Concomitant Injuries in Chronic Ankle Instability
Received: 24-Oct-2018 / Accepted Date: 15-Nov-2018 / Published Date: 22-Nov-2018 DOI: 10.4172/2329-910X.1000281
Abstract
Chronic ankle instability is associated with a number of coincident injuries about the ankle joint. Improvements in ankle arthroscopy and preoperative imaging modalities have aided in the identification and treatment of these lesions. Although their clinical significance may be variable, the presence of concomitant lesions in chronic ankle instability predisposes patients to chronic pain and osteoarthritis. A comprehensive review of the literature reveals that a multitude of studies have described associated lesions in patients with chronic ankle instability. These lesions include peroneal tendon injuries, chondral and osteochondral lesions of the tibial plafond and talar dome, intraarticular loose bodies, anterior/anterolateral ankle soft tissue impingement, lateral malleolus ossicles, tibiofibular syndesmosis injuries, and peroneal nerve injuries. This review serves as a comprehensive analysis of the literature, focusing on identification, treatment, and long-term outcomes of concomitant injuries in chronic ankle instability.
Keywords: Ankle; Instability; Arthroscopy; Peroneal; Osteochondral; Impingement; Sports; Tendon disorders trauma; Instability; Arthroscopy
Level of Evidence
Level V, review article
Introduction
Chronic ankle instability (CAI) occurs in individuals with a history of at least one prior ankle sprain resulting in chronic laxity of the ligaments surrounding the ankle joint [1,2]. Lateral ankle sprains are the most common injury in sports, resulting typically from excessive inversion, plantarflexion, and internal rotation of the ankle [3]. Lateral ankle sprains are most commonly due to injury to the anterior talofibular ligament (ATFL), and less commonly the calcaneofibular ligament (CFL) or posterior talofibular ligament (PTFL) which completes the lateral ankle ligament complex. Injuries to the deltoid ligament and subsequent medial ankle instability are rare [4].
Due to the frequency of the injury and the perception of ankle sprains as being minor injuries, a majority of patients with an acute ankle sprain do not seek medical care which may lead to increased residual symptoms such as chronic ankle instability [1,5]. Ankle instability can be described as mechanical instability (pathologic laxity of the ligaments in the ankle) or functional instability (insufficiency in proprioception/ neuromuscular control) [6,7].
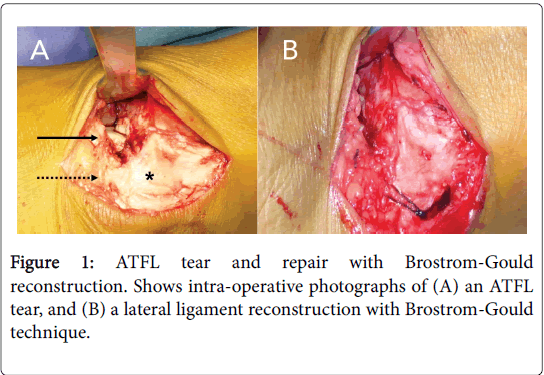
Chronic ankle instability has been estimated to occur in 10 to 20 percent of patients who sustain an acute ankle sprain [8]. A majority of patients with chronic ankle instability continue to have instability with conservative management and a small subset will have chronic pain and progress with osteoarthritis of the ankle joint [9]. Advances in lateral ankle ligament reconstruction in the past 50 years, specifically with the Brostrom and Brostrom-Gould techniques, have improved clinical results with surgery (Figure 1) [10-12].
However, 13 to 35 percent of patients have persistent pain and symptoms after a successful lateral ligament reconstruction which some attribute to concomitant intraarticular lesions [13,14]. Improvements in preoperative imaging modalities, specifically magnetic resonance imaging (MRI), have aided in more accurately identifying these lesions prior to surgery. Prior to the rise in prevalence of ankle arthroscopy, intraarticular lesions were evaluated through an open ankle arthrotomy which has limited visualization and increased morbidity compared to arthroscopy.
The ability to identify and treat concomitant lesions in chronic ankle instability has improved, and their role in functional outcomes are significant. The most frequently encountered lesions include peroneal tendon injuries, osteochondral lesions of the tibia and talus, chondral injuries and chondromalacia, intraarticular loose bodies, anterior and anterolateral ankle impingement, lateral malleolus ossicles, syndesmosis widening, and peroneal nerve injuries.
A majority of the current literature looking at concomitant injuries in chronic ankle instability is primarily retrospective case series and cohorts. The prevalent studies are highlighted in detail in the following manuscript. To our knowledge, this is the first comprehensive review of the literature highlighting the diagnosis, frequency, clinical significance, and treatments for all injuries associated with chronic ankle instability.
Review
Diagnosis
One of the first large case series to study associated injuries in patients with CAI was by DiGiovanni, et al. which was a retrospective review of 61 patients with chronic ankle instability that underwent lateral ligament reconstruction and open ankle arthrotomy. The authors found a number of associated injuries about the ankle joint. These injuries and their frequencies included: peroneal tenosynovitis (47/61, 77%), anterolateral impingement lesion (41/61, 67%), attenuated peroneal retinaculum (33/61, 54%), ankle synovitis (30/61, 49%), loose bodies (16/61, 26%), peroneus brevis tear (15/61, 25%), osteochondral lesion of the talus (14/61, 23%), ATFL avulsion (7/61, 11%), accessory peroneus quartus muscle (5/61, 8%), medial ankle tendon tenosynovitis (3/61, 5%), and capsular avulsion fracture (2/61, 3%). One hundred percent of patients had at least one associated injury [15]. This study demonstrates that a variety of concomitant injuries are associated with CAI, and they are present in the vast majority of patients.
Similarly, Strauss, et al. looked at 180 ankles in 160 patients undergoing modified Brostrom-Gould lateral ankle ligament reconstruction for chronic ankle instability. In this cohort, the authors reviewed physical examination, clinical history, radiographs, and intraoperative findings to find the incidence of concomitant extraarticular lesions in CAI. They found that 64% of all patients had associated extra-articular conditions. These included peroneal tendon injuries (51/180, 28%), os trigonum lesions (23/180, 13%), lateral gutter ossicles (18/180, 10%), hindfoot varus malalignment (15/180, 8%), anterior tibial spurs (5/180, 3%), and tarsal coalitions (3/180, 2%) [16]. This study reported lower incidence of concomitant injuries, but there was no mention of intraarticular assessment with arthrotomy or arthroscopy. In addition to these injuries, anterior process fractures of the calcaneus can occur in conjunction with acute ankle sprains, and are at risk of misdiagnosis [17].
Magnetic resonance imaging
Diagnosis of concomitant lesion in chronic ankle instability was difficult prior to the increased utilization of MRI and arthroscopy. Improvements in MRI have allowed for more accurate diagnoses of lesions about the foot and ankle and help in the work up of chronic ankle pain. O’Neill, et al. found that preoperative MRI radiology reports identified 39% (15/38) of chondral injuries, 56% (10/18) of peroneal tears, and 57% (4/7) of loose bodies, with an overall sensitivity of 45% for detecting lesions that were visualized intraoperatively [18]. Additionally, the attending surgeon’s review of the MRI’s yielded identification of 47% (18/38) of chondral injuries, 89% (16/18) of peroneal tears, and 71% (5/7) of loose bodies with an overall sensitivity of 63%. The conclusion of the study was that while having the surgeon review the MRI improves preoperative diagnosis of concomitant injuries, MRI may not be adequate to detect lesions before surgery [18].
Cha et al. similarly compared preoperative MRI findings to intraoperative arthroscopy in patients who had surgery for chronic lateral ankle instability. The sensitivities for MRI in detecting each individual lesion were 60% for ATFL injury, 46% for osteochondral lesions of the talus (OLT), 21% for syndesmosis injury, 21% for synovitis, and 22% for anterior osteophyte impingement [19]. The low sensitivity and interobserver reliability of preoperative MRI tests prompted the authors of this study to strongly recommend arthroscopic examination in all cases to identify and treat concomitant injuries [19].
Arthroscopy
A multitude of case series and retrospective cohorts are present in the literature looking at the use of arthroscopy for diagnosis of concomitant injuries in chronic ankle instability. Ankle arthroscopy has increased the ability to accurately identify intraarticular ankle pathology while maintaining low long term morbidity to the patient [20]. The general consensus is that Intraarticular lesions associated with chronic ankle instability are common, and ankle arthroscopy is currently the gold standard in diagnosing the injuries.
Schafer et al. studied 110 consecutive patients prospectively with chronic ankle instability who underwent ankle arthroscopy. Arthroscopy identified 42 patients (38%) patients had synovialitis, 7 (6%) had ventral scarring, 11 (10%) had a synovial plica, 8 (7%) had syndesmosis injury, 59 (54%) had talar cartilage injuries, and 19 (17%) had distal tibial cartilage injuries. The ligamentous injuries included rupture of the ATFL in 64%, rupture of CFL in 41%, and deltoid ligament rupture in 6% [21]. Choi et al. looked at the arthroscopic findings in patients undergoing modified Brostrom procedure for chronic lateral ankle instability. This case series found that 97% (63/65) of ankles had associated intraarticular lesions. They included syndesmotic widening (19/65, 29%), osteochondral lesion (15/65, 23%), lateral malleolus ossicles (25/65, 38%), soft tissue impingement (53/65, 82%), and osteophyte formation (7/65, 11%).
The authors found that the postoperative outcome scores negatively correlated with the number of lesions, and syndesmotic widening, osteochondral lesions, and ossicles were independently predictors of poor outcome. Osteophyte formation and soft tissue impingement had no significant correlation [13]. Similarly, Hua, et al. found intraarticular lesions in 91% (79/87) of ankles undergoing arthroscopic evaluation prior to modified Brostrom procedure in a retrospective review. The lesions included synovitis/soft tissue impingement (75/87, 86%), chondral injury (33/87, 38%), anterior tibial osteophyte (23/87, 26%), loose bodies (7/87, 8%), and syndesmotic injury (6/87, 7%). Outcome scores at least 12 months postoperatively were significantly higher in patients without chondral lesions [22]. A number of additional case series have been performed looking at the incidence and outcomes of patients with concomitant intraarticular lesions in the setting of chronic ankle instability and are included in Table 1.
| Study(N) | Soft tissue impingement | Synovitis | Syndesmosis injury | Osteochondral lesions |
Chondral injury | Ossicles | Osteophytes | Loose bodies |
|---|---|---|---|---|---|---|---|---|
| Choi [13] (65) |
82% | NR | 29% | 23% | NR | 39% | 11% | NR |
| Schafer [21] (110) |
NR | 38% | 7% | NR | 54% | NR | NR | NR |
| Hua[22] (87) |
86% | NR | 6.90% | NR | 38% | NR | 26% | 8.00% |
| Ferkel [20] (21) |
NR | 76% | NR | 19% | 33% | 29% | 19% | 24% |
| Lee [23] (28) |
14% | 100% | NR | 7.10% | 39% | NR | 14% | 11% |
| Liszka [24] (25) |
NR | 75% | NR | NR | 56% | NR | 52% | 20% |
| Hinterman [25] (148) |
17% | 32% | 8.80% | NR | 54% | NR | 12% | NR |
| Komenda [26] (55) |
NR | 69% | NR | 16% | 22% | 25% | 11% | 22% |
| Odak [27] (100) |
NR | 63% | NR | 17% | NR | NR | 12% | 1.00% |
Table 1: Incidence of intra-articular lesions in patients with chronic ankle instability found on arthroscopy.
The overall incidence of associated intraarticular lesions is as high as 100 percent in several studies. Additionally, these studies identified the following associated intraarticular lesions with arthroscopy: Synovitis (range of incidence 32%-100%), soft tissue impingement (14%-86%), chondral injury (22%-56%), osteochondral lesion (7%-23%), lateral malleolus ossicle (25%-39%), anterior osteophyte (11%-52%), and intraarticular loose body (1%-24%) [12,22-28]. What can be concluded from these studies is that chronic ankle instability is associated with an extremely high prevalence of associated intraarticular pathology. In the hands of many surgeons, this evidence shows that arthroscopic evaluation of the ankle joint during lateral ligament reconstruction is indicated in all cases to identify intraarticular pathology. Preoperative imaging and examination may identify some associated pathology, but a significant number of intraarticular lesions will be missed without arthroscopic evaluation of the joint.
Specific Lesions: Diagnosis and Management
Peroneal tendon injuries
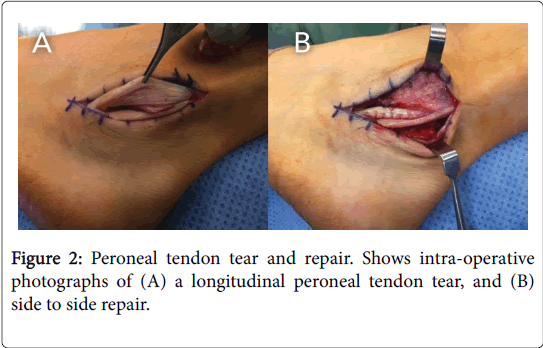
Peroneal tendon injuries, specifically peroneus brevis, are commonly seen in association with chronic ankle instability (Figure 2). The proposed mechanism is that laxity in the superior peroneal retinaculum allows for anterior slipping of the peroneus brevis tendon in the retrofibular groove. This causes the tendon to ride over the sharp posterior edge of the fibula, leading to longitudinal tears in the central tendon [29]. The incidence of peroneal tendon pathology in the setting of CAI is relatively common. A cadaveric study found an incidence of peroneal tears in 11% (14/124) of ankles with unknown history; however the clinical relevance of this number is unknown [30]. A clinical retrospective study found that 38% (31/82) of ankles operated on with chronic lateral ankle instability had peroneal tendinopathy and 13% (11/82) had frank peroneal tendon tears [31]. Most patients with a peroneal tendon injury will complain of retromalleolar pain and tenderness, and may present with clinical subluxation of the peroneal tendons with ankle circumduction. MRI is a useful tool in assisting with the diagnosis of peroneal tendinopathy with a sensitivity of 84% and specificity of 75% [31]. In assessing for peroneal tendinopathy in patients with CAI, one should utilize clinical history, physical examination, and imaging studies as well as thorough intraoperative assessment.
Conservative management of peroneal tendon tears is an option; however, in the setting of chronic lateral ankle instability and chronic ankle pain, operative management may be considered. Operative management with a simple debridement of the diseased split tendon and side to side repair is appropriate in cases with less than 50% tendon involvement and has been described with 90% good to excellent results [32,33]. In cases with greater than 50% tendon involvement, the surgeon must consider allograft augmentation or lateral ligament reconstruction utilizing the peroneus brevis tendon such as in a Chrisman-Snook procedure [34].
Osteochondral/chondral injuries
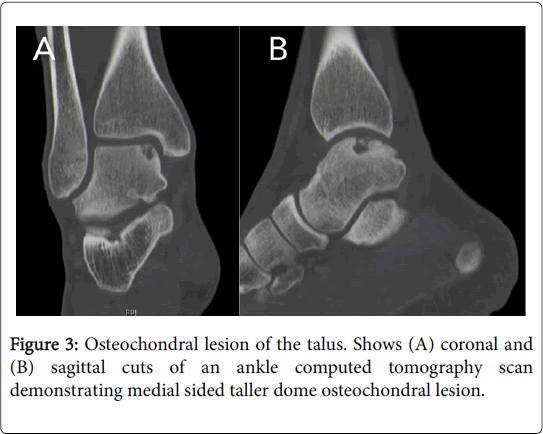
One of the most classically recognized lesions seen with chronic ankle instability is in the spectrum of chondral and osteochondral lesions of the talus (OLT) and the tibial plafond (Figure 3). These intraarticular lesions are a common source of pain in chronic ankle instability, and may be a precursor to posttraumatic ankle arthritis. The incidence of chondral injuries in CAI varies in the literature greatly from 22% to 95%. Osteochondral lesions are diagnosed less frequently in CAI with an incidence of 7% to 23% in the literature [13,23]. Taga et al. looked at 31 ankles with lateral ligament injury and found that eight out of nine freshly injured and 21 of 22 chronic injured ankles had cartilage injuries. The most common area of injury was the anteromedial edge of the tibial plafond. Chondral injuries greater than one half the thickness of the articular cartilage were only found in chronic instability patients, leading the authors to suggest that chondral injuries increase in severity over time [35]. In a more recent study by Sugimoto et al., cartilage injuries were graded in patients with CAI. The group found 23% (23/99) with normal cartilage, 35% (35/99) with grade one chondromalacia, 24% (24/99) with grade two, and 17% (17/99) with grade three. They also found a significant association between worse cartilage injury and increased patient age and talar tilt angle [36]. Deltoid ligament insufficiency is associated with a significantly higher rate of chondral injuries in patients compared to isolated lateral ankle instability [20,24].
When assessing medial versus lateral osteochondral lesions in the talus, it has been shown that lateral talar are nearly always traumatic in nature, while medial lesions are not necessarily. Furthermore, medial lesions typically present later, have more cystic changes, and have worse clinical outcomes than lateral lesions [37]. Nondisplaced osteochondral lesions can often be treated conservatively, although this is more successful in the pediatric population. Smaller lesions, typically less than 15 mm in diameter, respond well to bone marrow stimulation techniques such as microfracture drilling. Large cystic lesions may require more aggressive techniques such as osteochondral autograft or allografts, autologous chondrocyte implantation, and matrixassociated chondrocyte implantation [38].
The results of specific treatment techniques for osteochondral and chondral lesions in the ankle joint are out of the scope of this review; however, it has been shown that outcomes for OLTs in patients with chronic ankle instability are significantly worse than patients without CAI [39]. Unfortunately, the natural course for many patients with chronic ankle instability is worsening chondromalacia leading to posttraumatic osteoarthritis [40].
Lateral malleolus ossicles
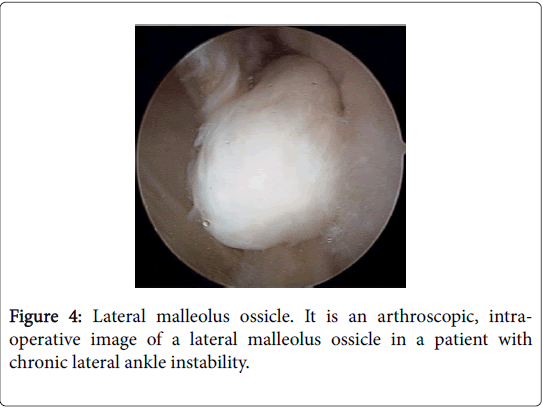
The presence of ossicles adjacent to the lateral malleolus in the setting of chronic lateral ankle instability are presumed to be from an avulsion of the tip of the lateral malleolus from pull of the CFL or ATFL most commonly (Figure 4). Ossicles typically are asymptomatic, but may be painful secondary to stress in the connection of the ossicle to the fibular tip [41]. The incidence of lateral malleolus ossicles in patients with CAI ranges from 25% to 38% in the literature.
Treatment in patients with symptomatic lateral malleolus ossicles is typically with ossicle resection and lateral ligament reconstruction. With a larger sized ossicle (greater than 10 mm), fibrous union takedown and ossicle fusion to fibular tip should be considered to prevent persistent anterior talar displacement [42]. The clinical significance of lateral malleolar ossicles in patients with CAI is mixed in the literature. Choi, et al. found that the presence of lateral malleolar ossicles independently predicted unsatisfactory results in patients undergoing lateral ligament reconstruction [13]. However, two other retrospective reviews showed no difference in clinical results when comparing patients with ossicle resection plus modified Brostrom procedure to patients with no ossicle at all [43,44].
Anterior ankle impingement
Anterior impingement is a common source of ankle pain, and is believed to be a direct consequence of chronic ankle instability in certain cases [45]. One study compared patients who underwent lateral ligament reconstruction to a cohort of normal ankles and found a 3.37 times increased incidence of anterior impingement spurs in the lateral ligament reconstruction group [46]. Anterior ankle impingement can be from osteophytes or soft tissue impingement and is seen clinically with restricted ankle dorsiflexion and anterior ankle pain. Osteophytes are present in 11% to 26% of chronic ankle instability cases according to the literature. Soft tissue impingement has a much broader incidence between studies, ranging between 14% and 82%. Bassett lesions can develop in CAI as a thickened cord in the anteroinferior tibiofibular ligament in response to recurrent ankle instability events and contribute to impingement as well [47].
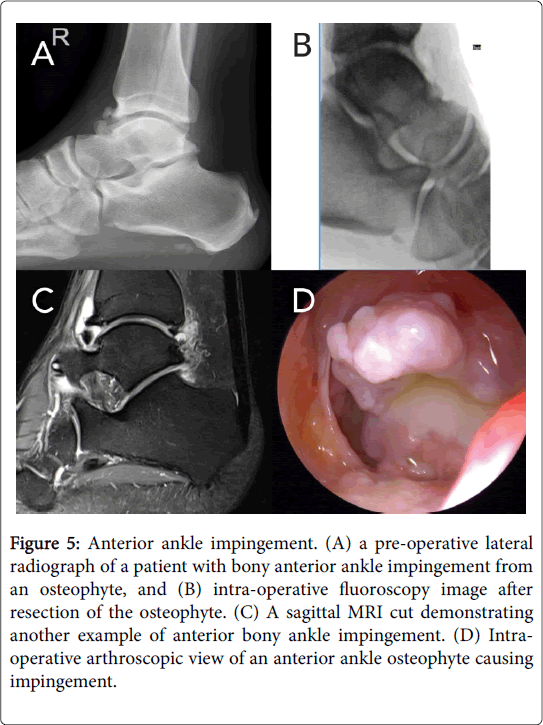
The diagnosis of anterior or anterolateral ankle impingement is typically with clinical examination, but MRI is a useful tool in diagnosis with 91.9% sensitivity and 84.4% specificity (Figure 5) [48]. Management of anterior impingement initially with conservative treatment may include activity modification, anti-inflammatory medications, physical therapy, bracing, and injections. With failure of conservative measures, operative intervention can be considered. The majority of anterior ankle impingement currently is treated with arthroscopic debridement. Recent studies have shown 90% to 97% good and excellent postoperative results with arthroscopic debridement of anterior ankle impingement in the setting of prior ankle instability event [49,50].
Figure 5: Anterior ankle impingement. (A) a pre-operative lateral radiograph of a patient with bony anterior ankle impingement from an osteophyte, and (B) intra-operative fluoroscopy image after resection of the osteophyte. (C) A sagittal MRI cut demonstrating another example of anterior bony ankle impingement. (D) Intraoperative arthroscopic view of an anterior ankle osteophyte causing impingement.
Syndesmosis injury
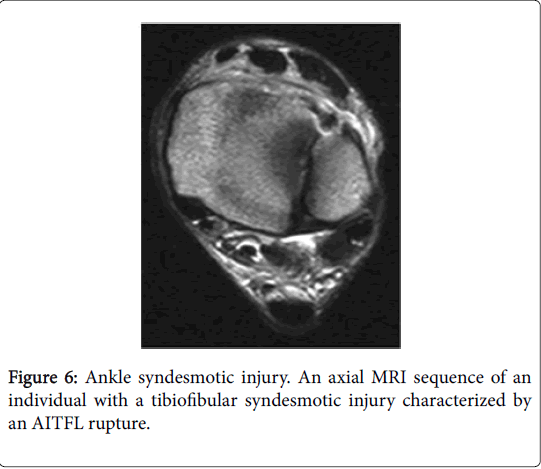
Ankle syndesmotic injuries can be associated with significant pain and morbidity in the ankle and often times are missed at the time of initial presentation of ankle sprains. A concomitant syndesmotic injury in a patient with CAI is an independent predictor of poor outcome [13]. A study by Takao et al. looked at different diagnostic tools in assessing for tibiofibular syndesmosis injuries. The authors found that MRI was significantly better at identifying syndesmosis injuries (sensitivity 100%, specificity 93.1% for anterior inferior tibiofibular ligament injury and 100%, 100% for posterior inferior tibiofibular ligament injury) compared to AP radiographs (44.1%, 100%) and mortise radiographs (58.3%, 100%) (Figure 6) [51]. In the chronic syndesmosis disruption, treatment with arthroscopic debridement alone typically is sufficient in providing pain relief, improved stiffness, and better ankle stability [52].
Peroneal nerve injury
Peroneal nerve injuries after ankle sprain are rare, but there are a number of case reports in the literature describing this injury. In the vast majority of cases, this occurs as a neuropraxic type injury at the time of ankle sprain and resolved with conservative management [53]. The insufficiency of the lateral ankle ligaments causes increased strain in the peroneal nerve. Although a rare injury, a case report described chronic peroneal nerve injury in the setting of recurrent lateral ankle instability events [54].
Conclusion
Concomitant injuries in chronic ankle instability are common sources of pain and morbidity for patients. Some of the most common injuries include osteochondral and chondral lesions, peroneal tendinopathy, syndesmotic injury, lateral malleolar ossicles, soft tissue and osteophyte impingement, and peroneal nerve injury. The incidence of these injuries is higher than many practitioners believe. Even with a thorough history and physical examination as well as cross-sectional imaging with MRI, a significant amount of these injuries are still missed preoperatively. The morbidity of missed concomitant injuries in chronic ankle instability is difficult to assess, and many surgeons recommend arthroscopic evaluation in all cases of ankle ligament reconstruction. Management of each individual lesion is different; therefore, one must be diligent in operative preparation for chronic ankle instability cases.
References
- Guillo S, Bauer T, Lee JW, Takao M, Kong SW, et al. (2013) Consensus in chronic ankle instability: Aetiology, assessment, surgical indications and place for arthroscopy. Orthop Traumatol Surg Res 99: 411-419.
- Konradsen L, Bech L, Ehrenbjerg M, Nickelsen T (2002) Seven years follow-up after ankle inversion trauma. Scand J Med Sci Sports 12: 129-135.
- Garrick JG (1977) The frequency of injury, mechanism of injury, and epidemiology of ankle sprains. Am J Sports Med 5: 241-242.
- Ferran NA, Oliva F, Maffulli N (2009) Ankle Instability. Sports Med Arthrosc 17: 139-145.
- McKay GD, Goldie PA, Payne WR, Oakes BW (2001) Ankle injuries in basketball: Injury rate and risk factors. Br J Sports Med 35: 103-108.
- Bonnel F, Toullec E, Mabit C, Tourné Y, Sofcot (2010) Chronic ankle instability: Biomechanics and pathomechanics of ligaments injury and associated lesions. Orthop Traumatol Surg Res 96: 424-432.
- Hertel J (2002) Functional anatomy, pathomechanics, and pathophysiology of lateral ankle instability. J Athl Train 37: 364-375.
- Karlsson J, Lansinger O (1992) Lateral instability of the ankle joint. Clin Orthop Relat Res 276: 253-261.
- Löfvenberg R, Kärrholm J, Lund B (1994) The outcome of nonoperated patients with chronic lateral instability of the ankle: A 20-year follow-up study. Foot ankle Int 15:165-169.
- Broström L (1966) Sprained ankles. VI. Surgical treatment of chronic ligament ruptures. Acta Chir Scand 132: 551-565.
- Gould N, Seligson D, Gassman J (1980) Early and late repair of lateral ligament of the ankle. Foot Ankle 1: 84-89.
- Hamilton WG, Thompson FM, Snow SW (1993) The modified brostrom procedure for lateral ankle instability. Foot Ankle 14: 1-7.
- Choi WJ, Lee JW, Han SH, Kim BS, Lee SK (2008) Chronic lateral ankle instability: The effect of intra-articular lesions on clinical outcome. Am J Sports Med 36: 2167-2172.
- Sammarco GJ, DiRaimondo CV (1988) Surgical treatment of lateral ankle instability syndrome. Am J Sports Med 16: 501-511.
- DIGiovanni BF, Fraga CJ, Cohen BE, Shereff MJ (2000) Associated injuries found in chronic lateral ankle instability. Foot ankle Int 21: 809-815.
- Strauss JE, Forsberg JA, Lippert FG (2007) Chronic lateral ankle instability and associated conditions: a rationale for treatment. Foot ankle Int 28: 1041-1044.
- Petrover D, Schweitzer ME, Laredo JD (2007) Anterior process calcaneal fractures: A systematic evaluation of associated conditions. Skeletal Radiol 36: 627-632.
- O’Neill PJ, Van Aman SE, Guyton GP (2010) Is MRI adequate to detect lesions in patients with ankle instability? Clin Orthop Relat Res 468: 1115-1119.
- Cha S Do, Kim HS, Chung ST, Yoo JH, Park JH, et al. Intra-articular lesions in chronic lateral ankle instability: comparison of arthroscopy with magnetic resonance imaging findings. Clin Orthop Surg 4: 293-299.
- Ferkel RD, Small HN, Gittins JE (2001) Complications in foot and ankle arthroscopy. Clin Orthop Relat Res 391: 89-104.
- Schäfer D, Hintermann B (1996) Arthroscopic assessment of the chronic unstable ankle joint. Knee Surg Sports Traumatol Arthrosc 4: 48-52.
- Hua Y, Chen S, Li Y, Chen J, Li H (2010) Combination of modified broström procedure with ankle arthroscopy for chronic ankle instability accompanied by intra-articular symptoms. Arthroscopy 26: 524-528.
- Lee J, Hamilton G, Ford L (2011) Associated intra-articular ankle pathologies in patients with chronic lateral ankle instability: Arthroscopic findings at the time of lateral ankle reconstruction. Foot Ankle Spec 4: 284-289.
- Liszka H, Depukat P, GÄ…dek A (2016) Intra-articular pathologies associated with chronic ankle instability. Folia Med Cracov 56: 95-100.
- Hintermann B, Boss A, Schäfer D (2002) Arthroscopic findings in patients with chronic ankle instability. Am J Sports Med 30: 402-409.
- Komenda GA, Ferkel RD (1999) Arthroscopic findings associated with the unstable ankle. Foot ankle Int 20: 708-713.
- Odak S, Ahluwalia R, Shivarathre DG, Mahmood A, Blucher N, et al. (2015) Arthroscopic evaluation of impingement and osteochondral lesions in chronic lateral ankle instability. Foot ankle Int 36: 1045-1049.
- Ferkel RD, Chams RN (2007) Chronic lateral instability: Arthroscopic findings and long-term results. Foot ankle Int 28: 24-31.
- Sobel M, Geppert MJ, Olson EJ, Bohne WH, Arnoczky SP (1992) The dynamics of peroneus brevis tendon splits: A proposed mechanism, technique of diagnosis, and classification of injury. Foot Ankle 13: 413-422.
- Sobel M, Bohne WH, Levy ME (1990) Longitudinal attrition of the peroneus brevis tendon in the fibular groove: An anatomic study. Foot Ankle 11: 124-128.
- Park HJ, Cha SD, Kim HS, Chung ST, Park NH, et al. (2010) Reliability of MRI findings of peroneal tendinopathy in patients with lateral chronic ankle instability. Clin Orthop Surg 2: 237-243.
- Demetracopoulos CA, Vineyard JC, Kiesau CD, Nunley JA (2014) Long-term results of debridement and primary repair of peroneal tendon tears. Foot ankle Int 35: 252-257.
- Karlsson J, Brandsson S, Kälebo P, Eriksson BI (1998) Surgical treatment of concomitant chronic ankle instability and longitudinal rupture of the peroneus brevis tendon. Scand J Med Sci Sports 8: 42-49.
- Bonnin M, Tavernier T, Bouysset M (1997) Split lesions of the peroneus brevis tendon in chronic ankle laxity. Am J Sports Med 25: 699-703.
- Taga I, Shino K, Inoue M, Nakata K, Maeda A (1993) Articular cartilage lesions in ankles with lateral ligament injury. An arthroscopic study. Am J Sports Med 21: 120-126.
- Sugimoto K, Takakura Y, Okahashi K, Samoto N, Kawate K, et al. (2009) Chondral injuries of the ankle with recurrent lateral instability: An arthroscopic study. J Bone Joint Surg Am 91: 99-106.
- Robinson DE, Winson IG, Harries WJ, Kelly AJ (2003) Arthroscopic treatment of osteochondral lesions of the talus. J Bone Joint Surg Br 85: 989-993.
- Looze CA, Capo J, Ryan MK, Begly JP, Chapman C, et al. (2017) Evaluation and management of osteochondral lesions of the talus. Cartilage 8: 19-30.
- Lee M, Kwon JW, Choi WJ, Lee JW (2015) Comparison of outcomes for osteochondral lesions of the talus with and without chronic lateral ankle instability. Foot ankle Int 36: 1050-1057.
- Harrington KD (1979) Degenerative arthritis of the ankle secondary to long-standing lateral ligament instability. J Bone Joint Surg Am 61: 354-361.
- Hasegawa A, Kimura M, Tomizawa S, Shirakura K (1996) Separated ossicles of the lateral malleolus. Clin Orthop Relat Res 330: 157-165.
- Kim BS, Choi WJ, Kim YS, Lee JW (2010) The effect of an ossicle of the lateral malleolus on ligament reconstruction of chronic lateral ankle instability. Foot ankle Int 31: 191-196.
- Ahn HW, Lee KB (2016) Comparison of the modified broström procedure for chronic lateral ankle instability with and without subfibular ossicle. Am J Sports Med 44: 3158-3164.
- Chun TH, Park YS, Sung KS (2013) The effect of ossicle resection in the lateral ligament repair for treatment of chronic lateral ankle instability. Foot ankle Int 34: 1128-1133.
- Cannon LB, Hackney RG (200) Anterior tibiotalar impingement associated with chronic ankle instability. J Foot Ankle Surg 39: 383-386.
- Scranton PE, McDermott JE, Rogers JV (2000) The relationship between chronic ankle instability and variations in mortise anatomy and impingement spurs. Foot ankle Int 21: 657-664.
- Bassett FH, Gates HS, Billys JB, Morris HB, Nikolaou PK (1990) Talar impingement by the anteroinferior tibiofibular ligament. A cause of chronic pain in the ankle after inversion sprain. J Bone Joint Surg Am 72: 55-59.
- Lee JW, Suh JS, Huh YM, Moon ES, Kim SJ (2004) Soft tissue impingement syndrome of the ankle: diagnostic efficacy of MRI and clinical results after arthroscopic treatment. Foot ankle Int 25: 896-902.
- DeBerardino TM, Arciero RA, Taylor DC (1997) Arthroscopic treatment of soft-tissue impingement of the ankle in athletes. Arthroscopy 13: 492-498.
- Urgüden M, Söyüncü Y, Ozdemir H, Sekban H, Akyildiz FF, et al. (2005) Arthroscopic treatment of anterolateral soft tissue impingement of the ankle: Evaluation of factors affecting outcome. Arthroscopy 21: 317-322.
- Takao M, Ochi M, Oae K, Naito K, Uchio Y (2003) Diagnosis of a tear of the tibiofibular syndesmosis. The role of arthroscopy of the ankle. J Bone Joint Surg Br 85: 324-329.
- Ogilvie-Harris DJ, Reed SC (1994) Disruption of the ankle syndesmosis: Diagnosis and treatment by arthroscopic surgery. Arthroscopy 10: 561-568.
- Mitsiokapa E, Mavrogenis AF, Drakopoulos D, Mauffrey C, Scarlat M (2017) Peroneal nerve palsy after ankle sprain: An update. Eur J Orthop Surg Traumatol 27: 53-60.
- Benchortane M, Collado H, Coudreuse JM, Desnuelle C, Viton J-M, et al. (2011) Chronic ankle instability and common fibular nerve injury. Joint Bone Spine 78: 206-208.
Citation: D’Hooghe P, Joyce CD, Hunt KJ, Kaux JF (2018) Concomitant Injuries in Chronic Ankle Instability. Clin Res Foot Ankle 6: 281. DOI: 10.4172/2329-910X.1000281
Copyright: © 2018 D’Hooghe P, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 4427
- [From(publication date): 0-2015 - Apr 05, 2025]
- Breakdown by view type
- HTML page views: 3596
- PDF downloads: 831