Concomitant Intraocular and Orbital Space-Occupied Lesions
Received: 24-Feb-2016 / Accepted Date: 30-Mar-2016 / Published Date: 04-Apr-2016 DOI: 10.4172/2476-2075.1000109
Abstract
Purpose/Background: Concomitant intraocular and orbital space-occupied lesions are relatively rare and this is the first report stressing the underlying causes of concomitant intraocular and intraorbital lesions. In this paper, we present cases showing both intraocular and orbital soft tissue masses and highlight their clinical, pathological and imaging features.
Materials and methods: A retrospective review was performed on cases with both intraocular and orbital spaceoccupied lesions who were treated at the Zhongshan Ophthalmic Center, of Sun Yat-sen University, China between Jan 1, 2000 and Dec 31, 2011.
Results: From an initial retrospective review of 1543 patients with a diagnosis of intraocular and/or orbital spaceoccupied lesions, 8 patients (4 males and 4 females) with a coexistence of both intraocular and orbital mass lesions were identified. Patients’ ages ranged from 22 months to 71 years (median = 3.0 years) and included 5 cases of retinoblastoma, 1 case of idiopathic inflammatory pseudotumor, 1 case of T-cell lymphoma, and 1 case of Sturge- Weber syndrome.
Conclusions: Based upon these findings, the presence of a lesion involving both the orbit and eye should be included when a diagnosis of retinoblastoma, idiopathic inflammatory pseudotumor, lymphoma, and/or Sturge- Weber syndrome is proposed.
Keywords: Orbit; Intraocular tumor; Retinoblastoma; Idiopathic inflammatory pseudotumor; Lymphoma; Sturge-Weber syndrome
6281Introduction
Retinoblastoma in children and uveal melanoma in adults represent two of the most common primary intraocular tumors [1,2]. The incidence of orbital lesions in rank order of occurrence include: thyroidal associated ophthalmopathy, vascular lesions, idiopathic inflammatory pseudotumor, and lymphoproliferative neoplasia [3]. Patients demonstrating a concomitant intraocular and orbital spaceoccupied lesion are relatively rare [4,5] and, to the best of our knowledge, this is the first report stressing the underlying causes of concomitant intraocular and intraorbital lesions in the literature. In this paper, we present eight cases showing simultaneous intraocular and orbital soft tissue masses and highlight their clinical, pathological and imaging features.
Materials and Methods
A retrospective review was performed on cases of Chinese patients with clinical findings of simultaneous intraocular and orbital spaceoccupied lesions. Patients were treated at the Zhongshan Ophthalmic Center, of Sun Yat-sen University, Guangzhou, China between Jan 1, 2000 and Dec 31, 2011. The ethics committee of the Zhongshan Ophthalmic Center approved this retrospective study, which was conducted according to the principles expressed in the Declaration of Helsinki. The committee specifically waived the need for consent. The subjects (or their legal guardians) reviewed this manuscript and figures and provided written consent for publication. Clinical, operative and pathological records were reviewed. All patients were seen and treated by a single surgeon (JH Yan). A complete medical history and physical examination with laboratory tests, along with a brain computed tomography (CT) or magnetic resonance imaging (MRI) scan were available for a minimal follow-up period of 1 month.
In addition to recording basic data on the patient’s age, sex, duration of intraocular and orbital lesion at presentation, ocular data included the affected eye and orbit, laterality, symptoms (visual problem, redness or swelling, proptosis, diplopia, palpable mass) and signs (best corrected vision, anterior segment and fundi of the eye, proptosis, ocular motility deficit, strabismus). Tumor data included orbital location (superior, inferior, anterior, posterior), configuration (round, ovoid, diffuse), size, margin (ill-defined, well-defined), quality (rigid, soft, medium), tenderness (present, absent), tissues or spaces involved, as well as findings from imaging and histopathologic examinations [6].
Results
From an initial retrospective review of 1543 cases with a diagnosis of intraocular and/or orbital space-occupied lesions, 8 patients (4 males and 4 females) with a simultaneous coexistence of both intraocular and orbital mass lesions were identified for inclusion in this report. The right orbit was involved in 2 patients, the left orbit in 5 patients and both orbits in 1 patient. The right eye was involved in 2 patients, the left eye in 2 patients and both eyes in 4 patients. The simultaneous coexistence of intraocular and orbital masses was located within the same side of the eye and orbit in these patients. Patients’ ages ranged from 22 months to 71 years (median = 3.0 years). Clinical data on individual patients are summarized in the brief case reports below and presented in detail in Table 1.
| Case No | Age/sex/eye/ diagnosis | Symptoms and signs | Imaging findings | Management | Histologic examination | Final outcomes |
|---|---|---|---|---|---|---|
| 1 | 36 years/F/R/ | Swollen &hyperemia of eyelid & conjunctiva; vision: hand movement/30cm; intraocular pressure: high; rigid, ill-defined mass in the superio-temporal orbit; a gray-white mass in the ciliary body | Ultrasonography and CT: a solid intraocular mass on the temporal side, measuring 22.8×19.3×13.8mm with a rich blood flow signal and an ambiguous soft tissue mass in the superio-temproal orbit; MRI:a homogeneous middle signal on both T1WI and T2WI, moderate enhancement | Systemic steroids;enucleation and biopsy of the orbital mass; a localized radiotherapy(20Gy) | Infiltration of lymphocytes, plasma cells and neutrophils. Immunohistochemistry stain of CD20, CD3 and CD45RO were positive | Cure, no recurrence 1 year after surgery |
| Idiopathic inflammatory pseudotumor | ||||||
| 2 | 71years/F/L | Vision: Light perception. a hard,poor-defined, non-tender, sized 30 × 20 ×5mm mass in the orbit; there was irregular peripheral iris uplift | Ultrasonography and CT: a homogeneous, poor-defined soft tissue mass, with a size of about 3×2cm in the anterior lower portion of left orbit; UBM: a large ciliary body mass from 10:00 to 6:00 o’clock | Incisional biopsy of the left orbital tumor | Tumor cells diffusely arranged, round or irregular in shape, large nucleus, remarkable cell atypia; LCA+, CD45RO+, L26 (-) | Referred to tumor hospital for further check-up and treatment. |
| T-cell lymphoma | ||||||
| 3 | 2 years/M/R | Vision: light perception; a diffuse red-purple soft tissue mass(15mm×16mm) in the middle of the upper eyelid and anterior orbit | Ultrasonography: a well-delineated, high internal echo choroidal mass (10mm×8mm) with a rich blood flow signal. | Refuse to accept any treatment | No | Lost to follow-up |
| Sturge-Weber syndrome | ||||||
| 4 | 3 years/M/R+L | Vision: light perception of right eye and no light perception of left eye; left conjunctival hyperemia, corneal edema, hyphema; white mass within both eyes | CT: soft tissue mass full of both eye with dot calcifition and similar mass in the left orbital and intracranial optic chiasm | Local and systemic chemotherapy | No | Death 6 months later |
| Retinoblastoma with orbital extension and intracranial metastasis | ||||||
| 5 | 3 years/F/R+L Retinoblastoma with orbital extension and intracranial metastasis | Left conjunctival hyperemia, corneal edema, shallow anterior chamber; white mass within both eyes | Ultrasound and CT: soft tissue mass full of both eyes with dot calcifition and similar mass in the left orbital and intracranian | Systemic chemotherapy | No | Death 4 months later |
| 2 years/M/R+L Retinoblastoma with orbital extension | “White eye” of the both eyes for half a year and two large tumors in the orbits for 1 year | CT: two large soft tissue masses with dot calcifition of both eyes and orbits (8.0×7.0cm in the right and 7.5×7.0cm in the left) | Systemic chemotherapy | No | ||
| 6 | 3 years/M/L Retinoblastoma with orbital extension | “White eye” for 1 year and “pain and red” for 2 weeks. remarkable conjunctival congestion, pus-like tumor tissue in the anterior chamber. | Ultrasound and CT: soft tissue mass of the left eye with dot calcifition and similar mass in the left orbit | Orbital evisceration | The diagnosis of retinoblastoma was confirmed | Death 6 months later |
| 7 | 22 months/F/R+L Retinoblastoma with left orbital extension | Atrophy right eye and left hyperemia, corneal opacity, anterior chamber disappeared, intraocular yellow-white mass | Ultrasound and CT: the right eye was atrophy and the left eye showed soft tissue mass with dot calcifition and similar mass in the left orbit | Orbital evisceration | The diagnosis of retinoblastoma was confirmed | Death 2 years later |
Table 1: Clinical Data on eight patients with coexistence of both eye and orbital lesions.
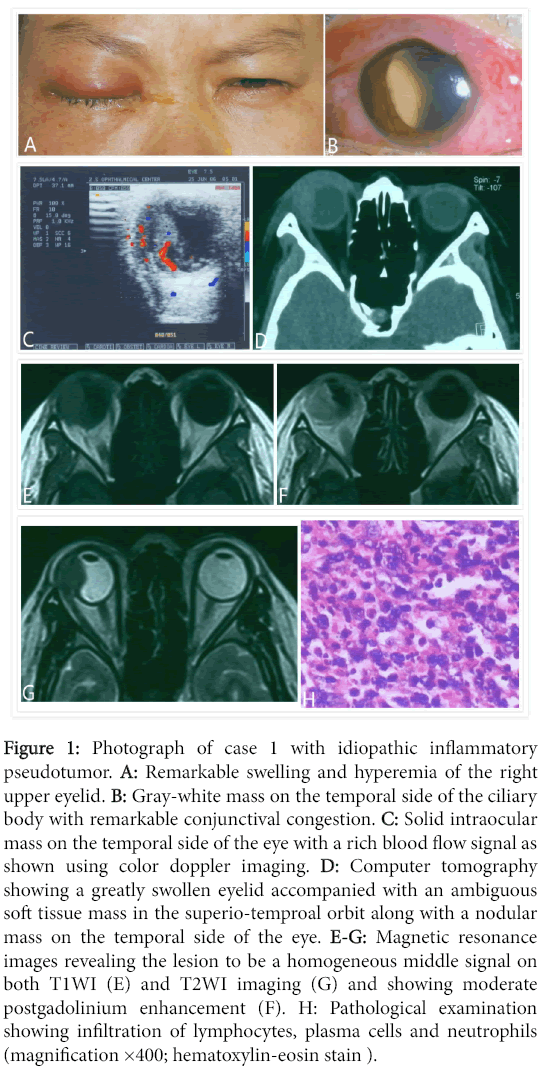
Case 1: A 36-year-old female presented with an aggressive, gradually swollen eyelid, reduced vision and right eye pain for 1.5 months. A remarkable swelling and hyperemia of the right upper eyelid and conjunctiva were present. A diffuse, rigid, ill-defined and tender mass was palpable in the superio-temporal orbit, together with a gray-white mass on the temporal side of the ciliary body. Computer tomography showed that the greatly swollen eyelid was accompanied with an ambiguous soft tissue mass in the superio-temproal orbit, along with a nodular mass on the temporal side of the eye (Figure 1).
Figure 1: Photograph of case 1 with idiopathic inflammatory pseudotumor. A: Remarkable swelling and hyperemia of the right upper eyelid. B: Gray-white mass on the temporal side of the ciliary body with remarkable conjunctival congestion. C: Solid intraocular mass on the temporal side of the eye with a rich blood flow signal as shown using color doppler imaging. D: Computer tomography showing a greatly swollen eyelid accompanied with an ambiguous soft tissue mass in the superio-temproal orbit along with a nodular mass on the temporal side of the eye. E-G: Magnetic resonance images revealing the lesion to be a homogeneous middle signal on both T1WI (E) and T2WI imaging (G) and showing moderate postgadolinium enhancement (F). H: Pathological examination showing infiltration of lymphocytes, plasma cells and neutrophils (magnification ×400; hematoxylin-eosin stain ).
Magnetic resonance imaging revealed the lesion to be a middle signal on both T1WI and T2WI imaging, with moderate postgadolinium enhancement. No appreciable therapeutic effects were observed following systemic corticosteroid and antibiotic administrations. Enucleation and biopsy of the orbital mass was performed. The pathological examination showed infiltrations of lymphocytes, plasma cells and neutrophils, supporting the diagnosis of idiopathic inflammatory pseudotumor involving both eye and orbit. At one month post-surgery, the patient received local administration of 20GY radiotherapy with no recurrence after a one year follow-up.
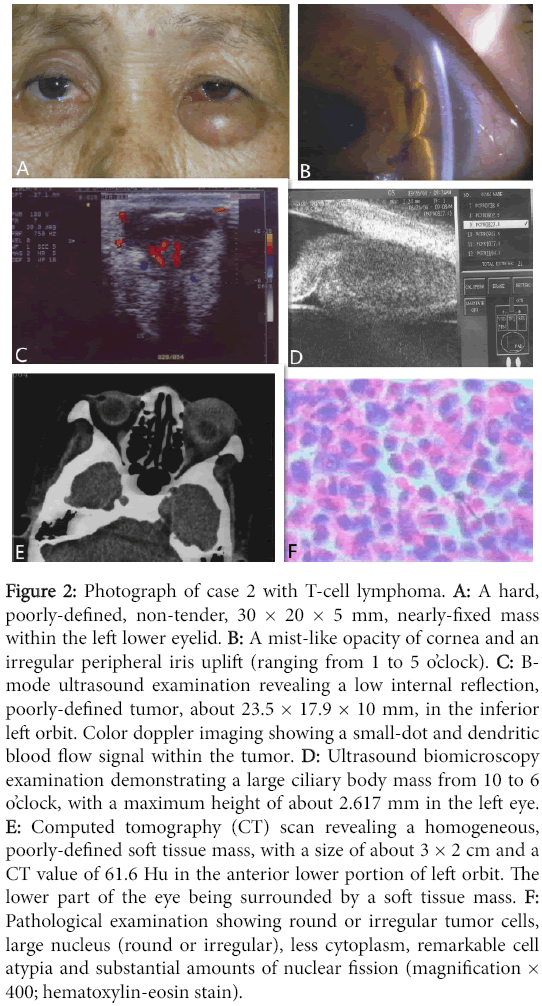
Case 2: A 71-year-old female patient experiencing blurred vision in her left eye for two months and the emergence of a left “lower eyelid” mass within the current month of her referral (Figure 2).
Figure 2: Photograph of case 2 with T-cell lymphoma. A: A hard, poorly-defined, non-tender, 30 × 20 × 5 mm, nearly-fixed mass within the left lower eyelid. B: A mist-like opacity of cornea and an irregular peripheral iris uplift (ranging from 1 to 5 o’clock). C: Bmode ultrasound examination revealing a low internal reflection, poorly-defined tumor, about 23.5 × 17.9 × 10 mm, in the inferior left orbit. Color doppler imaging showing a small-dot and dendritic blood flow signal within the tumor. D: Ultrasound biomicroscopy examination demonstrating a large ciliary body mass from 10 to 6 o’clock, with a maximum height of about 2.617 mm in the left eye. E: Computed tomography (CT) scan revealing a homogeneous, poorly-defined soft tissue mass, with a size of about 3 × 2 cm and a CT value of 61.6 Hu in the anterior lower portion of left orbit. The lower part of the eye being surrounded by a soft tissue mass. F: Pathological examination showing round or irregular tumor cells, large nucleus (round or irregular), less cytoplasm, remarkable cell atypia and substantial amounts of nuclear fission (magnification × 400; hematoxylin-eosin stain).
There was a hard, poorly-defined, non-tender 30 × 20 × 5 mm, nearly-fixed mass within the left lower eyelid. The cornea showed a mist-like opacity. There was an irregular peripheral iris elevation (ranging from 1 to 5 o’clock). Ultrasound biomicroscopy examination revealed a large ciliary body mass in the left eye from 10 to 6 o’clock, with a maximum height of about 2.617 mm. A homogeneous, poorlydefined soft tissue mass about 3 × 2 cm located in the lower, anterior portion of the left orbit was identified with computed tomography scan. An incisional biopsy of the left orbital tumor was performed with the patient under local anesthesia. The tumor tissue had the texture of fresh fish-like material, was gray-white, hard, brittle, ill-defined and bled profusely. Pathological examination confirmed the diagnosis of a T-cell lymphoma.
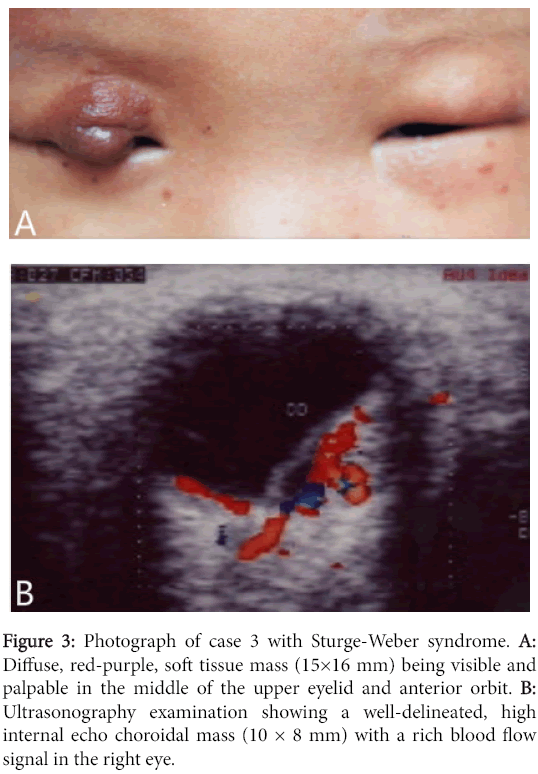
Case 3: A 2-year-old male was referred because of a “red tumor” in the right eye that was present since birth. The tumor enlarged with the growth of the child. No similar lesions were present on other skin areas. A diffuse, red-purple, soft tissue mass (15 × 16 mm) was visible and palpable in the middle portion of the upper eyelid and anterior orbit. Ultrasonography examination showed a well-delineated, high internal echo choroidal mass (10 × 8 mm) with a rich blood flow signal in the right eye. The child was diagnosed with Sturge-Weber syndrome. His parents refused any treatment, believing that the lesion was attributable to “God” and the patient was lost to follow-up (Figure 3).
Figure 3: Photograph of case 3 with Sturge-Weber syndrome. A: Diffuse, red-purple, soft tissue mass (15×16 mm) being visible and palpable in the middle of the upper eyelid and anterior orbit. B: Ultrasonography examination showing a well-delineated, high internal echo choroidal mass (10 × 8 mm) with a rich blood flow signal in the right eye.
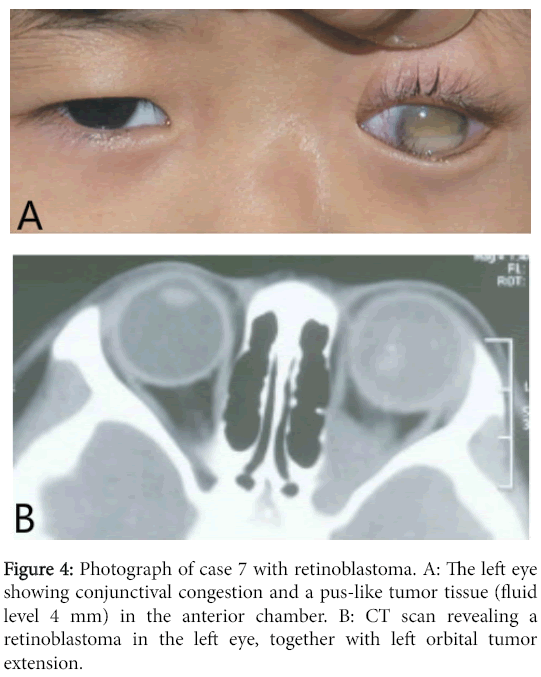
Cases 4-8: These consisted of children with intraocular retinoblastoma combined with orbital extension. Briefly, case 4 was a 3-year-old male referred with a one-year history of bilateral “whitish eye” that was diagnosed as retinoblastoma. His parents refused any treatment. Within the past month of his referral, his left eye enlarged and reddened. CT scan revealed that the tumor remained within the eye of the right eye while the tumor of the left eye extended into the orbit protruding posteriorly to the optic chiasm. The diagnosis was bilateral retinoblastoma with orbital extension and intracranial metastasis. Local and systemic chemotherapy were administered to control eye pain. The child died 6 months later. Case 5 was a 3-year-old female experiencing “pain and reddening” of the left eye that were present for two weeks. Results of her eye examination indicated left conjunctival hyperemia, corneal edema and a shallow anterior chamber. B-mode ultrasound and CT scans showed bilateral retinoblastoma, combined with left orbital tumor extension and intracranial metastasis. She was referred for systemic chemotherapy and died 4 months later. Case 6 was a 2-year-old male experiencing bilateral “white eye” for 6 months and two large bilateral orbital tumors for 12 months. CT scan revealed bilateral retinoblastoma with remarkable orbital extensions. He received systemic chemotherapy and died 6 months later. Case 7 (Figure 4) was a 3-year-old male with “white eye” for one year and “pain and redness” in the left eye for 2 weeks. Eye examination results indicated that left eye vision was no light perception and intraocular pressure was high.
A remarkable conjunctival congestion and pus-like tumor tissue (fluid level 4 mm) were present in the anterior chamber. B-mode ultrasound and CT scans revealed a retinoblastoma in the left eye, combined with left orbital tumor extension. Orbital evisceration was performed, however, his parents refused postoperative radiotherapy and he died of intracranial metastasis 2 years later. Case 8 was 22- month-old female experiencing bilateral “white eye” since 1 month after birth. Bilateral retinoblastoma was diagnosed but her parents refused any treatment. Her right eye became “reddened and enlarged” at 6 months followed by a reduction in size and atrophy. She also experienced “redness and pain” in her right eye 2 months prior. Bmode ultrasound and CT scans showed retinoblastoma in the left eye, combined with left orbital tumor extensions. Orbital evisceration was performed but postoperative radiotherapy was refused and she died of intracranial metastasis 1 year later.
Discussion
Idiopathic orbital inflammatory pseudotumor (IOIP) is the third most common cause of unilateral exophthalmos in adults, accounting for 5-20% of orbital biopsies [3,7]. The exact etiology is unknown but may be related to an autoimmune disorder. It can involve a variety of orbital tissues including lacrimal gland (dacryoadenitis), periscleral tendon’s capsule (periscleritis), orbital fat (optic perineuritis) and extraocular muscles (myositis). Due to the robust nature of the cornea and sclera, the eye is usually not affected by IOIP. Currently, there exists no previous report of inflammatory pseudotumor involving both the orbit and eye of which we are aware. Medical records of 209 IOIP cases at the Zhongshan Ophthalmic Center of Sun Yet-sen University, China, were reviewed between the periods of Jan 1,1978 and Dec 31,1999 with no patient demonstrating both orbital and eye involvement [8,9]. With regard to an IOIP involving both the orbit and eye, our cases were particularly unique in that we found that the lateral rectus muscle and temporal sclera of the right eye were severely affected. Glucocorticoids represent the first treatment of choice for IOIP. If glucocorticoids prove ineffective or contraindicated due to severe side effects, immunosuppressants and low-dose radiotherapy can be considered. Surgical management is suitable for patients whose lesions lie within the anterior orbit and show an unambiguous mass with a well-defined border.
Lymphoma is the most common malignant tumor of the orbit in adults, most often involving low-grade B-cell activity [10]. Either one or both orbits may be affected. However, intraocular lymphoma is rare, often involving high-grade diffuse large B-cell activity and can be regarded as an aspect of primary central nervous system lymphoma [10,11]. Coexistence of orbital and intraocular lymphoma is extremely rare. A review of 110 medical records of lymphoma from the Zhongshan Ophthalmic Center of Sun Yet-sen University, China, between Jan 1,1978 and Dec 31,1999 failed to identify any patients demonstrating both orbital and eye involvement [8]. Currently, only one report of lymphoma involving both the orbit and eye and classified as a B-cell phenotype has been reported in the literature [12]. Here, to the best of our knowledge, we present the first report of a T-cell lymphoma involving both the orbit and eye. In light of the patient’s orbital lymphoma and the solitary ciliary body mass, a presumptive diagnosis of intraocular lymphoma was made in this case. Commonly, orbital lymphoma can be managed with radiotherapy alone using a dose of 30-40 Gy or radiotherapy combined with systemic chemotherapy, protocols which result in very high cure rates. The management of primary intraocular lymphoma consists of an initial high-dose chemotherapy, followed by whole brain and orbital radiotherapy [10]. Cure rates are less than 50%. Our case was referred to the Tumor Hospital for more extensive systemic oncological evaluation and offered local radiotherapy and systemic chemotherapy, but was lost to follow-up.
Vascular malformations such as the Sturge-Weber syndrome (SWS) of our case 3 may show both choroidal hemangioma and orbital lymphoangioma [13,14]. SWS, a neurocutaneous syndrome, characterized by a facial port-wine stain extending to the first branch of the trigeminal nerve, results in ophthalmologic abnormalities (choroidal hemangioma and glaucoma) and neurologic signs (ipsilateral leptomeningeal angioma, seizure, mental retardation). In some patients this can be accompanied by orbital hemangioma. Though recurrence is frequent, pulsed dye laser is the standard treatment for the port-wine stain.
Retinoblastoma is the most common intraocular malignant tumor in children with about two-thirds of these cases occurring before the end of their third year. Such retinoblastomas usually remain undetected until they grow large enough to produce a white pupil or result in “redness and pain” of the involved eye due to secondary glaucoma. Retinoblastoma often spreads through the optic nerve and orbital tissues, therefore, it is common to see concomitant intraocular and orbital space-occupied lesions in patients with advanced retinoblastoma, like that observed in this study. Highly individualized aggressive treatments involving a combination of radical surgery, chemotherapy and external beam radiation therapy is required for cases with orbital retinoblastoma (International Retinoblastoma Staging System stage III) and extra-orbital metastatic retinoblastoma [15,16]. However, due to poor compliance and the advanced stage of the disease, very high mortality rates occur, in spite of the use of combining treatment regimens [17]. It should be noted that retinoblastoma represents a very rare human malignancy where definitive treatment can be started without any confirmed histopathological diagnosis, as imaging plays an important role in the corrective diagnosis of this condition.
In clinical practice supplementary space-occupied disorders that might involve both intraocular and orbital tissues require consideration. Some examples may include: (1) Wegener’s granuloma, a condition which may also result in the destruction of the eye wall and involves both the orbit and eye. However, upon pathological examination, this condition manifests typical characteristics of vasculitis, granulomatous inflammation and tissue necrosis, (2) Orbital cellulites and abscess can also present as space-occupying masses within orbital and intraocular regions. Both demonstrate signs of acute infectious inflammation, with most originating from the sinuses and include pain, eyelid swelling, chemosis of conjunctiva, high fever and increased blood leukocyte levels, (3) Extraocular extensions or secondary orbital inflammation of other intraocular malignant tumors, such as choroidal melanoma [18]. Choroidal melanoma often presents as a black spherical or mushroom-shaped intraocular mass. Uveal melanoma rarely metastasizes to the contralateral orbit, (4) Orbital malignant tumors involving the eye. Notably, malignant lacrimal gland tumors and other orbital malignancies may also manifest as symptoms of the orbit and eye, (5) A small subset of patients with Erdheim- Chester disease, neurofibroma or myofibroblastoma may also show both unilateral/bilateral orbital space-occupying lesions and intraocular lesions [19-21], (6) Simultaneous orbital and intraocular metastasis. While most patients with systemic cancer have metastasis to either the orbit or eye, a few may show both orbital and intraocular metastasis [5,22,23].
In summary, based upon the findings of this study, the presence of a lesion involving both the orbit and eye should include a consideration of retinoblastoma, idiopathic inflammatory pseudotumor, lymphoma, and/or Sturge-Weber syndrome.
References
- Villegas VM, Hess DJ, Wildner A, Gold AS, Murray TG (2013) Retinoblastoma. CurrOpinOphthalmol 24: 581-588.
- Shields CL, Manalac J, Das C, Ferguson K, Shields JA (2014) Choroidal melanoma: clinical features, classification, and top 10 pseudomelanomas. CurrOpinOphthalmol 25: 177-185.
- Rootman J: Inflammatory diseases (2003) In: Rootman J (ed), Diseases of the Orbit, a multidisciplinary approach, 2nd edition. Philadelphia: Lippincott Williams & Wilkins, pp 455-506.
- Savino G, Petroni S, Balia L, Caputo CG, Battendieri R, et al. (2013) Secondary orbital and intraocular lymphoma treated with immunochemotherapy. Retin Cases Brief Rep 7: 267-270.
- Buys R, Abramson DH, Kitchin FD, Gottlieb F, Epstein M (1982) Simultaneous ocular and orbital involvement from metastatic bronchogenic carcinoma. Ann Ophthalmol 14: 1165-1167, 1170-1.
- Yan J, Zhou S, Li Y (2012) Benign orbital tumors with bone destruction in children. PLoS One 7: e32111.
- Gordon LK (2006) Orbital inflammatory disease: a diagnostic and therapeutic challenge. Eye (Lond) 20: 1196-1206.
- Yan J, Wu Z, Li Y (2004) The differentiation of idiopathic inflammatory pseudotumor from lymphoid tumors of orbit: analysis of 319 cases. Orbit 23: 245-254.
- Yan J, Qiu H, Wu Z, Li Y (2006) Idiopathic orbital inflammatory pseudotumor in Chinese children. Orbit 25: 1-4.
- Woolf DK, Ahmed M, Plowman PN (2012) Primary lymphoma of the ocular adnexa (orbital lymphoma) and primary intraocular lymphoma. ClinOncol (R CollRadiol) 24: 339-344.
- Loriaut P, Charlotte F, Bodaghi B, Decaudin D, Leblond V, et al. (2013) Choroidal and adnexal extranodal marginal zone B-cell lymphoma: presentation, imaging findings, and therapeutic management in a series of nine cases. Eye (Lond) 27:828-835.
- Neudorfer M, Kessler A, Anteby I, Goldenberg D, Barak A (2004) Co-existence of intraocular and orbital lymphoma. ActaOphthalmolScand 82: 754-761.
- MartÃnez-Gutiérrez J, López-Lancho R, Pérez-Blázquez E (2008) [Angiomatous choroidal and orbital lesions in a patient with Sturge Weber syndrome]. Arch SocEspOftalmol 83: 429-431.
- Vavvas D, Fay A, Watkins L (2004) Two cases of orbital lymphangioma associated with vascular abnormalities of the retina and iris. Ophthalmology 111: 189-192.
- Radhakrishnan V, Kashyap S, Pushker N, Sharma S, Pathy S, et al. (2012) Outcome, pathologic findings, and compliance in orbital retinoblastoma (International Retinoblastoma Staging System stage III) treated with neoadjuvant chemotherapy: a prospective study. Ophthalmology. 119:1470-1477.
- Kiratli H, Bilgiç S, Ozerdem U (1998) Management of massive orbital involvement of intraocular retinoblastoma. Ophthalmology 105: 322-326.
- Leal-Leal CA, Rivera-Luna R, Flores-Rojo M, Juárez-Echenique JC, Ordaz JC, et al. (2006) Survival in extra-orbital metastatic retinoblastoma:treatment results. ClinTranslOncol 8: 39-44.
- Blasi MA, Giammaria D, Balestrazzi E (2006) Necrotic uveal melanoma with orbital inflammation. Eur J Ophthalmol 16: 647-650.
- BiccasNeto L, Zanetti F (2007) [Intraocular involvement in Erdheim-Chester disease--first report in the literature: case report]. Arq Bras Oftalmol 70: 862-867.
- Yazici B, Özgün G, Adim SB (2014) Choroidal ganglioneuroma in a patient with orbitopalpebral neurofibromatosis. OphthalPlastReconstrSurg 30: e140-142.
- Costin BR, Plesec TP, Rubinstein TJ, Medina CA, Singh AD, et al. (2014) Orbital and intraocular myofibroblastoma. Orbit 33: 202-205.
- Kiratli H, Soysal HG, Demir S (2004) Orbital metastasis and intraocular invasion of malignant mixed tumor (carcinosarcoma) of the parotid gland in a child. Arch Ophthalmol 122: 114-118.
- Kiratli H, Uzun S, Tarlan B, Ates D, Baydar DE, et al. (2015) Renal Carcinoid Tumor Metastatic to the Uvea, Medial Rectus Muscle, and the Contralateral Lacrimal Gland. OphthalPlastReconstrSurg31: e91-93.
Citation: Yan J, Shen T, Chen J (2016) Concomitant Intraocular and Orbital Space-Occupied Lesions. Optom open access 1: 109. DOI: 10.4172/2476-2075.1000109
Copyright: © 2016 Yan J, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 12897
- [From(publication date): 6-2016 - Apr 07, 2025]
- Breakdown by view type
- HTML page views: 11956
- PDF downloads: 941