Comparison of Diet, Exercise and Auricular Vagus Nerve Stimulation Effectiveness for Weight Reduction in Obese Individuals
Received: 01-Jan-2024 / Manuscript No. jowt-23-121887 / Editor assigned: 03-Jan-2024 / PreQC No. jowt-23-121887 / Reviewed: 17-Jan-2024 / QC No. jowt-23-121887 / Revised: 22-Jan-2024 / Manuscript No. jowt-23-121887 / Accepted Date: 28-Jan-2024 / Published Date: 29-Jan-2024 DOI: 10.4172/2165-7904.1000647 QI No. / jowt-23-121887
Abstract
Background: This study investigated the effects of diet, exercise, and vagus nerve stimulation (VNS) methods on body composition, functional capacity, and blood parameters in the short term.
Methods: We performed our research in obese individuals(N:90) aged 18-65 years, who were stage I, II, and III according to WHO. Laboratory measurements and evaluation scales of individuals in the Diet, Exercise, and VNS groups were compared. Anthropometric changes were recorded as well as changes in functional capacity (6-minute walk test(6MWT)), muscle strength (hand grip strength test); stair climbing test(SCT), food choice (Excessive food cravings Questionnaire(FCQ), Visual analog scale(VAS), and quality of life(The 36-Item Short Form Health Survey questionnaire(SF-36)).
Results: A weight loss of 4%-10% in total body weight (4.7–10.4 kg) in a 4-week period improved anthropometric features, functional capacity, and quality of life (p <0.05). Considering the parameters and tests examined in the study, although there were no statistically significant differences between the groups, it was observed that there was a positive effect on health status in all 3 groups compared to the beginning of the study. Weight loss was statistically significant in DG compared to other groups (p <0.05). Percentage distribution of weight loss, respectively, Diet Group(DG): 10%; Exercise Group(EG): 6%; VNS Group: 4%.
Conclusion: 3 different methods - diet, exercise, and VNS - that we have examined in a 4-week period were effective in creating weight loss. Although there is no significant weight loss with auricular VNS, it has been observed as a result of the scale data that there may be a behavioral change in terms of appetite/food choice orientation. We think that auricular VNS can be used alone or in addition to other weight loss methods in the treatment of obesity. There is a need for long-term research on this three methods related to body weight change.
Keywords
Auricular vagus nerve stimulation; Diet; Obesity; Exercise; Weight loss
Introduction
Obesity is a chronic, recurrent disease process that is increasing in prevalence worldwide and affects both children and adults (Bray et at,2017; Hales et al, 2018; Rodgers et al, 2018). According to the data specified by the World Health Organization (WHO) in 2020, more than 650 million adults suffer from obesity, and its prevalence as the most important global public health problem has increased rapidly in the last 50 years (World Health Organization, 2020). Most guidelines for obesity treatment recommend a comprehensive lifestyle program as a first step (Jensen et al, 2013 [1]; Garvey et al, 2016 [2]; Apovian et al, 2015 [3]; Ryan & Kahan, 2018 [4-6]). This recommendation is derived from large lifestyle intervention studies that have developed programs around changing behaviors based on changing food intake and physical activity (Paixao et al, 2020). However, in terms of sustainability, it may be necessary to add new alternative treatments to behavioral changes and lifestyle interventions in the long term. Autonomic nervous system controls the visceral functions of the body, plays a role in maintaining homeostasis, and is mainly controlled by centers located in the spinal cord, brain stem, and hypothalamus. The parasympathetic system, which forms the autonomic nervous system together with the sympathetic nervous system, consists of the 3rd, 7th, 9th, and 10th cranial nerves and sacral spinal nerve roots, and distributes to the visceral organs by traveling within the vagus nerve (VN) (10th cranial nerve), which constitutes 75% of all parasympathetic nerves. The effects of the VN on the treatment of obesity focus on the interaction between the central nervous system (CNS) and the gastrointestinal system. It has also been shown that VN afferent neurons transmit information to the brain in the control of food intake, thus contrabuting homeostasis.
Findings in studies on VNS suggest that the VN is associated with the neurobiological systems related to hunger and satiety. In line with these data, our study was planned to compare the effectiveness of noninvasive auricular VNS application, on obesity, by weight loss with diet and exercise methods.
Method
Inclusion and exclusion criteria
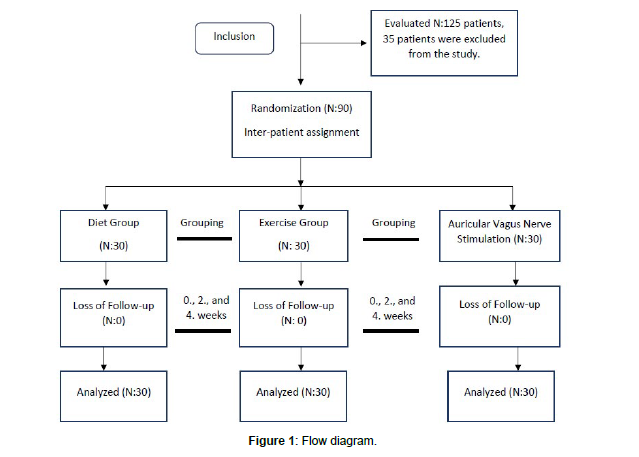
This study was carried out randomly, with 3 different treatment approaches planned to be performed on 3 groups (Each group N:30) for 4 weeks (Figure 1). It was approved by the Medipol University Clinical Research Ethics Committee (Study Registration E-10840098- 772.02-3009). The study has also been registered on ClinicalTrials.gov (ID number: NCT05511376). Included participants were overweight and obese individuals (N:90) aged 18-65 years with a BMI ≥25 kg/ m2 (WHO degree of obesity Stages I, II, and III) who agreed for diet, exercise, or VNS therapy. Those with unstable Diabetes Mellitus (DM), unstable hypertension, cardiovascular disease (like myocardial infarction), pulmonary disease, kidney disease, orthopedic restrictions, motor neuron disease (MND), and wheelchair mobilization were excluded from the study.
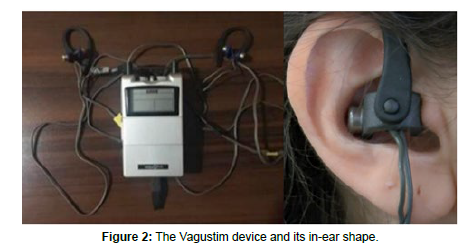
Vagus nerve stimulation group
Vagustim device was applied to the participants bilaterally from the ears with a frequency of 10 Hz and a pulse width of 300 μs in a biphasic current mode. The current intensity was kept constant where the participants felt comfortable sensation. A total of 12 sessions were applied during the study, with 3 sessions of 30 minutes per week. The application was performed from the tragus and concha parts of the ear (Figure 2).
Diet group
The protein intake of the participants was organized as 30% of the total daily calories or 1–1.2 g/kg. The Mediterranean-type, proteinbased diet program was prepared specifically for the participants.
Exercise group
Participants were asked to walk at moderate intensity for 30 minutes, 5 days a week, as aerobic exercise (AE). Heart rate was calculated by averaging according to Karvonen and American Council on Exercise (ACE) formulations. Activity requiring 40-59% of heart rate reserve was defined at baseline. Depending on individual tolerance, participants were encouraged to increase this rate to 60-80%. A home exercise program (ie, warm-up and stretching; elastic band resistance exercises (RE)) was prepared to burn an average of 500-750 kcal in each 1-hour session, 3 days a week. REs were made using elastic bands. Specific muscle groups were targeted (ie, pectoral arch, biceps, triceps, gluteal, hip abductors, quadriceps, and hamstrings). A 4/7-strength green 1.5 m tape was used for exercise by female patients and a 5/7-strength blue 1.5 m tape was used by male patients. The number and sets of muscle group exercises were gradually increased under the supervision of the physiotherapist: week 1 = 2 sets/8 reps; 2nd week = 2 sets/10 reps; Weeks 3 and 4 = 3 sets/10 reps.
Evaluation methods
BMI and weight: Participants' BMI and weight loss were assessed at study initiation, Weeks 2 and 4.
Activity level: The activity levels of the participants during the study were monitored in order not to go beyond the applied treatment procedure. The patients' activity levels were assessed with the International Physical Activity Questionnaire (IPAQ-short), a selfadministered patient questionnaire describing the current physical activity level at baseline and at weeks 2 and 4.
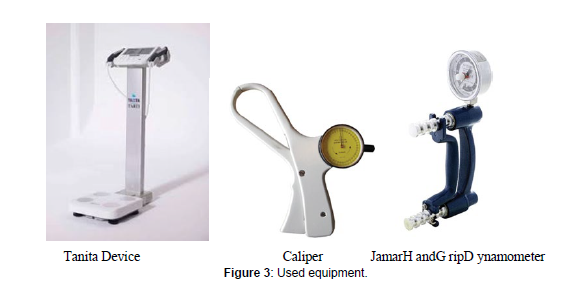
Body fat and muscle mass
Changes in anthropometric measurements were recorded. Bone, fat, and muscle mass as well as total body fluid mass were measured with the Tanita device and total skinfold thickness was measured with the Skinfold. To determine whether there was any change in the arm and hand muscle strength, right and left-hand grip strength was evaluated with a hand dynamometer. SCT was used as a method to measure potential functional change in lower extremity muscle strength in RE.
Fasting Blood Sugar, HDL, LDL, TG, and Total Cholesterol
At the baseline of the study and at the end of the 4th week, FSB (fasting(preprandial) blood sugar), HDL (high-density lipoprotein), LDL (low-density lipoprotein), TG (Triglyceride), and Total cholesterol values were measured to examine the effectiveness of weight loss (Ryan & Yockey 2017).
Dyspnea
The 6MWT was used to compare group walking distance averages and to assess dyspnea symptoms in the context of the Pre- and Post- Gait Modified Borg Dyspnea Scales (Pre-MBDS/Post-MBDS). The Borg scales provided a validated numerical scoring system (score range 0-10) to measure the severity of patient-reported dyspnea symptoms during moderate exercise. Systolic/diastolic blood pressure, pulse rate, and oxygen (O2) saturation were also evaluated as indicators of dyspnea before and after.
Appetite and food choice
Participants were asked to fill out an Internationally validated Excessive Food Craving Questionnaire to assess appetite status at baseline and at Week 4. The visual analog scale (score range 0-10) was applied at the beginning of the study and at the 4th week for sweet and salty food choices.
Quality of life
The SF-36 scale was completed by participants at baseline and at Week 4 to assess the impact of their current weight on physical performance, mood, and overall health.
Statistical analysis
In the descriptive statistics of the data, mean, standard deviation, median minimum, maximum, frequency, and ratio values were used. The distribution of variables was measured with the Kolmogorov- Smirnov test. ANOVA(Tukey test), Kruskal-Wallis, and Mann- Whitney U test were used in the analysis of quantitative independent data. The chi-square test was used in the analysis of qualitative independent data. SPSS 28.0 program was used in the analysis.
Results
When the demographic characteristics of the 3 groups were examined for comparative evaluations, no statistically significant difference was observed in terms of age, height, and gender (p >0.05). There was also no significant difference between the groups in the before and after systolic/diastolic blood pressure values (p >0.05).
BMI and weight changes
There was no significant difference between groups in BMI or total body weight at the start of the study (p >0.05). BMI values at Week 2 and Week 4 were significantly (p <0.05) lower in the diet group than in the exercise and VNS groups. There was no significant difference (p >0.05) in the 2nd week and 4th week BMI values between the exercise and VNS groups (Respectively, 4-week mean decrease DG: 3.7 kg/m2, EG: 1.9kg/m2, VNS:1.9kg /m2).
The amount of weight loss in the 2nd week and 4th week in the diet group was significantly higher (p <0.05) than in the exercise and VNS groups. The amount of weight loss at Week 2 in the exercise group was significantly (p <0.05) higher than the VNS group. The amount of weight reduction at Week 4 in the exercise group was not significantly different (p >0.05) from the VNS group.
Activity level outputs
Patient responses to the IPAQ short questionnaire increased only in the Exercise group, as expected. No significant difference was observed in the other groups (p >0.05).
Body fat and muscle mass changes
At the end of the 4-week period, body density increased in all three groups due to the decrease in fat mass. In all three groups, there was a decrease in total skinfold thickness, as well as a decrease in waist, hip, right-left middle-upper arm, right-left femur, and right-left lower leg circumferences and waist/hip ratios (p ˂0.05). There was no statistically significant difference between waist/hip measurements at baseline, 2nd week, and 4th week (p >0.05).
The decrease in body fat mass was significantly higher in the diet group than in the exercise and VNS groups (mean fat mass loss: 8.3 kg).
At the end of the 4-week study, while muscle mass loss was less in only the exercise group (Loss muscle mass in 4 weeks - average DG: 2.00 kg; VNS: 1.2 kg; EG: 0.5 kg), total body fluid mass and bone mass did not differ significantly between the 3 groups.
The 4th-week right-hand grip test (HGT) score reduction was significantly (p <0.05) lower in the exercise group than in the diet and VNS groups. There was no significant difference (p >0.05) in the 4th week right HGT score reduction between the diet and VNS groups.There was no significant difference (p >0.05) in the 4th week left HGT score decrease between diet, exercise, and VNS groups.
The amount of decrease in the total duration of SCT did not differ significantly (p >0.05) between the three groups.
Changes in Fasting Blood Sugar, HDL, LDL, TG, and Total Cholesterol.
There was no statistically significant difference between the groups in the baseline and 4th-week results of FSB, HDL, LDL, TG, and Total Cholesterol values observed to control the effectiveness of weight loss (p>0.05). However, among these values, postprandial blood sugar, LDL, TG and Total Cholesterol values decreased in all three groups, while HDL values increased.
Dyspnea results
After 6MWT, there was no statistically significant difference between the groups in functional capacity or pre-gait modified Borg dyspnea scale (Pre-gait MBDS) and post-walk modified Borg dyspnea scale (Post-gait MBDS) scales (p ˃0.05); however, a significant decrease was observed in the post-MBDS scores in all three groups compared to baseline (p <0.05). There was no significant difference between the groups in the walking distances reached at week 4 (p ˃0.05).
Appetite and food choice changes
The decrease in appetite score at week 4 in the diet and VNS group was significantly (p <0.05) higher than in the exercise group. There was no significant difference (p>0.05) in the decrease in appetite score at week 4 between the diet and VNS groups.
In the diet and VNS group, the decrease in the desire to eat sweets score in the 4th week was significantly (p<0.05) higher than the exercise group. There was no significant difference (p> 0.05) between the diet and VNS groups in the 4th week of sweet craving score reduction.
There was no significant difference (p> 0.05) between the diet, exercise, and VNS groups in the decrease in the desire to eat salty in the 4th week.
Quality of life
There was no significant difference between the three groups in the results obtained from the Short Form 36 scale (p>0.05). However, a significant difference was observed in intragroup measurements (p<0.05).
Discussion
In our study, in which the effects of exercise, diet, and VSS methods on weight control were examined for a short time, it was observed that all three methods cause weight loss, in addition, they can make positive changes in obesity-related anthropometric parameters and can be used as alternatives to each other for weight loss. As stated by van Baak and Mariman, high protein diets (HPD), are promising types of diet that creates a negative energy balance by increasing the feeling of satiety and reducing fat mass. Especially the secretion of intestinal neuropeptides, which play an active role in the formation of the satiating effect, is the most prominent feature of HPD, and thanks to this effect, it helps to maintain successful weight loss along with a decrease in energy intake. In addition, diet-induced thermogenesis, the “thermic effect of food,” is highest for protein. These types of HPDs may also help maintain lean body mass during weight loss. A meta-analysis published in 2020 also showed that protein supplementation can help individuals maintain lean body mass. However, it is a known fact that its effects on muscle strength and synthesis are not clear. When we looked at our study data, we observed a different result from the findings of Pasiakos. Although we saw an effective weight loss (Mean: 10.4 kg) with YPD in a short period of 4 weeks, we encountered a decrease in lean body mass. In addition, we can say the following about the view of Wirth et al that YPD will affect muscle strength and muscle synthesis as a result. While there was a loss in body muscle mass as a result of the measurements we took in (Figure 3). the study (Average Body Muscle Mass Loss: 2 kg), the measurements we evaluated for HGT showed that there was a statistically significant difference in the grip strengths of the right and left hands, which indicates that it is not sufficient for the preservation of muscle strength (Mean Right HGT: 1.5 kg; Average Left HGT: 0.7 kg loss was observed.). Therefore, in our study, we think that the application of a protein-based diet may cause loss of muscle strength and mass. Physical activity has two known important roles. The first is to support the energy deficit and the second is to preserve muscle mass. Studies have shown that an exercise protocol that includes both AE and RE is the only component that can significantly change Total Energy Expenditure (TEE). In defense of this idea, AE supports fat burning, RE plays an important role in maintaining weight loss, and at the same time, it is effective in maintaining lean muscle mass, which determines basal metabolic rate (BMR). Because in cases of weight loss with the loss of muscle mass, there is a decrease in BMR. RE reduces the loss of lean muscle mass during weight loss. In the studies published by Agergaard et al and Liu et al, the role of RE in increasing muscle mass and muscle strength was expressed as a decrease in catabolic levels simultaneously with an increase in skeletal muscle protein expression. Based on these data, we can say that the AE and RE combination we have given is effective in burning fat and preserving lean muscle mass without changing the diet in any way. In the 4-week period, an average of 3.6 kg loss in fat mass was observed, while a 0.5 kg loss in total body muscle mass was observed. These data support the view of Tchang et al and Fothergill et al that the loss of muscle mass may be less during weight loss in RE. In addition, based on the studies published by Agergaard et al and Liu et al, if we try to explain the role of RE in increasing muscle mass and muscle strength with the HGT results we have done in our study, we can say that there was no statistically significant difference (p>0.05) with the initial data (Right HGT: 0.5 kg; Left HGT: 0.5 kg loss was observed). When we encounter such a result, it may be that the patients are tired because the measurements are repeated 3 times. VN is the main neural pathway that carries information to the gastrointestinal tract. In a review published by McClelland et al, it was stated that VNS induces brain satiety signals by mimicking anorexigenic hormonal signals, resulting in both a decrease in body weight and a feeling of satiety. In addition, it has been stated that the effects of VNS on body weight can also be manifested by changes in appetite/nutritional choice behaviors and metabolism. In human and animal studies, it has been shown that especially with VNS, the desire to eat sweets and the preference for high-carbohydrate food decreases. This situation has been tried to be explained in relation to body composition parameters such as weight, BMI, increased energy expenditure due to adipose tissue activity, and metabolic activities observed in glucose metabolism (de Lartigue 2016). Looking at the studies published in recent years, it is understood that VNS is important for short-term control of food intake, while it is stated that it also plays a role in long-term energy balance. With the noninvasive auricular VNS method we applied in our study, we observed a statistically significant (p<0.05) difference especially in food craving and sweet eating craving scores, while no significant difference was observed in salty cravings (p>0.05). These data support the work of Bodenlos et al and the work of Val-Laillet (Bodenlos et al, 2007b; Val-Laillet et al, 2010). On the other hand, weight loss (4.3 kg) was observed, unlike Val-Laillet et al's view of preventing weight gain rather than weight loss. This may be the result of stimulation of the auricular branch of the VN with different stimulation parameters, affecting different brain regions (for example, the hypothalamus). On the other hand, feeding behavior was investigated in the study published by Khan et al. 12% weight loss (~ 6kg) was observed after cervical implanted VNS application. However, when the cervical VNS was restarted after a 6-month interval, it was reported that the weight remained stable despite the higher current amplitude. This case study has similar results to the study of Pardo, in which there is a relationship between baseline BMI values and weight loss. It supports the view that a significant effortless weight loss can be achieved in proportion to BMI. In line with the data in our study, we observed that weight loss occurred in proportion to BMI. In the measurements carried out in 2-week periods, a 2.4 kg loss was observed with a decrease of 0.7 kg/m2 in BMI in individuals with an average BMI value of 36.8 kg/m2, while a loss of 1.9 kg was observed despite a 1.2 kg/m2 decrease in the average BMI value in the last 2-week measurements (2nd week BMI average: 36.1 kg/m2; 4th week BMI average: 34.9 kg/m2). The 30-minute neuromodulation current we applied may have an effect on obtaining this result. Apart from this, some studies try to explain the neurohormonal mechanism focused on the fact that dysfunction in vagal afferent neurons may cause hyperphagia and weight gain, and there are reported effects on body weight, metabolism, and adipose tissue activity in animal models in studies using the invasive VNS method. When the changes in muscle mass loss in our study were examined, it was observed that it was less than the dietary intervention, which indicates that VNS may be more effective in neurohormonal stimulation compared to a high protein diet, although it is not clear. On the other hand, another published literature states that modest weight loss (especially a 5%-10% reduction in body weight) improves glycemia, blood pressure and lipids, drug requirement, mobility, and quality of life in order to reduce disease risks and improves health in obese or overweight individuals. In another study published by Bray and Ryan, it was stated that 3% weight loss was effective for improvements in glycemia and triglycerides, and 5% weight loss was effective for improvements in lipid and blood pressure. In light of these data, when we evaluated our study in terms of blood parameters, it was observed that there were positive changes in FSB, HDL, LDL, TG, and Total Cholesterol values despite the shortterm evaluation process. Apart from this, the SF-36 test, which we used to evaluate the quality of life in the study, and the 6 MWT and parameters for functional evaluation, although the SCT scores did not differ significantly between the groups, they showed a positive change in the dynamics within the group. In this respect, our study data supports the literature data (weight loss percentage distribution, respectively, mean DG: 10%; EG: 6%; VNS: 4%). Although the present findings are based on a comparative study, their implications are limited due to the short duration of the study and the single-blind randomization(Single-blind randomization was applied at the time of the selection of study participants). No side effects were observed in the study groups.
Conclusion
Among the 3 alternative weight loss methods we have examined in the short term; diet, exercise, and VNS methods can be used as alternatives or combined in the weight loss process. By stimulating the neurohormonal mechanism with auricular VNS, behavioral changes can be created in terms of appetite/food choice orientation. Thus, it can be predicted that weight reduction can be achieved in the short term without any diet or exercise. Short and long-term studies with more participants are needed.
Informed Consent
Informed consent was obtained from all study participants.
Ethical Approval Statement
All procedures of the study are compliant with the ethical standards of the Medipol University Clinical Research Ethics Committee (Study Registration E-10840098-772.02-3009) and with the 1964 Helsinki declaration and its later amendments.
Conflict of Interest
Ali Veysel Ozden is the co-founder of the Vagustim Company
Grant Support
None
References
- Biesalski HK, Erdman JW, Hathcock J, Ellwood K, Beatty S, et al. (2013) Nutrient reference values for bioactives: new approaches needed? A conference report.Eur J Nutr 52:1-19.
- Cai Y, Sun M, Corke H (2003) Antioxidant activity of betalains from plants of the Amaranthaceae. J Agric Food Chem 51:2288-2294.
- Stintzing FC, Carle R (2007) Betalains-emerging prospects for food scientists. Trends Food Sci Technol 18:514–525.
- Sarker U, Oba S (2018) Catalase, superoxide dismutase and ascorbate-glutathione cycle enzymes confer drought tolerance of Amaranthus tricolor. Sci Rep 8:16496.
- Sjögren K, Endhal C, Henning P, Lerner UH, Tremaroli V, et al. (2012) The gut microbiota regulates bone mass in mice. J Bone Miner Res 27:1357-1367.
- Sarker U, Oba S (2019) Salinity stress enhances color parameters, bioactive leaf pigments, vitamins, polyphenols, flavonoids and antioxidant activity in selectedAmaranthusleafy vegetables.J Sci Food Agric 99:2275-2284.
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Citation: Gozde IN, OZDEN AV (2024) Comparison of Diet, Exercise and AuricularVagus Nerve Stimulation Effectiveness for Weight Reduction in Obese Individuals.J Obes Weight Loss Ther 14: 647. DOI: 10.4172/2165-7904.1000647
Copyright: © 2024 Gozde IN, et al. This is an open-access article distributed underthe terms of the Creative Commons Attribution License, which permits unrestricteduse, distribution, and reproduction in any medium, provided the original author andsource are credited.
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 586
- [From(publication date): 0-2024 - Apr 03, 2025]
- Breakdown by view type
- HTML page views: 393
- PDF downloads: 193