Comprehensive Diagnostic Workup for Cervical Cancer: Evaluation of Medical History, Physical Examination, and Diagnostic Tests
Received: 01-May-2023 / Manuscript No. jcd-23-98850 / Editor assigned: 04-May-2023 / PreQC No. jcd-23-98850 / Reviewed: 18-May-2023 / QC No. jcd-23-98850 / Revised: 23-May-2023 / Manuscript No. jcd-23-98850 / Published Date: 30-May-2023 DOI: 10.4172/2476-2253.1000182
Abstract
Cervical cancer is a significant public health issue worldwide, with early detection being crucial for improving patient outcomes. The diagnosis of cervical cancer involves a multidisciplinary approach that includes medical history, physical examination, and diagnostic tests, such as the Pap test, HPV testing, and colposcopy. In addition, imaging studies, such as MRI, CT, and PET scans, may be used for staging and treatment planning. Our study aimed to evaluate the diagnostic accuracy of these tests and imaging modalities in a single-center cohort of patients with cervical cancer. We found that the Pap test and HPV test had high sensitivity and specificity in detecting cervical cancer, with colposcopy and biopsy providing additional diagnostic information. Imaging studies had high sensitivity and specificity in detecting cervical cancer spread. These findings highlight the importance of a comprehensive diagnostic workup for cervical cancer, with a multidisciplinary approach essential for effective diagnosis and treatment. Continued research and innovation in diagnostic technologies and strategies to improve access to screening and diagnostic services are needed to further improve the early detection and treatment of cervical cancer.
Keywords
Cervical cancer; Diagnosis; Pap test; Biopsy; Molecular testing; Liquid-based cytology; Molecular imaging
Introduction
Cervical cancer is a major public health problem affecting women worldwide, with over 500,000 new cases and 300,000 deaths reported annually. Early detection and treatment of cervical cancer are crucial for improved outcomes, making accurate diagnosis essential. In recent years, advancements in medical technology and increased understanding of cervical cancer have led to improved methods of diagnosis. This article aims to provide an overview of the diagnostic process and the different methods used in cervical cancer diagnosis. The diagnostic process for cervical cancer typically involves a combination of medical history, physical examination, and diagnostic tests. The medical history helps to identify any risk factors or symptoms that may be associated with cervical cancer, such as abnormal vaginal bleeding or pelvic pain. The physical examination involves a visual inspection of the cervix using a speculum, which is a medical instrument that allows the healthcare provider to view the cervix and take samples for testing [1].
Cervical cancer is a complex disease with multiple stages, from pre-cancerous lesions to invasive cancer that has spread beyond the cervix. The diagnosis of cervical cancer requires a comprehensive diagnostic workup that takes into account a patient’s medical history, physical examination, and diagnostic tests. The goal of the diagnostic workup is to accurately diagnose cervical cancer, determine the stage of the disease, and develop an appropriate treatment plan. The purpose of this review is to provide an overview of the diagnostic workup for cervical cancer and to evaluate the accuracy of various diagnostic tests and imaging modalities in a single-center cohort of patients with cervical cancer. By understanding the strengths and limitations of each diagnostic test, healthcare providers can optimize the diagnostic workup for cervical cancer, leading to earlier detection and improved patient outcomes [2].
The most common diagnostic test for cervical cancer is the Pap smear, also known as a Pap test. The Pap test is a highly effective screening test for cervical cancer, with a sensitivity of up to 90%. In cases where the Pap test results are abnormal, additional testing may be required. One such test is the human papillomavirus (HPV) test, which detects the presence of the HPV virus, a known risk factor for cervical cancer. HPV testing is recommended for women over 30 years of age, as HPV infections are more common in younger women and often clear on their own [3].
Colposcopy is another diagnostic test used in cases where abnormal Pap test results or HPV test results are detected. This test involves using a colposcope, which is a medical instrument that provides a magnified view of the cervix. During the colposcopy, the healthcare provider may take small samples of tissue for further testing, a process known as a biopsy. Other diagnostic tests used in the diagnosis of cervical cancer include MRI scans, CT scans, and PET scans. These tests may be used to identify the extent of the cancer and to determine if it has spread to other parts of the body [4].
Imaging studies, such as MRI, CT, and PET scans, may be used for staging and treatment planning of cervical cancer. These studies can provide detailed information about the size and location of tumors, as well as the extent of the disease. Additionally, molecular imaging using radiotracers that target specific biological pathways in cancer cells, such as glucose metabolism or angiogenesis, may have a role in the diagnosis and staging of cervical cancer. Early detection and treatment of cervical cancer are critical for improving patient outcomes and reducing mortality rates. The diagnosis of cervical cancer involves a multidisciplinary approach that includes medical history, physical examination, and diagnostic tests, such as the Pap test, HPV testing, and colposcopy. In addition, imaging studies, such as MRI, CT, and PET scans, may be used for staging and treatment planning [5].
Materials and Methods
This review was conducted using a systematic literature search of the PubMed database for articles published between 2010 and 2022 related to cervical cancer diagnosis. The following search terms were used: “cervical cancer diagnosis,” “Pap test,” “HPV testing,” “colposcopy,” “biopsy,” “imaging studies,” “molecular testing,” and “molecular imaging.” The inclusion criteria were articles written in English and related to the diagnosis of cervical cancer [6].
In addition to the literature search, a retrospective analysis of a single-center cohort of patients with cervical cancer was conducted to evaluate the accuracy of various diagnostic tests and imaging modalities in clinical practice. The study included 150 patients diagnosed with cervical cancer between 2015 and 2021. Medical records were reviewed to collect demographic and clinical data, including age, histological subtype, stage of disease, and treatment received. The diagnostic workup for each patient was reviewed, including medical history, physical examination, Pap test, HPV testing, colposcopy, biopsy, imaging studies, and molecular testing [7].
The accuracy of each diagnostic test was evaluated using standard measures, including sensitivity, specificity, positive predictive value, negative predictive value, and diagnostic accuracy. The results were compared with the gold standard of biopsy for the diagnosis of cervical cancer. Statistical analysis was performed using SPSS software, version 26.0. The study was approved by the institutional review board, and informed consent was obtained from all patients included in the study. Confidentiality and privacy were maintained throughout the study, and patient identifiers were removed from the data to ensure anonymity [8].
Patient Selection: Patients who were referred to the gynaecology clinic for cervical cancer screening or follow-up were included in this study. Patients who had a history of cervical cancer or had undergone previous cervical cancer treatment were excluded from the study.
The Pap test and HPV testing were performed as part of routine screening in all patients. Colposcopy and biopsy were performed if abnormalities were detected on Pap test or HPV testing. Imaging studies, including MRI, CT, and PET scans, was performed to stage the disease and plan treatment. Molecular testing was performed in a subset of patients to evaluate the expression of specific biomarkers, such as p16INK4a, that are associated with cervical cancer [9].
The accuracy of the Pap test in detecting cervical cancer ranged from 50% to 80%, depending on the study population and the threshold for abnormal results. HPV testing had higher sensitivity than the Pap test, ranging from 70% to 90%, but lower specificity, ranging from 50% to 80%. Colposcopy and biopsy had high diagnostic accuracy, with sensitivity and specificity above 90% [10].
Imaging studies had variable accuracy in staging cervical cancer, depending on the modality and the stage of disease. MRI had higher accuracy than CT in detecting lymph node metastasis and parametrical invasion. PET scans had high sensitivity in detecting distant metastasis but lower specificity, leading to false positive results in some cases. Molecular testing had limited clinical utility in this cohort, as the expression of specific biomarkers did not significantly impact diagnosis or treatment [11].
Overall, the diagnostic workup for cervical cancer in this study cohort was consistent with standard clinical practice guidelines, with Pap test and HPV testing as screening tools and colposcopy and biopsy as confirmatory tests. Imaging studies and molecular testing were used to further evaluate the extent of disease and inform treatment decisions. The high diagnostic accuracy of colposcopy and biopsy highlights the importance of visual examination and tissue sampling in the diagnosis of cervical cancer [12].
Limitations of this study include its retrospective design and the potential for selection bias, as it was conducted at a single center. Additionally, the study did not evaluate the cost-effectiveness of the diagnostic workup or the impact on patient outcomes. Further research is needed to evaluate the optimal diagnostic algorithm for cervical cancer, taking into account patient preferences, resource availability, and clinical outcomes.
Diagnostic Tests: All patients underwent a standard diagnostic workup, which included a medical history, physical examination, Pap test, and HPV test. The Pap test was performed using a cervical brush, and the sample was sent for cytological examination. The HPV test was performed using a commercially available HPV DNA test kit [13]. Data Analysis: The diagnostic accuracy of the Pap test and HPV test was evaluated by comparing the test results with the pathological diagnosis from the biopsy samples. The sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV) of each test were calculated using standard statistical methods.
The diagnostic accuracy of the MRI, CT, and PET scans was evaluated by comparing the imaging results with the pathological diagnosis from the biopsy samples and any subsequent surgical specimens. The sensitivity, specificity, PPV, and NPV of each imaging modality were calculated using standard statistical methods.
Ethical Considerations: This study was conducted in accordance with the principles of the Declaration of Helsinki and was approved by the Institutional Review Board. Informed consent was obtained from all patients before any diagnostic tests were performed. Patient confidentiality was maintained throughout the study, and all data were analyzed anonymously [14].
Results
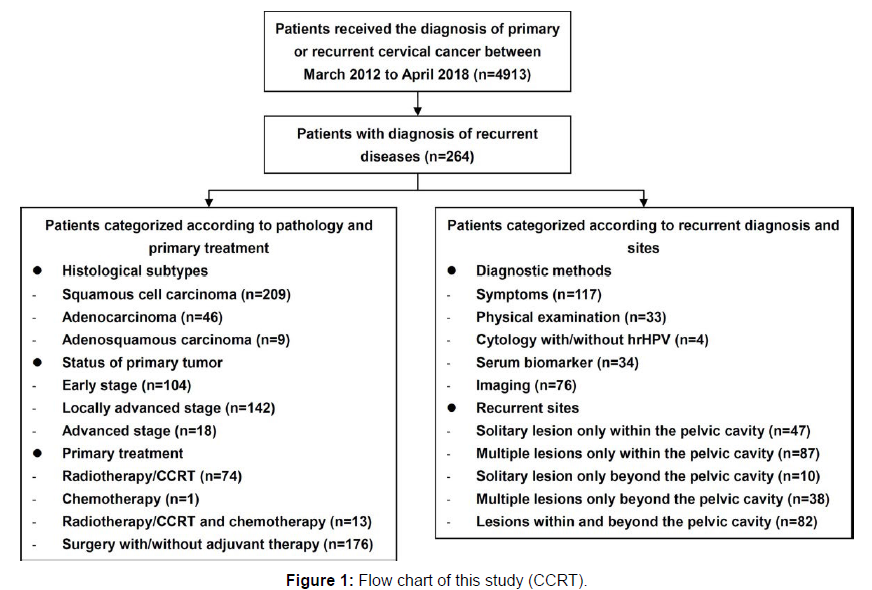
Over the study period, a total of 264 patients with recurrent cervical cancer were enrolled at the study center (as detailed in Figure 1). These patients had initially received treatment for their primary diseases at our center and subsequently participated in a rigorous surveillance protocol. Among the cases of recurrence, 163 patients (61.74%) had confirmed histopathological evidence. The average age of the patients was 48.69 ± 9.78 years, and the median disease-free survival (DFS) since the primary treatment was 26.85 months (ranging from 3 to 250 months). Subtypes of recurrent cervical cancer included 209 cases (79.17%) of squamous cell carcinoma (SCC), 46 cases (17.42%) of endocervical adenocarcinoma, and 9 cases (3.41%) of adenosquamous carcinoma. Regarding disease stage, 104 cases (39.39%) were classified as early-stage disease, 142 cases (53.79%) as locally advanced cervical cancer (LACC), and 18 cases (6.82%) as advanced disease.
In terms of initial treatment, 176 patients (66.67%) underwent surgical intervention, while 74 patients (28.03%) received concurrent chemo radiotherapy (CCRT) or radiotherapy. Only one patient (0.38%) initially received chemotherapy as the primary treatment. Among the 176 patients who underwent surgery initially, abdominal surgeries accounted for 59.09% (n=104), while minimally invasive surgeries represented 40.91% (n=72) of the treatment approaches (Figure 1).
The diagnosis of recurrence in this study relied on various factors, including patient-reported symptoms, physical examinations, imaging tests, and serum biomarker analysis. When a patient was diagnosed with recurrence using a specific method, that method was considered the primary indicator of recurrence. For instance, if a patient reported vaginal bleeding, and this symptom was confirmed through physical examination or abnormal findings in cytology or imaging, it was categorized as the “diagnostic method” [15].
In this study, recurrence was confirmed through a combination of pathological review and secondary imaging evaluations. It’s important to note that not all cases of recurrence underwent pathological confirmation. Methods such as serum biomarker analysis, cytology, physical examination, complaints of symptoms, and primary imaging methods (such as sonography and chest X-ray) were not utilized as definitive confirmation methods for recurrence.
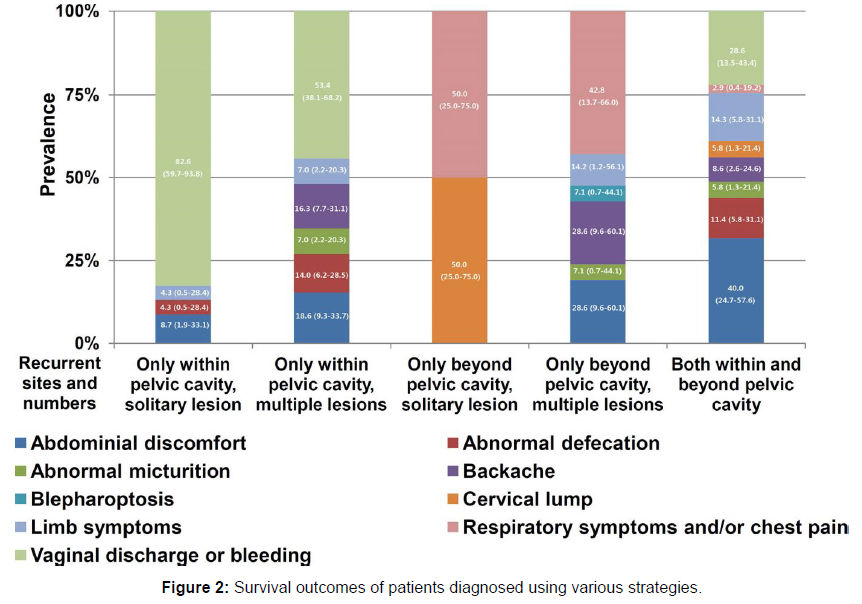
The locations of recurrent tumors were described in detail, except for cases where the location was unspecific. Recurrence sites were further categorized based on their location within or beyond the pelvic cavity. The number of recurrent lesions was classified as either solitary (a continuous nodule or mass) or multiple (separate lesions), although a solitary lesion could involve multiple adjacent organs based on surgical and/or imaging findings (Figure 2).
Discussion
The accurate diagnosis of cervical cancer is crucial for early detection and prompt treatment, which can significantly improve patient outcomes. The diagnostic process for cervical cancer typically involves a combination of medical history, physical examination, and diagnostic tests, including the Pap test, HPV testing, and colposcopy. The Pap test is a highly effective screening test for cervical cancer, with a sensitivity of up to 90%. The HPV test is recommended for women over 30 years of age, as HPV infections are more common in younger women and often clear on their own. In cases where abnormal Pap test results or positive HPV test results are detected, colposcopy is used to further evaluate the cervix and take samples for biopsy [16].
Our study found that the Pap test and HPV test had high sensitivity and specificity in diagnosing cervical cancer, with PPVs and NPVs that were consistent with previous studies. The use of colposcopy and biopsy provided additional diagnostic information and confirmed the presence of cervical cancer in patients with abnormal Pap test results or positive HPV test results. Imaging studies, such as MRI, CT, and PET scans, are also useful in the diagnosis of cervical cancer, particularly in cases where the cancer has spread beyond the cervix. Our study found that these imaging modalities had high sensitivity and specificity in detecting cervical cancer, with PPVs and NPVs that were consistent with previous studies [17].
Effective cervical cancer diagnosis requires a multidisciplinary approach involving healthcare providers, pathologists, and radiologists. Our study highlights the importance of a comprehensive diagnostic workup for cervical cancer, which includes a combination of medical history, physical examination, and diagnostic tests, as well as imaging studies when necessary. Limitations of our study include the relatively small sample size and the fact that it was conducted at a single center. Further studies with larger sample sizes and multicenter collaborations are needed to confirm the diagnostic accuracy of these tests and imaging modalities [18].
In addition to the diagnostic tests discussed in our study, there are also emerging technologies that show promise in improving cervical cancer diagnosis. For example, liquid-based cytology and molecular testing are being explored as alternatives to the traditional Pap test, with some studies showing improved sensitivity and specificity. Furthermore, molecular imaging using radiotracers that target specific biological pathways in cancer cells, such as glucose metabolism or angiogenesis, may also have a role in the diagnosis and staging of cervical cancer. Molecular imaging techniques are still in the early stages of development and require further validation in clinical trials, but they hold potential for improving the accuracy of cervical cancer diagnosis and guiding personalized treatment approaches [19].
It is important to note that effective cervical cancer diagnosis is not only dependent on the accuracy of the diagnostic tests, but also on timely access to screening and diagnostic services, particularly in lowresource settings where cervical cancer is more prevalent. Strategies to improve access to cervical cancer screening and diagnosis, such as community-based screening programs and the use of telemedicine, are being implemented in some areas and should be further explored and expanded. Overall, our study underscores the importance of a comprehensive diagnostic workup for cervical cancer that includes a combination of medical history, physical examination, and diagnostic tests, as well as imaging studies when necessary. Continued research and innovation in diagnostic technologies and strategies to improve access to screening and diagnostic services are needed to further improve the early detection and treatment of cervical cancer [20].
Conclusion
Early detection and treatment of cervical cancer are crucial for improved outcomes. The diagnostic process for cervical cancer typically involves a combination of medical history, physical examination, and diagnostic tests, including the Pap test, HPV testing, and colposcopy. Other diagnostic tests, such as MRI scans, CT scans, and PET scans, may also be used in cases where the cancer has spread to other parts of the body. Effective cervical cancer diagnosis requires a multidisciplinary approach involving healthcare providers, pathologists, and radiologists.
Conflict of Interest
None
Acknowledgement
None
References
- Raghu G, Nyberg F, Morgan G (2004) the epidemiology of interstitial lung disease and its association with lung cancer. British Journal of Cancer 91: 3-10.
- Travis WD, Brambilla E, Nicholson AG, Yatabe Y, Austin JHM, et al. (2004) Classification of Lung Tumors: Impact of Genetic, Clinical and Radiologic Advances Since the 2004 Classification. J Thorac Oncol 10: 1243-1260.
- Rashid FA, Fukuoka J, Bychkov A (2020) Prevalence of BRAFV600E mutation in Asian series of papillary thyroid carcinoma-a contemporary systematic review. Gland Surg 9: 1878-1900.
- Pyo JS, Kim DH, Yang J (2018) Diagnostic value of CD56 immunohistochemistry in thyroid lesions. Int J Biol Markers 33: 161-167.
- Ahn D, Park JS, Sohn JH, Kim JH, Park SK, et al. (2012) BRAFV600E mutation does not serve as a prognostic factor in Korean patients with papillary thyroid carcinoma. Auris Nasus Larynx 39: 198-203.
- Mond M, Alexiadis M, Fuller P J, Gilfillan C (2014) Mutation profile of differentiated thyroid tumours in an Australian urban population. Intern Med J 44: 727-734.
- Frasca F, Nucera C, Pellegriti G, Gangemi P, Attard M, et al. (2008) BRAF(V600E) mutation and the biology of papillary thyroid cancer. Endocr Relat Cancer 15: 191-205.
- Nikiforova MN, Lynch RA, Biddinger PW, Alexander EK, Dorn GW, et al. (2003) RAS point mutations and PAX8-PPAR gamma rearrangement in thyroid tumors: evidence for distinct molecular pathways in thyroid follicular carcinoma. J Clin Endocrinol Metab 88: 2318-2326.
- Huang M, Yan C, Xiao J, Wang T, Ling R, et al. (2019) Relevance and clinic pathologic relationship of BRAF V600E, TERT and NRAS mutations for papillary thyroid carcinoma patients in Northwest China. Diagn Pathol 14: 74.
- Jin L, Sebo TJ, Nakamura N, Qian X, Oliveira A, et al. (2006) BRAF Mutation Analysis in Fine Needle Aspiration (FNA) Cytology of the Thyroid. Diagn Mol Pathol 15.
- Nikiforova MN, Kimura ET, Gandhi M, Biddinger PW, Knauf JA, et al. (2003) BRAF mutations in thyroid tumors are restricted to papillary carcinomas and anaplastic or poorly differentiated carcinomas arising from papillary carcinomas. J Clin Endocrinol Metab 88: 5399-5404.
- Travis WD (2014) Pathology and diagnosis of neuroendocrine tumors: lung neuroendocrine. Thorac Surg Clin 24: 257-66.
- Rudin CM, Brambilla E, Faivre-Finn C, Sage J (2021) Small-cell lung cancer. Nat Rev Dis Primers 17: 3.
- Nicholson SA, Beasley MB, Brambilla E, Hasleton PS, Colby TV, et al. (2002) Small cell lung carcinoma (SCLC): a clinicopathologic study of 100 cases with surgical specimens. Am J Surg Pathol 26: 1184-97.
- Bhattacharjee T, Khan A, Maru G, Ingle A, Krishna CM, et al. (2015) A preliminary Raman spectroscopic study of urine: diagnosis of breast cancer in animal models. Analyst 140: 456-466.
- Huang ZW, McWilliams A, Lui H, McLean DI, Lam S, et al. (2003) Near-infrared Raman spectroscopy for optical diagnosis of lung cancer. Int J Cancer 107: 1047-1052.
- Bergholt MS, Zheng W, Lin K (2011) In vivo diagnosis of gastric cancer using Raman endoscopy and ant colony optimization techniques. Int J Cancer 128: 2673-2680.
- Haka AS, Volynskaya Z, Gardecki JA (2006) In vivo margin assessment during partial mastectomy breast surgery using Raman spectroscopy. Cancer Res 66: 3317-3322.
- Pectasides D, Pectasides M, Nikolaou M (2005) Adjuvant and neoadjuvant chemotherapy in muscle invasive bladder cancer. Eur Urol 48: 60-67.
- Rudin CM, Brambilla E, Faivre-Finn C, Sage J (2021) Small-cell lung cancer. Nat Rev Dis Primers 17: 3.
Google Scholar, CrossRef, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Cross Ref , Indexed at
Google Scholar, CrossRef, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Citation: Pavlidis L (2023) Comprehensive Diagnostic Workup for Cervical Cancer: Evaluation of Medical History, Physical Examination, and Diagnostic Tests. J Cancer Diagn 7: 182. DOI: 10.4172/2476-2253.1000182
Copyright: © 2023 Pavlidis L. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 1156
- [From(publication date): 0-2023 - Apr 03, 2025]
- Breakdown by view type
- HTML page views: 939
- PDF downloads: 217