Compartment Syndrome of the Foot Following Ankle Open Reduction and Internal Fixation - A Case Report
Received: 07-Jan-2022 / Manuscript No. CRFA-21-50540 / Editor assigned: 10-Jan-2022 / PreQC No. CRFA-21-50540 (PQ) / Reviewed: 17-Jan-2022 / QC No. CRFA-21-50540 / Revised: 24-Jan-2022 / Manuscript No. CRFA-21-50540 (R) / Accepted Date: 27-Jan-2022 / Published Date: 31-Jan-2022 DOI: 10.4172/2329-910X.1000326
Abstract
Compartment syndrome of the foot is an extremely rare complication following ankle open reduction and fixation (ORIF). The first clinical manifestations following compartment syndrome include pain out of proportion and on passive stretch. We present a rare case of compartment syndrome following ankle ORIF using general anesthesia and a sciatic nerve block where the patient’s initial complaint was plantar paraesthesia. Pressure testing revealed increased foot osseo-fascial compartment pressures treated with open fasciotomy. To our knowledge this represents the first reported case of compartment syndrome in the foot requiring fasciotomy after ankle open reduction and internal fixation.
Keywords: Internal Fixation; Anesthesia; Fasciotomy; Tomography
Keywords
Internal Fixation; Anesthesia; Fasciotomy; Tomography
Case Report
A 49-year-old female stepped off a low platform at home sustaining an injury to the right ankle, resulting in immediate pain, swelling, and inability to weight bear. She presented to the emergency department via ambulance. Examination ninety minutes post-injury documented a closed injury with swelling of the ankle joint. Sensation of the superficial and deep peroneal, saphenous, sural, medial, and lateral plantar nerves was normal. Furthermore, she demonstrated active flexion and extension of the hallux and lesser toes, capillary refill time of the right hallux was less than two seconds and the dorsalis pedis pulse was palpable.
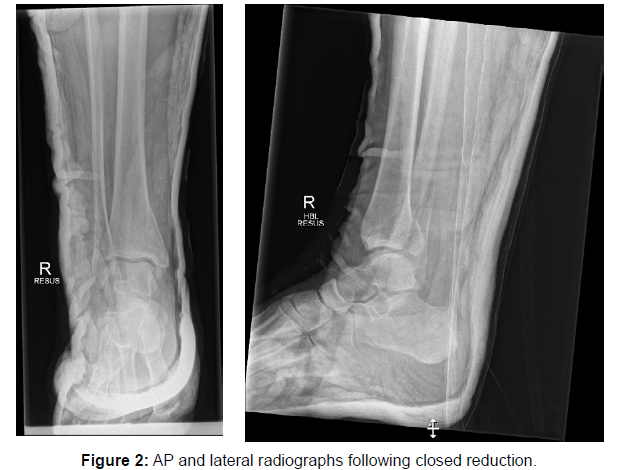
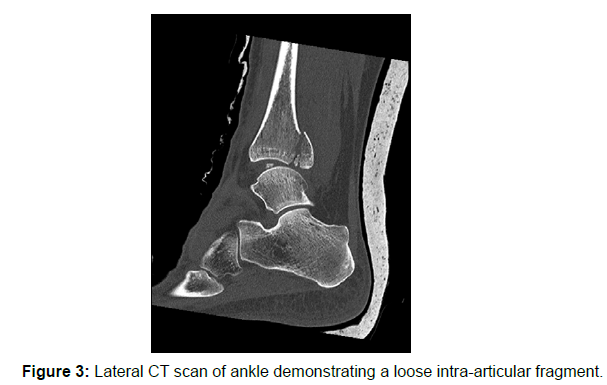
An initial radiograph demonstrated comminuted fractures of the distal tibia and fibula with talar shift (Figure 1). Immediate closed reduction of the ankle followed by application of a below knee ankle back slab was performed successfully, with the use of intravenous midazolam. Post-reduction radiographs demonstrated satisfactory reduction (Figure 2). Following this, the patient reported some paraesthesia in the right toes. On review, the right toes appeared dusky with a capillary refill time of approximately five seconds. The back slab was loosened, with a return of capillary refill time and normal sensation. A computed-tomography (CT) scan was performed to further characterise the fractures for operative planning and revealed a 14 mm intra-articular loose bone fragment as well as several other tiny intra-articular loose bodies (Figure 3). The patient was admitted to an orthopaedic ward, with the limb elevated using a James pillow with regular neurovascular observations and analgesia.
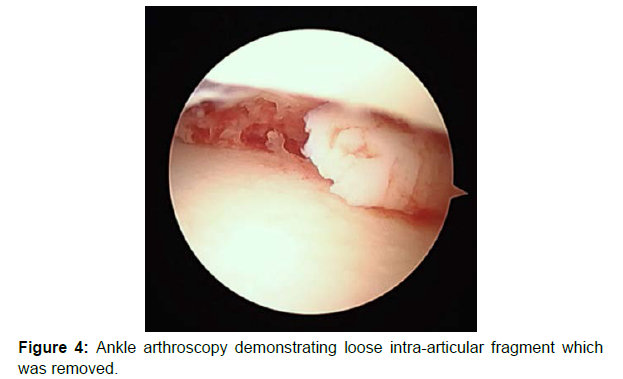
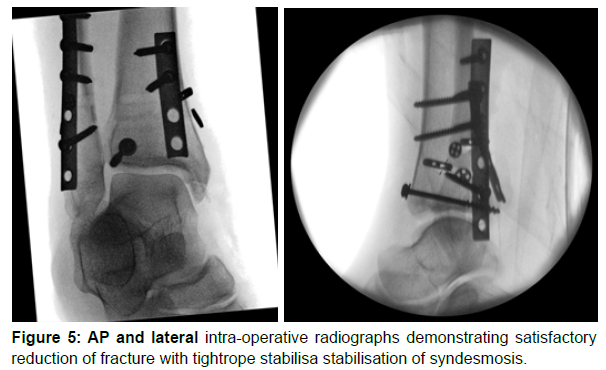
The patient underwent an ankle arthroscopy, open reduction, and internal fixation four days later. The procedure was performed und general anesthesia at approximately 3 pm. additionally, an ultrasoundguided adductor canal block was performed, and the sciatic nerve (proximal, anterior approach using a landmarks and nerve stimulator technique) was blocked using 25 ml 0.375% ropivacaine. A tourniquet was applied to the right thigh and inflated to 300mmHg. The ankle arthroscopy was performed with the irrigation solution under gravity pressure without pumping. This revealed a large osteochondral fragment which was removed and a lateral mid talar dome chondral lesion (Figure 4). A lateral approach was performed through the lateral malleolus fracture the posterior malleolus was reduced. This was percutaneous fixed using an interfragmentary screw (4.5 mm/20 mm) and washer. The lateral malleolus fracture was anatomically reduced, and a six-hole one-third tubular antiglide plate was applied to the poster lateral aspect of the lateral malleolus and fixed with screws. A posteromedial incision was performed and the tibialis posterior tendon was mobilised posteriorly. A four-hole one-third tubular antiglide plate was applied to the posterior medial malleolus and fixed with screws. Intra-operative stress testing revealed tibio-fibular diastasis. This was reduced with a tibio-fibula clamp and two syndesmotic sutureendobuttons were inserted. The tourniquet was released. The wounds were closed in layers with 2-0 vicryl (subcutaneous) and 3-0 stratafix plus (subcuticular) sutures. Dressings and a boot were applied. The total tourniquet time was 56 minutes. The patient had an uncomplicated return to the orthopaedic ward post-operatively was instructed to nonweight bear. Intra-operative radiographs demonstrated satisfactory reduction (Figure 5).
On day 1 post-operation, the patient noticed worsening medial and lateral ankle pain as expected with the sciatic nerve block starting to wear off. This pain was relieved with slow release tape) ntadol. However, while all other aspects of her foot showed a sensory return to normal, the patient also noted a tingling sensation and neuropathictype pain especially in the plantar aspect of toes 2-5, as well as the dorsal aspect of the toes. This was first felt at approximately 4 am and continued over several hours, but Liu X-d later in the afternoon turned into a loss of sensation in this area. On examination there was no overt oozing and as expected there was mild swelling around the medial and lateral incisions. There was no swelling around the foot. Sensation was densely altered at the plantar aspect of the first, second, third, fourth and fifth toes and at the dorsal aspect of the third, fourth and fifth toes with mildly altered sensation in the dorsal first web space and normal sensation in the medial border of the hallux. The patient tolerated passive dorsiflexion of the hallux, second and fourth toes with only mild pain around the ankle and not in the foot which may have been as a result of interrogating calf rather than foot muscle passive stretch.
Differential Diagnosis
The anesthetist was also consulted. However, due to the distribution of numbness in only the area of one distinct peripheral nerve (tibial posterior) and the spread of numbness over the next hour from the sole into the toes, as well as the onset of neuropathic pain in the same area, the anaesthetist was not convinced that the examination findings were consistent with nerve injury secondary to the sciatic nerve block. Differential diagnoses at the time included a haematoma compressing the tarsal tunnel ora compartment syndrome. A joint decision between the patient, surgeon and anaesthetist was to return to theatre for exploration of the medial wound, compartment pressure testing, and consideration of fasciotomy.
Treatment
On return to theatre the limb was prepped and draped without a tourniquet. The medial wound was opened and minimal haematoma found. Compartment pressures were then measured using a 16G needle connected to a pressure monitor by sterile tubing. This was zeroed to atmosphere at the level of leg. Compartment pressures in the leg were 10mmhgwhereas those measured in the foot are shown in Table 1. The patient had a diastolic blood pressure of 40 mmHg with pre-release pressures recorded at 60mmHg for interosseous, 30mmHg medial, 10mmHg lateral and 10mmHg central compartments respectively. The medial wound incision was then extended distally, and the tarsal tunnel released to the level of abductor hallucis, its fascia released, and muscle mobilised off the deep plantar fascia. The medial plantar nerve was identified and protected, and the deep fascia identified and released. Compartment pressures were retested, and all were 30mmHg lower than the patient’s diastolic blood pressure. A negative pressure dressing was applied to the wound.
| Compartment | Interosseous | Medial | Lateral | Central |
|---|---|---|---|---|
| Pre-release pressure (mmHg) | 60 | 30 | 10 | 10 |
| Post-release pressure (mmHg) | 14 | 6 | 3 | 2 |
Table 1: Pre-release and post-release foot compartment pressures.
On returning to the ward, the patient’s foot had normal colour and a capillary return time of less than two seconds. Sensation in the dorsomedial branch of the hallux was normal, at the dorsolateral was altered but present, at the dorsomedial aspect of the second toe was normal, at the dorsolateral aspect of the second toe was abnormal but present, at the third toe was normal and altered at the dorsal of the fourth and fifth toes. She demonstrated active flexion of the hallux and lesser toes. At 10 days post-fasciotomy, the medial wound was debrided and closed in a staged manner using interrupted 3-0 nylon sutures.
Outcome and Follow-Up
At two months post-fasciotomy, the patient’s sensation remained densely altered in the third toe with the second toe improving. The fractures went on to radiographic union without complication. The medial plate was removed due to concerns with tibialis posterior tendon irritation. Nerve conduction studies were performed demonstrating tibial nerve neuropathy at the level of the tarsal tunnel and not the sciatic nerve. At 4 months post-fasciotomy, sensation in the third toe was gradually improving and there was normal posture of the lesser toes indicating no residual effect because of the compartment syndrome. At 12 months post-fasciotomy, the patient has full sensation, can fully weight bear without pain and is able to participate in hiking.
Discussion
Foot compartment syndrome is a very rare entity following an ankle fracture and has been seldom reported in the literature which warrants sharing with colleagues. To date, there has only been two published cases of foot compartment syndrome secondary to an ankle fracture and no reports requiring foot fasciotomies. The first reported case was detailed in a Chinese (traditional) language journal by Liu et al. [1] who described compartment syndrome of the foot following a Weber B fracture-dislocation [1]. Guo et al [2] described compartment syndrome of the foot following open reduction and internal fixation of a bimalleolar ankle fracture with resolution of compartment pressures recorded after wounds decompressed so that no fasciotomy was required [2].
Compartment syndrome of the foot results when the osseofascial compartment pressure increases to a level which impairs perfusion potentially resulting in irreversible muscle and neurovascular damage. Foot compartment syndrome is typically associated with Chopart and Lisfranc joint dislocations and is rarely observed following isolated midfoot fractures [3,4]. The main symptoms which manifest compartment syndrome include pain, paraesthesia, and paresis, pain that worsens with the passive motion of the toes, pallor skin colour and poor or absent peripheral pulses [5,6]. Additionally, firmness and decreased compressibility of the compartments is often present [7]. Needle compartment pressures are diagnostic in cases of inconclusive physical exam findings and in sedated patients. Diagnosed compartment syndrome of the foot requires immediate fasciotomy to release pressure from the affected compartment. The earlier a manifest compartment is released, the less likely that long-term complications will develop. McQueen et al. [8] demonstrated that the time between apparent onset of compartment syndrome and surgical release influenced the outcome rather than the time between trauma and fracture stabilisation in patients with tibial fractures [9].
The time between the onset of symptoms and definitive treatment, tourniquet time and use of a sciatic nerve block may have been contributing factors which resulted in the development of foot compartment syndrome and subsequent neuropraxia in this case. There is strong evidence in the literature that early surgical fixation of ankle fractures results in the best post-operative outcomes provided there are no pre-operative adverse features including blisters or gross swelling. Fixation of ankle fractures within 24 hours has been shown to result in lower wound infection rates, post-operative length of hospital stay, loss of fixation and general post-operative complications (such as deep vein thrombosis and pulmonary embolus) [10-12]. In our case, the patient underwent a timely closed reduction and operative fixation within 24 hours of injury.
Nerve injury is the most common complication of tourniquet use [13]. Furthermore, prolonged tourniquet time is associated with increased risk of compartment syndrome [14]. There are no guidelines relating to the safe duration and pressure for tourniquet use in orthopaedic surgery. However, the literature suggests a safe time limit of 1 to 3 hours [15]. There is a strong correlation between total tourniquet time and nerve injury, with a 30 minute increase in tourniquet inflation time resulting in a threefold increase in neurological complications [16]. The use of tourniquet for more than 2 hours and pressures of above 350mmHg in lower limb surgery has been shown to increase risk of compression neurapraxia and compartment syndrome. If the tourniquet time required exceeds 2 hours, the tourniquet should be deflated for 5 minutes for every 30 minutes of inflation time [17]. Additionally, there have been no reports of the use of a thigh tourniquet resulting in interosseus compartment syndrome, likely due to being distal to site of tourniquet application. There have been reported cases of anterior thigh compartment syndrome following the use of a thigh tourniquet [14,18]. In our case, the tourniquet time was 56 minutes with a pressure of 300mmHg which is within limits of a typical ankle open reduction internal fixation procedure published in the literature and not a major contributing factor this patient’s morbidity [19].
To the best of our knowledge, this compartment syndrome in the foot after ankle surgery is an extremely rare condition and this case report is possibly the only one in the English language literature. Correspondingly, it is not surprising that the recognition of the condition did initially present some difficulty. The appreciation of clinical findings was also delayed by the fact that the patient had received a sciatic nerve block. Though the nerve block ultimately did not obscure the clinical signs of our patient’s condition, it presented a confounding explanation for some of the observed symptoms. The patient’s primary post-operative symptom was neuropathic pain followed by paraesthesia at the plantar aspect of the foot. Later in the afternoon the formerly painful aspects turned into loss of sensation, likely consistent with proceeding nerve damage. Typically, the first manifesting symptom is severe pain, which is out of proportion which may be less useful in the periphery. Furthermore, the patient did not demonstrate any pain on passive stretch on examination [20]. Potential complications related to distal sciatic nerve blocks include infection at the injection site, bleeding, nerve injury, and local anaesthetic toxicity. A systematic review of 18 upper and limb compartment syndrome cases, including a case of revisional arthroplasty of the forefoot by Elazab et al [21] demonstrated that peripheral nerve blocks do not affect pain perception in acute compartment syndrome, with all cases presenting with severe pain [21]. Conversely Mar et al’s review of 35 cases of lower limb acute compartment syndrome demonstrated that 32 out of 35 patients had the classic signs and symptoms of compartment syndrome were present [22].
Though there is reasonably good indication that blocks do not mask compartment syndrome, it is vitally important to very carefully evaluate symptoms and patient complaints as some may be related to the block (or may easily be attributed to the block) and also because pain may not always be the cardinal symptom of foot compartment syndrome.
Conclusion
Compartment syndrome of the foot is an extremely rare complication following ankle fixation. The cardinal signs and symptoms associated with the syndrome may be concealed, particularly if the patient has received a peripheral nerve block. Regardless of the type of analgesia used, a high index of clinical suspicion, ongoing assessment of the patient at different time points and compartment pressure measurement are essential for early diagnosis and treatment to optimize final outcomes.
References
- Liu XD, Xie YB, Zhang XJ (2008) Weber B fracture-dislocation of the ankle with compartment syndrome of the foot: a case report. China J Orthop Traumatol 21: 628-628.
- Guo S, Sethi D, Prakash D (2010) Compartment syndrome of the foot secondary to fixation of ankle fracture - A case report. Foot Ankle Surg 16: e72-e75.
- Richter M, Wippermann B, Krettek C, Schratt HE, Hufner T, et al. (2001) Fractures and fracture dislocations of the midfoot: occurrence, causes and long-term results. Foot Ankle Int 22: 392-398.
- Frink M, Geerling J, Hildebrand F, Knobloch K, Zech S, et al. (2006) Etiology, treatment and long-term results of isolated midfoot fractures. Foot Ankle Surg 12: 121-125.
- Griffiths D L (1948) The management of acute circulatory failure in an injured limb. J Bone Joint Sur 30: 280-289.
- Cascio BM, Wilckens JH, Ain MC, Toulson C, Frassica FJ (2005) Documentation of acute compartment syndrome at an academic health-care center. JBJS 87: 346-350.
- Frink M, Hildebrand F, Krettek C, Brand J, Hankemeier S (2010) Compartment syndrome of the lower leg and foot. Clin Orthop Relat Res 468: 940-950.
- McQueen MM, Christie J, Court-Brown CM (1990) Compartment pressures after intramedullary nailing of the tibia. J Bone Joint Surg 72: 395-397.
- McQueen MM, Christie J, Court-Brown CM (1996) Acute compartment syndrome in tibial diaphyseal fractures. J Bone Joint Surg 78: 95-98.
- Singh R A, Trickett R, Hodgson P (2015) Early versus late surgery for closed ankle fractures. J Orthop Surg 23: 341-344.
- Konrath G, Karges D, Watson JT, Moed BR, Cramer K (1995) Early versus delayed treatment of severe ankle fractures: a comparison of results. J Orthop Trauma 9: 377-380.
- Schepers T, De Vries MR, Van Lieshout EM, Van der Elst M (2013) The timing of ankle fracture surgery and the effect on infectious complications; a case series and systematic review of the literature. Int Orthop 37: 489-494.
- Estebe J (2011) Complications of tourniquet use.
- Seybold EA, Busconi BD (1996) Anterior thigh compartment syndrome following prolonged tourniquet application and lateral positioning. Am J Orthop (Belle Mead NJ) 25: 493-496.
- Pedowitz RA (1991) Tourniquet-induced neuromuscular injury: a recent review of rabbit and clinical experiments. Acta Orthop Scand 62: 1-33.
- Horlocker TT, Hebl JR, Gali B, Jankowski CJ, Burkle CM, et al. (2006) Anesthetic, patient, and surgical risk factors for neurologic complications after prolonged total tourniquet time during total knee arthroplasty. Anesth Analg 102: 950-955.
- Sharma JP, Salhotra R (2012) Tourniquets in orthopedic surgery. Indian J Orthop 46: 377-383.
- Koepplinger ME, Ellis LA, Davis KR (2011) Complicated thigh compartment syndrome. Curr Orthop Pract 22:116-121.
- Konrad G, Markmiller M, Lenich A, Mayr E, Rüter A (2005) Tourniquets may increase postoperative swelling and pain after internal fixation of ankle fractures. Clin Orthop Relat Res 433: 189-194.
- Elliott KG, Johnstone AJ (2003) Diagnosing acute compartment syndrome. J Bone Joint Surg 85: 625-632.
- Elazab A, Abd-Elgawad A, Attia M (2018) Peripheral Nerve Block: Does it Affect Pain Perception in Acute Compartment Syndrome? A Systematic Review. J orthop rheumatol 12: 72-77.
- Mar GJ, Barrington MJ, McGuirk BR (2009) Acute compartment syndrome of the lower limb and the effect of postoperative analgesia on diagnosis. Br J Anaesth 102: 3-11.
Indexed at Google Scholar Crossref
Indexed at Google Scholar Crossref
Indexed at Google Scholar Crossref
Indexed at Google Scholar Crossref
Indexed at Google Scholar Crossref
Indexed at Google Scholar Crossref
Indexed at Google Scholar Crossref
Indexed at Google Scholar Crossref
Indexed at Google Scholar Crossref
Indexed at Google Scholar Crossref
Indexed at Google Scholar Crossref
Citation: Moniz S, Sobhi S, Ledowski T, Blythe M (2022) Compartment Syndrome of the Foot Following Ankle Open Reduction and Internal Fixation - A Case Report. Clin Res Foot Ankle, 10: 326. DOI: 10.4172/2329-910X.1000326
Copyright: © 2022 Moniz S, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.