Case Report Open Access
Complete Remission of Primary Cutaneous Cryptococcosis in an Immunosuppressed Patient after Fluconazole Treatment
Landucci G1, Farinelli P2, Zavattaro E3*, Giorgione R2, Gironi LC2, Veronese F1, Astolfi S2, Tiberio R2, Boldorini RL1, Colombo E3 and Savoia P1
1Department of Health Sciences, University of Eastern Piedmont, Novara, Italy
2Maggiore della Carita University-Hospital, Novara, Italy
3Department of Translational Medicine, University of Eastern Piedmont, Novara, Italy
- *Corresponding Author:
- Elisa Zavattaro
Department of Translational Medicine
University of Eastern Piedmont
Via Solaroli 17, 28100, Novara, Italy
Tel: 39 0321 3733269
Fax: 39 0321 3733586
E-mail: elisa.zavattaro@med.uniupo.it
Received date: June 25, 2017; Accepted date: July 20, 2017; Published date: July 26, 2017
Citation: Landucci G, Farinelli P, Zavattaro E, Giorgione R, Gironi LC, et al. (2017) Complete Remission of Primary Cutaneous Cryptococcosis in an Immunosuppressed Patient after Fluconazole Treatment. J Infect Dis Ther 5:326. doi: 10.4172/2332-0877.1000326
Copyright: © 2017 Zavattaro E, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Infectious Diseases & Therapy
Abstract
Cryptococcus neoformans is opportunistic encapsulated yeast that represents the most frequent cryptococcal species found in humans. It can cause three types of infections: pulmonary cryptococcosis, cryptococcal meningitis and cutaneous cryptococcosis. Cutaneous cryptococcosis may represent the dissemination of a systemic infection (especially from nervous or pulmonary primary site of infection) or may be the only localization, due to a direct inoculation into the skin, because of a traumatic injury. Primary cutaneous cryptococcosis (PCC) is rare and mainly affects elderly patients, from rural areas, with history of cutaneous injuries and activities predisposing wounds or exposure to bird droppings. Immunosuppression may be a predisponing factor. The most utilized treatment is fluconazole, but often, especially for ulcers or deep wounds; surgery is required for complete tissues repair. Herein, we present a case of PCC in an immunosuppressed patient, with destroying ulcers involving deep tissues, completely resolved after fluconazole treatment, without surgical intervention.
Keywords
Primary cutaneous cryptococcosis; Immunosuppression; Skin lesions; Fluconazole
Introduction
Cryptococcus neoformans is opportunistic encapsulated yeast and represents the most frequent cryptococcal species found in humans. Four serotypes are considered pathogenic for humans: C. neoformans var. grubii (serotype A), C. neoformans var. neoformans (serotype D) and C. neoformans var. gattii (serotypes B and C) [1,2].
C. neoformans has a worldwide distribution and can be isolated from decaying wood, tree hollows, fruit, vegetables, grass, hay, soil, dust and bird droppings, especially from pigeons [2]. Cryptococcosis is considered an opportunistic infection as it affects mainly individuals with impaired cell-mediated immunity such as HIV-infected subjects, patients who underwent to a prolonged glucocorticoid-treatment, with malignancies or organ transplant recipients [3-6]. However, some reports show that C. gattii seems to be more virulent and, for such reason, it can affect apparently healthy hosts [7-10].
In humans, C. neoformans causes three types of infections: pulmonary cryptococcosis, cryptococcal meningitis and wound or cutaneous cryptococcosis [11]. A secondary involvement of the skin is seen in approximately 15% of patients with systemic dissemination and cutaneous lesions are also found in 5% of patients affected by cryptococcal meningitis [12]. Skin lesions can represent the initial clinical manifestation of a disseminated disease. Multiple scattered polymorphic skin lesions spread on both clothed and unclothed areas are the most common clinical feature, but Molluscum contagiosum-like umbilicated papules are often found in patients with disseminated disease [1,13]. Direct traumatic inoculation into the skin can cause primary cutaneous cryptococcosis (PCC). In PCC, skin lesions are usually isolated or confined to a limited and unclothed body area, with different clinical presentations: whitlow, cellulitis, ulceration, with or without regional lymphadenopathy [4]. PCC without systemic infection has been noticed to be a rare distinct clinical entity [1,2,10]. Fluconazole is the most common treatment for PCC, with a daily dose of 400 mg and lasting up to 12 months. In immunosuppressed patients, lifelong manteinance treatment with fluconazole may be required. However, surgery is sometimes needed to complete tissue repair [14].
Case Presentation
We present a case of a 75-year-old man with a history of bullous pemphigoid treated with prednisone (average dose 25 mg daily) for more than one year. He had a past medical history of poorly controlled type-2 insulin dependent mellitus diabetes, chronic renal failure in medical therapy, class 2 NYHA heart failure and chronic atrial fibrillation; thus he was in treatment with multiple drugs, including rivaroxaban to reduce the risk of stroke and systemic embolism.
The patient was admitted to the Infectious Diseases Department presenting with skin ulceration, swelling, erythema and pain on his left forearm and hand. He reported the appearance of a small erythematous papule on the forearm about 5 months before, which converted into an ulcer and gradually grew until reaching the entire dorsal surface of his left forearm and hand. He denied any previous skin lesion as well as any contact with animals, especially birds. He also denied fever and any other systemic symptoms. The patient lived in a rural area and he had no outdoor activities that could represent a risk factor for skin injuries.
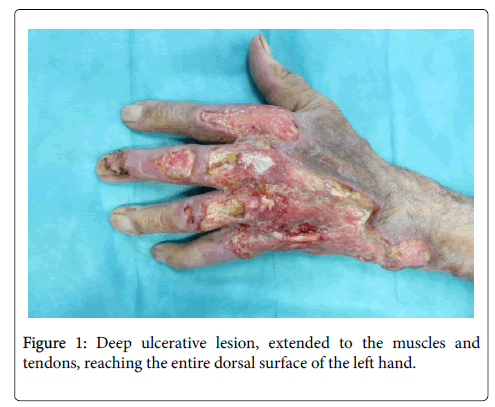
In suspicion of streptodermitis, the patient was treated with piperacillin-tazobactam, but despite therapy, the lesions progressively extended to the muscles and tendons (Figure 1). No regional lymphadenopathy was detectable. Inflammatory markers were elevated (CRP 280 mg/L, leukocytes 12*103/μL) and the differential blood count demonstrated an increased percentage of neutrophils (79.4% corresponding to 9.67*103/ μL), whereas serology for HBV, HCV and HIV were found to be negative.
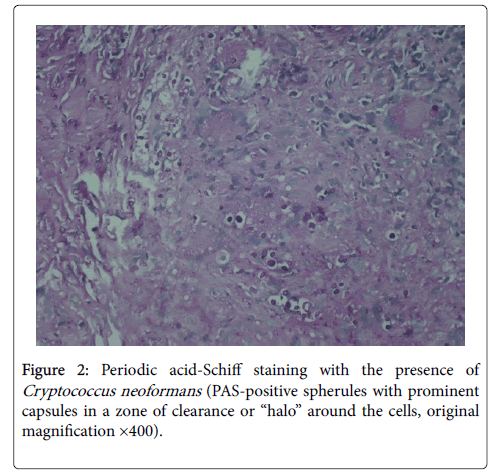
A skin biopsy showed, under a loss of epidermis, the presence of a chronic granulomatous inflammation in the dermis, with a marked giant cell reaction around pale spherical structures. These latter were identified as fungal colonies composed by different sizes spores, that were detected by periodic acid-Schiff staining and suspicious for cryptococcal infection (Figure 2). This finding was subsequently confirmed by microbial culture, showing the growth of milky colonies typical of Cryptococcus neoformans var. neoformans.
Workup for disseminated disease including blood and urine culture, analysis for fungal antigen in serum, chest x-ray, abdomen and pelvis US evaluation returned negative. Of note, skull tomography and lumbar puncture were not performed because the patient did not complaint any neurological symptoms.
After the diagnosis, we attempted to gradually reduce the dose of prednisone, but the recurrence of pemphigoid forced us to return to the initial dose. Systemic therapy with oral fluconazole 200 mg/day was started: the low dosage was chosen taking into account the absence of systemic involvement, the reduced renal function and the potential pharmacological interaction with rivaroxaban. Local treatment included daily dressings with topical protease enzymes (Clostridiopeptidase A), to remove necrotic tissues. Treatment with fluconazole was continued for six months at the same dosage, until the lesion had completely healed. At the end of the treatment, a complete re-epithelialization was obtained, even if scarring caused a partial inability to completely extend the last three fingers of the left hand (Figure 3).
Discussion
PCC is defined as identification of C. neoformans in a skin lesion, without evidence of simultaneous disseminated disease. Most cases of PCC have been reported from Europe, Japan, and South America [1].
Du et al. reviewed 21 cases of PCC published from 2004 to 2014, reporting that males were more likely to develop PCC infections (male-female ratio 17:4) [15]. They were almost all elderly subjects and upper limbs were the most common site of infection. Asymptomatic or moderate itching manifesting in a painful nodule was the most common presentation, although no typical clinical manifestation was recorded. Of the 12 serotypes isolates, 6 strains were C. neoformans, 5 C. gattii, and 1 C. laurentii. Regarding therapy, fluconazole was administered in 10 cases; however, only in 8 it was able to clear the infection. Interestingly, itraconazole was effective in other seven cases reported by literature. Despite the efficacy of medical treatment, some patients needed surgical debridement to remove infected tissues and repair skin damages [15,16].
Our patient was a 75 year-old male presenting with various comorbidities, which could have led him to a moderate state of immunosuppression. Despite the clinical features were the same observed in other patients affected by PCC, diagnosis was delayed because of the absence of risk factors and other systemic symptoms.
Although C. gattii is the most frequent agent of PCC reported by literature, C. neoformans var. neoformans has been identified in the skin lesions of our patient, according to the geographical distribution of the different serotypes of C. neoformans (C. gattii seems to be much more prevalent in the South America, while C. Neoformans var. neoformas in Europe) [1,2,7].
We report a PCC case in which skin lesions completely resolved with fluconazole in oral monotherapy, without resorting to surgery. Despite the severity of clinical feature, that extended deeply in the tissues, fluconazole in low-dosage was effective in treating such rare clinical entity. To our knowledge, this is the first case report showing the efficacy of low-dosage fluconazole in a mild immunosuppressed patient.
With this in mind, we think that the role of surgical debridement should be considered for patients at high risk of pharmacologic adverse events by use of antifungal azole (early drug intolerance, potential hepatotoxicity, QTc prolongation, drug-drug interactions) [16].
Conclusion
In summary, our case emphasizes that microbiologic testing and evaluations for opportunistic atypical infections, such as cryptococcosis, should be considered in diabetic or immunocompromised patients, who present with cellulitis not responding to widespread spectrum of antibiotic therapy.
References
- Neuville S, Dromer F, Morin O, Dupont B, Ronin O, et al. (2003) Primary cutaneous cryptococcosis: a distinct clinical entity. Clin Infect Dis 36: 337-347.
- Leão CA, Ferreira-Paim K, Andrade-Silva L, Mora DJ, da Silva PR, et al. (2011) Primary cutaneous cryptococcosis caused by Cryptococcus gattii in an immunocompetent host. Med Mycol 49: 352-355
- Chen S, Sorrell T, Nimmo G, Speed B, Currie B, et al. (2000) Epidemiology and host-and variety-dependent characteristics of infection due to Cryptococcus neoformans in Australia and New Zealand. Australasian Cryptococcal Study Group. Clin Infect Dis 31: 499-508.
- Christianson JC, Engber W, Andes D (2003) Primary cutaneous cryptococcosis in immunocompetent and immunocompromised hosts. Med Mycol 41: 177-188.
- Moosbrugger EA, Adams BB, Kralovic SM (2008) Cutaneous cryptococcosis in a patient on corticosteroid therapy for rheumatoid arthritis. Int J Dermatol 47: 630-632.
- Singh N, Dromer F, Perfect JR, Lortholary O (2008) Cryptococcosis in solid organ transplant recipients: current state of the science. Clin Infect Dis 47: 1321-1327.
- Severo LC, Berta-E-Zardo I, Londero TL (2001) Cutaneous cryptococcosis due to Cryptococcus neoformans var. gattii. Rev Iberoam Micol 18: 200-201.
- Revenga F, Paricio JF, Merino FJ, Nebreda T, Ramirez T, et al. (2002) Primary cutaneous cryptococcosis in an immunocompetent host: case report and review of the literature. Dermatology 204: 145-149
- Santos WR, Meyer W, Wanke B, Costa SP, Trilles I, et al. (2008) Primary endemic Cryptococcus gattii by molecular type VGII in the state of Parà, Brazil. Mem Inst Oswaldo Cruz 103: 813-818.
- Walsh TL, Bhanot N, Murillo MA, Uchin JM, Min Z (2017) Creeping Skin Lesions: Primary Cutaneous Cryptococcosis. Am J Med 130: 666-668.
- Dromer F (2001) Cryptococcosis. Rev Prat 51: 738-741.
- Probst C, Pongratz G, Capellino S, Szeimies RM, Scholmerich J, et al. (2010) Cryptococcosis mimicking cutaneous cellulitis in a patient suffering from rheumatoid arthritis: a case report. BMC Infect Dis 10: 239.
- Sarosi GA, Silberfarb PM, Tosh FE (1971) Cutaneous cryptococcosis. A sentinel of disseminated disease. Arch Dermatol 104: 1-3.
- Perfect JR, Dismukes WE, Dromer F, Goldman DL, Graybill JR, et al. (2010) Clinical practice guidelines for the management of cryptococcal disease: 2010 Update by the Infectious Diseases Society of America. Clin Infect Dis 50: 291-322.
- Du L, Yang Y, Gu J, Chen J, Liao W, et al. (2015) Systemic Review of Published Reports on Primary Cutaneous Cryptococcosis in Immunocompetent Patients. Mycopathologia 180: 19-25.
- Wang J, Bartelt L, Yu D, Joshi A, Weinbaum B, et al. (2015) Primary cutaneous cryptococcosis treated with debridement and fluconazole monotherapy in an immunosuppressed patient: a case report and review of the literature. Case Rep Infect Dis 2015: 131356.
Relevant Topics
- Advanced Therapies
- Chicken Pox
- Ciprofloxacin
- Colon Infection
- Conjunctivitis
- Herpes Virus
- HIV and AIDS Research
- Human Papilloma Virus
- Infection
- Infection in Blood
- Infections Prevention
- Infectious Diseases in Children
- Influenza
- Liver Diseases
- Respiratory Tract Infections
- T Cell Lymphomatic Virus
- Treatment for Infectious Diseases
- Viral Encephalitis
- Yeast Infection
Recommended Journals
Article Tools
Article Usage
- Total views: 2944
- [From(publication date):
August-2017 - Nov 21, 2024] - Breakdown by view type
- HTML page views : 2297
- PDF downloads : 647