Case Report Open Access
Complications of Adult Bacterial Meningitis and their Neurocritical Care Management – A Case Report and Short Review
Carmen Murr1*, Silvia Schonenberger1, Sabrina Klein2 and Julian Bosel1
1Department of Neurology, Neurocritical Care Unit, University of Heidelberg, Heidelberg, Germany
2Department of Infectious Diseases, Medical Microbiology, University of Heidelberg, Heidelberg, Germany
- *Corresponding Author:
- Carmen Isabelle Murr
Department of Neurology
University of Heidelberg
69120 Heidelberg, Germany
Tel: +49 6221 5639951
E-mail: carmen.murr@med.uni-heidelberg.de
Received January 27, 2015; Accepted March 28, 2015; Published March 31, 2015
Citation: Murr C, Schonenberger S, Klein S, Bosel J (2015) Complications of Adult Bacterial Meningitis and their Neurocritical Care Management– A Case Report and Short Review. J Neuroinfect Dis 6:169. doi:10.4172/2314-7326.1000170
Copyright: © 2015 Murr C, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Neuroinfectious Diseases
Abstract
Worldwide, bacterial meningitis is among the top ten causes of infection-related death. Although effective antimicrobial treatment is available and administered, fatality rates are still very high. Furthermore, 50% of affected patients suffer long-term sequelae due to severe complications, such as hydrocephalus, brain edema, cerebrovascular complications and ventriculitis. The following short review summarizes the most important complications and the neurocritical care management of acute bacterial meningitis in adults, illustrated by an instructive case report.
Introduction
According to estimates of the World Health Organization 1.2 million cases of bacterial meningitis occur every year [1]. Furthermore, acute bacterial meningitis is one of the top ten causes of infectionrelated death worldwide and 30-50% of the patients suffer from longterm sequelae [2]. Since the implementation of vaccination routines in many countries, the average age of manifestation has shifted from childhood to adulthood [3]. The three most common pathogens in adults are Neisseria meningitidis , Streptococcus pneumoniae and Listeria monocytogenes, [3-5]. In Europe, pneumococcal meningitis is the most common type of bacterial meningitis and is associated with the highest mortality rate [6]. Despite the widespread use of effective antimicrobial agents the fatality rates are still very high reaching up to 15-20% [6-8]. Many studies indicate that acute bacterial meningitis is a medical emergency and requires a specific management in intensive care units (ICU) [7,9,10]. The following article summarizes the most important complications of adult bacterial meningitis and their management, illustrated by one of our recent cases.
Case Report
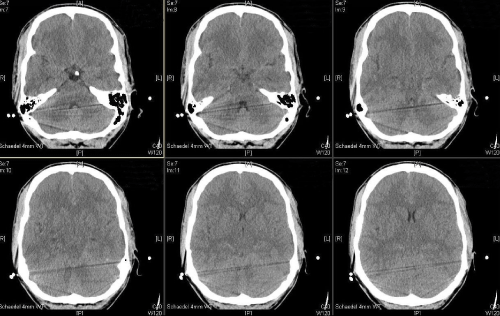
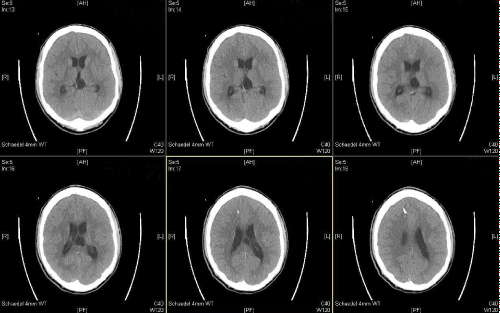
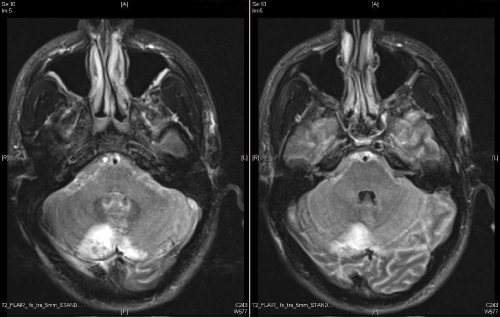
A 22 year old male patient presented to our emergency room with fever (38.5°C), severe headache and general indisposition. The headache started mildly two days before related to a cough. On admission he showed meningism without focal neurological deficits in the clinical examination. There was no rash. After drawing blood for microbiological analysis, performing a computed tomography (CT) scan and lumbal puncture (LP), an empirical i.v. antimicrobial therapy with ceftriaxone (first dose 4 g, then 2 g every 12 hours), ampicillin (5 g every 8 hours) and acyclovir (750 mg every 8 hours) was initiated. Simultaneously, the patient was treated with dexamethasone (10 mg). Gram staining of cerebrospinal fluid (CSF) was performed. It later showed a high amount of Gram positive diplococcal bacteria (Figure 1), hence acyclovir was discontinued. The CSF studies showed also a high cell count (2707 cells/μl), elevated levels of protein (1.65 g/l) and lactic acid (6.39 mmol/l), but normal concentration of glucose (61 mg/ dl). There were also elevated levels of leucocytes in the blood sample (14.69/nl), especially neutrophil granulocytes (11,6/nl), and low platelet counts (62/nl). Still in the emergency room, the patient got agitated, developed impairments in coordination and speech and finally got somnolent. He was immediately submitted to the ICU, where he soon had to be intubated and mechanically ventilated due to respiratory deterioration. A few hours later the patient presented wide, fixed pupils on both sides. A second CT scan displayed an increasing diffuse cerebral edema with narrow basal cisterns, compressed ventricles and effaced cortical sulci (Figure 2). To lower intracranial pressure (ICP) an osmotic therapy with mannitol and hypertonic sodium chloride, and –since this was not sufficient- thiopental were administered, which eventually resulted in a normal pupil status. To monitor ICP and cerebral perfusion pressure (CPP) continuously, an intraparenchymal probe was inserted in the right frontal lobe. On the following day, ICP crises re-occurred which were not responsive to the aforementioned therapy. Another cranial CT showed the known brain edema and additionally widened ventricles with beginning of cerebral herniation indicative of hydrocephalus malresorptivus (Figure 3). An extraventricular drain (EVD) was inserted, CSF drainage led to immediate normalization of ICP. An additional magnetic resonance imaging (MRI) showed cerebellar lesions probably caused by tentorial compression during the transient herniation (Figure 4), but no other signs of irreversible secondary brain damage. To test for the occurrence of vasculitis and/or vasospasms transcranial Doppler ultrasound (TCD) was applied daily. This showed no pathological results at any time. After microbiological analysis of the CSF, identifying the pathogen as Streptococcus pneumoniae, antibiotic treatment was adapted to penicillin G (5 Mio. units every four hours) for 14 days. The analysis of five pairs of blood culture probes remained sterile. In anticipation of a long and complicated course of disease a dilational tracheostomy was performed. The further clinical course was favorable. There were no more ICP crises or other complications, so the sedation was slowly tapered and the patient started to be weaned from the ventilator 10 days after submission. The weaning was successfully completed on day 12. The ICP probe and external ventricular drain (EVD) could be removed on the 11th day. Clinical examination revealed an anisocoria, a slight dysphagia and a hyperactive delirium, but no other neurological impairments. The patient was transferred to a rehabilitation center on day 13.
Discussion - Complications of Acute Bacterial Meningitis in Adults
Even if guideline-recommended treatment with third generation cephalosporins, ampicillin, and dexamethasone is applied, about half of adults with acute bacterial meningitis suffer severe complications, occurring most frequently during the first week [11-13]. Hence admission to a, preferably neurological, ICU is recommended to ensure close monitoring and rapid treatment.
The most common complications of bacterial meningitis in adults are brain edema and hydrocephalus, posing the threat of herniation. The frequency is approximately 10-15% [11]. Keeping in mind that there is no need for routine imaging before LP in uncomplicated cases of bacterial meningitis, CT or MRI are required in patients presenting with decreased level of consciousness or severe neurological impairments. Effaced basal cisterns, ventricles and cortical sulci, descent of cerebellar tonsils and brainstem through the foramen magnum and the cerebellar reversal sign (the cerebellum appears bright relative to hypodense anoxic supratentorial brain) are the best predictors of impending herniation on CT [14]. An LP should not be performed in these cases, but even a normal CT does not ensure that LP is safe according to some reports [15].
It is recommended to insert a probe to monitor the ICP, if the patient does not regain consciousness, and therefore cannot be monitored clinically, one day after starting antibiotic treatment [16]. Brain edema with raised ICP can often be effectively treated by osmotic therapy with mannitol and/or hypertonic sodium chloride in pulsatile or on-demand fashion according to ICP monitoring. Barbiturates and mild hyperventilation are means to escalate, but should only be used short-term because of frequent side effects.
The occurrence of hydrocephalus in patients with acute bacterial meningitis is associated with worse outcome: The fatality rate of these patients reaches up to 46%, whereas the fatality rate of patients without this complication is around 17% [17]. Pathophysiologically, meningeal adhesion at the bottom of the 4th ventricle leads to a hydrocephalus occlusus, while blocking the absorption of CSF in the Pacchonian granulations causes a hydrocephalus malresorptivus. Consequently, the circulation of CSF is blocked and the ICP rises. Appropriate treatment of ICP crises and impending herniation caused by hydrocephalus is the insertion of an EVD [18]. A mild hydrocephalus is seen in most patients with meningitis and does not have to be treated. Furthermore, the ventricular system of some patients remains dilated, but stable (“arrested hydrocephalus”), which also requires no therapeutic intervention [14].
Arterial cerebrovascular complications
Arterial cerebrovascular complicationssuch as stroke and cerebral hemorrhage, occur in approximately 15-20% of patients with bacterial meningitis [12]. Vasculitis, i.e. a severe inflammation of the vessel walls, and/or vasospasms are the most likely cause of these complications [11,19]. To monitor the cerebral hemodynamics TCD sonography has been reported to be a very useful diagnostic tool [20,21]. Usually the treatment of vasospasms, as caused by subarachnoid hemorrhage, involves the elevation of blood pressure in combination with intravenous or oral nimodipine [22]. Sometimes these strategies are adopted for the treatment of bacterial meningitis as well, although a study has shown that a therapy with nimodipine does not necessarily reduce the risk of stroke, hence a beneficial effect on outcome remains to be proven [23]. Furthermore, a strong elevation of blood pressure during the course of bacterial meningitis may be associated with a higher risk of intracerebral hemorrhage and cannot routinely be recommended for patients with meningitis-related vasospasms [23].
Septic thrombosis
Septic thrombosis of cerebral veins and sinus´ occurs in about 10% of patients with bacterial meningitis [11,12]. It can be a direct consequence of meningitis or secondary to mastoiditis - itself a probable cause of meningitis. There is a risk of infarction or hemorrhage due to a reduction of intracranial venous blood flow or stasis. It can be detected by MRI or CT venography [14,24]. There are few and controversial findings concerning the treatment with intravenous heparin: whereas a retrospective study showed a beneficial effect in patients with septic thrombosis of the sinus cavernosus, there is also a high risk for intracerebral bleedings for patients with a thrombosis of the sinus transverses [25]. Nonetheless some guidelines recommend anticoagulation in this setting [26].
Epileptic seizures
Epileptic seizures are a common complication of bacterial meningitis. In some cases they are the first presenting symptom, indicating impending herniation or the presence of an intraparenchymal abscess or cerebritis/encephalitis. Approximately 5% of patients with acute bacterial meningitis suffer from seizures [5,27]. In severe cases a prophylactic antiepileptic treatment, for example with levetiracetam or valproate can be considered, although there are no prospective studies to prove a benefit thereof so far. Manifest seizures or status epilepticus need to be treated vigorously with antiepileptics.
Cerebritis and brain abscesses
Cerebritis and brain abscesses occur in approximately 1-5% of patients with bacterial meningitis [11-13]. In the clinical examination the patients often present a focal neurological deficit, e.g. partial paralysis or speech disorder, suffer from epileptic seizures or solely cephalgia, which is commonly one-sided. Abscesses can be the cause or the consequence of meningitis and are best detected by MRI or even MR spectroscopy (differentiation of abscess and tumor) [14]. A stereotactic puncture with drainage of the abscess should be performed promptly, as the treatment with antibiotics is often not sufficient in these cases. A retrospective study identified cefotaxime and metronidazole as an efficient combination for empiric antimicrobial therapy [28]. An adjunctive therapy with corticosteroids is also recommended, if perifocal edema, impending herniation or multiple abscesses are detected [29,30].
Many aspects of optimal neurocritical care in adult bacterial meningitis, such as those relating to airway, ventilation, circulation, metabolism or temperature management, remain to be elucidated by prospective research. The principle of neuroprotective and antiedematous hypothermia was recently investigated in a large French multicenter randomized trial on 98 patients with bacterial meningitis which showed more harm than benefit [31].
Conclusion
Bacterial meningitis is still a life-threatening disease associated with high morbidity and mortality. Intracranial complications are associated with a worse outcome and often the cause of long-term sequelae. Rapid identification and treatment of patients at risk is crucial and can be life-saving. The admission to a neurological ICU is strongly recommended to ensure continuous monitoring and prompt treatment.
Acknowledgements
I warmly thank Silvia Schönenberger and Julian Bösel for their support and constructive discussions, as well as Sabrina Klein and the department of Infectious Diseases for providing the Gram staining and for their cooperation. Furthermore I thank H.W. Pfister and U. Ködel, (Department of Neurology, KlinikumGroßhadern, Munich, Germany) for introducing me to the topic of bacterial meningitis.
References
- WHO (2003) Annual Report of Cummunicable Diseases. San Francisco.
- Chaudhuri A, Martinez-Martin P, Kennedy PG, Andrew Seaton R, Portegies P, et al. (2008) EFNS guideline on the management of community-acquired bacterial meningitis: report of an EFNS Task Force on acute bacterial meningitis in older children and adults. European journal of neurology: the official journal of the European Federation of Neurological Societies 15: 649-659.
- Schuchat A, Robinson K, Wenger JD, Harrison LH, Farley M, et al. (1997) Bacterial meningitis in the United States in 1995. Active Surveillance Team. N Engl J Med 337: 970-976.
- Hussein AS, Shafran SD (2000) Acute bacterial meningitis in adults. A 12-year review. Medicine (Baltimore) 79: 360-368.
- van de Beek D, de Gans J, Spanjaard L, Weisfelt M, Reitsma JB, et al. (2004) Clinical features and prognostic factors in adults with bacterial meningitis. N Engl J Med 351: 1849-1859.
- Brouwer MC, Tunkel AR, van de Beek D (2010) Epidemiology, diagnosis, and antimicrobial treatment of acute bacterial meningitis. Clinical microbiology reviews 23: 467-92.
- van de Beek D, de Gans J, Tunkel AR, Wijdicks EF (2006) Community-acquired bacterial meningitis in adults. N Engl J Med 354: 44-53.
- van de Beek D, Brouwer MC, Thwaites GE, Tunkel AR (2012) Advances in treatment of bacterial meningitis. Lancet 380: 1693-1702.
- Flores-Cordero JM, Amaya-Villar R, Rincon-Ferrari MD, Leal-Noval SR, Garnacho-Montero J, et al. (2003) Acute community-acquired bacterial meningitis in adults admitted to the intensive care unit: clinical manifestations, management and prognostic factors. Intensive care medicine 29: 1967-1973.
- Auburtin M, Porcher R, Bruneel F, Scanvic A, Trouillet JL, et al. (2002) Pneumococcal meningitis in the intensive care unit: prognostic factors of clinical outcome in a series of 80 cases. Am J RespirCrit Care Med 165: 713-717.
- Pfister HW, Feiden W, Einhäupl KM (1993) Spectrum of complications during bacterial meningitis in adults. Results of a prospective clinical study. Arch Neurol 50: 575-581.
- Kastenbauer S, Pfister HW (2003) Pneumococcal meningitis in adults: spectrum of complications and prognostic factors in a series of 87 cases. Brain 126: 1015-1025.
- Weisfelt M, van de Beek D, Spanjaard L, Reitsma JB, de Gans J (2006) Clinical features, complications, and outcome in adults with pneumococcal meningitis: a prospective case series. Lancet Neurol 5: 123-129.
- Hughes DC, Raghavan A, Mordekar SR, Griffiths PD, Connolly DJ (2010) Role of imaging in the diagnosis of acute bacterial meningitis and its complications. Postgrad Med J 86: 478-485.
- Rennick G, Shann F, de Campo J (1993) Cerebral herniation during bacterial meningitis in children. BMJ 306: 953-955.
- Winkler F, Kastenbauer S, Yousry TA, Maerz U, Pfister HW (2002) Discrepancies between brain CT imaging and severely raised intracranial pressure proven by ventriculostomy in adults with pneumococcal meningitis. Journal of Neurology 249: 1292-7
- Kasanmoentalib ES, Brouwer MC, van der Ende A, van de Beek D (2010) Hydrocephalus in adults with community-acquired bacterial meningitis. Neurology 75: 918-923.
- Kramer AH, Bleck TP (2007) Neurocritical care of patients with central nervous system infections. Curr Infect Dis Rep 9: 308-314.
- Klein M, Paul R, Angele B, Popp B, Pfister HW, et al. (2006) Protein expression pattern in experimental pneumococcal meningitis. Microbes and infection / Institut Pasteur 8: 974-83.
- Muller M, Merkelbach S, Huss GP, Schimrigk K (1995) Clinical relevance and frequency of transient stenoses of the middle and anterior cerebral arteries in bacterial meningitis. Stroke 26: 1399-403.
- Manno EM (1997) Transcranial Doppler ultrasonography in the neurocritical care unit. Crit Care Clin 13: 79-104.
- Rabinstein AA, Lanzino G, Wijdicks EF (2010) Multidisciplinary management and emerging therapeutic strategies in aneurysmal subarachnoid haemorrhage. Lancet Neurol 9: 504-519.
- Klein M, Koedel U, Pfefferkorn T, Zeller G, Woehrl B, et al. (2011) Arterial cerebrovascular complications in 94 adults with acute bacterial meningitis. Critical care 15: R281.
- Ducreux D, Oppenheim C, Vandamme X, Dormont D, Samson Y, et al. (2001) Diffusion-weighted imaging patterns of brain damage associated with cerebral venous thrombosis. AJNR Am J Neuroradiol 22: 261-268.
- Southwick FS (1995) Septic thrombophlebitis of major dural venous sinuses. CurrClin Top Infect Dis 15: 179-203.
- LeitlinienfürDiagnostik und Therapie in der Neurologie (2012) ThiemeVerlag Stuttgart.
- Ostergaard C, Konradsen HB, Samuelsson S (2005) Clinical presentation and prognostic factors of Streptococcus pneumoniae meningitis according to the focus of infection. BMC infectious diseases 5: 93.
- Jansson AK, Enblad P, Sjolin J (2004) Efficacy and safety of cefotaxime in combination with metronidazole for empirical treatment of brain abscess in clinical practice: a retrospective study of 66 consecutive cases. European journal of clinical microbiology & infectious diseases : official publication of the European Society of Clinical Microbiology 23: 7-14.
- Seydoux C, Francioli P (1992) Bacterial brain abscesses: factors influencing mortality and sequelae. Clinical infectious diseases : an official publication of the Infectious Diseases Society of America 15: 394-401.
- Patel K, Clifford DB2 (2014) Bacterial brain abscess. Neurohospitalist 4: 196-204.
- Mourvillier B, Tubach F, van de Beek D, Garot D, Pichon N, et al. (2013) Induced hypothermia in severe bacterial meningitis: a randomized clinical trial. JAMA 310: 2174-2183.
Relevant Topics
- Bacteria Induced Neuropathies
- Blood-brain barrier
- Brain Infection
- Cerebral Spinal Fluid
- Encephalitis
- Fungal Infection
- Infectious Disease in Children
- Neuro-HIV and Bacterial Infection
- Neuro-Infections Induced Autoimmune Disorders
- Neurocystercercosis
- Neurocysticercosis
- Neuroepidemiology
- Neuroinfectious Agents
- Neuroinflammation
- Neurosyphilis
- Neurotropic viruses
- Neurovirology
- Rare Infectious Disease
- Toxoplasmosis
- Viral Infection
Recommended Journals
Article Tools
Article Usage
- Total views: 18334
- [From(publication date):
May-2015 - Jul 04, 2025] - Breakdown by view type
- HTML page views : 13613
- PDF downloads : 4721