Research Article Open Access
Comparison of Mulligans Spinal Mobilization with Limb Movement (SMWLM) and Neural Tissue Mobilization for the Treatment of Lumbar Disc Herniation: A Randomized Clinical Trial
Nisar Ahmed1*, Zainy Khan2 and Chandan Chawla31Jamia Millia Islamia, Centre for Physiotherapy and Rehabilitation Sciences, New Delhi, India
2MPT Orthopedics, Jamia Millia Islamia, New Delhi, India
3Osteomyology, Jamia Millia Islamia, New Delhi, India
- Corresponding Author:
- Nisar Ahmed
Senior Physiotherapist, Jamia Millia Islamia
Centre for Physiotherapy and Rehabilitation Sciences (CPRS)
New Delhi-10025, India
Tel: +91 9873282252
E-mail: physio_nisar@yahoo.co.in
Received Date: August 08, 2016; Accepted Date: August 26, 2016; Published Date: August 31, 2016
Citation: Ahmed N, Khan Z, Chawla C (2016) Comparison of Mulligan’s Spinal Mobilization with Limb Movement (SMWLM) and Neural Tissue Mobilization for the Treatment of Lumbar Disc Herniation: A Randomized Clinical Trial. J Nov Physiother 6:304. doi: 10.4172/2165-7025.1000304
Copyright: © 2016 Ahmed N, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Novel Physiotherapies
Abstract
Lumbar disc herniation (LDH) with radiculopathy is one of the most common diagnoses encountered in orthopedic clinical practice and it is believed to be a major contributor to the estimated 60-80% lifetime incidence of low back pain. This study was designed to compare the effects of two dissimilar manual therapy techniques viz neural tissue mobilization and Mulligan’s spinal mobilization with limb movement (SMWLM) in patients with L4/L5-L5/S1 lumbar disc herniation associated with radiculopathy. A pre-test post-test experimental design using random sampling was used on 24 patients between 25-60 years of age. Group A patients received neural mobilization with conventional physiotherapy and group B patients received mulligan’s spinal mobilization with limb movement in addition to conventional physiotherapy. The efficacy of the both the treatment groups was assessed using self-report measures namely Numeric pain rating scale (NPRS), Modified Oswestry Disability Index (MODI) and H-Reflex latency which were measured both at baseline and after four weeks of intervention. The results of the study revealed that there was a statistically significant difference between both the groups in terms of pain (p=0.002*) and functional disability (p=0.002*); but no significant post-test difference could be found in H-reflex latency (p=0.632) between groups A and B. This concludes the fact that the neural tissue mobilization group was statistically better than the spinal mobilization with limb movement (SMWLM) group and hence the magnitude of response in relieving pain, improving functional disability and promoting centralization was better in patients who received neural tissue mobilization.
Keywords
Pain; Lumbar disc herniation; Neural tissue mobilization; Spinal mobilization with limb movement; Disability
Introduction
Lumbar disc herniation (LDH) is a common condition which frequently affects the spine in young and middle-aged patients [1-3]; it is one of the most common diagnoses encountered in orthopedic clinical practice [4] with peak incidence usually occurring between 30 and 55 years of age [5]. Lumbar disc herniation can be best defined as localized displacement of disc material beyond the normal margins of the intervertebral disc space leading to pain, weakness, or numbness in a myotomal or dermatomal distribution [6]. Cost of treatment of low back pain due to lumbar disc herniation in United States is estimated to be approximately 31 billion dollars per year [7]. The majority of herniated discs occur in a posterolateral direction, compressing the ipsilateral nerve root as it exits from the dural sac chiefly affecting the L4-L5, L5-S1 nerve roots; it usually presents with low back ache with or without radicular pain [8]. Many studies have demonstrated that lumbar disc herniation, protrusions, and annular tears are present even in asymptomatic individuals and only 50% of patients feel the radicular symptoms [9].
Herniation of the intervertebral disc usually causes impingement of neural structures and various spinal structures like the paravertebral muscles, ligaments, facet joints, annulus fibrosus and spinal nerve roots have been suggested as the cause of pain [10]. Some researchers believe that neural compression due to herniation of intervertebral disc is the main generator of pain and it has been suggested that if nociceptive input continues over time it may lead to functional, chemical and structural alterations in peripheral system and at various levels within the central nervous system [11]. So the pain associated with lumbar radiculopathy occurs due to a combination of nerve root ischemia and inflammation resulting from local pressure and also the neurochemical inflammatory factors present within the disc material [2,3,12,13]. It is also worthy to mention that the size of the disc herniation has not been found to be related to the severity of the patient‘s pain [11]. Electrodiagnostic studies also have the utility in diagnosing nerve root compression and of late Hoffmann reflex (H-reflex) is found to be more helpful in this context [14]. H-reflex is an essential diagnostic criterion for radiculopathy, especially when clinical and electrophysiological signs of motor root involvement are lacking [15]. For example, Hreflex recordings from the soleus muscle are helpful in identifying dysfunctional pathologies and radiculopathy arising from the S1 nerve root; the inferences are used to diagnose nerve root impingement which could be corroborated with a standard physical examination and radiographic imaging studies [16].
Lumbar disc herniation greatly impacts both individuals and society as a whole so it is essential that clinicians must have an in depth understanding of underlying mechanisms and efficacy of treatments being given [17]. Various operative and non-operative treatment strategies are being tried for lumbar disc herniation with varying degrees of success [18]. The most frequently used advocated nonsurgical treatments are short-term rest, exercises, steroidal antiinflammatory medications, muscle relaxants, and opioid analgesics.
Physical therapy is commonly given in the form of physical modalities (Traction, TENS, Ultrasound, Heat), strengthening and core stabilization exercises, manual therapy techniques involving the Mc kenzie approach, Maitland mobilization, neural tissue mobilization, Mulligan’s mobilization and soft tissue interventions [19,20]. Studies evaluating the effectiveness of physiotherapy interventions for disc herniation have been the subject of debate among clinicians and none of the treatment techniques has been found to be superior to others. Hence the interventions should always be decided and given after an accurate diagnosis and consideration of prognostic findings.
Manual therapy interventions have always demonstrated greater improvements in pain and functional outcomes in the treatment of patients of both neural and non-neural types of low back pain [21] involving disc herniation. Despite the widespread use of manual therapy in clinical settings, very little is known about the effectiveness of these procedures and there is a paucity of research due to the absence of controlled clinical trials. Mulligan‘s mobilization with movement (MWM) technique is being widely used as an intervention for low back dysfunction. The theoretical basis for the effectiveness of mobilization with movement is based on the concept related to a “positional fault” which usually occurs secondary to injury leading to maltracking of the joint that in turn causes symptoms like pain, stiffness or weakness [22]. One of the commonly used Mulligan’s spinal mobilization technique is the Mulligan‘s Spinal mobilization with limb movement (SMWLM); it has been shown to be effective and produces immediate results in spinal joint dysfunction as well as abnormal neural dynamics [23]. Vincenzino proposed that Mulligan techniques helps in improving patient‘s symptoms by correcting the minor positional fault and also by the neurophysiologic mechanisms [24]. However valid research is needed to acclaim these results and generalize the same in patients with Lumbar disc herniation.
Neural mobilization is another form of manual therapy devised by Davidson [25] similar to joint mobilization; they are set of techniques designed to restore elasticity and plasticity of the nervous system which is defined as the ability of nerve surrounding structures to shift in relation to other structures [26]. The effect of Neurodynamic techniques in exploration of sciatic nerve root from compression of disc herniation was explained by McGill [27], who stated that if the nerve root is impinged and cannot slide, instead of moving, the pain would be elicited along the nerve trunk. The reported benefits from such techniques involves the increase in vascular and axoplasmic flow of nerve, reduce the intraneural and extraneural fibrosis necessary for the functional and structural integrity of a neuron and thus restoring the mobility of tissues [28]. So it is clear from previous studies that neurodynamic techniques will have a great role in reducing pain and improving disability in patients with LDH. However valid robust in vitro and in vivo clinical trials are required to support the purported benefits of nerve mobilization techniques.
There is no published evidence or clinical data for the use of both of these manual therapy techniques in patients with lumbar disc herniation. In order to maximize the success of conventional physiotherapy the above mentioned treatment techniques, one involving solely the nerve and other involving the spinal joint segments would be utilized and further treatment strategies in lumbar disc herniation could be planned.
Objective
To compare the efficacy of two different manual therapy approaches on pain, nerve excitability and functional disability in patients with lumbar disc herniation and to device a rehabilitation protocol which will be more beneficial, safer and cost-effective in patients with disc herniation.
Methodology
Subject and study design
Sample: The study sample consisted of twenty four patients both male (n=8) and female (n=16) referred to the outpatient physiotherapy department (CPRS clinic), Jamia Millia Islamia University and ESI hospital, New Delhi respectively. Patients with confirmed MRI and clinical diagnosis of L4-L5/L5-S1 disc herniation with radiculopathy were recruited for the study. Ethical clearance was obtained from the Institutional Review Board, Jamia Millia Islamia. Sample size was estimated using G Power 3.1.7 software at 90 percent power and effect size of 1.01 at significance level of 0.05 (α) came out to be 24 i.e. minimum 12 in each group [29].
Inclusion criteria: Patients aged 25-65 years who had confirmed MRI findings of L4-L5/L5-S1 of disc herniation (grade 2 and above). The system used in grading compromise of the intraspinal extradural lumbar nerve root consists of four grade categories, summarized as follows. Grade 0 (normal), Grade 1 (contact), Grade 2 (deviation), Grade 3 (compression) [30] with radicular symptoms distal to the knee were recruited for this study. Patients exhibiting symptoms for more than 10 days and less than 4 months with a Numeric pain rating score (NPRS) greater than 4/10 were included in this study; all patients had a baseline Modified Oswestry score of greater than 10%.
Exclusion criteria: Patients with infectious, metabolic diseases of spine, malignancy, history of vertebral fractures, spinal surgery, lumbar canal Stenosis, neurologic disorders, Pregnancy, Rheumatoid arthritis, spinal compression fractures, prolonged history of steroid use were excluded from the study.
Study design: Pretest posttest experimental group design with random allocation into two study groups using lottery system.
There were 44 patients were screened out of which 12 patients were excluded from the study due to not fulfilling the inclusion criteria and 8 drop outs at different time frame. Those subjects who do not fulfilled the criteria had given conventional physiotherapy.
Procedure
After the study had been approved by ethical committee, male and female patients with MRI confirmed and clinically diagnosed cases of L4-L5 and L5-S1 disc herniation with radiculopathy were recruited from CPRS clinic, Jamia Millia Islamia and ESI hospital, New Delhi respectively. Patients were explained about the purpose, methodology and the possible risks involved in the study. All patients gave written informed consent prior to participation in the study. The identifying information on the consent form and demographic/injury history questionnaire was kept confidential by assigning a number to each patient.
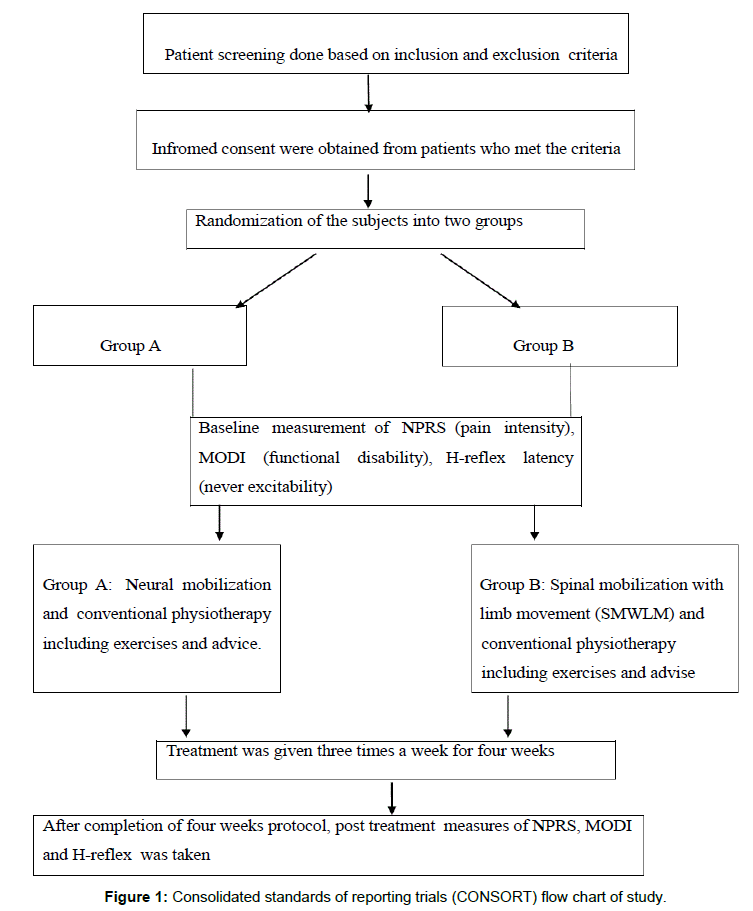
Patients were selected on the basis of inclusion and exclusion criteria and divided into two groups, group A and group B. Patients in Group A were treated with neural tissue mobilization in addition to conventional physiotherapy and Group B patients were treated with mulligan spinal mobilization with limb movement (SMWLM) in addition to conventional physiotherapy. Patients in both the two different groups were treated three days a week for four weeks (Figure 1).
Protocol
Group A: Neural Mobilization with conventional physiotherapy: The patient was made to lie supine and relaxed in the center of the bed with one pillow under the head; trunk and pelvis were in the neutral position. The therapist stood on the opposite side to the patient and placed one hand under the ankle joint and the other hand was placed above the knee joint. The affected leg was raised perpendicular to the bed while maintaining the knee in extension as in SLR testing position. The technique was progressed to a point where symptoms were reproduced, or it was taken to a point where resistance of the movement was encountered. The limb was taken down few degrees from this symptomatic point and graded sciatic nerve mobilization was then given to mobilize the sciatic nerve by a sequence of gentle oscillations. Neural tissue mobilizations were given in the form of either tibial nerve bias (L4-L5 ankle dorsiflexion and eversion SLR/DF/EV/ HAd) or peroneal nerve bias (L5-S1 ankle plantar flexion and inversion SLR/PF/IV/HAd) depending upon the level of disc herniation and the effect was then reassessed. The number of these sequences was repeated many times, through which the amplitude of the technique was increased according to the patient response. Further sensitization and tension in the sciatic nerve was increased with the following additions/ maneuvers: Hip adduction, medial rotation and trunk side flexion. As the symptoms were relieved, the therapist increased the range of motion until reaching the maximum range of pain free SLR. Neural tissue mobilization procedures were given in the form of 3 sets of 10 oscillatory movements thrice a week for four weeks
Group B: Mulligan’s spinal mobilization with limb movement (SMWLM) with conventional physiotherapy: According to Mulligan, this technique is performed by two practitioners working as a team with one performing the sustained medial glide on the patient’s lumbar spinous process whilst the other moves, passively, the patient’s uppermost leg into hip flexion. Spinal Mobilization with Leg Movement technique was performed in side lying, with the affected leg uppermost; patient lies facing the therapist, and an assistant therapist supporting his affected leg (Figure 2). Therapist flexes over patient and places one thumb reinforced over other on the spinous process of the chosen vertebra (L4/L5 or L5/S1 vertebra) as palpated with reference to posterior superior iliac crest. The therapist then pushes down on the chosen spinous process. This pressure is sustained and the patient actively performs SLR for the leg supported by the assistant provided there is no pain. If this approach is successful, on subsequent visits, as the patient improves, assistant applies overpressure, provided there is no discomfort. Furthermore, [22] advocates that on the patient’s first visit, this technique should be performed only three times (rule of three) as a precaution against any latent exacerbation. On subsequent days three sets of six repetitions was applied. Six sessions with 48 hr interval between each were given.
Conventional physiotherapy
Conventional physiotherapy was given in both the groups based on the recommendations of North American spine society clinical guidelines. It included moist hot pack (28×46 cm) which were kept under the temperature of 71-74°C was given for 15 minutes in prone lying position , TENS (Sonopulse 692V - Enraf Nonius, 4-Pole) two channel TENS with conventional mode is used. The unit produces an asymmetrical biphasic waveform, 100 Hz and pulse duration 125 μs. While the patient in the prone position four carbons rubber electrodes (3.5×5 cm) or vacuum electrodes are used positioned over the lumbar paraspinal muscles and other two over the course of tibial nerve (mid of posterior thigh and over the bulk of calf muscles). TENS was applied for continuous 20 minutes period [31] and supervised back strengthening exercise program consisting of pelvic tilts, Bridging, quadruped alternate arms/legs activities, abdominal bracing as described by Stuart Mc Gill. Patients ask to perform 2 sets of 10 repetitions of each exercise 3 times a week for four weeks and progress the exercise routine according to the symptoms. Precautions and ergonomic advice was also explained to all patients of both the groups.
Criterion measures
Magnetic resonance imaging (MRI) was used to measure the degree of nerve root compression due to disc herniation using grading system (0-3). The accuracy of MRI for predicting the presence of disc herniation at surgery is relatively high (varying from 76% to 96%) and thus it has become the investigation of choice for patients suspected of lumbar disk herniation [32]. In this study the patients with grade 2 disc herniation and above were selected.
Pain assessment
The Numeric pain rating score (NPRS) is a reliable and valid outcome measure and has been used extensively in LBP research. The 11-point NPRS ranges from 0 (no pain‘‘) to 10 (worst pain imaginable‘‘) and is used to indicate the intensity of current pain, at its best and worst level [33]. These 3 ratings were then averaged to arrive at an overall pain score. The scale has been shown to have adequate reliability, validity, and responsiveness in patients with LBP when the 3 scores are averaged [34,35] found the intraclass correlation coefficient (ICC) for internal consistency ranged between 0.64 and 0.86 for many diagnoses including LBP.
Measurement of H-reflex
Stretanski [36] explained the concept on which H reflexes are based; he stated that when the tibial nerve (at the popliteal fossa) is stimulated electrically, excitation of the afferent portion of a reflex arc will travel to the dorsal root ganglion of S1. If there is a problem with S1 nerve conduction, then the motor response will be slow or non-existent.
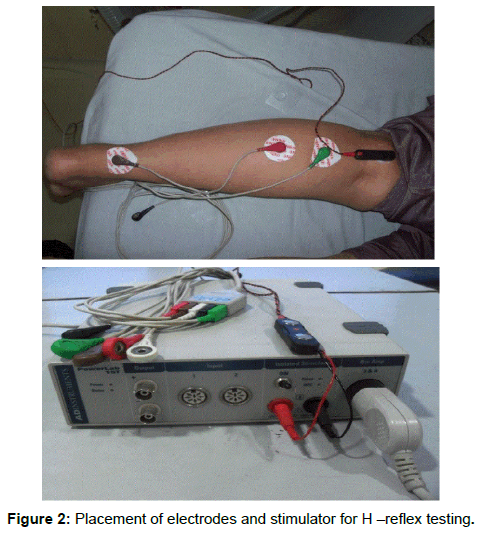
Position of the electrodes and their application
The recording electrode consisted of R1 placed over the soleus and R2, the reference electrode, placed over the Achilles tendon. Although the H-reflex can be recorded over any portion of gastronomies and soleus muscles, the optimal location that yields the largest H-reflex was two or three finger breadth distal to where the soleus meets the two bellies of the gastrocnemius. The tibial nerve was stimulated in the popliteal fossa, with cathode placed proximal to anode and beginning at very low stimulus intensities (Figure 2).
The stimulation parameters were 1.0 ms pulse duration at a frequency of 0.2 Hz and intensity was increased until H-reflex maximum with minimum and stable M-response. Ground electrode (G) placed at half distance between stimulating and recording electrodes. Three readings of the maximum H-reflex with minimum and stable M-response were recorded and averaged in each condition.
Modified Oswestry disability index
Modified Oswestry disability index is the most commonly used functional back scale consisting of 10 items, each item scored from 0-5, higher values representing greater disability. The final score is calculated as follows: Total score=(Sum of items scored/Sum of sections answered)×100%. The test–retest reliability of the modified ODI has been shown to be high. Score range is 0-100, reliability of ICC=0.90, sensitivity=91% and specificity=83% [37].
For both the groups A and B take the criterion measurements immediately before, and after four weeks of intervention.
Statistical design and data analysis
Sample size was estimated using G Power 3.1.7 software at 90 percent power and effect size of 1.01 at significance level of 0.05 (α) came out to be 24 i.e. minimum 12 in each group [29]. Statistical Analysis was done by using SPSS 21.0 and data was assessed by a Shapiro Wilk test for normality of the distribution scores. Numeric pain rating scale scores that demonstrated non normal distribution were log-transformed for further analysis. Twelve participants (n=12) in each group were assessed at baseline and after 4 weeks of intervention protocol. Then a paired t–test was applied to analyze the effect of intervention in two groups for the measures of pain (NPRS), functional disability (MODI) and nerve excitability (H-reflex). To test the difference between groups an independent t-test was employed, significance level was set at p-value<0.05.
Results
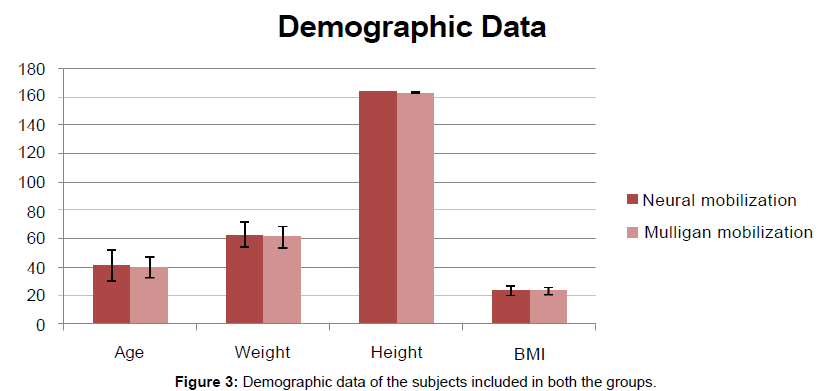
For this study twenty four (n=24) subjects were selected to compare the effects of neural mobilization and mulligan spinal mobilization with limb movement. These subjects were then randomly divided into two groups, group A (n=12) and group B (n=12). The demographic data is shown in Table 1.
| Variables | Neural mobilization group | Mulligan mobilization group | t-value | p-value |
|---|---|---|---|---|
| Mean (SD) | Mean (SD) | |||
| Age | 41.17 (11.16) | 39.75 (7.48) | 0.365 | 0.718 |
| Weight (kg) | 62.97 (8.97) | 61.25 (7.59) | 0.509 | 0.616 |
| Height (m) | 1.64 (0.08) | 1.63 (0.06) | 0.453 | 0.655 |
| BMI | 23.47 (3.49) | 23.15 (2.59) | 0.261 | 0.796 |
Table 1: Comparison of demographic data between groups.
There was no significant difference for the demographic characteristics between the groups. Both the groups were comparable in terms of age, height, weight and BMI which represents the homogeneity of participants (Table 1).
In the present study, data were assessed by a Shapiro-Wilk test for the normality of the distribution scores, as the sample size used in the study was less than fifty. Numeric pain rating scale (NPRS) scores that demonstrated non normal distribution were log- transformed for further analysis.
Comparison of baseline criterion measurement between the two experimental groups was done using independent t-test to prove the homogeneity between the groups. No significant difference Numeric pain rating scale (NPRS), Modified Oswestry disability questionnaire (MODI) and Hoffman reflex (H-reflex) latency was found between the groups (Table 2). Paired t test was used in order to compare the outcome variables at the baseline and Post-test measures in the neural mobilization group. There was a significant difference in all the variables except the H reflex latency of the unaffected leg as shown in Table 3. Paired t test was used in order to compare the outcome variables at the baseline and Post-test measures in the Mulligan spinal mobilization group. There was a significant difference in all the variables except the H reflex latency of the unaffected leg as shown in Table 4.
| Variables | Neural mobilization group | Mulligan mobilization group | t-value | p-value |
|---|---|---|---|---|
| Mean (SD) | Mean (SD) | |||
| NPRS | 0.90 (0.04) | 0.89 (0.05) | 0.28 | 0.782 |
| MODI | 53.75 (8.93) | 52.59 (8.33) | 0.331 | 0.744 |
| H-reflex 1 | 28.01 (1.68) | 27.60 (1.73) | 0.589 | 0.562 |
| H-reflex 2 | 29.98 (1.97) | 29.21 (1.64) | 1.032 | 0.313 |
Table 2: Comparison of baseline criterion measures between groups.
| Variables | Pre Mean (SD) | Post Mean (SD) | p- value | Df | t-value |
|---|---|---|---|---|---|
| NPRS | Â 0.90 (0.04) | 0.30 (0.21) | <0.001* | 11 | 10.432 |
| MODI | 53.75 (8.93) | 9.90 (5.87) | <0.001* | 11 | 27.389 |
| H-reflex 1 | 28.01 (1.68) | 27.90 (1.74) | 0.27 | 11 | 1.161 |
| H-reflex 2 | 29.98 (1.97) | 28.35 (1.72) | <0.001* | 11 | 6.957 |
Table 3: Comparison of pre and post intervention measures in neural mobilization group.
| Variables | Pre Mean (SD) | Post Mean (SD) | p- value | Df | t-value |
|---|---|---|---|---|---|
| NPRS | 0.89 (0.05) | 0.57 ( 0.14) | <0.001* | 11 | 10.965 |
| MODI | 52.59 (8.33) | 19.39 (7.27) | <0.001* | 11 | 16.914 |
| H-reflex 1 | 27.60 (1.73) | 27.55 (1.76) | 0.663 | 11 | 0.447 |
| H-reflex 2 | 29.21 (1.64) | 28.91 (1.61) | <0.001* | 11 | 6.306 |
Table 4: Comparison of pre and post intervention measures in mulligan mobilization group.
Comparison of post-test criterion measurement between the neural mobilization and Mulligan mobilization group were done by using independent t-test. There was no significant difference between the two groups on H-reflex latency of affected leg where (p=412), but the mean difference (0.63) shows better results in neural mobilization (M=28.35, SD=1.70) as compared to Mulligan mobilization group (M=28.91, SD=1.61). However there was a significant difference between the groups in NPRS and MODI as shown in Figure 3 and Table 5.
| Variables | Neural mobilization group Mean (SD) | Mulligan mobilization group  Mean (SD) | p-value | t- value |
|---|---|---|---|---|
| NPRS | 0.30 (0.21) | 0.57 (0.14) | 0.002* | 3.587 |
| MODI | 9.90 (5.87) | 19.39 (7.27) | 0.002* | 3.514 |
| H-reflex 1 | 27.90 (1.74) | 27.55 (1.76) | 0.631 | 0.488 |
| H-reflex 2 | 28.35 (1.72) | 28.91 (1.61) | 0.412 | 0.491 |
Table 5: Comparison of post-test Criterion measures between groups.
Numeric pain rating scale
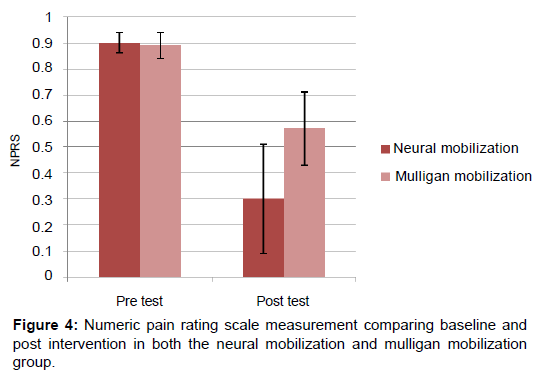
Baseline comparison of Neural mobilization (M=0.90, SD=0.04) and Mulligan Mobilization group (M=0.89, SD=0.05) showed no difference in Numeric pain rating scale, t (24)=0.280, p=0.782. NPRS measured at the baseline (M=0.90, SD=0.04) and after four weeks of intervention in neural mobilization group (M=0.30, SD=0.21) showed significant difference, t (12)=10.432, SEM=0.056, pË?0.001*. Similarly NPRS in Mulligan mobilization group also showed significant difference between the baseline measurements (M=0.89, SD=0.05) and post-test measures (M=0.57, SD=0.14), t (12)=10.965, SEM=0.028, pË?0.001*. However there was significant difference between neural mobilization (M=0.30, SD=0.21) and mulligan mobilization (M=0.57, SD=0.14) in their post-test measurements t (24)=3.587, p=0.002* (Figure 4).
Modified Oswestry disability questionnaire
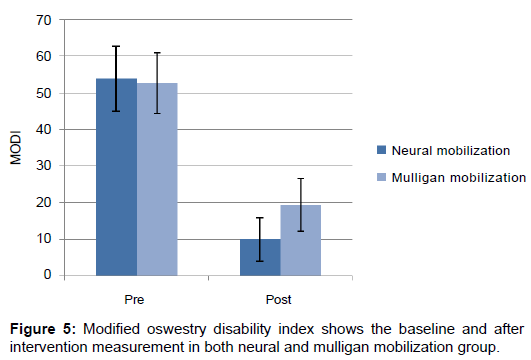
When comparing baseline data of Neural mobilization (M=53.75, SD=8.93) and Mulligan mobilization group (M=52.59, SD=8.33) showed no difference in modified Oswestry disability questionnaire (MODI), t (24)=0.331, p=0.744. In neural mobilization group when measured at the baseline (M=53.75, SD =8.93) and after four weeks intervention (M=9.90, SD=5.87) data showed significant difference, t (12)=27.389, SEM=1.60, pË?0.001*. Similarly MODI in Mulligan mobilization group also showed significant difference between the baseline measurements (M=52.59, SD=8.33) and post-test measures (M=19.39, SD=7.27), t (12)=16.914, SEM=1.96, p<0.001*. However there was significant difference between neural mobilization (M=9.90, SD=5.87) and Mulligan mobilization group (M=19.39, SD=7.27) in their post-test measurements t (24)=3.514, p=0.002* (Figure 5).
Hoffman reflex latency
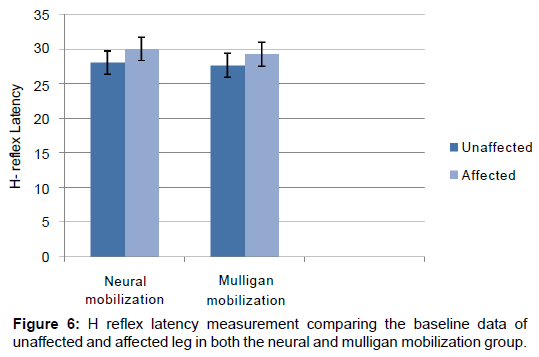
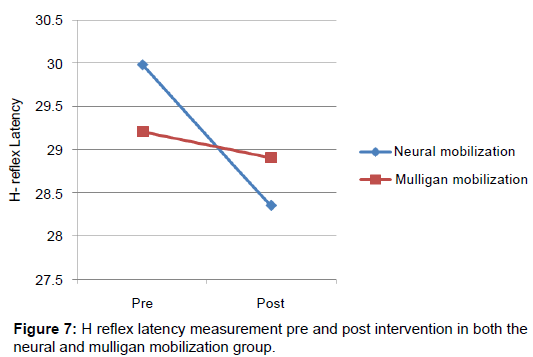
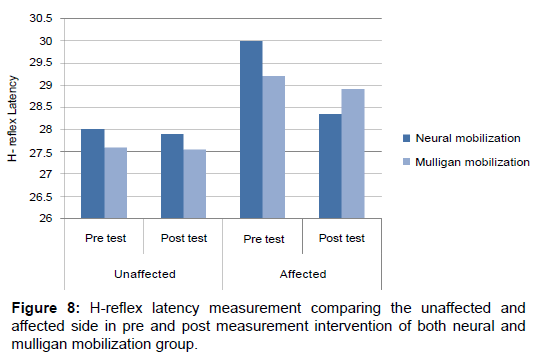
When comparing the baseline data of neural mobilization group for unaffected (M=28.01, SD=1.68) and affected leg (M=29.9, SD=1.97) with the Mulligan mobilization group for unaffected (M=27.60, SD=1.73) and affected leg (M=29.21, SD=1.64) respectively showed no difference in H reflex latency, t (24)=0.589, p=0.562 (unaffected leg) and t (24)=1.032, p=0.313 (affected leg). While comparing the baseline measures of H reflex latency to see the difference between unaffected and affected leg for Neural mobilization t (12)=8.16, p<0.001 and for Mulligan mobilization group t (12)=8.425, p=<0.001 showed significant difference between the legs in both the groups, which means there was a significant variation in unaffected and affected legs . In neural mobilization group when measured at the baseline for affected leg (M=29.9, SD=1.97) and after four weeks of intervention (M=28.35, SD=1.72) data showed significant difference, t (12)=6.957, SEM=0.233, pË?0.001*,But there was no difference for the unaffected leg t(12)=1.16, SEM=0.09, p=0.270. Similarly H-reflex latency in Mulligan mobilization group also showed significant difference between the baseline measurements for affected leg (M=29.21, SD=1.64) and posttest measures after four weeks of intervention (M=28.91 SD=1.61), t (12)=6.306, SEM=0.133, p<0.001*, and there was no difference for the unaffected leg. However when comparing the post H-reflex latency difference between neural mobilization (M=28.35, SD=1.72) and Mulligan mobilization group (M=28.91 SD=1.61) for the affected side in their post-test measurements t (24)=3.514, p=0.002* showed no statistically significant difference but the mean difference=0.63, shows better results in neural mobilization compared to mulligan mobilization group (Figures 6-8).
Discussion
The findings of this study clearly demonstrate that both the techniques along with conventional physiotherapy have a great impact on pain, functional disability and nerve function as measured by H-reflex latency. The between group analyses was done using unpaired t-test and the result of the study confirm the hypothesis that there was a significant difference between the two groups.
The results prove that the group which received neural tissue mobilization along with conventional physiotherapy was more effective than spinal mobilization with limb movement (SMWLM); the patients in both groups showed pronounced effects in improving pain and functional disability but the magnitude of response was significantly and clinically higher in the group B patients. The result of this study supports the fact that neural tissue mobilization does have a greater role in the management of lumbar radiculopathy compared to the traditional segmental joint mobilization techniques. The hypothesized benefits of neural mobilization include facilitation of nerve gliding, reduction of nerve adherence, and dispersion of noxious fluids, increased neural vascularity, and improvement of axoplasmic flow. These results are in agreement with [38,39], who mentioned that if the nerve root gets impinged and microcirculation compromised it will lead to inflammation along the course of the nerve; moreover the presence of disc material in the epidural space causes direct toxic injury to the nerve by chemical mediation and then exacerbation of intra neuronal and extra neuronal swelling causing venous congestion and conduction block. These findings also support the study done by Mc Cracking [40], who concluded that without restoring the mechanics and the mobility of the nerve roots the radicular symptoms will not resolve. Hence it becomes clear from the results that altering nerve mechanics via a neurodynamic treatment would have a more direct effect in patients with radiculopathy due to disc herniation. Because of the aforesaid reasons, the neurodynamic techniques involving the gliding and sliding of the nerve produced a greater magnitude of improvements in relieving pain and functional ability in patients with disc herniation as compared to spinal joint mobilization (SMWLM) technique as is evident from the between group analysis(P-value =<0.001.). These findings vividly delineate that the mobility of the nerve roots and nerve among the spinal segments are more important than segmental joint mobilization as advocated by. He explained that the mechanisms responsible for SMWLM treatment effects (such as decrease pain and functional disability) may feasibly involve changes in the joint, muscle, pain and motor control systems, possibly indicating that the underlying mechanisms of this technique may be related to local joint or muscle structures rather than the pain system and neurophysiology [41].
The patients in Group B treated with Mulligan‘s spinal mobilization (SMWLM) also showed improvements but the magnitude of effects were less pronounced compared to Group A patients treated with neural mobilization. These results could be attributed to the fact that the unilateral joint mobilization in the spinal mobilization group could have produced only the sympathoexcitatory effects localized to the spinal segment rather than direct mobilization of the involved nerve roots and the nerve. Vincenzino et al. suggested that the immediate effects of Mulligan’s techniques on pain reduction may be due to the activation of (as measured by recordings of sympathetic nervous system SNS- activity) non-opioid endogenous pain inhibition pathways especially the descending pain inhibitory systems via the periaquaductal gray (PAG) regions in the mid-brain [42,43]. Also it is worthy to mention that Mulligan’s joint mobilization restores the “positional fault” which produces the immediate hypoalgesic but without affecting the neural component. Further research in this area is warranted to better understand the underlying mechanism(s) of SMWLM techniques in patients with or without nerve compression due to disc herniation.
There were improvements in H-reflex latency in both the groups at a statistically significant level before and after the treatment. Both the groups showed positive outcomes in terms of H-reflex in pre to post intervention with a mean difference (0.63) but there was no significant difference between them. It is unclear how the spinal mobilization group had an obvious effect on H-reflex latency. These findings are in agreement with Bulbulian et al., who investigated the effects of H-reflex measures on spinal mobilization and revealed that H-reflex amplitude and H/M ratio decreased.
Within group analysis of both the groups showed statistically significant improvement in pain, functional disability and H-reflex latency in patients with lumbar disc herniation. As mentioned above the improvements in the SMWLM group could be attributed to the fact that correction of a small positional fault which frees the pressure off the structures that produce the pain and limitation [22]; this might have relieved the radicular pain caused by the compression of the nerve and may have also reduced the extent of pain by the mechanism of “centralization”.
According to the results, Modified Oswestry disability index (MODI) and NPRS pain score indicated the greater effectiveness of neural mobilization technique compared to spinal mobilization in patients with radiculopathy due to disc herniation. The improvements in functional ability which was measured using Modified Oswestry disability index (MODI) is found to have more superior measurement properties and more reliable than other disability scales [25]. The MODI score was found to be more in neural mobilization group and it has been reported that reductions in the MODI of 6 points or greater are considered clinically meaningful [37].
The technical difference between neural mobilization and spinal mobilization with limb movement leads us to speculate that the neural mobilization technique have greater ability to improve the symptoms related to the radiculopathy than spinal mobilization with limb movement. However when deciding to implement neural tissue mobilization as an intervention, meticulous evaluation should be performed for signs of abnormal CNS sensitivity (e.g hyperalgesia, allodynia) as the response to mechanical treatments such as nerve mobilization is expected to be limited. With regards to compression related radiculopathy, an important factor while choosing the technique is to consider the duration of the compression. Sustained mechanical compression for a longer duration may cause injury to neurons of the dorsal root ganglion [44], and damage to nerve axons leading to irreversible structural changes which may respond well to neural tissue mobilization.
The results of the present study indicate that the effects could have also been attributed to the use of conventional physiotherapy which was given in the form TENS and strengthening exercises. It has been proved in previous studies that the patients with lumbar disc herniation show both asymmetry and atrophy of the multifidus muscle on the side of pain, and a decreased ability to recruit multifidus in chronic LBP and deficits in the ability to recruit the transverses abdominis across all subcategories of LBP. But the stabilization and strengthening exercises cannot be generalizable to all the subgroups of LBP due to disc herniation. The application of TENS in this study seems to have no decompression effect on the involved nerve roots and it produces only the analgesic effect by altering the pain gate mechanism; moreover TENS has been found to have no effects on H-reflex as investigated by Goulet [45].
The findings of the present study do support the notion that segmental joint mobilization and exercise alone are not effective in treating radiculopathy due to lumbar disc herniation. The combination of manual therapy with interventions directed at the neural component and specific adjuvant exercise had the greatest efficacy for treatment, so more attention needs to be given to add nerve mobilization as a viable and cost effective treatment approach. However well controlled robust clinical trials are required before it could be generalized to all the patients with lumbar disc herniation.
Clinical implications
Both the manual therapy techniques seem to provide short term improvement in pain, functional disability and nerve excitability in patients with lumbar disc herniation. The monetary and temporal cost of performing these techniques is minimal and hence can be used as a viable treatment option as a part of conventional physiotherapy.
Limitations
This study was limited by certain factors. The absence of a true control group makes it difficult to differentiate between the treatment effect and the natural course of the disorder, thus threatening the internal validity of the study. This study employed a relatively small sample size of only 24 patients which is known to affect the validity and generalizability of the results; Second, long-term outcomes were not assessed, and it is not known whether the differences observed at post-treatment could be maintained over longer periods of time. In electrophysiological testing with H-reflex the effect of noise and any external waves could have interfered with the accuracy of Hoffmann reflex (Latency) in EMG lab.
Future recommendation
Future studies should be conducted to know the effect of these techniques on various other causes of low back pain with or without radiculopathy. Since both the techniques produced clinically meaningful results future studies should be done to see the combined effects of joint and neural tissue mobilization in patients with lumbar disc herniation. The relationship between spinal manipulation and H-reflex changes is not clear and hence warrants further investigation.
References
- Anderson PA, McCormick PC, Angevine PD (2008) Randomized controlled trials of the treatment of lumbar disk herniation: 1983-2007. J Am AcadOrthopSurg 16: 566-573.
- McCulloch JA, Edwards CC II, Riew KD (2002) Lumbar microdiscectomy. In: Bradford DS, Zdeblick TA, editors. Master Techniques in Orthopaedic Surgery: The Spine. Lippincott Williams & Wilkins, Philadelphia, USA.
- Bono CM, Wisneski R, Garfin SR (2006) Lumbar disc herniations. In: Herkowitz HN, Garfin SR, Eismont FJ, Bell GR, Balderston RA. The Spine. 5th ed. Saunders, Philadelphia, USA.
- Tarulli AW, Raynor EM (2007) Lumbosacral radiculopathy.Neurology Clinic 25:387-405.
- Atlas SJ, Chang Y, Kammann E, Keller RB, Deyo RA, et al. (2000) Longterm disability and return to work among patients who have a herniated lumbar disc: the effect of disability compensation. J Bone Joint Surg Am 82:4-15.
- Kreiner DS, Hwang SW, Easa JE, Resnick DK, Baisden JL (2014) An evidence-based clinical guideline for the diagnosis and treatment of lumbar disc herniation with radiculopathy. Spine J 14: 180âÂ?Â?191.
- Schenk RJ, Jozefczyk C, Copf A (2003) A randomized trial comparing intervention in patient with lumbar posterior derangement. Journal of Manual and Manipulative Therapy 11: 95-102.
- Koes BW, vanTulder MW, Peul WC (2007) Diagnosis and treatment of sciatica. BMJ 334: 1313-1317.
- Schoenfeld AJ, Weiner BK (2010) Treatment of lumbar disc herniation: Evidence-based practice. International Journal of General Medicine 3: 209-214.
- Airaksinen O, Brox JI, Cedraschi C, Hildebrandt J, Klaber-Moffett J, et al. (2006) Chapter 4 European guidelines for the management of chronic nonspecific low back pain. Eur Spine J 15: S192-S300.
- Sertpoyraz F,Eyigor S, Karapolat H (2009) Comparison of Isokinetic exercise versus standard exercise training in patients with chronic low back pain: A randomized controlled study. Clinical rehabilitation 23: 238-247.
- Car ragee E (2006) Surgical treatment of disk disorders.Jama296:2485-2487.
- Majlesi J, Togay H, Unalan H, Toprak S (2008) The sensitivity and specificity of the slump and the straight leg raising tests in patients with lumbar disc herniation.J ClinRheumatol14:87-91.
- Beyaz EA, Akyuz G (2009) The role of somatosensory evoked potentials in the diagnosis of lumbosacral radiculopathies. Electromyogr Clinical Neurophysiology 49:131-142.
- Mazzocchio R, Scarfò GB, Mariottini A, Muzii VF, Palma L (2001) Recruitment curve of the soleus H-reflex in chronic back pain and lumbosacral radiculopathy. BMC MusculoskeletDisord 2: 4.
- Alrowayeh HN, Sabbahi MA (2011)H-reflex amplitude asymmetry is an earlier sign of nerve root involvement than latency in patients with S1 radiculopathy.BMC Res Notes5:102.
- Dawson DM (2012) The Effect of a Neurodynamic Treatment on Nerve Conduction in Clients with Low Back Pain.
- Weinstein JN,Lurie JD, Tosteson TD, Skinner JS, Hanscom B, et al. (2006)Surgical Vs. non operative treatment for lumbar disk herniation. JAMA 296: 2451-2459.
- Bakhtiary AH, Safavi-Farokhi Z, Rezasoltani A (2005) Lumbar stabilizing exercises improve activities of daily living in patients with lumbar disc herniation. J Back Musculoskeletal Rehabil 18: 55-60.
- Thackeray A, Fritz JM, Brennan GP, Zaman FM, Willick SE (2010) A pilot study examining the effectiveness of physical therapy as an adjunct to selective nerve root block in the treatment of lumbar radicular pain from disk herniation: a randomized controlled trial. PhysTher 90: 1717-1729.
- Schäfer A, Hall T, Müller G, Briffa K (2011) Outcomes differ between subgroups of patients with low back and leg pain following neural manual therapy: a prospective cohort study. Eur Spine J 20: 482-490.
- Mulligan BR(2004) Manual therapy: NAGS, SNAGS, MWMS etc. 5th edtn. Plane View Services Ltd, New Zealand.
- Mulligan BR(1993) Mobilisation with movement (MWM's). J Man ManipTher 1: 154e6.
- Vincenzino B, Paungmali A, Teys P (2007) MulliganâÂ?Â?s mobilization with movement, positional faults and pain relief: current concepts from a critical review of literature. Man Ther 12: 98-108.
- Davidson M,Keating JL (2002)A Comparison of Five Low Back Disability Questionnaires: Reliability and Responsiveness. PhysTher 82: 8-24.
- Shacklock M (2005) Improving application of neurodynamic (neural tension) testing and treatments: A message to researchers and clinicians (Editorial). Man Ther 10: 175-179.
- McGill S (2007) Low back disorders: Evidencebasednprevention and rehabilitation. 2ndedtn, Human kinetics, Ontario, Canada.
- Oskay D, Meriç A, Kirdi N, Firat T, Ayhan C (2010) Neurodynamic Mobilization in the Conservative Treatment of Cubital Tunnel Syndrome. J Manipulative PhysiolTher 33: 156-163.
- Kolakovic H (2013) Effects of neural mobilization on pain, straight leg raise test and disability in patients with radicular low back pain. Journal of health sciences 3: 109.
- Pfirrmann CW, Dora C, Schmid MR, Zanetti M, Hodler et al. (2004) MR ImageâÂ?Â?based Grading of Lumbar Nerve Root Compromise due to Disk Herniation: Reliability Study with surgical correlation. Radiology 230:583-588.
- Ahmed N, Tufel S, Khan MH, Khan PB (2013) Effectiveness of Neural Mobilization in Sciatica. Journal of Musculoskeletal Research 16: 4.
- van Rijn JC, Klemetsö N, Reitsma JB, Majoie CB, Hulsmans FJ, et al. (2005) Observer variation in MRI evaluation of patients suspected of lumbar disk herniation. AJR Am J Roentgenol 184: 299-303.
- Jensen MP, Turner JA, Romano JM (1994)What is the maximum number of levels needed in pain intensity measurement? Pain 58: 387-392.
- Childs JD, Fritz JM, Flynn TW, Irrgang JJ, Johnson KK, (2004) A clinical prediction rule to identify patients likely to benefit from spinal manipulation: a validation study. Ann Intern Med 141: 920-928.
- Stratford PW, Spadoni GF(2001) The reliability, consistency, and clinical application of a numeric pain rating scale. Physiothe Can 53:88-91.
- Stretanski MF (2004) H-reflex latency and nerve root tension sign correlation in Fluoroscopically guided, contrast-confirmed, translaminar lumbar epidural steroid-bupivacaine injections. Arch Phys Med Rehabil 85: 1479-1482.
- Fritz JM, George SZ, Delitto A (2001) The role of fear-avoidance beliefs in acute low back pain: relationships with current and future disability and work status. Pain 94: 7-15.
- Cleland JA, Childs JD, Palmer JA, Eberhart S (2006) Slump stretching in the management of non-radicular low back pain: a pilot clinical trial. Man Ther 11: 279-286.
- Gladson RB, Taciane SS, Danilo LT, Adriano PC, Alberito RC (2009) Neural mobilization and static stretching in an experimental sciatica model- an experimental study. Brazilian Journal of Physical Therapy 13.
- Mc Cracking HV (2008) The long-term effects of a neurodynamic treatment technique using a treatment-based classification approach to low back pain. Journal of Manual & Manipulative Therapy 16: 161-181.
- Bulbulian R, Burke J, Dishman JD (2002) Spinal reflex excitability changes after lumbar spine passive flexion mobilization. J Manipulative PhysiolTher 25: 526-532.
- Vicenzino B, Paungmali A, Teys P (2007) Mulligan's mobilization-with-movement, positional faults and pain relief: current concepts from a critical review of literature. Man Ther12:98-108.
- Bialosky JE, Bishop MD, Price DD, Robinson ME, George SZ (2009) The mechanisms of manual therapy in the treatment of musculoskeletal pain: a comprehensive model. Man Ther 14: 531-538.
- Kobayashi S, Yoshizawa H, Yamada S (2004) Pathology of lumbar nerve root compression part 2: morphological and immunohistochemical changes of dorsal root ganglion. J Orthop Res 22: 180-188.
- Goulet C, Arsenault AB, Levin MF, Bourbonnais D (1994) Absence of consistent effect of repetitive transcutaneous electrical stimulation on soleus H reflex in normal subjects. Arch Phys Med Rehab 75: 1132-1136.
Relevant Topics
- Electrical stimulation
- High Intensity Exercise
- Muscle Movements
- Musculoskeletal Physical Therapy
- Musculoskeletal Physiotherapy
- Neurophysiotherapy
- Neuroplasticity
- Neuropsychiatric drugs
- Physical Activity
- Physical Fitness
- Physical Medicine
- Physical Therapy
- Precision Rehabilitation
- Scapular Mobilization
- Sleep Disorders
- Sports and Physical Activity
- Sports Physical Therapy
Recommended Journals
Article Tools
Article Usage
- Total views: 17744
- [From(publication date):
August-2016 - Mar 31, 2025] - Breakdown by view type
- HTML page views : 16403
- PDF downloads : 1341