Comparison of Short-Term Outcome between Laparoscopic and Open Appendectomy in Adults: A Meta-Analysis of Randomized Controlled Trials
Received: 27-Oct-2017 / Accepted Date: 20-Nov-2017 / Published Date: 22-Nov-2017 DOI: 10.4172/2476-2024.1000131
Abstract
Objective: Despite many randomized controlled trials, it is still not clear whether open appendectomy or laparoscopic appendectomy is the most appropriate surgical approach to acute Appendicitis. It is also widely recognized that laparoscopic removal of appendectomy is a well-established procedure with good outcomes. The aim of this study was to evaluate the short-term results of open appendectomy versus laparoscopic appendectomy in adults.
Methods: We undertook a meta-analysis of randomized controlled trials comparing open appendectomy and laparoscopic appendectomy in adults. We searched the PubMed, EMBASE, and Cochrane Library databases up to June 20, 2017. Calculations were made of the effect sizes of short-term outcomes: wound infection, intra-abdominal abscess, postoperative complications, peritonitis, postoperative ileus, urinary tract infection, and reoperation, the effect sizes were then pooled by a fixed or random-effects model.
Results: Twenty-nine randomized controlled trials with 4311 participants were included. Meta-analysis of the available literature demonstrated that laparoscopic appendectomy in adults was associated with lower incidence of wound infection (OR=0.54, 95% CI: 0.42-0.70, P<0.00001), and fewer postoperative complications (OR=0.77, 95% CI: 0.66-0.90, P= 0.001). Further analysis did not reveal significant differences between the two surgery approaches in intra-abdominal abscess, peritonitis, postoperative ileus, urinary tract infection, and reoperation in adults.
Conclusion: Laparoscopic appendectomy reduces wound infections and postoperative complications in the treatment of adult acute appendicitis. Laparoscopic appendectomy is worth recommending as an effective and safe procedure for acute appendicitis in adults.
Keywords: Appendectomy; Laparoscopic surgery; Open surgery; Meta-analysis
Introduction
Appendicitis is the most common cause for acute abdominal pain with a life-time incidence between 6.7% and 8.6% [1,2]. It is also the most common emergency in abdominal surgery [3]. Since 1889, when Mc Burney first reported appendectomy as the treatment for acute appendicitis, surgical intervention has been the standard treatment strategy for acute appendicitis [4]. Open appendectomy (OA) performed through the right lower quadrant incision was first described in 1894. It has become the standard treatment of choice for acute appendicitis, remaining mainly unchanged for 100 years due to its favorable efficacy and safety. The evolution of Endoscopic surgery led to the idea of performing appendectomy via laparoscopy; this was first described by Semm in 1983 [5]. It’s has gradually gained acceptance. However, there remains a continuing controversy in the literature regarding the most appropriate method of removing the inflamed appendix.
Endoscopic techniques have been recommended reportedly because of their lesser invasiveness, fewer complications and overall better results compared to open appendectomy techniques [6-8]. However, several randomized controlled trials comparing laparoscopic with open appendectomy have provided conflicting results [9,10]. Previous studies have demonstrated better clinical short-term outcomes with the laparoscopic approach [11-13], while other studies have shown marginal or no short-term clinical benefits [14-16]. Bearing in mind that laparoscopic appendectomy, unlike other laparoscopic procedures, has not been found superior to open surgery for acute appendicitis [17]. Therefore, we conducted the present meta-analysis to compare the short-term outcomes (wound infection, intra-abdominal abscess, postoperative complications, peritonitis, postoperative ileus, urinary tract infection, and reoperation) between open appendectomy and laparoscopic appendectomy (LA) in adults.
Methods
Study search
We conducted a search of PubMed, EMBASE, and Cochrane Library databases till August 25, 2017 using a mix of the following keywords: appendicitis, appendectomy, laparoscopic, and laparoscopic and open appendectomy/appendicectomy. Two investigators independently reviewed all relevant studies. Eligible trials were then selected according to the inclusion criteria below. Discrepancies were resolved, if necessary, by discussion and consulting a senior reviewer.
Inclusion and exclusion criteria: Published randomized controlled trials researches are going to be involved in the present meta-analysis on reaching the criteria as follows:
(a) A prospective randomized study format only. (b) A comparison of laparoscopic and open appendectomy. (c) The study reported at least one of the desirable outcomes mentioned below. (d) Studies with human adult participants.
Key omission criteria included:
(a) Non-randomized studies. (b) Pediatric participants. (c) When replicated researches were published, merely the research having huge specimen size was involved.
Data extraction and quality assessment: Two authors independently extracted data from all eligible studies: first author, country, year of publication, sex of subjects, age, size of the appendectomy (laparoscopic vs. open). The Jadad scale was used to evaluate the overall quality of all included articles [18]. According to Kjaergard et al. recommendation, low-quality studies have a score of ≤ 2 and highquality studies have a score of ≥ 3 (Table 1) [19].
| Author | Year | Country | Case | Mean Age (y) | Sex (male/female) | *Outcomes | Jadad Score | |||
|---|---|---|---|---|---|---|---|---|---|---|
| LA | OA | LA | OA | LA | OA | |||||
| Al-Mulhim | 2002 | Saudi Arabia | 30 | 30 | 23 | 26 | all woman | all woman | 1,7 | 3 |
| Cipe | 014 | Turkey | 121 | 120 | 27 | 30 | 65/56 | 71/49 | 1,2,7 | 3 |
| Clarke | 2011 | USA | 23 | 14 | 31 | 33 | 15 | 09 | 1,2,3,4,7 | 3 |
| Cox | 1996 | Australian | 33 | 31 | 25 | 25 | all man | all man | 1,5,7 | 3 |
| Hansen | 1996 | Australian | 79 | 72 | 25 | 22 | 32/52 | 25/49 | 1,4,5,7 | 4 |
| Hellberg | 1999 | Sweden | 244 | 256 | NA | NA | NA | NA | 1,3,4,6,7 | 5 |
| Ignacio | 2004 | USA | 26 | 26 | 28 | 27 | all man | all man | 1,7 | 4 |
| Kald | 1999 | Sweden | 49 | 50 | 24 | 32 | 28/21 | 21/29 | 1,3,7 | 4 |
| Kaplan | 2009 | Tuikey | 50 | 50 | 24 | 26 | 33/17 | 31/19 | 1,2,6,7 | 4 |
| Kargar | 2010 | Iran | 50 | 50 | 27 | 25 | 23/27 | 28/22 | 1,7 | 4 |
| Katkhouda | 2005 | USA | 113 | 134 | 29 | 28 | 78/35 | 104/30 | 1,2,4,7 | 5 |
| Khalil | 2011 | Pakistan | 72 | 75 | 23 | 23 | 40/32 | 44/31 | 1,4,7 | 5 |
| Klingler | 1998 | Australian | 87 | 82 | 30 | 24 | 44/43 | 39/43 | 1,2,4,6,7 | 2 |
| Kocatas | 2013 | Istanbul | 50 | 46 | 27 | 28 | 27/23 | 44/4 | 1,2,4,6,7 | 4 |
| Laine | 1997 | Finland | 25 | 25 | 27 | 28 | all women | all women | 1,4,7 | 2 |
| Long | 2001 | USA | 93 | 105 | NA | NA | NA | NA | 1,2,7 | 4 |
| Macarulla | 1997 | Spain | 106 | 104 | 27 | 29 | 42/64 | 48/56 | 1,2,5,6,7 | 4 |
| Martin | 1995 | USA | 81 | 88 | 27 | 29 | 51/37 | 49/32 | 1,2,7 | 2 |
| Mantoglu | 2015 | Turkey | 31 | 32 | 32 | 31 | 14/17 | 21 | 1,7 | 3 |
| Moberg | 2005 | Sweden | 81 | 82 | 31 | 31 | 46/35 | 58/24 | 1,4,5,7 | 5 |
| Moirangthem | 2008 | Indian | 25 | 25 | 31 | 35 | 19 | 17 | 1,7 | 2 |
| Mutter | 1996 | France | 50 | 50 | 29 | 27 | all man | all man | 1,2,7 | 3 |
| Ozmen | 1999 | Turkey | 35 | 35 | 23 | 28 | 17/18 | 15/20 | 1,4,7 | 2 |
| Pedersen | 2001 | Denmark | 282 | 301 | 26 | 27 | 131/151 | 143/158 | 1,2,4 | 4 |
| Reiertsen | 1997 | Norway | 42 | 42 | 34 | 33 | 31/11 | 26/16 | 1,2,6,7 | 3 |
| Shirazi | 2010 | Karachi | 30 | 30 | 27 | 26 | 18 | 20 | 1,7 | 2 |
| Taguchi | 2016 | Japan | 42 | 39 | 46 | 49 | 28/14 | 25/14 | 1,2,3,6 | 5 |
| Tzovaras | 2010 | Greece | 72 | 75 | 26 | 22 | all man | all man | 1,2,4,7 | 5 |
| Wei | 2009 | China | 112 | 108 | 29 | 27 | 67/45 | 66/42 | 1,7 | 3 |
*Outcomes: 1) wound infection; 2) Intra-abdominal abscess; 3) peritonitis; 4) Postoperative ileus; 5) Urinary tract infection; 6) reoperation; 7) Postoperative complications. NA: Not Available
Table 1: Main Characteristics of 29 studies included in our meta-analysis.
Statistical analysis: The strength of association was calculated by risk ratios (RRs) with 95% confidence interval (CI), comparing the laparoscopic appendectomy group with the open appendectomy group. Use of the Q-test and I2 statistics was made for quantifying statistical heterogeneity. The use of random-effect framework was made once the heterogeneity was significant (P<0.05) or else, the fixed effects framework was utilized. The sensitivity analysis performed by sequentially excluding any individual researches one by one, with an objective of examining the impact of each individual research or summarized findings. Furthermore, use of the Begg’s funnel plot and the Egger’s test was made for estimating the publication bias (P
Results
Study characteristics
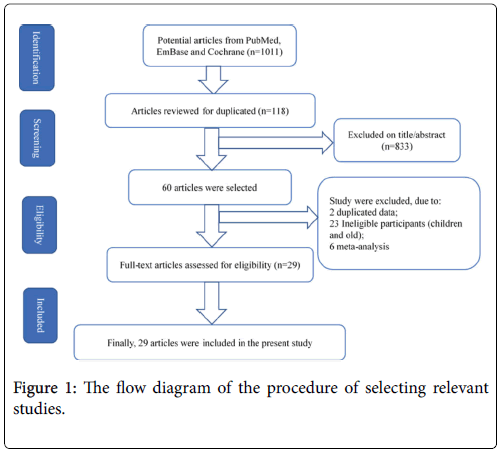
The selection mechanism of entitled research works has been displayed in Figure 1. 1011 considerably significant research works were primarily attained from databases of the PubMed, EBMASE, and Cochrane Library. After eliminating duplicate articles, we evaluated the titles and abstracts of these studies according to the inclusion and exclusion criteria, after which 61 articles remained. After the full texts of these articles were read and the ineligible studies were excluded, 29 randomized controlled trials involving 2134 laparoscopic appendectomy (LA), in addition to 2177 open appendectomy (OA) [10-15,19-41]. The characteristics of these studies are listed in the Table 1.
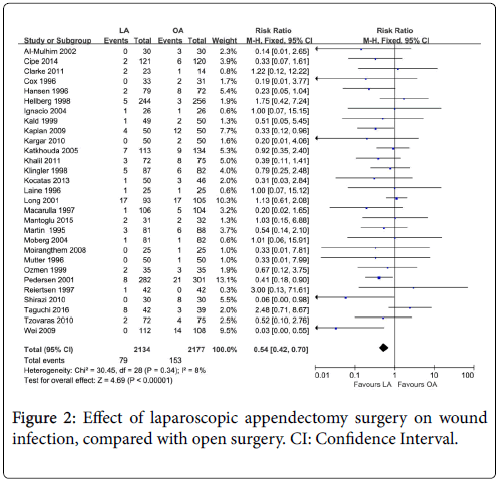
Wound infection
Twenty-nine studies and 4,311 participants (2,134 for laparoscopic appendectomy and 2,177 for open appendectomy) were included for this outcome. The total numbers of events were 79 in the laparoscopic appendectomy group (3.70%) and 153 in the open appendectomy group (7.03%). Wound infection significantly reduced with LA versus OA (OR=0.54, 95% CI: 0.42-0.70, P<0.00001). A fixed-effects model was used because there was no heterogeneity between the two groups (I2=8%, P=0.34) (Figure 2).
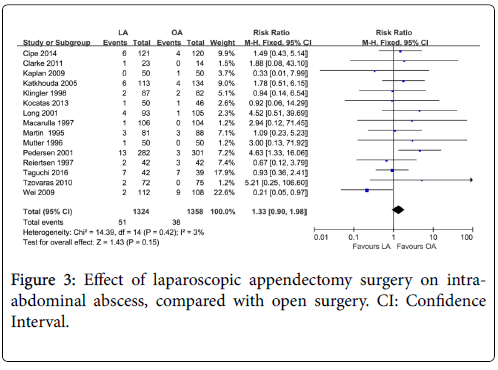
Intra-abdominal abscess
This outcome analysis included 15 relevant studies with a total of 2682 participants (1,324 for laparoscopic appendectomy and 1,358 for open appendectomy). 51 (3.85%) and 38 (3.80%) incidences of postoperative intra-abdominal abscess were seen in the laparoscopic and open appendectomy groups, respectively, and there was no significant difference between the two groups (OR=1.33, 95% CI: 0.90-1.98, P=0.15). A fixed-effects model was used because there was no heterogeneity between the two groups (I2=3%, P=0.42) (Figure 3).
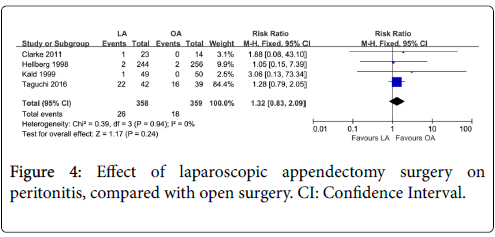
Peritonitis
There were 4 studies with a total of 717 participants (358 for laparoscopic appendectomy and 359 for open appendectomy) that compared the postoperative peritonitis between laparoscopic appendectomy and open appendectomy. 26 (7.26%) and 18 (5.01%) incidences of postoperative peritonitis were seen in the laparoscopic and open appendectomy groups, respectively, and there was no significant difference between the two groups (OR=1.32, 95% CI: 0.83-2.09, P=0.24). A fixed-effects model was used because there was no heterogeneity between the two groups (I2=0%, P=0.94) (Figure 4).
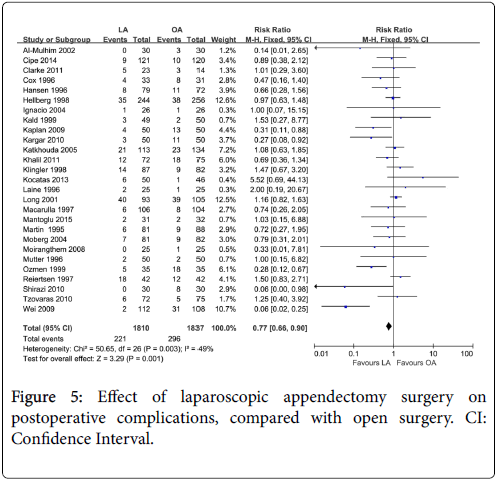
Postoperative complications
There were 27 studies with a total of 3,647 participants (1,810 for laparoscopic appendectomy and 1,837 for open appendectomy) that compared the postoperative complications between laparoscopic appendectomy and open appendectomy in adults. A fixed-effects model was used because there was no significantly heterogeneity between the two groups (I2=49%, P=0.003), and the results demonstrated that laparoscopic appendectomy was associated with a significantly reduced incidence of postoperative complications (OR=0.77, 95% CI: 0.66-0.90, P=0.001) (Figure 5).
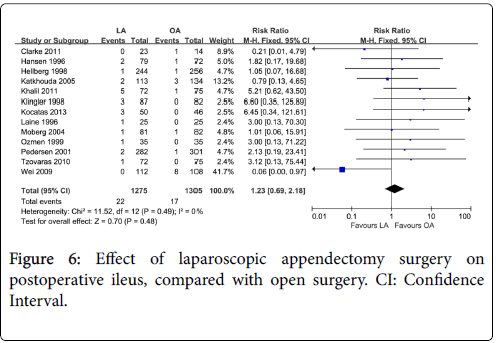
Postoperative ileus
The combined data from 13 studies showed that the incidence of postoperative ileus was 1.73% (22/1275) for laparoscopic appendectomy, and 1.30% (17/1305) for open appendectomy. The effect size of the difference in the ORs was 1.23 (95% CI: 0.69-2.18; P=0.48). A fixed-effects model was used because there was no heterogeneity between the two groups (I2=0%, P=0.49) (Figure 6).
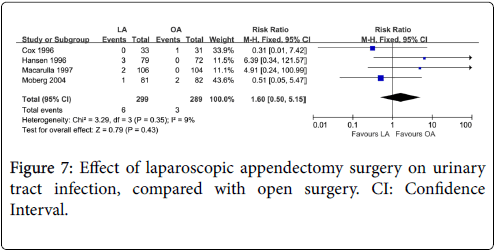
Urinary tract infection
The urinary tract infection in adults was reported in 4 studies, and the postoperative urinary tract infection rate was 6 in 299 (2.01%) patients in laparoscopic appendectomy and 3 in 289 (1.04%) patients in open appendectomy. There was no significant difference between the two groups (OR=1.60, 95% CI: 0.50-5.15, P=0.43). A fixed-effects model was used because there was no heterogeneity between the two groups (I2=9%, P=0.35) (Figure 7).
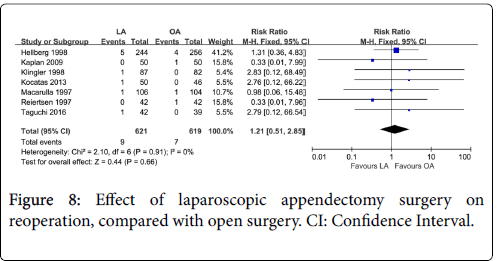
Reoperation
The combined data from only 7 studies revealed that the incidence of reoperation was 1.45% (9/621) for laparoscopic appendectomy and 1.13% (7/619) for open appendectomy. The effect size of difference in ORs was 1.21 (95% CI: 0.51-2.85, P=0.66). A fixed-effects model was used because there was no heterogeneity between the two groups (I2=0%, P=0.91) (Figure 8).
Sensitivity analysis and publication bias
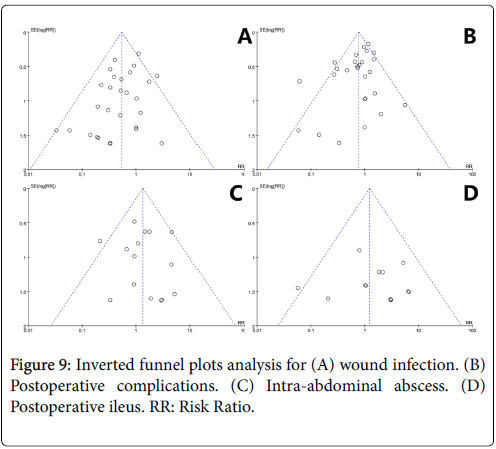
The sensitivity analysis was performed by sequentially excluding any individual researches individually, with an objective of examining the impact of every single research work on summarized findings. Consequently, as revealed by the findings of the sensitivity analysis, our findings exhibited statistical robustness and credibility (data not shown). The shapes of the funnel plot seemed symmetrical (Figure 9), suggesting that there was no obvious publication bias.
Discussion
Although laparoscopic appendectomy (LA) has unique advantages in several areas of daily surgical practice as a minimally invasive technique, superiority of laparoscopic appendectomy to open approach has been discussed for many years [10,21]. Similar results with regard to surgical and cosmetic outcomes and low cost are the important issues favoring open appendectomy (OA) [42]. Several retrospective and prospective studies have suggested that laparoscopic appendectomy can decrease postoperative complications and wound infections, intra-abdominal abscesses are slightly increase after laparoscopy [10,12,39].
Semm et al. first described laparoscopic appendectomy in 1983 [5], laparoscopic appendectomy increased in popularity throughout the 1990s; nevertheless, its superiority over open appendectomy is still being debated. Some investigators reported better results in LA when compared to OA [20], while others determined that the clinical benefit obtained was inadequate, and emphasized that the technique had higher cost [10]. Currently, there is no consensus on whether LA should be routinely used or not. To our knowledge, this is the first comprehensive and systematic meta-analysis to evaluate the shortterm results of open appendectomy versus laparoscopic appendectomy in adults.
Meta-analysis is a useful statistical tool that can be used to evaluate the existing literature in both quantitative and qualitative ways by comparing and integrating the results of different studies, taking into account variations in characteristics that can influence the overall estimate of the outcome of interest. It is especially valuable when previous studies have been unable to show significant differences between treatments because of small sample sizes, or when there is no consensus of opinions. The results of the present meta-analysis demonstrated that, when compared with open appendectomy, laparoscopic appendectomy in adults was associated with lower incidence of wound infection, fewer postoperative complications, and there was significantly statistical difference between the two groups. However, laparoscopic appendectomy in adults was associated with slightly higher incidence of intra-abdominal abscess, peritonitis,postoperative ileus, urinary tract infection, and reoperation, and there was not statistical difference between the two groups.
Infectious complications represented by wound infections and intraabdominal abscesses are two variables by which the techniques have been traditionally compared. Wound infections may not be serious complications per se but represent a major inconvenience to the patient, impacting his convalescence time and quality of life. Wound infections are the most common complication after appendectomy, although the answer to the question as to why wound infections might be reduced during laparoscopic appendectomy is unclear. A possible reason for this is that in open appendectomies the appendix is delivered directly through the wound, thereby risking contamination, whereas in laparoscopic surgery the inflamed appendix never comes in to contact with the wound as it is removed via a trocar or bag. In our study, the risk of wound infection is lower in laparoscopic appendectomy as compared to open appendectomy, and the difference between laparoscopic appendectomy and open appendectomy groups was significantly statistical association (Z=4.69, P<0.00001). Intraabdominal abscess formation is a serious complication and can potentially be life threatening. In our study, the postoperative intraabdominal abscess rate was slightly higher in the laparoscopic group, the present meta-analysis did not show a statistically significant increase in the rate of intra-abdominal abscess formation in the laparoscopic appendectomy (Z=1.43, P=0.15). This is consistent with the literature [43,44].
Postoperative complications are usually considered in an assessment of a procedure’s safety. The common complications of appendectomy are wound infections, intra-abdominal abscess, postoperative ileus, peritonitis, urinary tract infection. In the present meta-analysis, we used the overall incidence of postoperative complications to assess the safety of laparoscopic appendectomy. The present meta-analysis results demonstrated that the overall incidence of postoperative complications in laparoscopic appendectomy was lower than in the open appendectomy group (Z=3.29, P=0.001).
This study has several limitations. First, the different operation methods were performed by different surgeons in different countries; thus different learning curves may have contributed to the reported difference between the two procedures. Second, not all the studies measured data based on a double-blind. In the absence of a doubleblind, subjective variables could be considerably influenced by the enthusiasm for a novel technique. Third, there was variation in surgical techniques and treatment protocols amongst the studies, and therefore heterogeneity in the studies might exist.
Conclusion
In conclusion, the present meta-analysis demonstrated that laparoscopic appendectomy provides considerable benefits over open appendectomy, including lower incidence of wound infections, and fewer postoperative complications. Therefore, the laparoscopic is a useful tool in the treatment of acute appendicitis and worth recommending as effective and safe procedures for adults.
Conflict of Interest
The authors claim to have no conflict of interest.
References
- Addiss DG, Shaffer N, Fowler BS, Tauxe RV (1990) The epidemiology of appendicitis and appendectomy in the United States. Am J Epidemiol 132: 910-925.
- Jaschinski T, Mosch C, Eikermann M, Neugebauer EA (2015) Laparoscopic versus open appendectomy in patients with suspected appendicitis: a systematic review of meta-analyses of randomised controlled trials. BMC Gastroenterol 15: 48.
- Casarotto A, Zarantonello FR, Rebonato M (2014) Appendectomy in women. Is the laparoscopic approach always better than the "open" approach in uncomplicated appendicitis? Surg Laparosc Endosc Percutan Tech 24: 406-409.
- McBurney C (1984) The Incision Made in the Abdominal Wall in Cases of Appendicitis, with a Description of a New Method of Operating. Ann Surg 20: 38-43.
- Biondi A, Grosso G, Mistretta A, Marventano S, Toscano C, et al. (2013) Laparoscopic vs. open approach for colorectal cancer: evolution over time of minimal invasive surgery. BMC Surg 13: 12.
- Garbutt JM, Soper NJ, Shannon WD, Botero A, Littenberg B (1999) Meta-analysis of randomized controlled trials comparing laparoscopic and open appendectomy. Surg Laparosc Endosc 1: 17-26.
- Kurtz RJ, Heimann TM (2001) Comparison of open and laparoscopic treatment of acute appendicitis. Am J Surg. 182: 211-214.
- Milewczyk M, Michalik M, Ciesielski M (2003) A prospective, randomized, unicenter study comparing laparoscopic and open treatments of acute appendicitis. Surg Endosc 17: 1023-1028.
- Katkhouda N, Mason RJ, Towfigh S, Gevorgyan A, Essani R (2005) Laparoscopic versus open appendectomy: a prospective randomized double-blind study. Ann Surg 242: 439-448.
- Kaplan M, Salman B, Yilmaz TU, Oguz M (2009) A quality of life comparison of laparoscopic and open approaches in acute appendicitis: a randomised prospective study. Acta Chir Belg. 109: 356-363.
- Cipe G, Idiz O, Hasbahceci M, Bozkurt S, Kadioglu H, et al. (2014) Laparoscopic versus open appendectomy: where are we now? Chirurgia (Bucur) 109: 518-22.
- Kargar S, Mirshamsi MH, Zare M, Arefanian S, Shadman Yazdi E, et al. (2011) Laparoscopic versus open appendectomy; which method to choose? A prospective randomized comparison. Acta Med Iran 49: 352-356.
- Kocatas A, Gonenc M, Bozkurt MA, Karabulut M, Gemici E, et al. (2013) Comparison of open and laparoscopic appendectomy in uncomplicated appendicitis: a prospective randomized clinical trial. Ulus Travma Acil Cerrahi Derg 19: 200-204.
- Tzovaras G, Baloyiannis I, Kouritas V, Symeonidis D, Spyridakis M, et al. (2010) Laparoscopic versus open appendectomy in men: a prospective randomized trial. Surg Endosc 24: 2987-2992.
- Olmi S, Magnone S, Bertolini A, Croce E (2005) Laparoscopic versus open appendectomy in acute appendicitis: a randomized prospective study. Surg Endosc. 19: 1193-1195.
- Biondi A, Grosso G, Mistretta A, Marventano S, Tropea A, et al. (2014) Predictors of conversion in laparoscopic-assisted colectomy for colorectal cancer and clinical outcomes. Surg Laparosc Endosc Percutan Tech 24: e21-26.
- Jadad AR, Moore RA, Carroll D, Jenkinson C, Reynolds DJ, et al. (1996)Assessing the quality of reports of randomized clinical trials: is blinding necessary? Control Clin Trials. 17: 1-12.
- Kjaergard LL, Villumsen J, Gluud C (2001) Reported methodologic quality and discrepancies between large and small randomized trials in meta-analyses. Ann Intern Med 135: 982-989.
- Ignacio RC, Burke R, Spencer D, Bissell C, Dorsainvil C, et al. (2004) Laparoscopic versus open appendectomy: what is the real difference? Results of a prospective randomized double-blinded trial. Surg Endosc. 18: 334-337.
- Wei B, Qi CL, Chen TF, Zheng ZH, Huang JL, et al. (2011) Laparoscopic versus open appendectomy for acute appendicitis: a metaanalysis. Surg Endosc 25: 1199-1208.
- Pedersen AG, Petersen OB, Wara P, Ronning H, Qvist N, et al. (2001) Randomized clinical trial of laparoscopic versus open appendicectomy. Br J Surg 88: 200-205.
- Mantoglu B, Karip B, Mestan M, Iscan Y, Agca B, et al. (2015) Should appendectomy be performed laparoscopically? Clinical prospective randomized trial. Ulus Cerrahi Derg 31: 224-228.
- Laine S, Rantala A, Gullichsen R, Ovaska J (1997) Laparoscopic appendectomy-is it worthwhile? A prospective, randomized study in young women. Surg Endosc11: 95-97.
- Rashid A, Nazir S, Kakroo SM, Chalkoo MA, Razvi SA, et al. (2013) Laparoscopic interval appendectomy versus open interval appendectomy: a prospective randomized controlled trial. Surg Laparosc Endosc Percutan Tech. 23: 93-96
- Reiertsen O, Larsen S, Trondsen E, Edwin B, Faerden AE, et al. (1997) Randomized controlled trial with sequential design of laparoscopic versus conventional appendicectomy. Br J Surg 84: 842-847.
- Shirazi B, Ali N, Shamim MS. Laproscopic versus open appendectomy: a comparative study. J Pak Med Assoc (2010) 60: 901-904.
- Taguchi Y, Komatsu S, Sakamoto E, Norimizu S, Shingu Y, et al. (2016) Laparoscopic versus open surgery for complicated appendicitis in adults: a randomized controlled trial. Surg Endosc 30: 1705-1712.
- Moberg AC, Berndsen F, Palmquist I, Petersson U, Resch T, et al. (2016) Randomized clinical trial of laparoscopic versus open appendicectomy for confirmed appendicitis. Br J Surg 92: 298-304.
- Mutter D, Vix M, Bui A, Evrard S, Tassetti V, et al. (2010) Laparoscopy not recommended for routine appendectomy in men:results of a prospective randomized study. Surgery 120: 71-74.
- Ozmen MM, Zulfikaroglu B, Tanik A, Kale IT (1999) Laparoscopic versus open appendectomy: prospective randomized trial. Surg Laparosc Endosc Percutan Tech 9: 187-189.
- Long KH, Bannon MP, Zietlow SP, Helgeson ER, Harmsen WS, et al. (2001) A prospective randomized comparison of laparoscopic appendectomy with open appendectomy: Clinical and economic analyses. Surgery 129: 390-400
- Macarulla E, Vallet J, Abad JM, Hussein H, Fernandez E, et al. (1997) Laparoscopic versus open appendectomy: a prospective randomized trial. Surg Laparosc Endosc. 7: 335-339.
- Martin LC, Puente I, Sosa JL, Bassin A, Breslaw R, et al. (1995) Open versus laparoscopic appendectomy. A prospective randomized comparison. Ann Surg 222: 256-261.
- Hellberg A, Rudberg C, Kullman E, Enochsson L, Fenyo G et al. (1999) Prospective randomized multicentre study of laparoscopic versus open appendicectomy. Br J Surg 86: 48-53.
- Klingler A, Henle KP, Beller S, Rechner J, Zerz A, et al. (1998) Laparoscopic appendectomy does not change the incidence of postoperative infectious complications. Am J Surg 175: 232-235.
- Hansen JB, Smithers BM, Schache D, Wall DR, Miller BJ, et al. (1996) Laparoscopic versus open appendectomy: prospective randomized trial. World J Surg. 20: 17-20.
- Kald A, Kullman E, Anderberg B, Wiren M, Carlsson P, et al. (1999) Cost-minimisation analysis of laparoscopic and open appendicectomy. Eur J Surg 165: 579-582.
- Clarke T, Katkhouda N, Mason RJ, Cheng BC, Olasky J, et al. (2011) Laparoscopic versus open appendectomy for the obese patient: a subset analysis from a prospective, randomized, double-blind study. Surg Endosc 25: 1276-1280.
- Cox MR, McCall JL, Toouli J, Padbury RT, Wilson TG, et al. (1996) Prospective randomized comparison of open versus laparoscopic appendectomy in men. World J Surg 20: 263-266.
- Al-Mulhim AS, Al-Mulhim FM, Al-Suwaiygh AA, Al-Masaud NA (2002) Laparoscopic versus open appendectomy in females with a clinical diagnosis of appendicitis. Saudi Med J 23: 1339-1342.
- Li X, Zhang J, Sang L, Zhang W, Chu Z, et al. (2010) Laparoscopic versus conventional appendectomy--a meta-analysis of randomized controlled trials. BMC Gastroenterol 10: 129.
- Chung RS, Rowland DY, Li P, Diaz J (1999) A meta-analysis of randomized controlled trials of laparoscopic versus conventional appendectomy. Am J Surg 177: 250-256.
- Sauerland S, Lefering R, Holthausen U, Neugebauer EA(1998) Laparoscopic vs conventional appendectomy--a meta-analysis of randomised controlled trials. Langenbecks Arch Surg 383: 289-295.
Citation: Zhang H, Gao H, Ma X (2017) Comparison of Short-Term Outcome between Laparoscopic and Open Appendectomy in Adults: A Meta-Analysis of Randomized Controlled Trials. Diagn Pathol Open 2: 131. DOI: 10.4172/2476-2024.1000131
Copyright: ©2017 Zhang H, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Open Access Journals
Article Tools
Article Usage
- Total views: 4589
- [From(publication date): 0-2017 - Jan 31, 2025]
- Breakdown by view type
- HTML page views: 3861
- PDF downloads: 728