and obesity in children and adolescents tend to track into adulthood [6,76,77]. However, establishing healthful eating behaviors during youth can be challenging because of the many competing sources of influence that can negatively impact dietary intake and eating habits. The food environments that children and adolescents are exposed to have a strong influence on their eating behaviors. The school food environment is particularly influential. Youth spend a large proportion of their time in school, so they consume a significant amount of their daily food intake at school [1]. Thus, the types of foods available at school influence what children and adolescents consume. Foods available through vending machines, snack bars, and school stores, which are often energy-dense, nutrient-poor snacks and beverages, can lead to excess caloric intake [1]. Access to these food options is also detrimental because they can replace consumption of more healthful food choices [1]. A recent study found that availability of energydense, nutrient-poor foods at vending machines or other sources in schools was associated with higher BMI z-scores of schoolchildren [1,78]. Evidence such as this demonstrates that the food available to children in the school environment can affect their food intake choices and have implications for excess weight gain.
Advertising represents another crucial influential factor for dietary intake and eating behaviors in children and adolescents. The food industry places a substantial focus on marketing to youth [3]. According to estimates from a recent Federal Trade Commission report, the food industry spends about $1.8 billion annually on marketing foods and beverages to children and adolescents [79]. This marketing is mostly for energy-dense, nutrient poor foods such as candy, fast food, SSBs, and high-sugar breakfast cereals [3]. This is important because evidence indicates that food advertising directly influences the foods that youth request and consume [3,80]. Further, a recent study found that exposure to fast food marketing may contribute to youth overweight and obesity in the U.S. [81]. Food advertising clearly has the potential to have a strong impact on eating behaviors and risk for excess weight gain in children and adolescents.
Household sociocultural factors also have a particularly poignant impact on dietary intake and eating habits in youth, especially during early childhood. Parenting practices, for example, can negatively impact eating behaviors despite good intentions. Feeding strategies aimed at controlling dietary intake such as restricting certain foods or pressuring children to eat certain foods can incite problem eating behaviors such as overeating and compulsion to eat “forbidden” foods [3]. Food intake by parents and siblings have also been shown to influence dietary intake by youth, particularly for fruits, vegetables, fat, and total energy [82].
Children and adolescents certainly do not have absolute control over the foods they consume, since factors that parents usually control such as home food availability [83] and parent feeding practices [84] are significant influences on youth’s dietary intake. However, what they choose to consume at school, how they adjust to parent feeding practices and other home environment factors, and how they react to media influences are factors over which youth can potentially have agency. Given that overweight, obesity, and obesity-related eating behaviors continue to be significant health issues among children and adolescents, youth need to develop skills that will enable them to make healthful dietary choices and practice healthful eating behaviors in the face of many influences.
Mindfulness Training: A possible Intervention Approach for Obesity-related Eating Behaviors
A large body of intervention research has been conducted pertaining to improving eating behaviors in children and adolescents. Most of this research has focused on family-based interventions aimed at improving eating behaviors and dietary intake in the home environment and school-based interventions aimed at improving nutrition knowledge and access to healthful foods in the school environment. Findings have shown that while these types of interventions can be successful at modifying eating behaviors in youth, novel approaches may be necessary to improve intervention efforts. For example, family-based interventions have been shown to be effective at improving child eating habits and dietary intake [85,86]. However, evidence indicates that family-based interventions are not always effective for all youth or their families, and post-intervention relapse is common [87].
School-based interventions aimed at improving dietary intake among children and adolescents have had mixed results. A recent meta-analysis and systematic review of school-based interventions for increasing fruit and vegetable intake in youth concluded that schoolbased interventions can have moderate positive impacts on fruit intake but have little impact on vegetable intake [6]. Another systematic review found that school-based interventions aimed at generally improving healthful dietary intake can lead to moderate improvements [88]. However, a different recent review of schoolbased lifestyle interventions to prevent obesity in children found results from dietary interventions to be short-term and inconsistent [89]. According to an overview of past research and future directions in school-based obesity intervention research, the modest effects from school-based interventions demonstrates that future interventions may need to incorporating alternative intervention approaches [90]. Although interventions aimed at improving eating behaviors in children and adolescents can be effective, integration of novel intervention components may be useful for improving short-term and long-term intervention effects.
Mindfulness training may be a promising complimentary or integrative approach for improving eating behavior outcomes in children and adolescents in various settings. Mindfulness is most commonly defined as a quality of consciousness characterized by continually attending to one’s moment-by-moment experiences, thoughts, and emotions in an open, non-judgmental manner [91]. It can be cultivated through systematic training by practicing mindfulness mediations and exercises [92]. Mindfulness-based interventions (MBIs) have gained popularity for treating obesityrelated eating behaviors. A recent systematic literature review by our research group examined the effectiveness of MBIs for obesity-related eating behaviors including binge eating, emotional eating, external eating, and dietary intake in adults [30]. The review found that MBIs appear to be effective for improving binge eating, emotional eating, and external eating behaviors [30]. The review also found that additional research is needed to determine if MBIs can improve dietary intake [30]. However, there is potential for MBIs to be effective intervention approaches for dietary intake. Only three studies examined the impact of a MBI on dietary intake, but two of the three studies reported improvements in dietary intake factors including total daily energy intake [93,94] and glycemic index and glycemic load of diet [93]. While the literature on MBIs lacks studies utilizing mindfulness training aimed at improving eating behaviors in youth, the growing field of mindfulness research in children and adolescents as well as the evidence from obesity-related eating behavior studies in adults indicates that this may be a potentially promising intervention approach for children and adolescents.
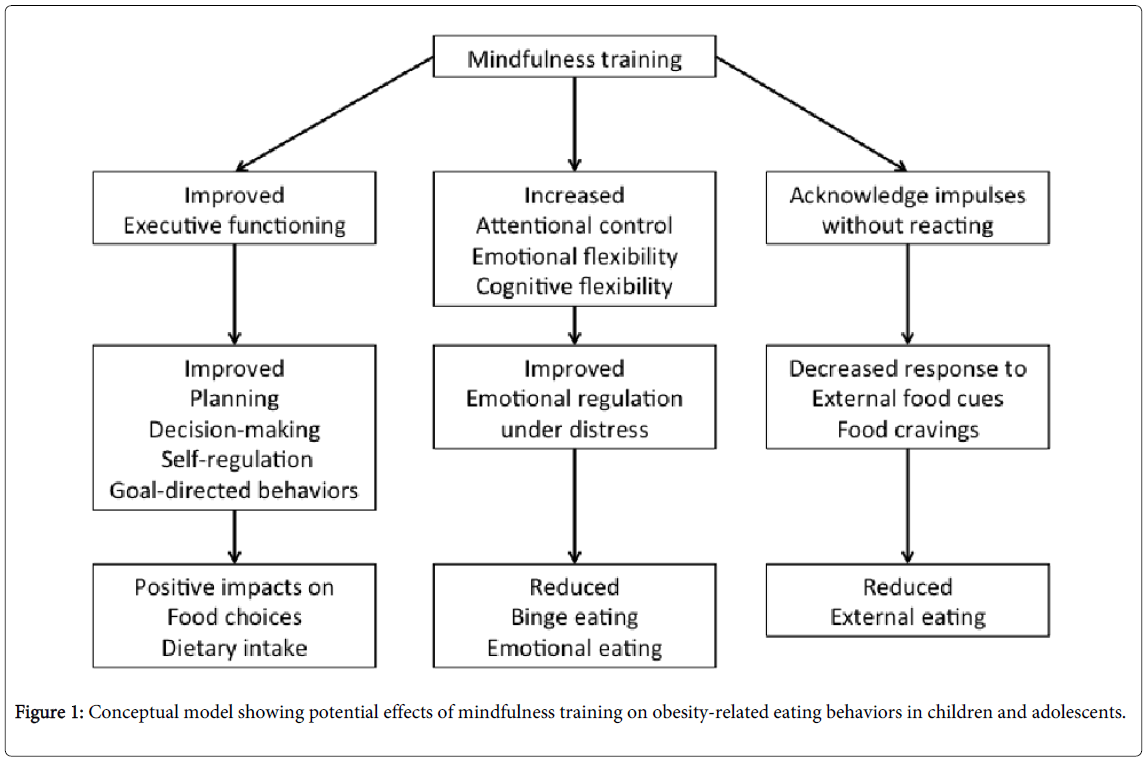
In recent years, there has been a surge in mindfulness training programs offered to youth by organizations in the U.S. and around the world as well as an increase in evidence from studies investigating the efficacy of mindfulness training for various health conditions that this intervention approach can be successfully implemented in children and adolescents [95,96]. The growth of MBIs for children and adolescents demonstrates that mindfulness programs are a viable intervention method for helping youth cultivate the ability to make healthful decisions about the foods they eat and establish healthful approaches to the way they eat. Regular engagement in mindfulness practice can modulate the neural systems involved decision-making and habitual reactions [97]. Findings from MBI studies in youth have shown that mindfulness training can improve executive functioning in children and adolescents [95]. Improved executive function has positive implications for planning, decision-making, self-regulation, and goal-directed behaviors [95,98].
These improved mental qualities could prime children to make healthful food choices in the midst of the obesogenic food environment. Regular engagement in mindfulness practice also strengthens attentional control, emotional flexibility, and cognitive flexibility, [99] which in turn reduces engagement in maladaptive, habitual behaviors that are often automatically carried out under stress [100]. A recent review of MBIs for children and adolescents found that mindfulness training leads to improved emotion regulation skills for youth spanning an age range of 6 to 18 years [95]. These skills could help children and adolescents develop adaptive responses to psychological distress and prevent them from forming maladaptive responses such engaging in emotional eating and binge eating. Mindfulness training can also cultivate skills that help one to acknowledge impulses, such as the impulse to eat in reaction to food cues, but not to act on those impulses [30]. This could mitigate external eating and eating in response to cravings in children and adolescents. Figure 1 provides a conceptual overview of possible ways in which mindfulness training may impact eating behaviors in children and adolescents.
Future Directions and Conclusions
Previous research has shown that MBIs have been successful for treating obesity-related eating behaviors in adults [30]. To our knowledge, no published trials to date have examined the impact of mindfulness training on obesity-related eating behaviors in children or adolescents. Consequently, our conceptual review serves as a call for formative research to understand how MBIs can be implemented for optimal effectiveness in young populations. One area that will require extensive research is the impact of mindfulness training on dietary intake. Few studies have been conducted to understand how MBIs can influence food choice and consumption. However, there is some evidence that mindfulness training may shift dietary intake to more healthful dietary patterns in adults. Given that poor dietary intake is such a prominent issue among children and adolescents, future studies should aim to determine if MBIs can be effective standalone interventions or supplementary components to family-based and school-based interventions aimed at improving dietary intake in youth.
Other obesity-related eating behaviors such as binge eating, emotional eating, and external eating are not typically targeted in family-based or school-based nutrition interventions. Future studies should also focus on determining if the positive impacts of mindfulness training on these obesity-related eating behaviors that have been observed in adults can be replicated in children and adolescents. Given findings from MBI eating behavior studies in adults and evidence that mindfulness training can be successfully implemented in children and adolescents, mindfulness training represents a potentially promising approach to help children and adolescents develop positive relationships with food and healthful eating behaviors in a manner that might reduce the costly impact of obesity in the United States.
References
- Story M, Neumark-Sztainer D, French S (2002) Individual and environmental influences on adolescent eating behaviors.J Am Diet Assoc 102: S40-51.
- Piernas C, Popkin BM (2011) Food portion patterns and trends among U.S. children and the relationship to total eating occasion size, 1977-2006.J Nutr 141: 1159-1164.
- Gidding SS, Dennison BA, Birch LL, Daniels SR, Gilman MW, et al. (2006) Dietary recommendations for children and adolescents: a guide for practitioners. Pediatrics 117:544-559.
- McGuire S (2011) US Department of Agriculture and US Department of Health and Human Services, Dietary Guidelines for Americans, 2010. Washington, DC: US Government Printing Office, January 2011. Advances in Nutrition: An International Review Journal 2:293-294.
- Lorson BA, Melgar-Quinonez HR, Taylor CA (2009) Correlates of fruit and vegetable intakes in US children.J Am Diet Assoc 109: 474-478.
- Evans CE, Christian MS, Cleghorn CL, Greenwood DC, Cade JE (2012) Systematic review and meta-analysis of school-based interventions to improve daily fruit and vegetable intake in children aged 5 to 12 y.Am J ClinNutr 96: 889-901.
- Andersen LF, Øverby N, Lillegaard IT (2004) [Intake of fruit and vegetables among Norwegian children and adolescents].Tidsskr Nor Laegeforen 124: 1396-1398.
- Vereecken CA, De Henauw S, Maes L (2005) Adolescents' food habits: results of the Health Behaviour in School-aged Children survey.Br J Nutr 94: 423-431.
- Timperio A, Ball K, Roberts R, Campbell K, Andrianopoulos N, et al. (2008) Children's fruit and vegetable intake: associations with the neighbourhood food environment.Prev Med 46: 331-335.
- Brauchla M, Juan W, Story J, Kranz S (2012) Sources of Dietary Fiber and the Association of Fiber Intake with Childhood Obesity Risk (in 2-18 Year Olds) and Diabetes Risk of Adolescents 12-18 Year Olds: NHANES 2003-2006.J NutrMetab 2012: 736258.
- Branum AM, Rossen LM (2014) The contribution of mixed dishes to vegetable intake among US children and adolescents.Public Health Nutr 17: 2053-2060.
- He K, Hu FB, Colditz GA, Manson JE, Willett WC, et al. (2004) Changes in intake of fruits and vegetables in relation to risk of obesity and weight gain among middle-aged women.Int J ObesRelatMetabDisord 28: 1569-1574.
- McGuire S, Ervin RB, Kit BK, Carroll MD, Ogden CL(2012). Consumption of added sugar among U.S. children and adolescents, 2005-2008. NCHS data brief no 87. Hyattsville, MD: National Center for Health Statistics. AdvNutr 3: 534.
- Park S, Blanck HM, Sherry B, Brener N, O'Toole T (2012) Factors associated with sugar-sweetened beverage intake among United States high school students.J Nutr 142: 306-312.
- Kit BK, Fakhouri TH, Park S, Nielsen SJ, Ogden CL (2013) Trends in sugar-sweetened beverage consumption among youth and adults in the United States: 1999-2010.Am J ClinNutr 98: 180-188.
- Braet C, Van Strien T (1997) Assessment of emotional, externally induced and restrained eating behaviour in nine to twelve-year-old obese and non-obese children.Behav Res Ther 35: 863-873.
- Kelly C, Ricciardelli LA, Clarke JD (1999) Problem eating attitudes and behaviors in young children.Int J Eat Disord 25: 281-286.
- Nguyen-Michel ST, Unger JB, Spruijt-Metz D (2007) Dietary correlates of emotional eating in adolescence.Appetite 49: 494-499.
- Nguyen-Rodriguez ST, Chou CP, Unger JB, Spruijt-Metz D (2008) BMI as a moderator of perceived stress and emotional eating in adolescents.Eat Behav 9: 238-246.
- Snoek HM, van Strien T, Janssens JM, Engels RC (2007) Emotional, external, restrained eating and overweight in Dutch adolescents.Scand J Psychol 48: 23-32.
- Czaja J, Rief W, Hilbert A (2009) Emotion regulation and binge eating in children.Int J Eat Disord 42: 356-362.
- Decaluwé V, Braet C, Fairburn CG (2003) Binge eating in obese children and adolescents.Int J Eat Disord 33: 78-84.
- Marcus MD, Kalarchian MA (2003) Binge eating in children and adolescents. International Journal of Eating Disorders34: S47-S57.
- Tanofsky-Kraff M (2008) Binge eating among children and adolescents. Handbook of childhood and adolescent obesity: Springer 43-59.
- Nederkoorn C, Braet C, Van Eijs Y, Tanghe A, Jansen A (2006) Why obese children cannot resist food: the role of impulsivity.Eat Behav 7: 315-322.
- van Strien T, Ouwens MA (2007) Effects of distress, alexithymia and impulsivity on eating.Eat Behav 8: 251-257.
- Heatherton TF, Baumeister RF (1991) Binge eating as escape from self-awareness.Psychol Bull 110: 86-108.
- Aldao A, Nolen-Hoeksema S, Schweizer S (2010) Emotion-regulation strategies across psychopathology: A meta-analytic review.ClinPsychol Rev 30: 217-237.
- Wedig MM, Nock MK (2010) The functional assessment of maladaptive behaviors: a preliminary evaluation of binge eating and purging among women.Psychiatry Res 178: 518-524.
- O'Reilly GA, Cook L, Spruijt-Metz D, Black DS (2014) Mindfulness-based interventions for obesity-related eating behaviours: a literature review.Obes Rev 15: 453-461.
- Bruch H (1964) Psychological aspects of overeating and obesity.Psychosomatics 5: 269-274.
- van Strien T, Herman CP, Verheijden MW (2009) Eating style, overeating, and overweight in a representative Dutch sample. Does external eating play a role?Appetite 52: 380-387.
- Schachter S, Rodin J (1974).Obese humans and rats: Lawrence Erlbaum.
- Rennie KL, Johnson L, Jebb SA (2005) Behavioural determinants of obesity.Best Pract Res ClinEndocrinolMetab 19: 343-358.
- Jebb SA (2007) Dietary determinants of obesity.Obes Rev 8 Suppl 1: 93-97.
- Adam TC, Epel ES (2007) Stress, eating and the reward system.PhysiolBehav 91: 449-458.
- TeMorenga L, Mallard S, Mann J (2012) Dietary sugars and body weight: systematic review and meta-analyses of randomised controlled trials and cohort studies.BMJ 346: e7492.
- Slavin JL (2005) Dietary fiber and body weight.Nutrition 21: 411-418.
- Lissner L, Lindroos AK, Sjöström L (1998) Swedish obese subjects (SOS): an obesity intervention study with a nutritional perspective.Eur J ClinNutr 52: 316-322.
- Kimm SY (1995) The role of dietary fiber in the development and treatment of childhood obesity.Pediatrics 96: 1010-1014.
- Flegal KM, Carroll MD, Kit BK, Ogden CL (2012) Prevalence of obesity and trends in the distribution of body mass index among US adults, 1999-2010.JAMA 307: 491-497.
- Ogden CL, Carroll MD, Kit BK, Flegal KM (2012) Prevalence of obesity and trends in body mass index among US children and adolescents, 1999-2010.JAMA 307: 483-490.
- Finkelstein EA, Khavjou OA, Thompson H, Trogdon JG, Pan L, et al. (2012) Obesity and severe obesity forecasts through 2030.Am J Prev Med 42: 563-570.
- Flegal KM, Carroll MD, Ogden CL, Curtin LR (2010) Prevalence and trends in obesity among US adults, 1999-2008.JAMA 303: 235-241.
- Skinner AC, Skelton JA2 (2014) Prevalence and trends in obesity and severe obesity among children in the United States, 1999-2012.JAMA Pediatr 168: 561-566.
- Slining MM, Mathias KC, Popkin BM (2013) Trends in food and beverage sources among US children and adolescents: 1989-2010.J AcadNutr Diet 113: 1683-1694.
- Ogden CL, Carroll MD, Kit BK, Flegal KM (2014) Prevalence of childhood and adult obesity in the United States, 2011-2012.JAMA 311: 806-814.
- Kahn SE, Hull RL, Utzschneider KM (2006) Mechanisms linking obesity to insulin resistance and type 2 diabetes.Nature 444: 840-846.
- Goran MI, Ball GD, Cruz ML (2003) Obesity and risk of type 2 diabetes and cardiovascular disease in children and adolescents.J ClinEndocrinolMetab 88: 1417-1427.
- Sorof J, Daniels S (2002) Obesity hypertension in children: a problem of epidemic proportions.Hypertension 40: 441-447.
- Faloia E, Giacchetti G, Mantero F (2000) Obesity and hypertension.J Endocrinol Invest 23: 54-62.
- Fabbrini E, Sullivan S, Klein S (2010) Obesity and nonalcoholic fatty liver disease: biochemical, metabolic, and clinical implications.Hepatology 51: 679-689.
- Angulo P (2007) Obesity and nonalcoholic fatty liver disease.Nutr Rev 65: S57-63.
- Van Gaal LF, Mertens IL, De Block CE (2006) Mechanisms linking obesity with cardiovascular disease.Nature 444: 875-880.
- Poirier P, Giles TD, Bray GA, Hong Y, Stern JS, et al. (2006).Obesity and cardiovascular disease pathophysiology, evaluation, and effect of weight loss. Arteriosclerosis, thrombosis, and vascular biology 26(5):968-976.
- Reilly JJ, Methven E, McDowell ZC, Hacking B, Alexander D, et al. (2003) Health consequences of obesity.Arch Dis Child 88: 748-752.
- Centers for Disease C, Prevention, Centers for Disease C, Prevention. National diabetes fact sheet: national estimates and general information on diabetes and prediabetes in the United States, 2011. Atlanta, GA: US Department of Health and Human Services, Centers for Disease Control and Prevention 201.
- Yanovski SZ, Yanovski JA (2011) Obesity prevalence in the United States--up, down, or sideways?N Engl J Med 364: 987-989.
- Wolk A, Gridley G, Svensson M, Nyrén O, McLaughlin JK, et al. (2001) A prospective study of obesity and cancer risk (Sweden).Cancer Causes Control 12: 13-21.
- Renehan AG, Tyson M, Egger M, Heller RF, Zwahlen M (2008) Body-mass index and incidence of cancer: a systematic review and meta-analysis of prospective observational studies.Lancet 371: 569-578.
- Calle EE, Teras LR, Thun MJ (2005) Obesity and mortality.N Engl J Med 353: 2197-2199.
- Ford ES, Moriarty DG, Zack MM, Mokdad AH, Chapman DP (2001) Self-reported body mass index and health-related quality of life: findings from the Behavioral Risk Factor Surveillance System.Obes Res 9: 21-31.
- Swallen KC, Reither EN, Haas SA, Meier AM (2005) Overweight, obesity, and health-related quality of life among adolescents: the National Longitudinal Study of Adolescent Health.Pediatrics 115: 340-347.
- Williams J, Wake M, Hesketh K, Maher E, Waters E (2005) Health-related quality of life of overweight and obese children.JAMA 293: 70-76.
- Petry NM, Barry D, Pietrzak RH, Wagner JA (2008). Overweight and obesity are associated with psychiatric disorders: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Psychosomatic medicine 70:288-297.
- Simon GE, Von Korff M, Saunders K, Miglioretti DL, Crane PK, et al. (2006) Association between obesity and psychiatric disorders in the US adult population.Arch Gen Psychiatry 63: 824-830.
- Onyike CU, Crum RM, Lee HB, Lyketsos CG, Eaton WW (2003) Is obesity associated with major depression? Results from the Third National Health and Nutrition Examination Survey.Am J Epidemiol 158: 1139-1147.
- Mustillo S, Worthman C, Erkanli A, Keeler G, Angold A, et al. (2003) Obesity and psychiatric disorder: developmental trajectories.Pediatrics 111: 851-859.
- Karnehed N, Rasmussen F, Hemmingsson T, Tynelius P (2006) Obesity and attained education: cohort study of more than 700,000 Swedish men.Obesity (Silver Spring) 14: 1421-1428.
- Gortmaker SL, Must A, Perrin JM, Sobol AM, Dietz WH (1993) Social and economic consequences of overweight in adolescence and young adulthood.N Engl J Med 329: 1008-1012.
- Herva A, Laitinen J, Miettunen J, Veijola J, Karvonen JT, et al. (2006) Obesity and depression: results from the longitudinal Northern Finland 1966 Birth Cohort Study.Int J Obes (Lond) 30: 520-527.
- Srinivasan SR, Bao W, Wattigney WA, Berenson GS (1996) Adolescent overweight is associated with adult overweight and related multiple cardiovascular risk factors: the Bogalusa Heart Study.Metabolism 45: 235-240.
- Gunnell DJ, Frankel SJ, Nanchahal K, Peters TJ, Davey Smith G (1998) Childhood obesity and adult cardiovascular mortality: a 57-y follow-up study based on the Boyd Orr cohort.Am J ClinNutr 67: 1111-1118.
- Baranowski T, Mendlein J, Resnicow K, Frank E, Cullen KW, et al.(2000). Physical activity and nutrition in children and youth: an overview of obesity prevention. Preventive Medicine. 31(2):S1-S10.
- Li J, Wang Y (2008) Tracking of dietary intake patterns is associated with baseline characteristics of urban low-income African-American adolescents.J Nutr 138: 94-100.
- Singh AS, Mulder C, Twisk JW, van Mechelen W, Chinapaw MJ (2008) Tracking of childhood overweight into adulthood: a systematic review of the literature.Obes Rev 9: 474-488.
- Maynard M, Gunnell D, Ness AR, Abraham L, Bates CJ, et al. (2006) What influences diet in early old age? Prospective and cross-sectional analyses of the Boyd Orr cohort.Eur J Public Health 16: 316-324.
- Fox MK, Dodd AH, Wilson A, Gleason PM (2009) Association between school food environment and practices and body mass index of US public school children.J Am Diet Assoc 109: S108-117.
- Federal Trade C (2012) A review of food marketing to children and adolescents: follow-up report. Washington, DC: Federal Trade Commission.
- Scully M, Wakefield M, Niven P, Chapman K, Crawford D, et al. (2012) Association between food marketing exposure and adolescents' food choices and eating behaviors.Appetite 58: 1-5.
- McClure AC, Tanski SE, Gilbert-Diamond D, Adachi-Mejia AM, Li Z, et al. (2013) Receptivity to television fast-food restaurant marketing and obesity among U.S. youth.Am J Prev Med 45: 560-568.
- van der Horst K, Oenema A, Ferreira I, Wendel-Vos W, Giskes K, et al. (2007) A systematic review of environmental correlates of obesity-related dietary behaviors in youth.Health Educ Res 22: 203-226.
- Campbell KJ, Crawford DA, Salmon J, Carver A, Garnett SP, et al. (2007) Associations between the home food environment and obesity-promoting eating behaviors in adolescence.Obesity (Silver Spring) 15: 719-730.
- Savage JS, Fisher JO, Birch LL (2007) Parental influence on eating behavior: conception to adolescence.J Law Med Ethics 35: 22-34.
- Müller MJ, Danielzik S, Pust S (2005) School- and family-based interventions to prevent overweight in children.ProcNutrSoc 64: 249-254.
- Young KM, Northern JJ, Lister KM, Drummond JA, O'Brien WH (2007) A meta-analysis of family-behavioral weight-loss treatments for children.ClinPsychol Rev 27: 240-249.
- Kitzmann KM, Beech BM (2006) Family-based interventions for pediatric obesity: methodological and conceptual challenges from family psychology.J FamPsychol 20: 175-189.
- De Bourdeaudhuij I, Van Cauwenberghe E, Spittaels H, Oppert JM, Rostami C, et al. (2011) School-based interventions promoting both physical activity and healthy eating in Europe: a systematic review within the HOPE project.Obes Rev 12: 205-216.
- Brown T, Summerbell C (2009) Systematic review of school-based interventions that focus on changing dietary intake and physical activity levels to prevent childhood obesity: an update to the obesity guidance produced by the National Institute for Health and Clinical Excellence. Obesity reviews10:110-141.
- Peterson KE, Fox MK (2007) Addressing the epidemic of childhood obesity through school-based interventions: what has been done and where do we go from here?J Law Med Ethics 35: 113-130.
- Brown KW, Ryan RM (2003) The benefits of being present: mindfulness and its role in psychological well-being. Journal of personality and social psychology. 84:822.
- Daubenmier J, Kristeller J, Hecht FM, Maninger N, Kuwata M (2011) Mindfulness intervention for stress eating to reduce cortisol and abdominal fat among overweight and obese women: an exploratory randomized controlled study. Journal of obesity.
- Miller CK, Kristeller JL, Headings A, Nagaraja H, Miser WF (2012) Comparative effectiveness of a mindful eating intervention to a diabetes self-management intervention among adults with type 2 diabetes: a pilot study. Journal of the Academy of Nutrition and Dietetics112:1835-1842.
- Timmerman GM, Brown A (2012) The effect of a mindful restaurant eating intervention on weight management in women.J NutrEducBehav 44: 22-28.
- Black DS (2015) Mindfulness Training for Children and adolescents. Handbook of Mindfulness: Theory, Research, and Practice PP :283.
- Black DS, Milam J, Sussman S (2009) Sitting-meditation interventions among youth: a review of treatment efficacy.Pediatrics 124: e532-541.
- Vago DR (2014) Mapping modalities of self-awareness in mindfulness practice: a potential mechanism for clarifying habits of mind.Ann N Y AcadSci 1307: 28-42.
- Suchy Y (2009) Executive functioning: overview, assessment, and research issues for non-neuropsychologists.Ann Behav Med 37: 106-116.
- Malinowski P (2013) Neural mechanisms of attentional control in mindfulness meditation.Front Neurosci 7: 8.
- Levesque C, Brown KW (2007) Mindfulness as a moderator of the effect of implicit motivational self-concept on day-to-day behavioral motivation. Motivation and Emotion 31:284-299.
Relevant Topics
- Adolescent Anxiety
- Adult Psychology
- Adult Sexual Behavior
- Anger Management
- Autism
- Behaviour
- Child Anxiety
- Child Health
- Child Mental Health
- Child Psychology
- Children Behavior
- Children Development
- Counselling
- Depression Disorders
- Digital Media Impact
- Eating disorder
- Mental Health Interventions
- Neuroscience
- Obeys Children
- Parental Care
- Risky Behavior
- Social-Emotional Learning (SEL)
- Societal Influence
- Trauma-Informed Care
Recommended Journals
Article Tools
Article Usage
- Total views: 16995
- [From(publication date):
June-2015 - Apr 07, 2025] - Breakdown by view type
- HTML page views : 12235
- PDF downloads : 4760