Case Report Open Access
Congenital Mucocele of Tongue: A Rare Cause of Acute RespiratoryDistress
Williams J*, Nagarkar NM and Arora RD
Department of E.N.T and Head and Neck surgery, All Indian Institute of Medical Sciences, Raipur, Chattisgarh, India
- *Corresponding Author:
- Williams J
Department of E.N.T and Head and Neck surgery
All Indian Institute of Medical Sciences
Raipur, Chattisgarh, India
Tel: 8518887334
E-mail: josephwilliams.joey@ymail.com
Received Date: November 13, 2016; Accepted Date: December 02, 2016; Published Date: December 09, 2016
Citation: Williams J, Nagarkar NM, Arora RD (2016) Congenital Mucocele of Tongue: A Rare Cause of Acute Respiratory Distress. Neonat Pediatr Med 2: 115. doi: 10.4172/2572-4983.1000115
Copyright: © 2016 Williams J, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Neonatal and Pediatric Medicine
Abstract
Introduction: Congenital tongue cyst is a very rare presentation with few cases reported in literature. Mucoceles involving the ventral surface of the tongue are very rare, with sporadic cases reported in the world literature accounting to 2-8% of oral mucoceles. Case report: We report a case of 4 months old male child presenting with respiratory distress for one day and complete cessation of feeding for last 3 days presented to our outpatient department. Examination revealed a cystic lesion over ventral aspect of tongue causing obstruction to both feeding and respiration, a provisional diagnosis of tongue cyst was made, urgent aspiration of the cyst was done which revealed a mucoid brownish fluid. This reduced the size of the cyst and breathing improved. The cyst was taken for marsupialization under GA and child had immediate relief of symptoms. Regular follow up shows no recurrence of symptoms for the last 6 months. Conclusion: Tongue base cysts should be considered in differential diagnosis in new born with stridor, respiratory difficulties, or swallowing problems. Definitive therapy requires marsupialization or complete excision of the cyst wall under general anesthesia.
Keywords
Tongue cyst; Mucocele; Respiratory distress
Introduction
Congenital mucocele of tongue is a very uncommon condition where the infant is presented with airway obstruction, feeding difficulty, respiratory destress and failure to thrive. Prenatal detection of these lesions is important since they may cause breathing problems at birth and interfere with breastfeeding. An approximate annual incidence of congenital mucocele is 1.82 per 100000 live births in an oriental population was reported [1]. The incidence of retention cyst in oral cavity is much more common in the general population and is estimated as 2.4 cases per 1,000 populations, frequently occurring in the second decade of life [2,3]. Mucoceles involving the ventral surface of the tongue are very rare, with sporadic cases reported in the world literature [4,5] accounting to 2-8% of oral mucoceles [6]. A tongue cyst could also be completely asymptomatic and could persist till adolescent with subsequent regression of the symptoms. A suspected case of tongue cyst should be followed up with routine investigation along with imaging to come to a conclusive diagnosis and to know the extent of the cyst. Here we present a case of 4-month male child with history of congenital tongue presenting with upper airway obstruction and difficulty in feeding.
Case Report
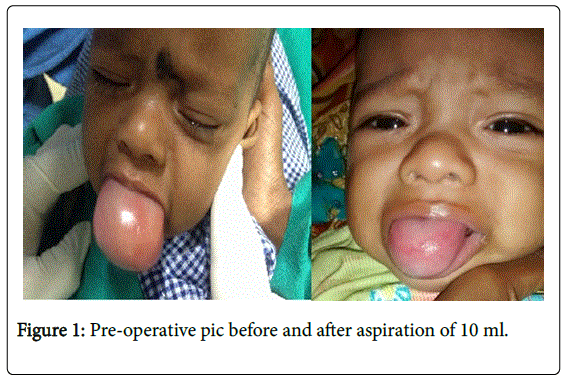
We present a case of, 4 months old infant presented to ENT outpatient clinic with respiratory destress difficulty for one day and complete cessation of breast feeding for 3 days. The child had history of swelling of the tongue since birth (Figure 1). The child was not able to close the mouth since birth and with history of excessive drooling of saliva. The child had a normal home delivery with immediate cry after birth. There was no history of respiratory distress, cyanosis or feeding difficulty after birth. Feeding difficulty started from 3 month and frequency of feeding had reduced subsequently.
Patient developed difficulty in breathing from last one day and complete cessation of feeding for the last 3 days. On examination the infant was on respiratory distress with noisy breathing, increased respiratory rate and in drawing of chest. The dorsum of tongue was in normal texture with a bulge of tongue seen with complete obstruction of oral cavity. The base of tongue couldn’t be visualized. The ventral aspect of tongue was thinned out and tense on palpation. Wide bore needle aspiration was done on the ventral aspect and 10 ml of purulent brownish fluid was aspirated reducing the total size of tongue, with mild relief of breathing difficulty.
Patient was taken up for surgery and trans oral intubation was done after aspiration of another 10 ml from the tongue cyst as it was a difficult intubation with the boggy tongue.
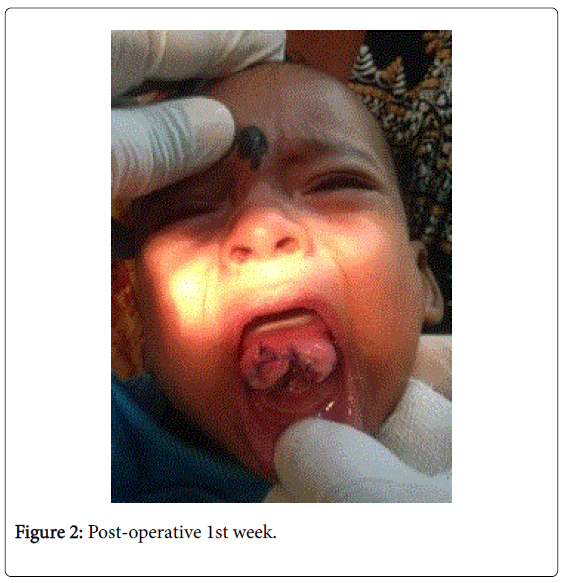
Stay suture was applied on the anterior aspect of the tongue to expose the ventral aspect of tongue and vertical incision was given deep to expose the cyst wall which extended from the tip of tongue to lower attachment of ventral part of tongue to floor of mouth. A mucoid brownish fluid had been expressed from the cyst which had been sent for culture and sensitivity. The cyst was completely opened and marsupialization was done. The child had been kept on intravenous steroids for 3 days post operatively to prevent tongue edema. The aspirate from the cyst was mucoid in nature and culture from the aspirate showed no growth after 48 hours of inoculation. One-week post OP child showed significant improvement with no respiratory difficulty and no difficulty in breast feeding (Figure 2).
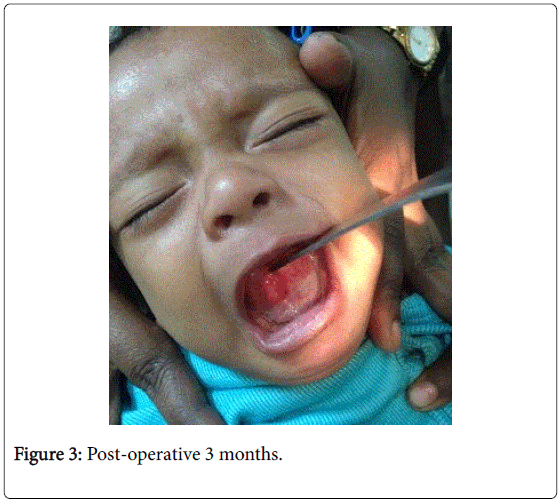
The child had been able to close his mouth while sleeping after 1st week of post OP. After 3 months the tongue has attained normal shape and mobility (Figure 3). Patient has been kept on regular follow-up every month with no recurrence till date (6 months). The child was able to close mouth and had reported weight gain also.
Discussion
Tongue cyst is a rather rare occurrence with very few cases reported in literature. Majority of cases with a tongue cyst are asymptomatic and would regress as age progresses. Two major hypotheses to explain the pathogenesis are that this cyst is a consequence of either ductal obstruction of mucus glands or an embryological malformation [4]. Histologically, the cyst contains respiratory epithelium with mucous glands, with an external lining of squamous epithelium [7-9]. Lingual cysts are variable in size. If large, they can encroach upon the airway and displace the epiglottis, causing airway obstruction. Small cysts are totally asymptomatic. Congenital lesions of the tongue can be a life threatening conditions when it cases stridor special which is usually presenting in base of tongue which would require immediate management after birth. In cases of neonatal stridor, evaluation of the airway anatomy and diagnosis of other causes of stridor are important to prevent any mortality and morbidity from these sources. The lesion present in anterior 2/3 of the tongue are less life threatening as in majority of cases there will not be an airway obstruction but in our case the child developed air way obstruction after early symptoms of swallowing difficulty. The respiratory difficulty could be either because of an infection, edema of the tongue or because the cyst could extent to base of tongue causing oropharyngeal obstruction leading to mechanical obstruction. A simple digital palpation of the tongue up to the base of tongue will give an idea about the location of the lesion in tongue which was not possible in this case as the cyst was large and obstructing the whole oral cavity. Treatment protocol includes a detailed investigation along with imaging to rule out other congenital abnormality as well as to know the extent of the lesion in tongue but may not be always possible due to the airway obstruction, making it an emergency. As the differential diagnosis includes benign tumors, hamartomas, dermoids, teratomas, vascular malformations, and hemangiomas, a fine needle aspiration cytology is recommended before planning for an excision or marsupialization. As the FNAC showed brownish fluid the diagnosis of mucocele was confirmed and planned for marsupialization or cyst excision. The procedure gives immediate relief and the results are gratifying.
Conclusion
Tongue base cysts should be considered in differential diagnosis in new born with stridor, respiratory difficulties, or swallowing problems. Definitive therapy requires marsupialization or complete excision of the cyst wall under general anesthesia.
References
- Wong KS, Huang YH, Wu CT (2007) A vanishing tongue-base cyst. The Turkish Journal of Pediatrics 49: 451-452.
- Coloma CB, Mahmud AJ, Martinez IM, Peñarrocha MA (2011) Congenital oral mucoceles: presentation of four new clinical cases. An Pediatr Barc 75: 424-425.
- Joshi SR, Pendyala GS, Choudhari S, Kalburge J (2012) Mucocele of the glands of blandin-nuhn in children: a clinical, histopathologic, and retrospective study. N Am J Med Sci 4: 379-383.
- Kaneko T, Horie N, Shimoyama T (2012) Congenital mucocele in the tongue: report of a case. J Oral Maxillofac Surg 70: 2596-2599.
- Fernández JMT, Hernández DSP (2001)Tratamiento con micromarsupialización de un mucocele congénito lingual: reporte de un caso. Revista ADM 58: 167-169.
- Yang MA, Kang MJ, Hong JN (2008) A case of congenital vallecular cyst associated with GER presenting with stridor, feeding cyanosis and failure to thrive. Korean Journal of Pediatrics 51: 775-779.
- Ahrens B, Lammert I, Schmitt M, Wahn U, Paul K, et al. (2004) Life-threatening vallecular cyst in a 3 month-old infant: case report and literature review. Clinical Pediatrics 43: 287-290.
- Hsieh WS, Yang PH, Wong KS, Li HY, Wang ECR, et al. (2000) Vallecular cyst: an uncommon cause of stridor in newborn infants. European Journal of Pediatrics 159: 79-81.
- Zaki Z, Ouattassi N, Alami N (2012) Congenital Tongue Base Cyst Presenting with Laryngeal Stridor in Youth: A Case Report. Case Reports in Otolaryngology.
Relevant Topics
- About the Journal
- Birth Complications
- Breastfeeding
- Bronchopulmonary Dysplasia
- Feeding Disorders
- Gestational diabetes
- Neonatal Anemia
- Neonatal Breastfeeding
- Neonatal Care
- Neonatal Disease
- Neonatal Drugs
- Neonatal Health
- Neonatal Infections
- Neonatal Intensive Care
- Neonatal Seizure
- Neonatal Sepsis
- Neonatal Stroke
- Newborn Jaundice
- Newborns Screening
- Premature Infants
- Sepsis in Neonatal
- Vaccines and Immunity for Newborns
Recommended Journals
Article Tools
Article Usage
- Total views: 7273
- [From(publication date):
December-2016 - Jul 14, 2025] - Breakdown by view type
- HTML page views : 6289
- PDF downloads : 984