Case Report Open Access
Complete Histopathological Disappearance of Rectal Malt Lymphoma after Eradication of Helicobacter pylori Confirmed by ESD
Jun Arimoto, Takuma Higurashi and Atsushi Nakajima*Division of Gastroenterology and Hepatology, Yokohama City University School of Medicine, Yokohama, Japan
- *Corresponding Author:
- Atushi Nakajima
Division of Gastroenterology and Hepatology
Yokohama City University School of Medicine
3-9 Fukuura, Kanazawa-ku, Yokohama 236-0004 Japan
Tel: +81-45-7872640
Fax: +81-45-7843546
E-mail: nakajima-tky@umin.ac.jp
Received date: February 24, 2015; Accepted date: March 1, 2015; Published date: March 18, 2015
Citation: Arimoto J, Higurashi T, Nakajima A (2015) Complete Histopathological Disappearance of Rectal Malt Lymphoma after Eradication of Helicobacter pylori Confirmed by ESD. J Gastrointest Dig Syst 5:263. doi:10.4172/2161-069X.1000263
Copyright: ©2015 Arimoto J, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited
Visit for more related articles at Journal of Gastrointestinal & Digestive System
Abstract
In a 77-year-old Japanese housewife who was undergoing regular colonoscopy for follow-up of a colon polyp, a total colonoscopy showed an elevated lesion in the rectum. Histological findings of a conventional biopsy from the lesion showed a mucosa-associated lymphoid tissue (MALT) lymphoma, and the patient was diagnosed as having clinical stage 1 disease. We elected to administer antibiotic therapy as the serological test for anti-Helicobacter pylori antibody was positive and Helicobacter pylori was detected in a culture of the biopsy specimens. The antibiotic therapy was successful, however, colonoscopy after the eradication therapy showed a residual lesion. Histologic examination can’t deny the possibility of the presence of a residual MALT lymphoma. Endoscopic ultrasonography revealed that the lesion was confined to the mucosa. We performed endoscopic submucosal dissection (ESD) and histological examination of the ESD specimen showed complete disappearance of the tumor. The patient remains in complete remission now, 1 year after the treatment.
Abstract
In a 77-year-old Japanese housewife who was undergoing regular colonoscopy for follow-up of a colon polyp, a total colonoscopy showed an elevated lesion in the rectum. Histological findings of a conventional biopsy from the lesion showed a mucosa-associated lymphoid tissue (MALT) lymphoma, and the patient was diagnosed as having clinical stage 1 disease. We elected to administer antibiotic therapy as the serological test for anti-Helicobacter pylori antibody was positive and Helicobacter pylori was detected in a culture of the biopsy specimens. The antibiotic therapy was successful, however, colonoscopy after the eradication therapy showed a residual lesion. Histologic examination can’t deny the possibility of the presence of a residual MALT lymphoma. Endoscopic ultrasonography revealed that the lesion was confined to the mucosa. We performed endoscopic submucosal dissection (ESD) and histological examination of the ESD specimen showed complete disappearance of the tumor. The patient remains in complete remission now, 1 year after the treatment.
Keywords
Rectal Malt Lymphoma; Helicobacter pylori; ESD
Introduction
Mucosa-associated lymphoid tissue (MALT) lymphoma, also known as extra-nodal marginal zone lymphoma, was first described by Isaacson and Wright in 1983 [1]. MALT lymphomas are most frequently found in the stomach, and have been shown to be closely associated with Helicobacter pylori (H. pylori) infection [2-4]. Colorectal lymphomas are rare, accounting for only 5-10% of all gastrointestinal lymphomas. Primary rectal MALT lymphomas are even rarer, therefore, their treatment has not been well-studied and there is no established standard therapy. Recent reports have documented the disappearance of rectal MALT lymphomas following H. pylori eradication therapy [5-16], however, this remains controversial, and it is yet to be clarified whether complete histological disappearance of rectal MALT lymphomas can be achieved following H.pylori eradiation therapy, since all previous reports are based on evaluation of only the endoscopic findings. We performed ESD and evaluated the disappearance of the lesions histopathologically. We encountered a patient in whom complete histopathological disappearance of a rectal MALT lymphoma was achieved by eradication therapy.
Case Report
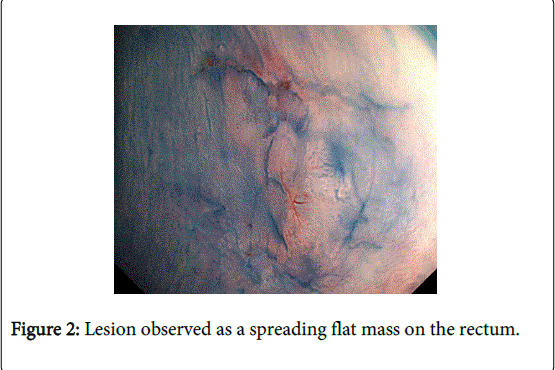
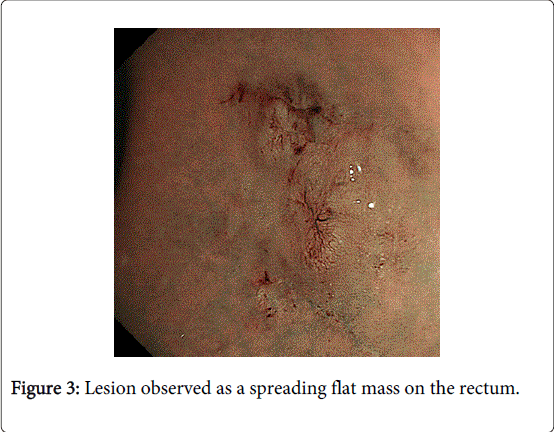
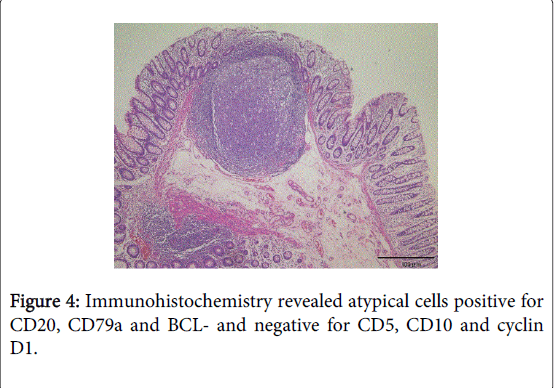
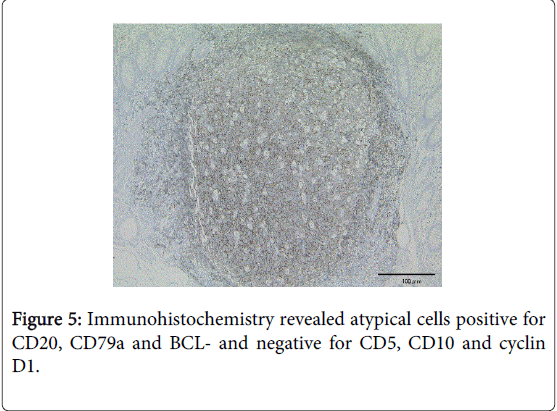
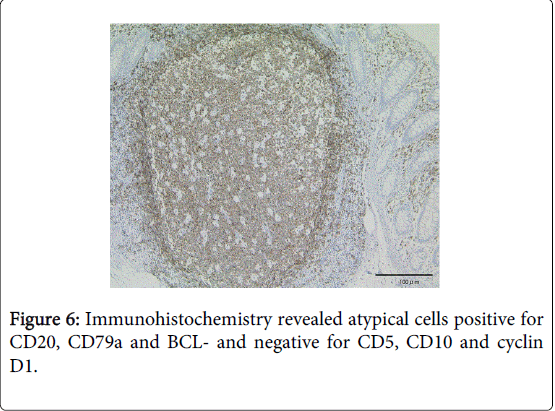
In a 77-year-old Japanese housewife who had been undergoing regular follow-up colonoscopy for a colon polyp, a total colonoscopy at another hospital showed an elevated lesion in the rectum. The lesion was observed as a spreading flat mass on the rectum (Figures 1-3). Immunohistochemistry revealed atypical cells positive for CD20, CD79a and BCL- and negative for CD5, CD10 and cyclin D1 (Figures 3-6).
A diagnosis of MALT lymphoma was made and the patient was referred to Yokohama City University Hospital. Physical examination and hematological examination at admission revealed no abnormalities.
A repeat colonoscopy at our hospital revealed a flat spreading mass lesion in the rectum measuring 15 mm in diameter, and magnifying endoscopy with narrow-band imaging revealed partial disappearance of the normal pit pattern and an abnormal vascular pattern on the nodule.
Abdominal computed tomography revealed no metastatic lesions, therefore, the patient was diagnosed as having clinical stage 1 (Lugano staging system) disease. We elected to administer antibiotic therapy, because the serological test for anti-H. pylori IgG antibody and H. pylori culture of biopsy specimens from the gastric mucosa were positive.
The eradication therapy selected was triple therapy, as follows: oral lansoprazole 60 mg/day, oral amoxicillin (AMPC) 1500 mg/day, and oral clarithromycin (CAM) 400 mg/day for 7 days.
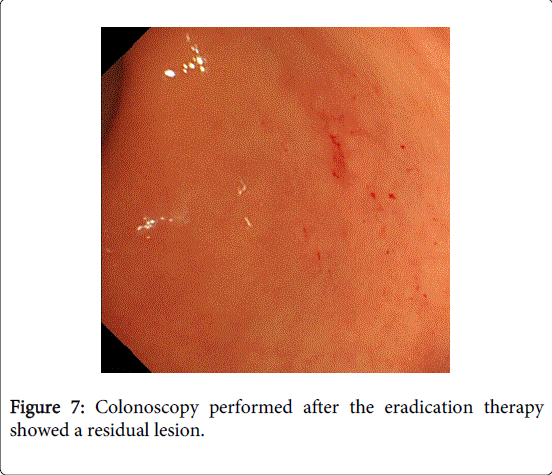
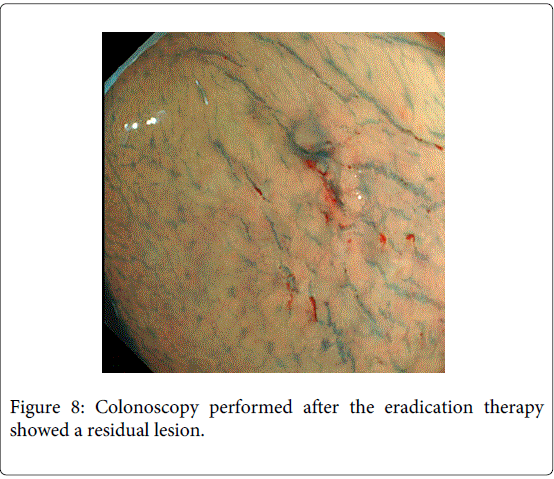
We performed the urea breath test and confirmed that the antibiotic therapy was successful, however, colonoscopy performed after the eradication therapy showed a residual lesion (Figures 7 and 8).
Histologic examination can’t deny the possibility the presence of residual MALT lymphoma. Endoscopic ultrasonography revealed that the lesion was confined to the mucosa. We performed endoscopic submucosal dissection (ESD) and histopathological examination of the ESD specimen showed complete disappearance of the lesion.
The ESD specimen showed aggregated lymphocytes in the lamina propria, however, the distribution of the CD3 and CD20 positive cells was normal and the specimen showed no evidence of the MALT lymphoma.
Until now, 1 year since the H.pylori eradication therapy, the patient has had an uneventful clinical course.
Discussion
The relationship between gastric MALT lymphoma and H. pylori infection has been clearly established. Low-grade gastric MALT lymphomas have been reported to regress after H. pylori eradication therapy [17]. However, it is still unclear whether colorectal MALT lymphoma is related to H. pylori infection and whether H. pylori eradication therapy is effective against colorectal MALT lymphomas. Recent reports have documented the disappearance of rectal MALT lymphomas by H. pylori eradication therapy [5-16], but it remains controversial as to whether H.pylori eradication therapy can cause complete histopathological disappearance of rectal MALT lymphomas, as most previous reports are based on the evaluation of only endoscopic findings.
In conclusion, we encountered a patient in whom complete histopathological disappearance of a rectal MALT lymphoma was achieved by H.pylori eradication therapy. We performed ESD and evaluated the lesion histopathologically. Our findings suggest that H. pylori eradication therapy is effective against rectal MALT lymphoma and that the eradication therapy can induce complete histopathological disappearance of the lesions. We recognize that our findings need to be confirmed in further studies carried out in a larger number of patients.
References
- Isaacson PG (1999) Mucosa-associated lymphoid tissue lymphoma. Semin Hematol 36: 139-147.
- Wotherspoon AC Doglioni C, Diss TC, Pan L, Moschini A, et al. (1993) Regression of primary low-grade B-cell gastric lymphoma of mucosa-associated lymphoid tissue type after eradication of Helicobacter pylori. Lancet 342: 575-577.
- Wotherspoon AC (1998) Helicobacter pylori infection and gastric lymphoma. Br Med Bull 54: 79-85.
- Wotherspoon AC (1998) Gastric lymphoma of mucosa-associated lymphoid tissue and Helicobacter pylori. Annu Rev Med 49: 289-299.
- Ahlawat S Kanber Y, Charabaty-Pishvaian A, Ozdemirli M, Cohen P, et al. (2006) Primary mucosa-associated lymphoid tissue (MALT) lymphoma occurring in the rectum: a case report and review of the literature. South Med J 99: 1378-1384.
- Tanaka S Ohta T, Kaji E, Kosaka T, Murakami I (2003) EMR of mucosa-associated lymphoid tissue lymphoma of the rectum. Gastrointest Endosc 57: 956-959.
- Matsumoto T, Iida M, Shimizu M (1997) Regression of mucosa-associated lymphoid-tissue lymphoma of rectum after eradication of Helicobacter pylori. Lancet 350: 115-116.
- Matsumoto T Shimizu M, Iida M, Amano K, Nakamura S, et al. (1998) Primary low-grade, B-cell, mucosa-associated lymphoid tissue lymphoma of the colorectum: clinical and colonoscopic features in six cases. Gastrointest Endosc 48: 501-508.
- Inoue F, Chiba T (1999) Regression of MALT lymphoma of the rectum after anti-H. pylori therapy in a patient negative for H. pylori. Gastroenterology 117: 514-515.
- Niino D Yamamoto K, Tsuruta O, Maeda T, Yakushijin Y, et al. (2010) Regression of rectal mucosa-associated lymphoid tissue (MALT) lymphoma after antibiotic treatments. Pathol Int 60: 438-442.
- Hisabe T, Imamura K, Furukawa K (2002) Regression of CD5-positive and Helicobacter pylori-negative mucosa-associated lymphoid tissue lymphoma of the rectum after administration of antibiotics: report of a case. Dis Colon Rectum 45: 1267-1270.
- Nakase H Okazaki K, Ohana M, Ikeda K, Uchida K, et al. (2002) The possible involvement of micro-organisms other than Helicobacter pylori in the development of rectal MALT lymphoma in H. pylori-negative patients. Endoscopy 34: 343-346.
- Hori K Suguro M, Koizuka H, Sakagami T, Tomita T, et al. (2004) Disappearance of rectal mucosa-associated lymphoid tissue lymphoma following antibiotic therapy. Dig Dis Sci 49: 413-416.
- Kikuchi Y, Matsui T, Hisabe T (2005) Deep infiltrative low-grade MALT (mucosa-associated lymphoid tissue) colonic lymphomas that regressed as a result of antibiotic administration: endoscopic ultrasound evaluation. J Gastroenterol 40: 843-847.
- Ahlawat S Haddad N, Kanber Y, Cohen P, Ozdemirli M, et al. (2005) Primary mucosa-associated lymphoid tissue lymphoma occurring in the rectum. Gastrointest Endosc 62: 443-444.
- Dohden K, Kaizaki Y, Hosokawa O (2004) Regression of rectal mucosa-associated lymphoid tissue lymphoma but persistence of Helicobacter pylori infection of gastric mucosa after administration of levofloxacin: report of a case. Dis Colon Rectum 47: 1544-1546.
- Takenaka R Tomoda J, Sakata T, Ichiba T, Motoi M, et al. (2000) Mucosa-associated lymphoid tissue lymphoma of the rectum that regressed spontaneously. J Gastroenterol Hepatol 15: 331-335.
Relevant Topics
- Constipation
- Digestive Enzymes
- Endoscopy
- Epigastric Pain
- Gall Bladder
- Gastric Cancer
- Gastrointestinal Bleeding
- Gastrointestinal Hormones
- Gastrointestinal Infections
- Gastrointestinal Inflammation
- Gastrointestinal Pathology
- Gastrointestinal Pharmacology
- Gastrointestinal Radiology
- Gastrointestinal Surgery
- Gastrointestinal Tuberculosis
- GIST Sarcoma
- Intestinal Blockage
- Pancreas
- Salivary Glands
- Stomach Bloating
- Stomach Cramps
- Stomach Disorders
- Stomach Ulcer
Recommended Journals
Article Tools
Article Usage
- Total views: 14130
- [From(publication date):
April-2015 - Nov 21, 2024] - Breakdown by view type
- HTML page views : 9704
- PDF downloads : 4426