Comparison of Double Row Insertional Achilles Tendinopathy Repair with or without Flexor Hallucis Longus Tendon Transfer
Received: 25-Apr-2024 / Manuscript No. CRFA-24-133006 / Editor assigned: 29-Mar-2024 / PreQC No. CRFA-24-133006(PQ) / Reviewed: 13-May-2024 / QC No. CRFA-24-133006 / Revised: 20-May-2024 / Manuscript No. CRFA-24-133006 (R) / Published Date: 27-May-2024 DOI: 10.4172/2375-4494.S4.004
Abstract
Purpose: Insertion achilles tendinitis recalcitrant to conservative care may require surgical interventiodouble-row repair technique has been shown to have biomechanical advantages in cadaveric studies and rehabilitation advantages in clinical studies. The addition of a flexor hallucis longus tendon transfer has been advocated in certain instances, but studies have called into question the benefit of this transfer. A retrospective study of patients that had undergone a double-row achilles tendon reattachment was performed comparing those with and without an adjunctive transfer. Fifty-one patients were included, 19 in the group with transfer and 32 in the group without transfer. Time to weight bearing in a boot and a brace were similar between groups but return to normal activity was faster in the group without transfer (145 days vs. 186 days, p=0.05). The group with the transfer was similar in regards to BMI but did skew older (52.3 years vs. 59.5 years, p=0.01). No other differences between the groups were found, including satisfaction, complications/revisions, and other demographics. The addition of a flexor hallucis longus transfer did not lead to increased complications but did not show a clear benefit either. The recovery was slower with the transfer, but this may correlate with the increased age in this group.
Keywords
Sports; Speed bridge; Comparative; Haglunds; Tenodesis; Calcific tendinosis
Introduction
Surgical repair of insertional achilles tendinopathy after the failure of conservative measures is well studied. This has been explored through various incision and repair techniques [1-5]. Although repair without anchor and single-row anchor repair have been reported on, double-row repair has been reported to have a superior biomechanical profile and may have faster clinical recovery [6-8]. However, two recent articles have called into question the superiority of a double row repair compared to a single anchor. A review of 37 patients that came in for strength testing at an average of 2 years found no difference in strength or satisfaction between those fixed with a double row or single anchor [9]. And another paper with 110 patients found there was no difference in complications or revisions between these groups, but the double row was substantially costlier [10]. A recent report looked at two different types of double-row repair, knotted versus knotless, and determined there was no significant difference in outcomes [11].
Flexor Hallucis Longus (FHL) tendon transfer is an adjunct possible with insertional achilles tendon repair. Volumetric evaluation as a measure of strength of the calf muscles has been used to offer that the FHL can provide additional strength to the achilles tendon [12]. Indications for adding an FHL transfer have been in cases of severe tendon degeneration and in older and heavier patients [13-15]. However, a level randomized controlled trial in patients over 50 years old was not able to show a clear clinical outcome advantage of using an FHL tendon transfer. In a report of 39 patients, the authors found no difference in outcome scoring measures, patient satisfaction, or pain. The patients with the FHL transfer had greater ankle plantar flexion strength at the post-operative testing, and although there was also no loss of strength at the hallux in plantar flexion, the authors did caution that this could still manifest in younger patients. While the FHL as an adjunct was safe, it was not able to show clearly superior results [16].
The purpose of the present study is to compare the results of double-row surgical repair of insertional achilles tendinopathy with or without the addition of an FHL transfer. This will be measured with the return to activity and complication data points. The hypothesis is that both patient groups will have a similar recovery and complication rate. Secondary data will be demographics, past medical history, cost, satisfaction, strength testing, and adjunctive procedures.
Materials and Methods
The study primary aim was to compare the clinical results of achilles tendon double-row repair with or without an FHL transfer. The secondary aim was to compare the groups for other differences. The study was granted IRB approval. Surgical and billing records identified all patients that had surgical care for insertional achilles tendinopathy from July 2014 until November 2020. A manual review of patient operative notes was performed by a research assistant (TAR) not involved in the surgery to confirm the exact procedure performed and appropriateness for inclusion in the study.
Patients were included if surgery was performed at least one year prior to data retrieval, use of double-row achilles repair, as well as a record of any complications and revisions. Indication for FHL transfer was at the surgeon’s discretion, but in general, considered if over 60% of the tendon appeared to be involved on pre-operative MRI, BMI over 40, or patients older than 65. Only one of these criteria needed to be met to consider an FHL transfer but was not an absolute addition of the transfer. Additional data was recorded, but a complete record of all secondary data points was not needed for inclusion. Clinical follow-up was performed until patients were released, resulting in a large disparity of follow-up times based on the patient returning to the clinic after release. Exclusion criteria included patients treated for achilles tendon ruptures, midsubstance repairs, debridement without partial excision of the calcaneus, and repair other than double-row repair.
Variables collected from the review of the medical record include age, Body Mass Index (BMI), smoking history, obesity (BMI>30), diabetes, surgical data, recovery, complications, and revisions. Surgical data includes the cost of implants, adjunctive Gastrocnemius Recession (GSR), or FHL transfer. Recovery data points recorded include time to weight bearing in a boot, time to weight bearing in a brace, return to normal shoes, and return to normal activity. Time to weight bearing in a boot and time to weight bearing in a brace was available for all 51 patients (100%), and time to full release/normal activity was available for 32 patients (62.7%), and this encompassed 11 patients with FHL transfer (85.9%) and 21 patients with FHL transfer (65.6%). Chart review recorded the presence and specifics of complications, treatments, and revisions. Only complications related to the achilles repair were analyzed. This excluded 1 patient with swelling at the GSR site in the FHL group, and 1 patient with a scar at the GSR site, and 1 patient with ankle pain in the group without FHL transfer.
Patients were all treated in the prone position with general anesthesia. Prophylactic intravenous antibiotics were infused prior to elevating the tourniquet, with the specific drug based on hospital protocol and patient needs. A thigh tourniquet applied at 300 mmHg was elevated prior to incision. If a gastrocnemius recession was necessary, this was performed first.
Double-row repair of the achilles was performed through a central longitudinal incision along the posterior aspect of the achilles. The achilles was exposed, and the entire tendon was released and elevated from the calcaneus and inspected. Complete debridement of any diseased tendon was performed at this point. Then resection of the bursa and calcaneus was performed to remove all pathological tissue. The repair was performed with a double-row, suture bridge technique with two 4.75 mm anchors proximally used to bring the tendon to the calcaneus. Then a second row of two 4.75 mm anchors was placed distal to the achilles, and the sutures from the first row of anchors were crossed over the achilles in a crisscross pattern into the second row of anchors, providing a large footprint of repair of the achilles to the calcaneus (Speed Bridge™, Anthrax, Naples, Florida, USA) (Figure 1).
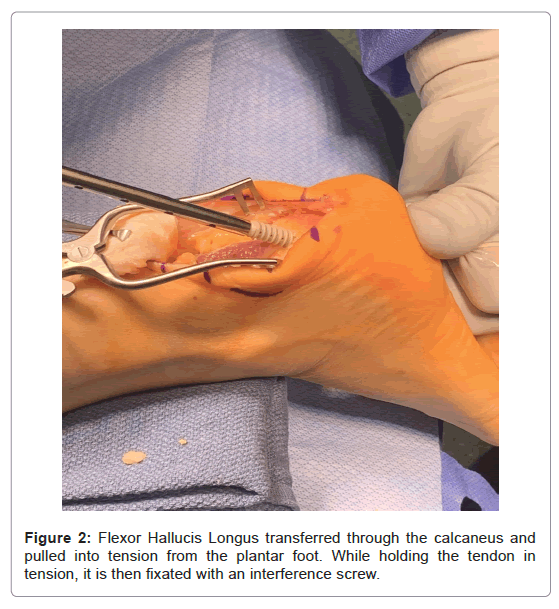
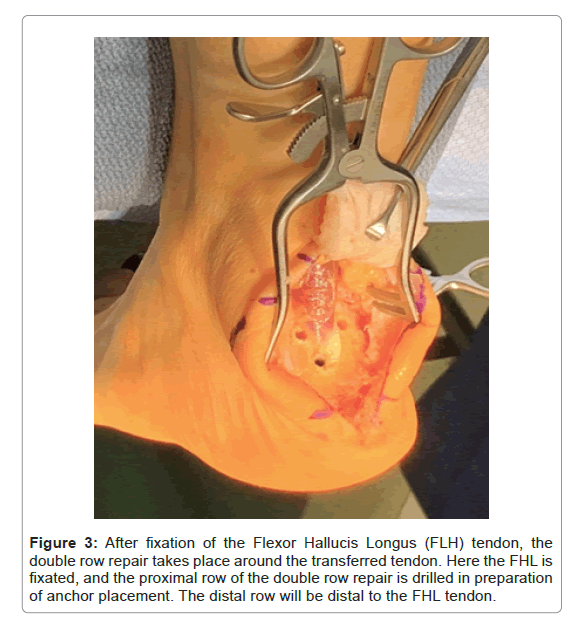
If a flexor hallucis longus tendon transfer was performed, it was done through the same incision. It was performed after achilles debridement and partial excision of the calcaneus and before the repair was performed. Fixation was performed with a 7 mm x 23 mm interference screw after passing the tendon from the dorsal to the plantar calcaneus (Tenodesis Screw, Anthrax, Naples, Florida, USA). The double-row repair was then performed around the fixated FHL tendon (Figures 2 and 3).
Figure 3: After fixation of the Flexor Hallucis Longus (FLH) tendon, the double row repair takes place around the transferred tendon. Here the FHL is fixated, and the proximal row of the double row repair is drilled in preparation of anchor placement. The distal row will be distal to the FHL tendon.
Patients were placed into a non-weight bearing plaster splint immediately after surgery, and follow-up was first at two weeks. Sutures were removed, the patient was placed into a below-the-knee walking boot and range of motion was started. Weight bearing was instituted at four weeks. The patient was then progressed from the boot to a brace, into physical therapy, and finally to a full release.
Statistics
Data sets of continuous variables (age, BMI, implant cost, time to WB in boot, time weight bearing in brace, and return to normal activity) are tested for normality using a Kolmogorov-Smirnov test. Age, BMI, time to weight bearing in a brace, and return to normal activity were found to be normally distributed, while implant cost and time to weight bearing in a brace were not normally distributed. Normally distributed variables are compared with a 2-tailed unpaired Student’s t-test. Non- normally distributed variables are compared with the 2-tailed Mann- Whitney U test. Categorical data (sex, tobacco use, past medical history variables, use of gastrocnemius recession, and complications and revisions) are compared with the 2-tailed Fisher’s exact test because certain conditions are a small cell count.
Results
A total of 51 patients met the criteria for inclusion, 19 in the group with FHL transfer and 32 in the group without FHL transfer. All surgeries were performed by a single author (JGD). All surgeries were performed at least 1 year prior to data collection, but specific follow-up time varied based on clinical assessment and was not recorded..
Recovery and complication data points are the primary outcome measure in this study. There were no statistically significant differences for time to weight bearing in the boot (p=0.78) and brace (p=0.59). In the FHL transfer group, these points were 27.5 ± 5.1 days (13-41 days) and 54.5 ± 10.4 days (41-83 days), respectively, and 27.4 ± 5.5 days (11-42 days) and 52.8 ± 11.0 days (39-84 days). However, there was a statistically significant longer time to return to normal activity in patients with an FHL transfer at 186.0 ± 53.2 days (111-246 days) compared to those without a FHL transfer at 145.1 ± 54.3 days (91-270 days), with p=0.05. Complications were recorded in 2 patients (10.5%) in the FHL transfer group, including 1 patient with neuropathy and 1 patient with cellulitis. In the group without FHL transfer, there were also 2 complications (6.3%), with 1 patient that had an achilles partial tear requiring revision and 1 patient with neuropathy. No difference was noted with p=0.62. Only one revision was noted in the study, a patient in the group without FHL transfer that had a partial tear after surgery that underwent achilles debridement with amniotic membrane augmentation (Table 1).
| Without FHL Transfer (n=32) | SD or Percentage | With FHL Transfer (n=19) | SD or Percentage | p value | |
|---|---|---|---|---|---|
| Time to WB in a boot (n=51) | 27.4 days | 5.5 days | 27.5 days | 5.0 days | 0.78 |
| Time to WB in a brace (n=51) | 52.8 days | 11.0 days | 54.5 days | 10.4 days | 0.59 |
| Return to normal activity (n=32) | 145.1 days | 54.3 days | 186 days | 53.2 days | 0.05 |
| Complications | 2 | 6.30% | 2 | 10.50% | 0.62 |
| Revisions | 1 | 3.10% | 0 | 0% | 1 |
Abbreviations: WB=Weight Bearing; FHL=Flexor Hallucis Longus; SD=Standard Deviation
Table 1: Recovery and Complications.
Secondary outcomes include demographics and past medical history. Age was a statistically significant difference in the two groups. The average age with FHL transfer was 59.5 ± 10.7 years old (38-79 years old) compared to the group without FHL transfer which was 52.3 ± 8.8 years old (28-79 years old) (p=0.01). No other statistically significant differences in demographics were identified. There were 10 females (52.6%) in the group with FHL transfer compared to 18 females (56.3%) without FHL transfer, p=1.00. In the group with FHL transfer, there were 2 current smokers (10.5%), 6 former smokers (31.6%), and 11 patients that never smoked (57.9%), compared to the group without FHL transfer with 3 current smokers (9.4%), 9 former smokers (28.1%) and 20 patients that never smoked (62.5%). No differences were noted when comparing current and former smokers to those who never smoked (p=0.49) or current smokers to former and those that never smoked (p=1.00). Obesity, defined as those above a BMI of 30, was noted in 16 patients (84.2%) in the FHL transfer group and 24 patients (75.0%) in the group without FHL transfer (p=0.51). Five patients (17.9%) had diabetes in the FHL transfer group compared to 4 patients (12.5%) without, p=0.58 (Table 2).
| Without FHL transfer (n=32) | SD or Percentage | With FHL transfer (n=19) | SD or Percentage | p value | |
|---|---|---|---|---|---|
| Age | 52.3 yrs | 8.8 yrs | 59.5 yrs | 10.7 yrs | 0.01 |
| Sex | 18 female | 56.30% | 10 female | 52.60% | 1 |
| BMI | 34.7 | 6.4 | 36.7 | 7.9 | 0.38 |
| Smoking Status | 3 current | 9.40% | 2 current | 10.50% | |
| 9 former | 28.10% | 6 former | 31.60% | 0.49 | |
| 20 never | 62.50% | 11 never | 57.90% | ||
| Morbid Obesity(BMI>30) | 24 patients | 75% | 16 patients | 84.20% | 0.51 |
| Diabetes | 4 patients | 12.50% | 5 patients | 17.90% | 0.58 |
| Side | 19 right | 59.40% | 11 patients | 57.90% | 1 |
| GSR | 27 patients | 84.40% | 16 patients | 84.20% | 1 |
| Implant cost | $1,811.29 | $169.47 | $1,971.84 | $478.71 | 0.73 |
Abbreviations: BMI=Body Mass Index; FHL=Flexor Hallucis Longus; SD=Standard Deviation; GSR Gastrocnemius Recession
Table 2: Secondary Outcomes of the Data.
Finally, adjunctive procedures and cost were compared as secondary measures. A Gastrocnemius Recession (GSR) was a common procedure in both groups, with 16 patients (84.2%) in the FHL transfer group and 27 (84.4%) in the group without FHL transfer (p=1.00). Cost was not statistically significantly different, even with the added procedure in the FHL transfer group. The cost was $1971.84 ± $478.71 ($590-$2430) in the FHL transfer group and $1811.29 ± $169.47 ($1660-$1995) in the group without FHL transfer (p=0.73) (Table 2).
Discussion
Insertional achilles tendinosis that is unresponsive to conservative treatments is traditionally surgically addressed with proper calcaneal resection, achilles debridement, and achilles reattachment. Some experts have advocated for the addition of augmentation with a flexor hallucis longus tendon transfer. Hunt et al. showed satisfactory results with no difference in complication rates in 39 patients with or without FHL transfer in the surgical treatment of insertional achilles tendinosis [16]. Our study showed similar findings with no statistical difference in complication rates between the two groups, with a complication rate of 10.5% in the FHL transfer group versus 6.3% in the group without.
Another data point we evaluated was time to weight bearing following surgical intervention. There were no statistically significant differences for time to weight bearing in the boot. The double row group without FHL transfer had a mean interval time to weight bearing of 27.4 days compared to the FHL group of 27.5 days. Rigby et al. showed comparable findings in a review of 43 patients who underwent double- row repair, with a mean interval to weight bearing of 10 days [17].
The final data point that we evaluated was time to normal activity reported a mean interval time to normal activity of 159 days with a modified double-row technique [18]. We showed similar findings in our double-row group without an FHL transfer at a mean interval time to normal activity of 145 days. However, there was a statistically significant longer time to return to normal activity in patients with an FHL transfer at 186 days. The patients in the FHL transfer group were significantly older in age, which could cause the increased time to return to normal activity.
Our study had inherent limitations within its retrospective nature and lack of prospective data and objective pre- and post-operative outcomes scores. Another limitation was the lack of variability in procedure selection since a single surgeon performed the procedures, and indication for FHL was at his discretion. Specific follow-up data was not available for each patient. Data retrieval from the chart review was performed at least 1 year after the surgical intervention, to allow for any complication or surveillance of other untoward events. However, if patients left the practice and were lost to follow-up, this could not be tracked.
Conclusion
In conclusion, we have reported that double-row repair for insertion achilles tendinitis was successful with low complication rate. The addition of an FHL tendon transfer did not show a statistically significant increase in the complication rate but did show that patients had a slower return to normal activities, which may also correlate with the advanced age of the patients.
Acknowledgements
IRB approval #17-038E through Advocate Aurora Health Research Subject Protection Program.
References
- Thompson JM, Nguyen K, Ahluwalia J, Casciato D, Tewilliager T, et al. (2021) Surgical takedown approaches to insertional Achilles tendinopathy: a systematic review. J Foot Ankle Surg 60:1217-1221.
[Crossref] [Google Scholar] [PubMed]
- Shakked RJ, Raikin SM (2021) Insertional tendiopathy of the Achilles:Debridement, primary repair, and when to augment. Foot Ankle Clin 22:761-780.
[Crossref] [Google Scholar] [PubMed]
- Irwin TA (2010) Current concept review:Insertional Achilles tendinopathy. Foot Ankle Int 31:933-939.
[Crossref] [Google Scholar] [PubMed]
- Myerson MS, Mc Garvey W (1998) Disorders of the insertion of the Achilles tendon and Achilles tendinits. J Bone Joint Surg Am 80:1814-1824.
- Devries JG, Summerhays B, Guehlstorf DW (2009) Surgical correction of Halgund’s triad using complete detachment and reattachment of the Achilles tendon. J Foot Ankle Surg 48:447-451.
[Crossref] [Google Scholar] [PubMed]
- Beitzel K, Mazzocca AD, Obopilwe E, Boyle JW, McWIlliam J, et al. (2013) Biomechanical properties of double-and single-row suture anchor repair for surgical treatment of insertional Achilles tendinopathy. Am J Sports Med 41:1642-1648.
[Crossref] [Google Scholar] [PubMed]
- Pilson H, Brown P, Stitzle J, Scott A (2012) Single-row versus double-row repair of the distal Achilles tendon: a biomechanical comparison. J Foot Ankle Surg 51:762-766.
[Crossref] [Google Scholar] [PubMed]
- DeVries JG, Scharer BM, Donnay RL, Romdenne TA (2024) No loss of strength after insertional Achilles tendon reconstruction with single-anchor or double-row repair. J Foot Ankle Surg 63:22-26.
[Crossref] [Google Scholar] [PubMed]
- DeVries JG, Scharer BM (2023) Double row fixation is more costly and does not have clinical benefit over single anchor for insertional Achilles tendon surgery. J Foot Ankle Surg 62:618-622.
[Crossref] [Google Scholar] [PubMed]
- Rigby RB, Cottom JM, Vora A (2013) Early weightbearing using Achilles suture bridge technique for insertional Achilles tendinosis: a review of 43 patients. J Foot Ankle Surg 52:575-579.
[Crossref] [Google Scholar] [PubMed]
- Scott AT, Long CS, Jaramillo TJ, Marois AJ (2022) Review of Achilles tendon reattachment using double-row knotted and knotless techniques in the management of insertional Achilles tendinopathy. J Foot Ankle Surg 61:927-931.
[Crossref] [Google Scholar] [PubMed]
- Jeng CL, Thawait GK, Kwon JY, Machado A, Boyle JW, et al. (2012) Relative strengths of the calf muscles based on MRI volume measurements. Foot Ankle Int 33:394-399.
[Crossref] [Google Scholar] [PubMed]
- Mc Garvey WC, Palumbo RC, Baxter DE, Leibman BD (2002) Insertional Achilles tendinosis: surgical treatment through a central tendon splitting approach. Foot Ankle Int 23:19-25.
[Crossref] [Google Scholar] [PubMed]
- Elias I Raikin SM, Besser MP, Nazarian LN (2009) Outcomes of chronic insertional Achilles tendinosis using FHL autograft through single incision. Foot Ankle Int 30:197-204.
[Crossref] [Google Scholar] [PubMed]
- Den Hartog BD (2003) Flexor hallucis longus tendon transfer for chronic Achilles tendinosis. Foot Ankle Int 24:233-237.
- Hunt KJ, Cohen BE, Davis WH, Anderson RB, Jones CP et al. (2015) Surgical treatment of insertional Achilles tendinopathy with or without flexor hallucis longus tendon transfer: a prospective, randomized study. Foot Ankle Int 36:998-1005.
[Crossref] [Google Scholar] [PubMed]
- Rigby RB, Cottom JM, Vora A (2013) Early weightbearing using Achilles suture bridge technique for insertional Achilles tendinosis: a review of 43 patients. J Foot Ankle Surg 52:575-579.
[Crossref] [Google Scholar] [PubMed]
- Saxena A, Mafulli N, Jin A, Isa E, Arthur WP, et al. (2021) Insertional Achilles tendinopathy: analysis of 166 procedures and return to activity. J Foot Ankle Surg 60:1117-1123.
Citation: Devries JG, Romdenne T, Scharer BM (2024) Comparison of Double Row Insertional Achilles Tendinopathy Repair with or without Flexor Hallucis Longus Tendon Transfer. Clin Res Foot Ankle S4:004. DOI: 10.4172/2375-4494.S4.004
Copyright: © 2024 Devries JG, et al. Comparison of Double Row Insertional achilles Tendinopathy Repair with or without Flexor Hallucis Longus Tendon Transfer.
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 632
- [From(publication date): 0-2024 - Apr 07, 2025]
- Breakdown by view type
- HTML page views: 454
- PDF downloads: 178