Thesis Open Access
Comparison of Diagnostic Performance of Multi Detector CT Angiography with Conventional Coronary Angiography for Assessment of Coronary Artery Disease
Surya Narayan Bayar and Qian Yin Feng*
Department of Radiology & Imaging, Anhui Medical University, Hefei, Anhui, China
- *Corresponding Author:
- Qian Yin Feng
Department of Radiology & Imaging, Anhui Medical University
81 Meishan Road, Sushan District, Hefei, Anhui, China
Tel: +86-13866187805
E-mail: 894206876@qq.com
Received date: January 01, 2017; Accepted date: August 03, 2017; Published date: August 08, 2017
Citation: Bayar SN, Feng QY (2017) Comparison of Diagnostic Performance of Multi Detector CT Angiography with Conventional Coronary Angiography for Assessment of Coronary Artery Disease. J Pain Relief 6: 299. doi:10.4172/2167-0846.1000299
Copyright: © 2017 Bayar SN, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Pain & Relief
Abstract
Aim: The point of this study was to reflectively assess the analytic exactness of multi detector angiography as a different option for conventional coronary angiography in evaluating coronary artery disease.
Materials and Methods: This review study selected 57 patients, who experienced both conventional coronary angiography (CCA), and additionally multi-detector computed coronary angiography (MDCT). Aggregate of 931 open segments were studied. Of which 95 portions indicated shifted level of stenosis, with 34 segments <50% stenosis, 43 segments 50-70% stenosis and 18 segments >70% stenosis.
Results: The affectability and specificity of 64 slice MDCT for identifying stenosis in <50%, 50-70% and >70% are 78.57% and 99.34%; 81.08% and 99.33%; 87.5% and 99.78%. The positive predictive value (PPV) and negative predictive value (NPV) are 78.57% and 99.34%; 83.33% and 99.22%; 87.5% and 99.78% individually. Over all exact nesses are 88.95%, 90.2% and 93.64% separately. There was no critical contrast in analytic exactness between conventional coronary angiography and 64 slice computed tomography in moderate (50-70%) and additionally severe (>70%) stenosis (p>0.05). Be that as it may, critical contrast was found in gentle (<50%) stenosis (p<0.05).
Conclusion: Indicative exactness of multi detector coronary angiography (MDCT) was found to be higher in moderate and extreme stenosis and can be utilized as a substitute to conventional coronary angiography (CCA).
Keywords
MDCT (Multi-detector computed coronary angiography); CAD (Coronary artery disease); CCA (Conventional coronary angiography); Coronary segments
Abbreviations
AVM: Arteriovenous Malformations; CAD: Coronary Artery Disease; CCA: Conventional Coronary Angiography; CCTA: Coronary Computed Tomography Angiography; CHD: Coronary Heart Disease; cMPR: Curved Multi Planar Reformation; CMRA: Coronary Magnetic Resonance Angiography; DMRI: Dobutamine stress Magnetic Resonance Imaging; DSA: Digital Subtraction Angiography; ICA: Invasive Coronary Angiography; LAO: Left Anterior Oblique; MDCCA: Multi Detector Computed Coronary Angiography; MDCT: Multi-Detector Computed Tomography; MIP: Maximum Intensity Projection; MPR: Multi-Planar Reformation; MRA: Magnetic Resonance Angiography; RAO: Right Anterior Oblique; SSFP: Steady-State with Free-Precession; VRT: Volume- Rendering Technique
Introduction
Coronary disease supported outline is the primary wellspring of death around the globe [1,2]. It is the after effect of gathering of plaques inside the dividers of the coronary artery (that supply the myocardium with oxygen and supplements) prompting narrowing of lumen of the course by diminishing its breadth. Despite the fact that conventional digital subtraction angiography (DSA) is the methodology of decision to assess coronary artery stenosis, in any case, it has a few confinements including a high aptitude required to perform the study alongside inconveniences connected with catheterization.
Conventional catheter angiography likewise gives just restricted data on the nearness and sort of atherosclerotic plaques not connected with luminal stenosis (i.e. framing a positive redesigning); on plaques that are defenseless for break, inevitably prompting thrombosis, impediment, and myocardial localized necrosis [3-5].
Along these lines it is clear that a noninvasive technique for envisioning coronary stenosis and plaques that addresses these issues would be cost useful, extraordinarily help conclusion, and extensively lessens the quantity of simply analytic angiogram and related bleakness [6]. As of late, multi detector computed tomography coronary angiography (MDCTA) has been considered as a promising different option for invasive conventional digital subtraction angiography (DSA) which is a more current, noninvasive strategy.
Starting encounters have likewise demonstrated that coronary injuries can be distinguished with great affectability and specificity [6-10] with multi detector CT coronary angiography (MDCTA). Coronary multi detector contrast enhanced computed tomography angiography (MDCECTA) additionally permits noninvasive identification of calcified, non-calcified and blended atheromatous plaques inside or nearby the mass of coronary veins and in addition surveying the level of stenosis.
Ischemic heart is the essential wellspring of death around the world. For patients with coronary artery disease (CAD), vital analytic apparatuses comprise of digital subtraction angiography (DSA), Coronary computed tomography angiography (CCTA), Coronary magnetic resonance angiography (CMRA), electrocardiography, echocardiography, and nuclear imaging. At present conventional coronary angiography is viewed as the highest quality level for the perception of coronary artery disease (CAD).
Conventional coronary angiography is an obtrusive method with a little, yet inalienable danger of myocardial infraction, stroke, potential arrhythmias and death. Others are non-obtrusive means.
Coronary artery disease (CAD); likewise, atherosclerotic warmth illness is the aftereffect of the aggregation of inside the mass of the coronary corridors that supply the myocardium (the muscle of the heart) with oxygen and supplement. The affidavit of the plaque in the lumen (free space in the artery for the stream of supplements, oxygen and so forth) of a course causes narrowing of lumen of the artery by diminishing its breadth. It is now and then likewise called coronary heart disease (CHD).
CAD is the main source of death around the world. While the side effects and indication of coronary artery disease is noted in the propelled condition of malady, most people with coronary artery disease demonstrates no confirmation of infection for quite a long time as the illness advances before the principal onset of manifestations, frequently a "sudden" heart attack, at long last emerges. Following quite a while of movement, some of these atheromatous plaques may burst and (alongside the initiation of blood thickening framework) begin restricting blood stream to the heart muscle.
The disease is most normal reason for sudden death and is likewise the most widely recognized explanation behind death of men and women more than 20 years old. As indicated by present patterns in United States, half of healthy 40 years old men will create CAD later on, and one in the three healthy 40 years old women.
History
The strategy of angiography itself was initially created in 1927 by the Portuguese doctor Egas Moniz at the College of Lisbon for cerebral angiography, the survey of cerebrum vasculature by X-beam radiation with the guide of a complexity medium presented by catheter.
Coronary catheterization was initially performed in 1929 when the German doctor Werner Forssmann embedded a plastic tube in his cubical vein and guided it to the right chamber of the heart.
The system of coronary angiography was initially performed by Dr. Artisan Sones at the Cleveland Facility in 1958. What's more, still includes the same fundamental reason, utilizing a progression of uncommonly planned catheters to convey X-beam contrast medium to picture the luminal respectability of the coronary epicardia bed. Also, through both blood vessel and venous access, every council of the heart can be hemodynamically surveyed.
Ordinarily, a complete left heart catheterization includes coronary angiography, as well as some measure of the ventricular filling weights and cardiovascular hemodynamics. Regularly, a complete left heart catheterization includes coronary angiography, as well as some measure of the ventricular filling pressure and cardiovascular hemodynamic.
Basics of coronary anatomy
The tri-leaflet aortic valve offers ascend to 3 cusp or sinuses in the aortic root. The left coronary and the right coronary cusp offer ascent to their individual coronary artery while the non- coronary cusp which emerges from the posterior root for the most part does not offer ascent to any coronary artery.
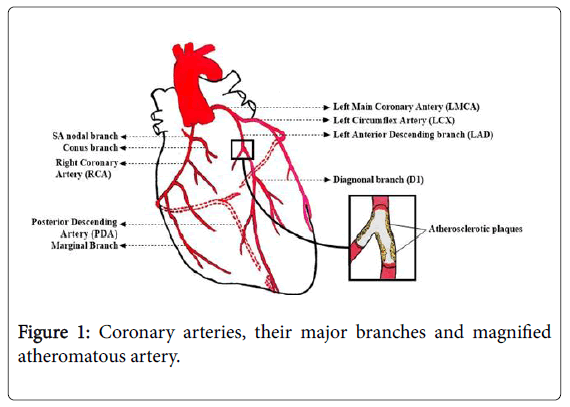
The major epicardia vessels supplying the myocardium are the left main coronary artery that partitions into the Left anterior descending artery and Left circumflex artery and the Right coronary artery. These arteries lie on the epicardia surface and supply small branch vessels that in the end offer ascent to the microvascular system supplying the myocardium (Figure 1).
Coronary artery obstruction
Coronary artery occlusion leads to Ischemic heart disease. Some of the important causes of coronary obstruction are given below.
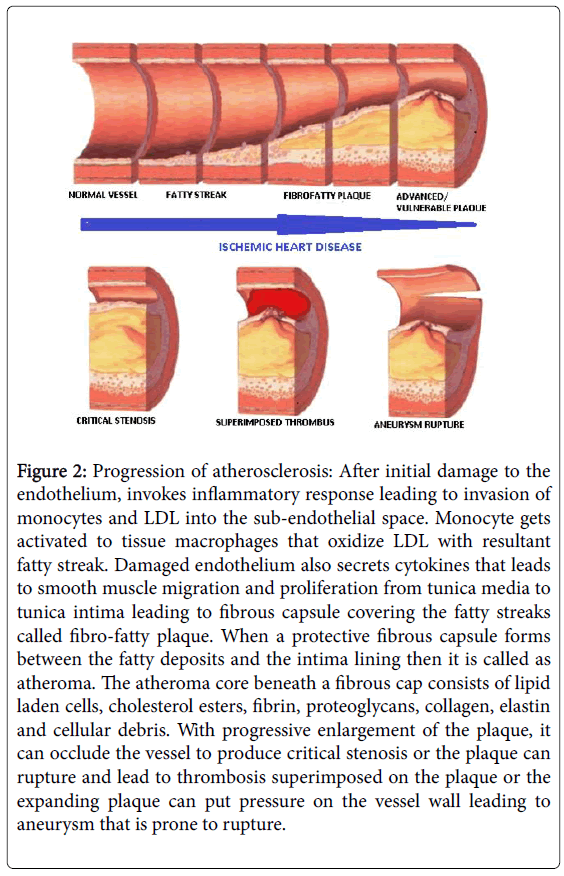
1. Intrinsic cause: Atherosclerotic plaque buildup (Figure 2).
Figure 2: Progression of atherosclerosis: After initial damage to the endothelium, invokes inflammatory response leading to invasion of monocytes and LDL into the sub-endothelial space. Monocyte gets activated to tissue macrophages that oxidize LDL with resultant fatty streak. Damaged endothelium also secrets cytokines that leads to smooth muscle migration and proliferation from tunica media to tunica intima leading to fibrous capsule covering the fatty streaks called fibro-fatty plaque. When a protective fibrous capsule forms between the fatty deposits and the intima lining then it is called as atheroma. The atheroma core beneath a fibrous cap consists of lipid laden cells, cholesterol esters, fibrin, proteoglycans, collagen, elastin and cellular debris. With progressive enlargement of the plaque, it can occlude the vessel to produce critical stenosis or the plaque can rupture and lead to thrombosis superimposed on the plaque or the expanding plaque can put pressure on the vessel wall leading to aneurysm that is prone to rupture.
2. Extrinsic and other causes: congenital abnormalities, spontaneous aortic root dissection, infective endocarditis, embolic events etc.
Coronary dominance
Depends on the vessel that offers ascend to the posterior descending artery (PDA) which goes in the posterior interventricular depression and supplies the atrioventricular node (AV node). This vessel, which can be perceived by the nearness of septal perforating branches, emerges from the RCA in 80% of the population and the LCx in 10% of the population. Co-predominance of the blood vessel flow is found in 10% of the population where the posterior interventricular artery is shaped by both the RCA and LCx.
The Right coronary artery (RCA)
Arises from the right coronary cusp. This vessel follows the right AV groove and provides branches to the right ventricle. The most proximal branches of the RCA are the conus branch which supplies the right ventricular outpouring tract and a branch that supplies the sinoatrial node (SA node) (60% of patients). The RCA then courses through the interventricular and offers ascend to marginal branches and branches to the atrium. Control of the coronary artery in 3 dimensions by means of exceptional recreations of the coronary artery are useful in translating coronary angiographic images.
The Left main coronary artery or Left main trunk (LMT)
Begins from the left coronary cusp and bifurcates to offer ascent to Left anterior descending (LAD) and Left Circumflex (LCx) coronary arteries. Every so often, a third branch vessel, the Ramus Intermedius (RI) emerges from the LMT. The LMT differs long in numerous patients and in a small number of patients, the two noteworthy branch vessels emerge from particular separate origins.
The Left anterior descending coronary artery (LAD)
Gives blood supply to anterior wall of the left ventricle. As it courses through the anterior intraventricular groove it gives different septal branches to the interventricular septum and diagonal branches to the anterior lateral wall. The LAD then courses to the ventricular summit and in a few patients wraps around the zenith to supply a little measure of the posterior apex.
The Left Circumflex coronary artery (LCx)
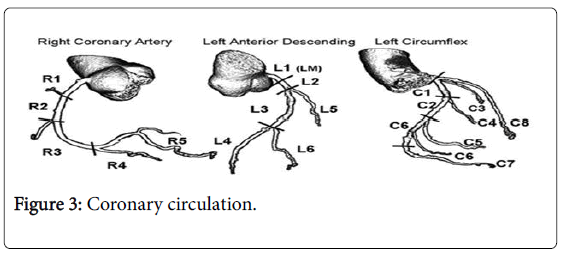
Courses around the lateral or left atrioventricular groove and offers ascend to numerous marginal or lateral branches. The branches are termed obtuse marginal (OM) or lateral branches relying upon institutional inclination. OM branches are successively numbered (OMI, OM2 etc.) while Lateral branches are termed based on the segment of the lateral wall they supply (High Lateral, Lateral, Posterior Lateral). As the LCx courses the AV groove it also gives rise to several atrial branches, and occasionally the sinoatrial branch (40% of the population) (Figure 3).
Anomalies of RCA origin
The RCA can have an atypical root. It is vital to know about this plausibility to abstain from confusing coronary CTA. Ordinarily, the anomalous starting point of the RCA is from the left coronary sinus of Valsalva, with a consequent course between the aortic root and right ventricular outpouring tract. Portrayal of these irregularities is past the extent of this article; be that as it may, this and different inconsistencies of RCA root are depicted by Kim et al. [11]
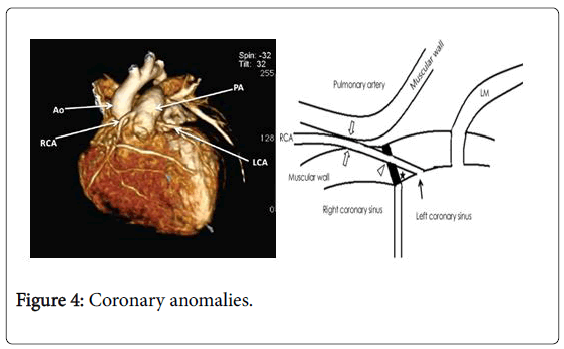
Anomalies of LCA origin
The LCA and its branches can have an irregular origin. It is imperative to know about this plausibility to abstain from misjudging coronary CTA. Some of these unconventionalities are connected with a developed danger of sudden death or heart failure. Portrayal of these abnormalities was past the extent of this article; in any case, peculiarities of LM, Fellow, and LCx root are audited by Kim et al. [11] (Figure 4).
DSA (Digital subtraction angiography)
It's an insignificantly invasive fluoroscopy system (that utilizations X-beams to acquire constant moving images of the inward structures of a patient using a fluoroscope) to plainly imagine within or lumen of veins and organs of the body, with specific enthusiasm for the arteries, veins and the heart chambers in a hard or thick soft tissue environment. It is performed for both indicative and interventional (treatment) purposes.
The image acquired would likewise incorporate all overlying structure other than the veins around there. This is helpful for deciding anatomical position and varieties however unhelpful for imagining veins precisely.
Keeping in mind the end goal to evacuate these diverting structures to see the vessels better, initial a veil image is obtained. The veil image is just an image of the same zone before the contrast is administrated.
Images are delivered utilizing contrast medium by subtracting a 'pre-contrast image' or the veil from later difference presented images. Accordingly, last created show up with an extremely pale dim foundation, which delivers a high complexity to the vessels, which show up a very dark grey. Subsequently, the term 'digital subtraction angiography'
• Blood vessel and venous impediments, including carotid artery stenosis, respiratory embolisms and intense appendage ischemia.
• Arterial stenosis, which is especially helpful for potential renal contributor in recognizing renal course stenosis. DSA is the highest quality level examination for renal artery stenosis [1].
• Cerebral aneurysms and arteriovenous malformations (AVM).
For all structures with the exception of the heart, the images are typically taken utilizing a system called digital subtraction angiography or DSA. Images for this situation are generally taken at 2-3 outlines for every second, which permits the interventional radiologist to assess the stream of the blood through a vessel or vessels. This procedure "subtracts" the bones and different organs so just the vessels loaded with contrast agent can be seen. The heart images are taken at 15-30 outlines for every second, not utilizing a subtraction strategy. Since DSA requires the patient to stay still, it can't be utilized on the heart. Both these procedures engage the interventional radiologist or cardiologist to see stenosis (blockages or narrowing) inside the vessel which might be hindering the stream of blood and causing pain.
Role of DSA in determining coronary artery disease
DSA is being utilized less and less routinely as a part of imaging department. It is being assumed control by computed tomography angiography (CTA), Heart CT and X-ray, which can deliver 3D images through a test which is less invasive and distressing for the patient however as indicated by the Australian and New Zealand Relationship of Neurologists, DSA is still the best quality level for blood arterial imaging [12].
Coronary computed tomography angiogram (CCTA)
Coronary computed tomography angiogram (CCTA) has as of late risen as a powerful noninvasive strategy to image the coronary arteries. CTA is likewise called multi slice computed tomography (MSCT), cardiovascular CT or heart CTA. It is imaging of heart that figures out whether plaque development has limited a patient's coronary arteries.
Plaque is made of different substances coursing in the blood, for example, fat, cholesterol and calcium which stores along the internal coating of the arteries. It can diminish the blood stream, or now and again, square it totally. This development happens more than quite a while.
Coronary CTA is like a CT scan, yet the differentiation color is infused into one of the veins in a matter of seconds before the X-beam image is performed. Since the dye is infused into a vein instead of into an artery, it is a noninvasive strategy for distinguishing blockages in the coronary arteries.
Progresses in multi detector CT (MDCT) innovation with sub millimeter slice collimation and high temporal determination grant contrast improved imaging of coronary artery and coronary plaque amid a solitary breath hold. Suitable patient planning, point by point specialized and innovative information with respect to acknowledgment of run of the typical imaging artifacts, (for example, beam solidifying or movement artifacts), and the satisfactory decision of post handling systems to recognize stenosis and plaque are requirements to accomplishing symptomatic image quality. A developing number of studies have proposed that 64 slice coronary CT angiography is exceptionally exact for the avoidance of huge coronary artery stenosis (50% luminal narrowing), with negative predictive estimations of 97-100%, in examination with invasive selective coronary angiography. What's more, a few studies have shown that MDC likewise can identify calcified and no calcified coronary atherosclerotic plaques, particularly in proximal vessel portions, demonstrating a decent relationship with intracoronary ultrasound. Studies on clinical utility, cost, and cost-adequacy are presently justified to show whether and how this system can change and enhance the flow administration of patients with suspected coronary artery disease.
CT angiography analyses a narrowing or impediment of the arteries, an aneurysm, profound vein thrombosis, pneumonic embolism, or another vascular. Coronary CTA can be performed much quicker (in under one minute) than a heart catheterization, with possibly less hazard and uneasiness and diminished recuperation time.
Indications
A scientific statement form the American Heart Association (AHA) [13] indicates that the potential benefit of noninvasive coronary angiography is likely to be the best for symptomatic patients who are at impending danger for coronary artery disease (CAD) after beginning danger stratification incorporating patients with dubious anxiety.
CCTA is suggested over coronary magnetic resonance angiography (MRA) due to unrivaled demonstrative exactness. Coronary CTA or MRA is not prescribed to screen for CAD in patients who have no sign or side effects of suggestive of CAD.
Propriety criteria were distributed in 2006 from 8 claims to fame social orders, including the American School of Cardiology and American School of Radiology. The taking after signs was evaluated as suitable for coronary CT angiography.
• Evaluation of chest pain syndrome in patients with intermediate pretest probability of CAD and uninterpretable electrocardiogram (ECG) or inability to exercise
• Evaluation of chest pain syndrome in patients with uninterpretable or equivocal stress test (exercise, perfusion. or echocardiogram)
• Evaluation of acute chest pain in patients with intermediate pretest probability of CAD and no ECG changes and serial enzymes negative.
• Evaluation of coronary arteries in patients with new-onset heart failure to assess etiology.
• Evaluation of suspected coronary anomalies
Note that coronary MRA is additionally precise in assessing coronary peculiarities, and the AHA experimental articulation demonstrates that MRA is favored when it is accessible in light of radiation insurance concerns.
Little information exits with regards to the cost-adequacy of CCTA. A wellbeing innovation [14] appraisal recommended that CCTA might be a financially savvy distinct option for myocardial perfusion scintigraphy. For whatever length of time that the commonness of CAD is not very high, CCTA was thought to be a possibly practical technique for maintaining a strategic distance from Conventional coronary angiography.
Role of MRI in visualizing coronary arteries
Coronary magnetic resonance angiography (cMRA) has developed over the previous decade as a conceivable noninvasive option for imaging coronary arteries [15].
It is likewise helpful in the assessment of coronary artery stenosis, Coronary MR angiographic methods can be subdivided in breath-hold (single or repeated breath-hold) and non-breath-hold strategies. The greater part of the clinical experience so far has been with a single breath-hold method, and was restricted to agreeable patients. The late presentation of guide heartbeats for ongoing respiratory gating or activating permits non-breath hold or repeated breath-hold 3D coronary MR angiography. In any case, it has not yet achieved a stage where it can be utilized as a part of routine clinical practice, although coronary MRA is a possibly helpful indicative apparatus. It has its constraints a few key specialized issues stay uncertain and are currently being tended to by the investigative and clinical group.
Coronary MRA is especially appealing in light of the fact that it doesn't open the patient to ionizing radiation, nor does it require the utilization of radiopaque, osmotically dynamic contrast media with potential nephrotoxicity. Since, it was initially reported by Paulin et al. [16].
Coronary MRA has increased impressive significance as a technique that could be utilized to analyze coronary artery stenosis. Besides, coronary MRA can be gotten in any bearing and plane, with no limitation to the angulation of the images. At last, coronary MRA can without much of a stretch be joined with an exhaustive assessment of the anatomical structures and function of the left ventricle and evaluation of myocardial practicality, in this way covering every one of the prerequisites of a thorough heart examination.
The potential advantage of coronary MRA is the representation of coronary arteries, as well as the perception of the heart morphology, procured ailments of the considerable vessels, and cardiovascular capacity very still and under anxiety [17-19]. Other advantages of MRA incorporate assessment of the patency of aortocoronary bypass graft, abnormal coronary arteries [20] and conceivable steadiness of plaques without noteworthy presentation of ionizing radiation [21,22]. Be that as it may, further studies are expected to validate these discoveries.
Acquiring diagnostic-quality images of the coronary arteries is verifiably a specialized test. Visualizing the small vessels and their pathology requires greatly high spatial determination. Image quality may likewise be traded off by movement artifacts from the heart and chest. The most recent era of multi slice CT scanners seems fit for defeating these issues, inciting a recharged concentrate on coronary CT angiography. Indeed, even enthusiasts of MRA admit that their favored radiation innovation can't contend in this domain.
Current coronary MRI techniques and technical limitations
Steady state with free-precession coronary MRA: Utilization of steady state with free-precession (SSFP) technique to perform MRA makes it Conceivable to get high signal intensity from the coronary artery and high contrast between the ventricular blood pool and the myocardium without the requirement for contrast agent [23] SSFP imaging allows top notch coronary MRA amid freebreathing with substantial enhancements in SNR, contrast to-noise proportion, and vessel sharpness as contrasted and standard T2 arranged gradient echo imaging [24]. In this manner, SSFP imaging may prompt enhanced distinguishing proof of noteworthy coronary artery stenosis. At present, SSFP is being assessed at numerous clinical and examination focuses.
Phase-contrast MR Imaging
The stage contrast method measures blood-stream [25] speed joined with blood vessel width to yield a quantitative estimation of blood stream (in milliliters every moment). Blood stream can be resolved when a patient is very still or after he or she is focused for estimation of coronary artery blood-stream reserved [25,26]. Despite the fact that it has been shown in clinical examination, this strategy can be connected on most 1.5 Tesla and exactly 3.0 Tesla MR scanners. Coronary blood flow is measured along a 2 cm straight proximal or mid arterial portion in vessels that are >2 mm in diameter [27].
Parallel Imaging for coronary MRA
Parallel imaging is a MR technique for decreasing MR examining time by a variable of 2 to 3 [28]. In any case, the exchange off for lessened securing time is diminished SNR for perception of the coronary artery.
3-Tesla coronary MRA
Most coronary MRA examinations are performed on 1.5 Tesla MR Frameworks. Higher field, 3.0 Tesla frameworks give better signal and differentiation values with respect to 1.5 Tesla frameworks. The late accessibility of 3.0 Tesla frameworks outfitted with devoted cardiovascular equipment (e.g. constant spectrometer, parallel recipient innovation with high data transmission, body radio recurrence send loop, vector ECG) and programming (parallel imaging, navigators, intelligent interface) may give a way to substantial coronary MRA upgrades later on [29].
Whole heart Coronary MRA
Up to this point, coronary MRA was performed with just divides of each blood vessel tree unmistakable in every arrangement of images [30]. This strategy requires the MR imaging technologist to have broad experience and nature with coronary artery anatomy structures. The late advancement of entire heart coronary MRA, which is comparable to coronary CTA, consider imaging of the whole coronary artery tree in an axially obtained 3D volume. Post preparing of the 3D images is performed in a way like that for coronary CTA to gather such huge volumetric information sets, spatial resolution is fairly lower (typically >1 mm in-plane and through-plane resolution), information is gathered over roughly 100 ms of each heart cycle (with potential for obscuring), and scan times are extensive (10 to 15 minutes), in this manner ordering the utilization of navigator echoes. By and by, the entire heart coronary MRA approach has increased quick acknowledgment on the premise of promising beginning results [31,32].
A substantial assortment of specialized methodologies has been portrayed for coronary MRA, which incorporate for all intents and purposes any imaging arrangement. Regardless of late advance, there is still not a uniform concession to the ideal securing plan for imaging of the coronary arteries. All in all, the three-dimensional methodologies appear to have increased more extensive acknowledgment, and the greater part of the present day frameworks can accomplish high spatial resolution (in plane resolution <1 mm). These incorporate the whole left main, the proximal 5-6 cm of the left anterior descending and the right coronary, and 2-3 cm of the left circumflex coronary artery.
Among the epicardial vessels, the left circumflex coronary artery is the hardest to picture, fundamentally as a result of the separation of the vessels from the surface loops that are utilized for information gathering. The assessment of local coronary artery integrity keeps on being the long looked for use of coronary MRA. With the utilization of bright blood (gradient-echo) approaches the quick moving coronary blood gives high signal (bright), while moderate or turbulent stream displays a sign void (dark).
In regions with central stenosis there is signal misfortune and the greatness of sign misfortune relates with the level of angiographic stenosis. In any case, with the bright blood angiographic approaches, false positive and false negative translations might be given. On the off chance that, for instance, there is moderate stream distally to a critical stenosis, this may present as complete sign loss, despite the fact that the vessel is patent.
Also, as these procedures are not touchy to the bearing of blood stream, an aggregate impediment with satisfactory security course may present as sufficient signal, even in the vessel lumen distal to the stenosis. As of late, the majority of the heart MR focuses utilize threedimensional coronary MRA systems, as these methodologies give naturally higher signal (increased signal to noise ratio) and permit recreation in any orientation.
Methods and Materials
Patients selection
Aggregate of 57 patients (37 male, 20 female; age range 44-86 years, mean age 65.5 years) were enlisted from January 2009 to August 2012 with suspected or proven coronary artery disease (CAD), Who underwent both conventional coronary angiography (CCA) and multi detector computed coronary angiography (MDCT) within four months interim. We considered routine conventional coronary angiography (CCA) as a highest quality level strategy and assessed all the portions in 57 patients. Absolute 969 segments in 57 patients were concentrated on, of which 20 segments with stent, 6 with movement artifact and 12 blocked off portions were barred. Of staying 931 segments, 95 segments indicated fluctuated level of stenosis, with 34 segments being <50% stenosed, 43 segments being 50-70% stenosed and 18 segments being >70% stenosed. Patients prohibition criteria were: >4 months interim of both the technique, tolerant experienced stand out of the methodology, unpredictable heart rate, known unfavorably susceptible response to iodinated complexity material; and segments rejection criteria were: segments with stent, movement artifact and segments those were distant.
CT protocol
Data were acquired using a 64 slice Multi detector computed tomography (MDCT) scanner.
Firstly, an electrocardiographic (ECG) gated scan without complexity media was performed to decide the aggregate calcium weight of the coronary tree (4 x 2.5 mm collimation, table feed 1.5 mm/revolution, viable tube current 133 mAs at 120 kV, powerful slice with 3.0 mm, recreation increase 1.5 mm).
Secondly, to decide the course time for the non-ionic differentiation upgraded filter, 20 ml of contrast media (20 ml at 4 ml/s, 370 mg iodine/ml, lopromide 370; Ultravist, and a bolus of 20 ml saline were managed in an antecubital vein and the bolus following programming used to discover right examining delay. The locale of interest was put inside the ascending aorta, and the scan began as the CT thickness was 100 Hounsfield units, higher than that of the pattern.
Thirdly, by utilizing a dual head power injector, an aggregate 150 ml intravenous differentiation operator in addition to a 20 ml bolus was infused (50 ml at 4.0 ml/s, then 100 ml at 2.5 ml/s).
Fourthly, a differentiation upgraded reflectively ECG gated scan (4 x 1.0 mm collimation, table feed 1.5 mm/revolution, compelling tube current 400 mAs at 120 kV) was obtained. CT volume dataset for the coronary artery is obtained; this dataset covers the whole heart from the proximal ascending aorta (roughly 1-2 cm underneath the carina) to the diaphragmatic surface of the heart. The begin of the reproduction window was set at 60% for all local images and was variable for the difference improved arrangement (40-70%). Betablocker was controlled to adjust heart rate compelling slice thickness was 1.25 mm; the recreation addition was 0.8 mm.
The calcium score was resolved in view of Agatston Score system, accepting edge estimation of 130 HU. Assessment of coronary stenosis by multi detector computed coronary angiography (MDCTA) was performed using axial, multi-planar reconstruction (MPR), curved multi-planar reconstruction (cMPR), maximum intensity projection (MIP) and three-dimensional volume rendering techniques (VRT) in most of the studies.
Study design and image analysis
Coronary arteries were isolated into 17 segment as indicated by the adjusted American Heart Association classification [33]. These segments were as per the following: The right coronary artery included segment 1, proximal segment; segment 2, middle segment; segment 3, distal segment; segment 4a, posterior descending coronary artery; and segment 4b, posterolateral artery. The left main coronary artery segment 5. The left anterior descending coronary artery included segment 6, proximal segment; segment 7, middle segment; segment 8, distal segment; segment 9, first diagonal segment and segment 10, second diagonal segment. The circumflex branch of the left coronary artery included segment 11, proximal segment; segment 12, first marginal segment; segment 13, middle segment; segment 14, second marginal segment; segment 15, distal segment; and segment 16, intermediate branch. segments l, 5, 6 and 11 were defined as proximal segments; segments 2, 7, and 13 were defined as middle segments; and segments 3, 4a, 4b, 8-10, 12, 14-16 were defined as distal segments or side branches.
Level of stenosis was assigned as gentle stenosis <50%, moderate stenosis 50-70% and severe stenosis >70% individually; while sorts of plaques were assigned as calcified plaques, non-calcified plaques and mixed plaques. Coronary calcium was recognized as a thick region in the coronary artery surpassing the edge of 130 HU. The worldwide Agatston score and in addition per coronary artery per section was recorded for every patient. An examination of the lumen at the area of narrowing with proximal and distal references empowers a quantitative appraisal of the level of luminal narrowing.
Statistical analysis
Microsoft-excel 2010 and SPSS 18 for Windows were used for data collection and analysis. The degree of stenosis (mild stenosis <50%, moderate stenosis 50-70% and severe stenosis >70%) between conventional coronary angiography and 64 slice MDCT angiography was compared using the independent two sample Student's t tests. A value of p= 0.05 was used for significant test. The sensitivity, specificity, positive predictive value, negative predictive value, and accuracy of multi-detector computed coronary angiography was calculated.
Patient participation
The patient being analyzed or treated is typically alert amid catheterization, in a perfect world with just nearby anesthesia, for example, lidocaine and irrelevant general sedation, all through the procedure. Performing the methodology with the patient conscious is more secure as the patient can quickly report any distress or issues and subsequently encourage fast amendment of any undesirable events. Therapeutic screens neglect to give an extensive perspective of the patient.
Patient preparation
Patients are encouraged to stay away from nourishments and fluids for least of 4 hours before the test, yet are permitted to keep bringing any recommended pharmaceuticals with the affirmation from the doctor before exam no doubt.
Prior to the test is performed, patients are re-quested to change into a doctor's facility outfit and evacuate all adornments and other metal articles, which can meddle with x beams. Beta-blocker organization is frequently useful in cardiovascular CT to the heart rate and decline movement relic. The level to which the heart rate brought down relies on upon the transient determination of the scan.
Possible contraindications of Beta blocker administration include the flowing [34,35]:
• Heart rate <60 bpm
• Systolic blood pressure <100 mm Hg
• Asthma or chronic obstructive pulmonary disease (COPD) on beta 2 agonist inhaler
• Active bronchospasm
• Second- or third-degree atrioventricular block
• Sick sinus syndrome
• Decompensated cardiac failure
• Pheochromocytoma (can be given in combination with an alpha blocker if the alpha blocker has been initiated beforehand)
Diagnostic procedure
Techniques: An expansive number of techniques can be performed on the heart by catheterization. This most regularly includes the insertion of a sheath into the femoral artery (but, in practice, any large peripheral artery or vein) and cannulating the heart under X-beam representation (most normally fluoroscopy). The first catheterization system was performed by means of brachial access.
The radial artery route may likewise be utilized as cannulation, this methodology offers a few focal points, including the availability of the artery in many patients, the simple control of draining even in anticoagulated patients, the upgrade of solace since patients are equipped for sitting up and strolling instantly taking after the strategy.
Anatomic milestones are utilized to distinguish the right site of blood vessel puncture. For the femoral artery route get to, the femoral head gives the best obvious historic landmark. Blood vessel puncture at this site stays beneath the inguinal ligament.
After the organization of subcutaneous analgesic, a 18G Cook needle is utilized to puncture the front wall of the artery. This strategy is known as the modified Seldinger system and avoids posterior blood vessel draining or venous correspondence from the puncture. Complications from arterial access include arterial dissection, AV fistula formation, retroperitoneal hemorrhage, and pseudo aneurysm formation.
When access is gotten, the Cook needle is steadied while the artery is gotten to with a wire through the lumen of the Cook needle. The Cook needle is then evacuated and a sheath is embedded into the course. Under fluoroscopy, catheters are then presented utilizing a 0.35 J tipped aide wire into the aortic root. The catheters are then joined to a 3 complex. Complex utilized takes into account persistent weight observing, saline flush instillation, and difference organization through the catheter tip.
After the artery is locked in it is essential to look at the pressure wave shape. Normally the waveform ought to imitate aortic root pressure. Destructuralization of the pressure waveform may demonstrate over engagement of the catheter or huge vessel stenosis. Great consideration ought to be taken before instillation of contrast medium without normal pressure waveforms.
The catheter is itself intended to be radio thick for deceivability and it permits a reasonable, watery, blood perfect radiocontrast agents, regularly called a X-beam dye, to be particular infused and mixed with the blood streaming inside the artery. Ordinarily 3-8 cc of the radiocontrast specialists is infused for every image to make the blood stream noticeable for about 3-5 seconds as the radiocontrast agents is quickly washed away into the coronary vessels and after that coronary veins. Without the X-beam dye infusion, the blood and encompassing heart tissues show up, on X-beam, as just a gently shape changing, generally uniform water thickness mass; no points of interest of the blood and interior organ structure is recognizable. The radiocontrast inside the blood stream permits representation of the inside the courses or heart chambers, contingent upon where it is infused.
In the event that atheroma or clumps are distending into the lumen creating narrowing, the narrowing might be seen rather expanded cloudiness inside the X-beam shadow images of blood color section inside that divide of the artery; this is contrasted with contiguous, assumed more beneficial, less stenotic zones.
Catheters
Catheter choice for a normal left heart catheterization is for the most part straight forward. By configuration, the catheter is smaller than the lumen of the artery it is put in.
Frequently, Judkins catheter sorts are most routinely utilized. For engagement of the left primary coronary artery course, A Judkins Left size 4 (JL4) catheters by and large will connect with the left coronary artery in many patients. Expanding catheter size (JL5) for tall patients or patients with widened aorta or diminishing size (JL 3.5) in small patients is at times required.
Obligation of the Left main coronary artery or Left Main Trunk (LMT) is normally mostly clear in the Left anterior oblique (LAO) projection. For to a great degree enlarged roots or peculiar arteries different catheters, for example, Amplatz catheters can be utilized. For the right coronary artery course, a Judkins Right Size 4 (JR4) is regularly utilized. The right coronary supply route is occupied with the LAO projection. Generally moderate clockwise turn of the JR4 in the aortic root will connect with the ostium of the Right Coronary artery (RCA).
Specific catheters are accessible to connect with anomalous origins of coronary arteries and saphenous and internal mammary artery bypass grafts.
Standard angiographic views
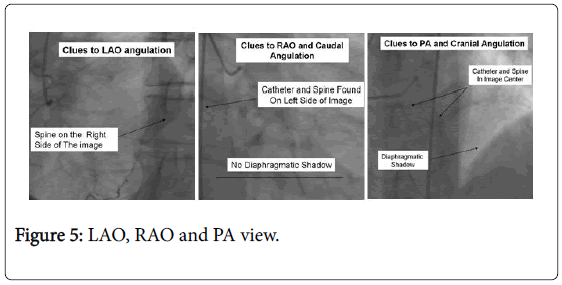
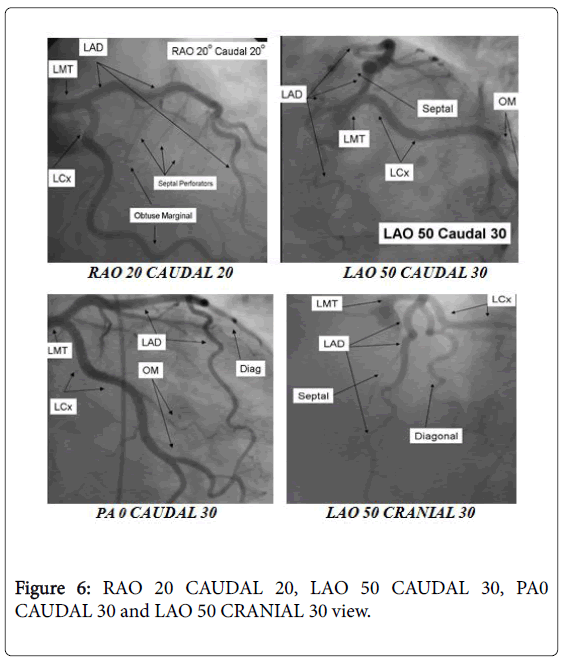
For the beginner angiographer, the anatomic landmark of interest framed by the spine, catheter and stomach give data to observe which tomographic view from which the image is obtained. In the LAO point of view the catheter and spine are seen on the right half of the image, while in the RAO, they are found on the left side. PA imaging puts these milestones in the center point of the image. Cranial angulation can normally be recognized from caudal angulation by the nearness of the diaphragm. For cranial imaging, the patient ought to be requested that move to expel the diaphragmatic shadow from the image (Figures 5 and 6).
Left coronary artery
The Left main coronary artery offers ascend to the left anterior descending artery and the left circumflex coronary artery. Complete representation of these arteries and their branches requires consideration and thoroughness to guarantee complete anatomical documentation. Frequently bifurcations and vessel foreshortening and cover cause mistakes in stenosis estimation.
There are no ardent principles in which tomographic perspectives are generally valuable. By and large, for circumflex and proximal epicardia perception the caudal perspectives are generally helpful. For LAD and diagonal bifurcation representation the cranial perspectives are generally helpful. By and large, if there is not a critical confinement on differentiation usage, standard left coronary anatomy.
Right coronary artery
• The Right coronary artery is engaged in the LAO position.
• Initial angiographic imaging of the RCA in this view (LAO 30) gives the best view of significant ostial and proximal RCA disease.
• The mid RCA is best visualized in the straight RAO 30 position.
• The bifurcation of the distal RCA and Right Posterior Descending Artery (rPDA) is best seen in the PA 0 Cranial 30 view with a small breath in.
Image acquisition and Image reconstruction
Image acquisition: Coronary Computed Tomography Angiography (CCTA) is an exceptional kind of X-ray beam examination. As the examination convention patients experiencing a coronary CT A scan get an ascertained measure of an iodine-containing contrast material (dye) as an intravenous (IV) infusion utilizing a programmed injector machine which controls the planning and rate of infusion. The contrast material may make feel flushed and warm, and it now and again can create a somewhat wiped out to your stomach sensation.
As the dye courses through the circulatory system, it will highlight the veins on the output to guarantee the most ideal image of the heart veins. The X-ray beam going through the body are gotten by finders in the scanner and later with the assistance of 3D reproduction postpreparing method 3D images are delivered on a PC screen.
Tolerant must stay still as the CT examining machine works. The administrator may approach to hold breath for 10 to 25 seconds at time; it is on account of even the movement of breathing can obscure the images.
The whole system for the most part takes 20 minutes to 1 hour to finish. These images empower to figure out if plaque or calcium stores are available in the course dividers arterial wall.
Image reconstruction
Underlying principles of interpreting CCTA studies Threedimensional data sets and workstations: Coronary computed tomography images ought to be procured as isotropic sub millimeter 3 dimensional electrocardiogram (EKG) gated information sets, which encourage reconstruction and showcase in an assortment of image formats [36,37]. In view of the multifaceted nature of coronary anatomy, the recurrence of movement and calcium related images artifacts, and the morphologic nuances of sores, mediators must audit CCTA intuitively on Workstations fit for 2 and 3 dimensional presentations in all conventional reconstruction formats.
These incorporate trans hub 2 dimensional image stacks ("raw information"), multi planar reformations (MPRs), maximum intensity projections (MIP's), curved multi planar reformations (cMPRs), and volume rendering technique (VRT) reproductions. Much of the time with heart rate related artifacts, analytic quality might be enhanced by extra image recreations at exchange times in the cardiovascular cycle with decreased cardiovascular movement [38-40]. On account of the potential requirement for extra reproductions, raw information records must be held until image translation is finished.
Both hub images and multi planar reformatted (MPR) pictures, which allow the perception of the coronary courses in different introductions orthogonal and opposite to the long hub of the vessel, are instrumental in identifying the nearness of noteworthy coronary artery stenosis. Be that as it may, unique pivotal images remain the foundation of the assessment, as basically all pathologies can be perceived.
Interpretation formats
Trans axial images ("raw data")
Trans axial images are the fundamental imaging consequence of the filtering and reproduction process and comprise of a progression of 2 dimensional images stacked in the longitudinal (cranial-caudal or zaxis) which they were gained. These are inspected specifically by looking through the image slice yet just from the straight caudalcranial point of view.
A noteworthy favorable position of this arrangement is that the image data content shows the base probability of mutilation or blunders ensuing to post handling and the most extreme determination and dim scale rendering [41,42], an inconvenience of this configuration is that it requires the pursuer to rationally recreate the 3 dimensional anatomic connections of the courses and different structures in the thorax, since the information are shown in 2 dimensional and from one perspective.
Multi-planar reformation (MPR)
MPR is an optional high resolution reconstruction arrange that permits presentation of planar images at any precise area through the securing volume, which licenses representation in the pivotal plane as well as in orthogonal (coronal and sagittal) or diagonal planes that better take after the blood vessel course in the thorax. Also, selfassertive planes crossing the volume at positive points, for example, right anterior oblique with cranial angulation, can replicate well known invasive angiographic views.
Most workstations will permit mediators to at the same time look through perspectives of three orthogonal oblique MPRs. Also, it is anything but difficult to turn the vessel on its longitudinal axis through 360 degrees, or page through transverse MPRs through the vessel.
These moves are helpful in outlining the morphology of plaque and its impact on the lumen [42,43]. When all is said in done, the smallest accessible slice width is utilized as a part of MPRs to enhance image quality, unless signal to noise requires an expansion in slice width to safeguard interpretability.
Curved multi-planar reformation (cMPR)
This configuration was produced to permit the mediator to take after the course of a convoluted vessel for more separations as it alters course [43,44]. This requires the centerline of the vessel be followed effectively, which should be possible physically or consequently. While cMPR has the upside of creating a perspective of the whole course of the vessel in one image, it has a potential genuine drawback in that wrong centerline following may bring about artefactual lesions. At the point when utilizing cMPR, the mediator ought to audit the centerline for accuracy.
Maximum intensity projection (MIP)
MIP is like MPR in that orthogonal or angled planes can be surveyed. Intelligently [44,45], they contrast in that, for the most part, MIP is made in thicker areas, consolidated a volume that incorporates the whole vessel lumen and divider diameter (commonly 5 mm as an underlying thickness for coronary elucidation), and that every pixel is spoken to by the greatest pixel esteem inside the section volume [46].
These elements permit the peruse to image a more extended fragment of a vessel's course and have a tendency to diminish saw image commotion. In any case, there is loss of injury data inside the slab volume, as the MIP does not give top to bottom data or constriction point of interest inside the slice [47]. Hence, MIP ought not be the sole procedure utilized for understanding.
Since current workstations permit exchanging forward and backward between organizations without a position change, flipping amongst MIP and MPR catches the upsides of both when perusing a specific vessel segments.
Volume-rendering technique (VRT)
Another procedure in common use is VRT, which makes volumetric 3 dimensional representations with the figment of spatial uprightness and shading. It is for the most part not valuable for the evaluation of coronary stenosis since the obvious thickness of the vessel lumen is subject to window settings and the PC calculation that is utilized to subtract non-vascular structures [44].
VRTs are helpful for imaging spatial connections, for example, characterizing the course of coronary inconsistencies and course of coronary bypass graft.
This system discovers a great deal more use in the investigation of thoracic cardiovascular anatomical structures, in CHD, and for showing purposes and outlines for patients.
Results
Our study enlisted 57 patients with suspected or demonstrated coronary artery disease (CAD) from January 2009 to August 2012; who experienced both conventional coronary angiography (CCA) and multi detector computed coronary angiography (MDCT).
Aggregate of 969 segments were considered, of which, 931 (96%) were open sections and remaining 38 (4%) distant portions (20 segments with stent, 6 with movement artifact and 12 segments <2 mm) were avoided from our studies.
Out of 931 available segments, 95 (10%) portions demonstrated shifted level of stenosis. Out of aggregate 95 stenosed sections, 34 (36%) segments were <50% stenosis, 43 (45%) segments were 50-70% stenosis and 18(19%) were segments >70% stenosis.
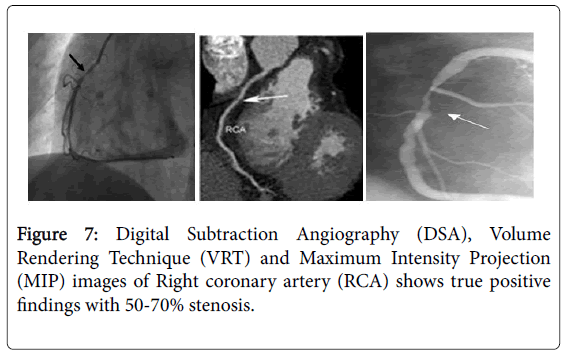
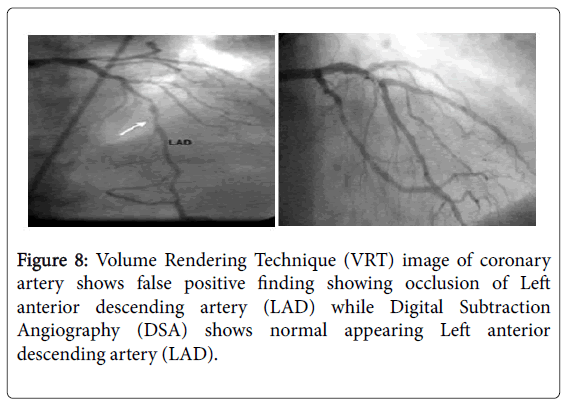
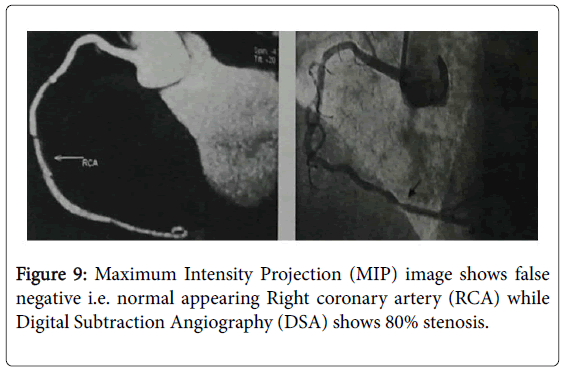
The aggregate number of true positive (TP, Figure 7), false positive (FP, Figure 8), false negative (FN, Figure 9) and true negative (TN) stenotic lesions(mild stenosis <50%, moderate stenosis 50-70% and severe stenosis >70%); alongside ascertained affectability, specificity, positive predictive value (PPV), negative predictive value (NPV) and general exact nesses utilizing computed tomography coronary angiography (CTA) in assessing stenosis, assuming conventional coronary angiography (CCA) as a best quality level technique is appeared in Table 1.
| Characteristic | <50% stenosis | 50-70% stenosis | >70% stenosis |
|---|---|---|---|
| True Positive | 22 | 30 | 36 |
| False Positive | 6 | 6 | 2 |
| False Negative | 6 | 7 | 2 |
| True Negative | 909 | 901 | 917 |
| Sensitivity (%) | 78.57 | 81.08 | 87.5 |
| Specificity (%) | 99.33 | 99.34 | 99.78 |
| Positive productive value | 78.57 | 83.33 | 87.5 |
| Negative productive value | 99.34 | 99.22 | 99.78 |
| Overall accuracy (%) | 88.95 | 90.2 | 93.64 |
Table 1: CTA assessment of coronary stenosis <50% stenosis, 50-70% stenosis and >70% stenosis.
Out of aggregate 95 stenosed segments, 24 (25%) stenosed segments were found in the proximal portions, 51 (54%) in the middle segments and 20 (21%) in the distal segments. So also, 33(35%) stenosed segments were found in right coronary artery and its marginal branch (segments 1-4), 2 (2%) stenosed segments were found in left main artery (segment 5), 44 (46%) stenosed segments were found in left anterior descending and its diagonal branches (segments 6-10) and 16 (17%) stenosed segments were found in left circumflex artery and its obtuse marginal branches (segments 11-16).
Underlying principles of CCTA interpretation
• Understanding ought to be made on 3-dimensional workstations prepared to show suggested image reconstruction formats.
• Image ought to be investigated in the proper post processing.
• Translators ought to be set up to alter picture reproductions if essential.
• The information set ought to look for artifacts.
• Non contrast studies ought to be preceding difference concentrates on.
• The coronary tree ought to be analyzed methodically.
• Lesions ought to be looked into in different planes and conceptualized in 3 dimensions.
• Lesions ought to be evaluated for degree and nature of plaque, not only for stenosis seriousness.
• Additional coronary heart and thoracic anatomical structures ought to be inspected inside cardiovascular field of view.
Recommended image post-processing formats
Post-processing formats: Recommended
Axial image review: Recommended
Multi planar reformation (MFR) image review: Recommended
Maximum intensity projection (MIP) image review: Recommended
Curved multi planar reformation (cMPR) image review: Optional
Volume-rendered reconstructions: Optional
Discussion
Conventional coronary angiography (CCA) gives a great perception of the coronary vasculature and has been considered as the reference standard for assessment of coronary stenosis and impediment with the benefit of high spatial determination and temporal determination. Be that as it may, it is an invasive and costly system with related morbidity and mortality. In this way, a noninvasive strategy for imaging of coronary artery disease is exceptionally alluring. The system of MDCT angiography in heart imaging is developing quickly. It has turned into a promising strategy with the expansion of locator lines from 4 slice to 16 slice and 64 slice scanners [48-51]. Expanding locator lines empower ensuing enhancements in image quality. Different points of interest of 64 slice CT incorporate diminished aggregate output time and lower measures of contrast media. These changes encourage breath holding and decrease the danger for complexity nephropathy [52].
Multi detector computed coronary angiography (MDCT) likewise permits noninvasive identification of calcified, non-calcified and mixed atheromatous plaques inside or neighboring of coronary artery and in addition surveying the level of stenosis. Our study included aggregate of 34 (36%) segments with <50% Stenosis, 43 (45%) segments 50-70% stenosis and 18 (19%) segments with >70% stenosis. The affectability and specificity of 64 slice MDCT for recognizing stenosis in 50-70% and >70% are 78.5% and 99%; 87.5% and 99.7%; 99.3% and 99.7% individually. The positive predictive value (PPV) and negative predictive value (NPV) are 71% and 99.3%; 87.5% and 99.8%; 99.2% and 99.7% individually. Over all correct nesses are 88.7%, 90.2% and 93.6% separately. Demonstrative exactness between conventional coronary angiography and 64 slice computed tomography for moderate 50-70% (p=0.316) stenosis and severe (p=0.865) stenosis were comparable with no critical distinction between both the methodology (p >0.05). Be that as it may, noteworthy contrast was found between conventional coronary angiography and 64 slice computed tomography with mild stenosis (p=0.033, p<0.05). 64 slice computed tomography overestimated mild <50% stenosis. Additionally, calcified plaques, non-calcified plaques and mixed plaques were likewise separated in light of CT thickness expecting limit of 130 HU for coronary calcium.
Radiation
Radiation measurements of 64 slice CT was assessed to be roughly around 15 mSv for men and 20 mSv for women [53]. These radiation dosage qualities were accomplished utilizing review ECG gating for stage synchronization. They are obviously a high viable measurement than is found in conventional coronary angiography (normal 7-10 mSv). A few dosage sparing methodologies, for example, planned ECG activating, X-beam pillar filtration, X-beam bar collimation, and programmed pitch adjustment, ECG controlled regulation of the tube present and low Kilo voltage [54] have brought about reduced radiation measurements of between 80% at lower heart rates and 50% at higher heart rates. Starting studies on the utilization of cutting edge iterative remaking methods for CT images, uncover as much as a 10 fold diminishment in the image noise and is unmistakably another energizing zone to potentially apply to heart imaging later on [55,56]. Planned gated step and shoot securing CT has fundamentally diminished the introduction measurements of coronary CTA route underneath the dosage of a conventional coronary angiogram. Late productions have demonstrated that by applying this method and suitable imaging conventions, exact images of the coronary arteries can be gotten at measurements as low as 1-2 mSv [57,58].
Calcification
Broad coronary artery calcification frequently restrains the capacity to investigate picture information by bringing on artifacts, for example, sprouting, shaft solidifying, streaking, dispersing, and noise. This applies to either 16 slice [59-61] or 64 slice scanners [62-64]. Sprouting artifacts are likely the most essential in the term of heart CTA and happen when high thickness items, such coronary artery calcium and small stent (<3 mm), involve a bit of >1 voxel [8].
The impact of these artifacts is to oversize calcified plaques on the CT image [65,66] with consequent over estimation of luminal narrowing and complementary underestimation of leftover coronary artery luminal measurement. One conceivable approach to go around the issue would be to perform an underlying unenhanced examine.
Despite the fact that this would maintain a strategic distance from imperfect coronary CTA in patients with extreme calcification [59,61]. This is greatly controversial [67]. Although spatial determination calculations have been appeared to diminish the degrees of sprouting [8] more propelled recreation calculations or iterative remaking methods will require serious processing control and have not been all around connected to CT.
Complications
Coronary angiographies are basic and significant complexities are uncommon. These incorporate cardiovascular arrhythmias, kidney harm, blood clusters (which can bring about heart assault or stroke), hypotension and pericardial emission. Minor complexities can incorporate draining or wounding at the site where the differentiation is infused, vein harm on the course to the heart from the catheter (uncommon) and unfavorably susceptible response to the contrast.
The general danger of Real confusions with left heart catheterization is 1-2%. An incorporate death, vascular inconveniences, MI, CVA, and contrast response. Variables expanding persistent danger incorporate Age, LMT or 3 vessels coronary disease, decompensated heart failure, serious aortic stenosis, diabetes, renal failure, and earlier CVA.
Side effects of contrast agent
• Anaphylactic reactions
• Non-anaphylactic reactions
• Cholesterol embolization syndrome
• Stroke
• Local complications
• Local hematoma and bleeding
• Pseudo aneurysm
• Arteriovenous fistula
• Retroperitoneal hematoma
Accuracy
• The dominant part of demonstrate that a negative CCTA (64 slice) can successfully preclude obstructive coronary artery disease.
• In a meta-examination [14] 64 slice CCTA had an affectability of 99% and negative predictive value (NPV) of 100% for patientbased location of significant CAD.
• However, the specificity has been lower than the affectability in many studies, and false positive results are conceivable, especially in patients with high calcium scores. In the planned multicenter trial of patients with chest pain without known CAD and intermediate disease prevalence, 64 slice CCTA had a patientbased affectability of 94% and a specificity of 83% in recognizing stenosis of 70% or more prominent (equivalent qualities were seen at a 50% stenosis level). Patients with high calcium scores were not avoided and calcium scores more noteworthy than 400 indicated critical lessening in specificity. The NPV of CCTA was 99% [68].
• In a meta-analysis, however, the sensitivity was highest in the left main artery and lowest (85%) in the circumflex artery [14].
Limitation of coronary CTA
Although coronary CTA examinations are expanding in use, coronary angiography is static methods for detecting coronary artery stenosis, which is a significant narrowing of an artery which normally desire treatment such as bypass surgery or stent.
• CTA is used only as a diagnostic test unlike, DSA which can be used for both diagnosis and treatment in single session. A high risk patient of coronary artery disease and classic symptoms might go through coronary angiography alternative to CTA.
• In many areas of old, calcified plaque patients, coronary CTA is generally not helpful.
• The opening of a conventional CT scanner might not be fit to a patient who is gigantic and over the weight limit 450 pounds for gigantic patients, some efficiency has extra-large bariatic capable CT scanners.
• This test would not be good for those candidates who are extremely over weighted or who have abnormal heart rhythms because quality of image might be compromised.
Coronary computed tomography angiography (CCTA) advantages over invasive coronary angiography (ICA)
CCTA has essential correlation and further distinction from invasive coronary angiography (ICA)
• CCTA may also provide information about the presence of extra luminal plaque and plaque composition that is not routinely available on ICA without the use of intravascular ultrasound [69-71].
• The CCTA information set additionally contains non coronary cardiovascular and additional heart thoracic data of significance [72-74] including myocardial, pericardial, and valvular morphology and capacity and additionally aortic and aspiratory vascular basic details.
• Subsequently cardiovascular CTA offers components in the same way as echocardiography and thoracic radiology not withstanding ICA.
Assessment of stenosis grading
There are many different methods to grade the degree of stenosis which includes
• Visual assessment.
• Manually decided width or cross-sectional range on multi planar reformats opposite to the middle centerline of the vessel ("end-on" perspective).
• Diameter on maximum intensity projection (MIP) images parallel to the long hub of the vessel
• Software count [75] of distance across or zone.
Dodd et al. found that the cross-sectional zone system had the most elevated connection with quantitative coronary angiography, and MIP procedure had the littlest bury onlooker variability Evaluating is less exact in calcified plaques and in distal coronary vessels.
Since the spatial determination is lacking for exact reviewing, coronary stenosis is regularly evaluated with semi quantitative descriptors.
Normal
Mild (<50%)
Moderate (50-70% stenosis)
Severe (>70% stenosis)
Occluded
Stenosis is typically overestimated in areas where heavily calcified plaques are present. Zhang et al offer the following suggestions to better assess the degree of stenosis when calcified plaques are present [76].
• A noteworthy luminal stenosis is far-fetched if the plaque thickness measures half or less of the width of a close-by typical portion and on the off chance that it is unconventionally situated on a crosssectional multi planar reconstruction (MPR) view or there is noticeable lumen nearby the plaque on a long-hub MPR view.
• A huge stenosis is likely if calcified plaque fills the whole focal bit of the lumen on a cross-sectional MPR image.
• A noteworthy stenosis can be recommended if calcified plaque is half or more prominent than distance across of a close-by ordinary portion on cross sectional MPR images yet does not totally fill the lumen; however, the translator may include that CCTA may overestimate the level of stenosis in this circumstance.
Recommended quantitative stenosis grading
0 Normal: Absence of plaque and no luminal stenosis; 1 Minimal: Plaque with 0.25% stenosis; 2 Mild: 25-49% stenosis; 3 Moderate: 50-69% stenosis; 4 Severe: 70-99% stenosis; 5 Occlusion
Optional quantitative stenosis grading
0 Normal: Absence of plaque and no luminal; 1 Mild: Plaque with 0.39% stenosis; 2 Moderate: 40-69%stenosis; 3 Severe: 70-99%stenosis; 4 Occluded
Benefits vs. Risk for CCTA
Benefits
• Coronary CTA is not invasive in appreciation to cardiovascular catheterization. Cardiovascular catheterization invasive, has more difficulties identified with the position of a long catheter into the arterial routes and the development of the catheter in the artery, and requires more opportunity for the patient to recover.
• A real point of interest of CT is that it can see bone, delicate tissue and veins all in the meantime. It is subsequently suited to distinguish different explanations behind your inconvenience, for example, harm to the aorta or blood coagulation in the lungs.
• Unlike routine X-ray, CT checking gives extremely point by point images of numerous sorts of tissue.
• CT examinations are quick and straightforward.
• CT has been appeared to be financially savvy for an extensive variety of therapeutic issues.
• CT is less touchy to patient development than MRI.
• CT can be performed in the event that you have an embedded restorative gadget of any sort, dissimilar to MRI.
• No radiation stays in a patient's body after a CT examination.
• X-ray utilized as a part of standard CT checks have no quick reactions.
Risks
• In some individuals with irregular kidney function, the dye utilized as a part of CT checking may decline kidney capacity.
• Not reasonable for patients with severe diabetes.
• Have unstable vital signs.
• If huge measure of X-ray contrast material leaks out from the vessel being infused and spreads under the skin where the IV is set, skin harm or harm to veins and nerves, however improbable, can come about. Continuously a slight possibility of malignancy from over the top presentation to radiation.
• There is dependably a slight shot of growth from intemperate introduction to radiation. Be that as it may, the advantage of a precise diagnosis will for the most part exceed the danger.
• Women ought to dependably educate their doctor and X-ray or CT technologist if there is any probability that they are pregnant. CT checking is, as a rule, not suggested for pregnant ladies unless therapeutically fundamental on account of potential danger to the infant.
• Manufacturers of intravenous contrast show mothers ought not breastfeed their children for 24-48 hours after contrast medium is given. In any case, both the American College of Radiology (ACR) and the European Society of Urogenital Radiology take note of that the accessible information propose that breastfeeding is sheltered to proceed subsequent to accepting intravenous contrast.
• The danger of genuine unfavorably susceptible response to contrast materials that contain iodine is to a great degree uncommon, and radiology offices are all around furnished to manage them.
Blooming artifacts
High attenuation structures, for example, calcified plaques or stents, seem broadened for (or blossomed) due to incomplete volume averaging impacts and cloud the adjoining coronary lumen. Although sharper filters or kernels and thinner slices (0.5-0.6 mm) may reduce these artifacts and may empower an enhanced evaluation of stent patency, they have little impact on calcified plaques. It is clear that serious coronary calcification is at present the real constraining component; in this way, the end of calcium blooming artifacts is of most extreme significance for the achievement of coronary CT A. Truth be told, the nearness of thick calcified plaques is the fundamental cause of false-positive results in coronary CTA on account of overestimation of the level of stenosis, possibly expanding the quantity of subjects experiencing both invasive specific coronary angiography and coronary CTA, particularly in patient populaces with a high prevalence of coronary calcification [15,77]. A non-contrast calcium screening examine before coronary CTA (radiation presentation of around 1.3 mSv) could be performed to choose whether to perform ensuing coronary CT A. Truth be told, a solitary expansive calcified plaque in a proximal area may keep the rejection of noteworthy coronary artery stenosis. In this way, until the calcium blossoming issue has been settled, the capacity to securely avoid the nearness of huge coronary artery stenosis stays constrained in population with a high predominance of coronary calcification.
Limitation of MRA
One of the issues that have as of late developed and confine the across the board clinical use of coronary MRA is the critical increment of percutaneous methodology with stent situation, as the long term patency is fundamentally superior to in the conventional balloon angioplasty procedures. Imaging with MRI is sheltered in these patients.
Indeed, even quickly after the situation of the stent, yet the material utilized for stents stainless steel, composite or tantalum) makes powerlessness artifacts from the metal-affected field inhomogeneity. These artifacts present as sign voids at the site of the stent, which forbid assessment of adjoining fragments of the coronary artery. The signal loss relies on upon the succession utilized and is moderately bigger for bright blood groupings. Assessment of the blood stream and its bearing proximally and distally to the stent may furnish roundabout data with reference to the stent patency and is an optional technique for evaluating stents that has been tried effectively.
In spite of the fact that, MRI is a non-invasive strategy with no short or long term hazard, patients may have contraindications, for example, pacemakers, intracranial clips, or certain other Metal inserts or they might be claustrophobic. To get a decent quality coronary MRA concentrate commonly requires a customary heart rhythm and reliable breath-holding or consistent respiratory rhythm.
Cardiac motion
Two wellsprings of movement are connected with coronary MRA: movement identified with characteristic cardiovascular constriction/ unwinding and movement owing to superimposed diaphragm and chest wall movement during respiration. Since the degree of movement surpasses the measurement of the coronary artery, obscuring artifact of the coronary artery lumen will happen unless sufficient movement motion strategies are connected. ECG gating is utilized to represent natural heart movement.
Respiratory motion
A clear way to deal with stifling respiratory movement includes the utilization of breath-holding during coronary MRA. Be that as it may, breath-holding methodologies have a few constraints. To start with, spatial and temporal image resolution is restricted by the patient's capacity to hold his or her breath. MRA have restricted appropriateness to the expansive scope of patients with cardiovascular illness.
Images acquired during coronary MRA can be envisioned in 2- dimensional (2D) or 3-dimensional (3D) views. The heart constrictions and the movement as far as possible the nature of images. Diverse strategies, for example, a breath hold procedure versus a free breathing with navigator echo based system, have been utilized to beat these impediments. For a 2D coronary MRA using the breath hold method, the patient might be required to do 30 or more breath holds for 16-20 seconds, and might be much more for a 3D coronary MRA. Then again, the free breathing with navigator method empowers respiratory synchronization of image obtaining to a particular stage and spatial area of the diaphragm with imminent or review gating.
Two principle approaches have been produced to envision the endovascular lumen. In the routine twist reverberation approach, the ranges of the vessel with turbulent stream (non-stenosed fragments) seem dark, though in the ordinarily utilized angle reverberation approach, with laminar stream seem dark in shading, and those with turbulent stream auxiliary to stenosis show up bright [78-80]. Other specialized hindrances incorporate a generally small coronary artery diameter (2.7 to 3.5 mm) [81], convoluted course of the vessels and the encompassing epicardial fat. Besides, the interpretation of the imaging of a left circumflex coronary artery in MRA is restricted by trouble to recognize the artery from the parallel running cardiovascular veins [80,81].
The analytic precision of 2D and 3D coronary MRA in contrast with conventional coronary angiography is not yet standardized, the present strategy for coronary MRA consolidates quick imaging 3D procedures with respiratory gated coronary MRA utilizing guide echo that enhances its indicative exactness. The navigator echo procedure appears to have more application in clinical practice, as the breath hold method is not generally possible for patients with congestive heart failure, CAD, and chronic obstructive pulmonary disease [79,80]. Nonetheless, in those cases the nature of images might be debased because of conflicting breathing patterns and patient developments [82]. The other option systems incorporate magnetic resonance subtraction techniques, which incorporate particular labeling of blood in the aortic root and suppression of the foundation tissue. This technique holds potential for representation of the proximal bit of the coronary artery, however the length of the vessel must be pictured if there is blood stream all through the coronary artery. In this manner, if the blood stream is impeded in the nearness of coronary artery stenosis, perception of the whole artery is impractical. Other strategy, for example, spiral acquisition planar imaging [83] and fragment echo planar imaging techniques [84], give a complete 3D information set packing the whole heart and can be gained in maybe a couple breath holds.
2D gradient-echo breath-hold coronary MRA has several drawbacks
• Relatively thick areas (4-6 mm in many studies) may block a precise evaluating for central stenosis [85-87]. This likely additionally clarifies the restricted assessment of convoluted vessels and the distal segments of major coronary artery, particularly the left circumflex coronary artery [87-89].
• Different oblique planes are required for various patients and for the representation of various arteries [88,89].
• Multiple breath holds can be a commonsense issue in certain patient population with the history of congestive heart failure, COPD, and severe CAD [79,80].
• Inconsistent breath-holds and miss-enrollment between the breath holds may prompt deficient vessel assessment [89-91].
Nevertheless, 3D coronary MRA also has several limitations
• Some pictures may not be gotten amid the sought end expiratory stage [92].
• Patient participation is vital with consistent, rhythmic breath and no development for the entire acquisition time of around 35 minutes.
• Temporal and spatial resolutions are basic components for picture quality in coronary MRA [93,94].
Application of coronary MRA
Coronary MRA is a symptomatic methodology with phenomenal delicate tissue contrast and, in this way, allows perception and investigation of plaques and the segments of the arteries. This has been appeared in the atherosclerotic injuries in vitro and in vivo in substantial arteries, for example, the carotid arteries [95,96]. Coronary MRA is profoundly compelling in distinguishing coronary artery anomalies [97]. Conventional coronary MRA is an imperative symptomatic instrument for the analysis of patency of coronary artery bypass grafts, as the arteries have lesser portability with heart and respiratory movement furthermore have a bigger lumen (5-10 mm) [98]. Nagel et al. thought about high measurement dobutamine stress magnetic resonance imaging (DMRI) with dobutamine stress echocardiography and found that DMRI was more delicate and more particular then dobutamine stress echocardiography in the recognition of myocardial ischemia utilizing coronary stenosis by arteriography as the best quality level. Hundley et al. [99] reported that DMRI gives excellent symptomatic data and additionally prognostic data.
Cardiovascular MRI is in a perfect world suited for the identification of myocardial suitability due to its capacity to survey the transmural of myocardial scar, and myocardial performance [100]. At the current situation with specialized improvement, the affectability and specificity of coronary MRA with retrospective navigator echo respiratory triggering is only modest. The strategy is poor and not valuable as a screening technique for CAD [101].
The benefit of traditional catheter angiography is that treatment with a stent should be possible instantly at the time of finding, while patients with stenosis analyzed by MRI or CT will probably need to calendar catheterization for treatment on one more day. What's more, CT angiography require introduction to radiation and conceivably harmful dye. Consolidating MRI with coronary angiography may give a noteworthy point of interest to certain sorts of patients
"The principle distinction/point of interest is the non-invasive nature of CT and MRI with lower examination time, higher patient comfort. Risk benefit must be considered for individual patient and depends on upon both patient qualities and the clinical situation’’.
Limitations
Despite the fact that this examination was attempted to be precisely set, I am still mindful of its unavoidable restrictions. Firstly, because of as far as possible, this examination was led on a small size of information (number of patient). Secondly, additionally experienced issues in visual investigation and measuring the distance across of coronary artery. Finally, over workload, as we were required to have full time obligations, contemplates, classes and so forth, these components may have influenced the result of results to some degree.
Conclusion
Coronary lesions can be distinguished with higher affectability, specificity. Negative predictive value and positive predictive value by multi detector computed tomography (MDCT). By and large, this study demonstrates that multi detector computed coronary angiography (MDCCA) could turn into an analytic distinct option for conventional coronary angiography (CCA) for reviewing and measurement of stenosis knowing the few restrictions of conventional coronary angiography. Notwithstanding, the capability of multi detector computed coronary angiography (MDCCA) in the recognition of distal anastomotic stenosis may be restricted.
Specifically, a small distal coronary vessel can prompt overestimation of anastomotic stenosis. However, multi detector computed coronary angiography (MDCCA) could be an accurate imaging technique for the exclusion of greater than 50% stenosis and occlusion. It can be utilized with higher precision as a part of clinical practice as a noninvasive option imaging strategy for clinically suspected coronary artery disease (CAD).
Coronary MRA is a quickly advancing, new non-invasive system. Although coronary MRA in no time has constrained clinical utility, it the possibility to help in the conclusion of coronary artery stenosis with a high level of exactness, particularly in the proximal and middle sections, however stays trying for distal coronary arteries. Magnetic resonance technology has some limitations, which improves it hard to have representation of the coronary arteries.
These confinements are optional to the convoluted course of the coronary arteries, coronary arteries of smaller breadth (2.7 to 35 mm), fast development brought on by respiratory and cardiovascular compressions, and the encompassing epicardia fat. It might likewise be hard to recognize the coronary arteries from the parallel running coronary veins during the interpretation of coronary MRA, particularly for the left circumflex coronary arteries [26,27,100,101]. Despite the fact that coronary MRA is a conceivably valuable clinical application, particularly in patients a low likelihood of CAD, it doesn't permit representation of smaller vessels, for example, side branches or the distal fragments of vast epicardia arteries [101]. A few ways to deal with coronary MRA have been depicted, however nobody method can be all around connected [102]. Future examination ought to concentrate on the advancement of ideal respiratory techniques by enhancing the demonstrative and spatial determination to picture more prominent lengths of coronary arteries and fast obtaining of the information.
New systems are being explored to enhance the indicative precision, particularly the utilization of intravenous contrast media, furthermore to decrease the securing time with volume target imaging. It is possible that advances in innovation will help in accomplishing this objective not long from now.
References
- American Heart Association (2001) Heart and stroke statistical update. Dallas, TX.
- (2017) Heart attack coronary artery disease. Mount sinai hospital, New York.
- Chow BJ, Veinot JP (2006) What are the most useful and trustworthy noninvasive anatomic markers of existing vascular disease? Curr Cardiol Rep 8: 439-445.
- Chen JW, Wasserman BA (2005) Vulnerable plaque imaging. Neuroimaging Clin N Am 15: 609-621.
- Kunimasa T, Sato Y, Sugi K, Moroi M (2005) Evaluation by multislice computed tomography of atherosclerotic coronary artery plaques in non-culprit, remote coronary arteries of patients with acute coronary syndorme. Circ J 69: 1346-1351.
- Hassan A, Nazir SA, Alkadhi H (2011) Technical challenges of coronary CT angiography: Today and tomorrow. Eur J Radiol 79: 161-171.
- Becker CR. Knez A, Leber A (2000) Initial experiences with multislice detector spiral CT in diagnosis of arteriosclerosis of coronary vessels. Radiology 40: 118-122.
- Becker CR, Ohnesorge BM, Schoepf UJ (2000) Current development of cardiac imaging with multidetector-row CT. Eur J Radiol. 36: 97-103.
- Kopp AF, Ohnesorge B, Flohr T (2000) Cardiac multidetector-row CT: First clinical results of retrospectively ECG-gated spiral with optimized temporal and spatial resolution. Fortschr Rontgenstr 172: 429-435.
- Kopp AF, Schroeder S, Kuettner A (2001) Coronary arteries: Retrospectively ECG-gated multi-detector row CT angiography with selective optimization of the image reconstruction window. Radiology 221: 683-688.
- Kim SY, Seo JB, Do KH (2006) Coronary artery anomalies: Classification and ECG-gated multi-detector row CT findings with angiographic correlation. Radiographics 26: 317-334.
- https://www.journals.elsevier.com/journal-of-clinical-neuroscience
- Bluemke DA, Achenbach S, Budoff M, Gerber TC, Gersh B, et al. (2008) Noninvasive coronary artery imaging magnetic resonance angiography and multidetector computed tomography angiography: A scientific statement from the american heart association committee on cardiovascular imaging and intervention of the council on cardiovascular radiology and intervention, and the councils on clinical cardiology and cardiovascular disease in the young. Circulation 118: 586-606.
- Mowatt G, Cummins E, Waugh N, Walker S, Cook J, et al. (2008) Systematic review of the clinical effectiveness and cost-effectiveness of 64-slice or higher computed tomography angiography as an alternative to invasive coronary angiography in the investigation of coronary artery disease. Health Technol Assess 12: 143.
- Schuijf JD, Bax JJ, Shaw LJ, de Roos A, Lamb HJ, et al. (2006) Meta-analysis of comparative diagnostic performance of magnetic resonance imaging and multislice computed tomography for noninvasive coronary angiography. Am Heart J 151: 404-411.
- Paulin S, von Schulthess GK, Fossel E, Krayenbuehl HP (1987) MR imaging of the aortic root and proximal coronary arteries. AJR Am J Roentgenol 148: 665-670.
- Nagel E, Lehmkuhl HB, Bocksch W, Klein C, Vogel U, et al. (1999) Noninvasive diagnosis of ischemia-induced wall motion abnormalities with the use of high-dose dobutamine stress magnetic resonance imaging: Comparison with dobutamine stress echocardiography. Circulation. 99: 763-770.
- (1998) The clinical role of magnetic resonance in cardiovascular disease: Task force of the european society of cardiology, in collaboration with the association of european pediatric cardiologist. Eur Heart J 19: 19-39.
- Sechtem U, Baer FM, Voth E, Theissen P, Schneider CA (1999) Stress functional MRI: Detection of ischemic heart disease and myocardial viability. J Magn Reson Imaging 10: 667-675.
- Van-Rossum AC, Galjee MA, Post JC, Visser CA (1997) A practical approach to MRI of coronary artery bypass graft patency and flow. Int J Card Imaging 13: 199-204.
- Toussaint JF, LaMuraglia GM, Southern JF, Fuster V, Kantor HL (1996) Magnetic resonance images lipid, fibrous, calcified, hemorrhagic, and thrombotic components of human atherosclerosis in vivo. Circulation 94: 932-938.
- Fayad ZA (2003) MR imaging for the noninvasive assessment of atherothrombotic plaques. Magn Reson Imaging Clin N Am 11: 101-13.
- Post JC, Van-Rossum AC, Hofman MB, de-Cock CC, Valk J, et al. (1997) Clinical utility of two-dimensional magnetic resonance angiography in detecting coronary artery disease. Eur Heart J 18: 426-433.
- Watanuki A, Yoshino H, Udagawa H, Yokoyama K, Nitatori T, et al. (2000) Quantitative evaluation of coronary stenosis by coronary magnetic resonance angiography. Heart Vessels 15: 159-166.
- Sakuma H, Caputo GR, Steffens JC, O'Sullivan M, Bourne MW, et al. (1994) Breath-hold MR cine angiography of coronary arteries in healthy volunteers: Value of multiangle oblique imaging planes. AJR Am J Roentgenol 163: 533-537.
- Yoshino H, Nitatori T, Kachi E, Yano K, Taniuchi M, et al. (1997) Directed proximal magnetic resonance coronary angiography compared with conventional contrast coronary angiography. Am J Cardiol 80: 514-518.
- Post JC, van-Rossum AC, Hofman MB, Valk J, Visser CA, (1995) Protocol for two-dimensional magnetic resonance coronary angiography studied in three-dimensional magnetic resonance data sets. Am Heart J 130: 167-173.
- Duerinckx AJ, Atkinson DP, Mintorovitch J, Simonetti OP, Vrman MK (1996) Two-dimensional coronary MRA: Limitations and artifacts. Eur Radiol 6: 312-325.
- Paschal CB, Haacke EM, Adler LP (1993) Three-dimensional MR imaging of the coronary arteries: Preliminary clinical experience. J Magn Reson Imaging 3: 491-500.
- Li D, Paschal CB, Haacke EM, Adler LP (1993) Coronary arteries: Three-dimensional MR imaging with fat saturation and magnetization transfer contrast. Radiology 187: 401-406.
- Wielopolski PA, van-Geuns RJ, de-Feyter PJ, Oudkerk M (2000) Coronary arteries. Eur Radiol 10: 12-35.
- Moshage W, Achenbach S, Daniel WG (2001) Novel approaches to the non-invasive diagnosis of coronary-artery disease. Nephrol Dial Transplant 16: 21-28.
- Austen WG, Edwards JE, Frye RL, Gensini GG, Gott VL, et al. (1975) A reporting system on patients evaluated for coronary artery disease. Report of the Ad hoc committee for grading of coronary artery disease, Council on cardiovascular surgery, American Heart Association. Circulation 51: 5-40.
- Pannu HK, Alvarez W, Fishman EK (2006) β-blockers for cardiac CT: A primer for the radiologist. Am J Roentgenol 186: S341–S345.
- (2009) Physicians' desk reference. Montvale, NJ: Thomson PDR.
- Beller GA (2006) A proposal for an advanced cardiovascular imaging training track. J Am Coll Cardiol. 48: 1299-1303.
- Achenbach S, Ropers D, Kuettner A, Flohr T, Ohnesorge B, et al. (2006) Contrast-enhanced coronary artery visualization by dual-source computed tomography-initial experience. Eur J Radiol 57: 331-335.
- Flohr T, Küttner A, Bruder H, Stierstorfer K, Halliburton SS, et al. (2003) Performance evaluation of a multi-slice CT system with 16-slice detector and increased gantry rotation speed for isotropic submillimeter imaging of the heart. Herz 28: 7-19.
- Halliburton SS, Stillman AE, Flohr T, Ohnesorge B, Obuchowski N, et al. (2003) Do segmented reconstruction algorithms for cardiac multi-slice computed tomography improve image quality? Herz 28: 20-31.
- Ohnesorge B, Flohr T, Becker C, Kopp AF, Schoepf UJ, et al. (2000) Cardiac imaging by means of electrocardiographically gated multisection spiral CT: Initial experience. Radiology 217: 564-571.
- Vogl TJ, Abolmaali ND, Diebold T, Engelmann K, Ay M, et al. (2002) Techniques for the detection of coronary atherosclerosis: Multi-detector row CT coronary angiography. Radiology 223: 212-220.
- Ropers D, Baum U, Pohle K, Anders K, Ulzheimer S, et al. (2003) Detection of coronary artery stenoses with thin-slice multi-detector row spiral computed tomography and multiplanar reconstruction. Circulation 107: 664-666.
- Kerl JM, Hofmann LK, Thilo C, Vogl TJ, Costello P, et al. (2007) Coronary CTA: Image acquisition and interpretation. J Thorac Imaging 22: 22-34.
- Ferencik M, Ropers D, Abbara S, Cury RC, Hoffmann U, et al. (2007) Diagnostic accuracy of image postprocessing methods for the detection of coronary artery stenoses by using multidetector CT. Radiology 243: 696-702.
- Dodd JD, Rieber J, Pomerantsev E, Chaithiraphan V, Achenbach S, et al. (2008) Quantification of nonculprit coronary lesions: Comparison of cardiac 64-MDCT and invasive coronary angiography. AJR Am J Roentgenol 191: 432-438.
- Lu B, Dai RP, Jiang SL, Bai H, He S, et al. (2001) Effects of window and threshold levels on the accuracy of three-dimensional rendering techniques in coronary artery electron-beam CT angiography. Acad Radiol 8: 754-761.
- Regenfus M, Ropers D, Achenbach S, Schlundt C, Kessler W, et al. (2003) Diagnostic value of maximum intensity projections versus source images for assessment of contrast-enhanced three-dimensional breath-hold magnetic resonance coronary angiography. Invest Radiol 38: 200-206.
- Nieman K, Oudkerk M, Rensing BJ (2001) Coronary angiography with multi-slice computed tomography. Lancet 357: 599-603.
- Kopp AF, Schroeder S, Kuettner A, Baumbach A, Georg C, et al. (2002) Non-invasive coronary angiography with high resolution multidetector-row computed tomography: Results in 102 patients. Eur Heart J 23: 1714-1725.
- Achenbach S, Giesler T, Ropers D (2001) Detection of coronary artery stenoses by contrast-enhanced, retrospectively electrocardiographically-gated, multislice spiral computed tomography. Circulation 103: 2535-2538.
- Kuettner A, Trabold T, Schroeder S (2004) Noninvasive detection of coronary lesions using 16?detector multislice spiral computed tomography technology. J Am Coll Cardiol 44: 1230-1237.
- Ehara M, Surmely JF, Kawai M (2006) Diagnostic accuracy of 64-slice computed tomography for detecting angiographically significant coronary artery stenosis in an unselected consecutive patient population: Comparison with conventional invasive angiography. Circ J 70: 564-571.
- Paul JF, Abada HT (2007) Strategies for reduction of radiation dose in cardiac multislice CT. Eur Radiol 17: 2028-2037.
- Leschka S, Stolzmann P, Schmid FT (2008) Low kilovoltage cardiac dual-source CT: attenuation, noise, and radiation dose. Eur Radiol. 18: 1809-1817.
- Hsieh J, Londt J, Dutta S, Okerlund D, Woodford M (2006) High-resolution low-noise reconstruction for EKG-gated chest scans.
- Supanich M, Rowley H, Chen G, Hsieh J, Mistretta C (2006) Dose reduction in neuro CT exams using highly constrained back projection (HYPR) techniques. RSNA.
- Husmann L, Valenta I, Gaemperli O (2008) Feasibility of low-dose coronary CT angiography: First experience with prospective ECG-gating. Eur Heart J 29: 191-197.
- Husmann L, Valenta I, Kaufmann PA (2008) Coronary angiography with low-dose computed tomography at 1.4?mSv. Herz 33: 75.
- Morgan-Hughes GJ, Roobottom CA, Owens PE (2005) Highly accurate coronary angiography with submillimetre, 16-slice computed tomography. Heart 91: 308-313
- Martuscelli E, Romagnoli A, D’Eliseo A (2004) Accuracy of thin-slice computed tomography in the detection of coronary stenoses. Eur Heart J 25: 1043-1048.
- Heuschmid M, Kuettner A, Schroeder S (2005) ECG-gated 16-MDCT of the coronary arteries: assessment of image quality and accuracy in detecting stenoses. Am J Roentgenol 184: 1413-1419.
- Mollet NR, Cademartiri F, van-Mieghem CA (2005) High-resolution spiral computed tomography coronary angiography in patients referred for diagnostic conventional coronary angiography. Circulation 112: 2318-2323.
- Leschka S, Alkadhi H, Plass A (2005) Accuracy of MSCT coronary angiography with 64-slice technology: First experience. Eur Heart J 26: 1482-1487.
- Thilo C, Auler M, Zwerner P, Costello P, Schoepf UJ (2007) Coronary CTA: Indications, patient selection, and clinical implications. J Thorac Imaging 22: 35-39.
- Mollet NR, Cademartiri F, Krestin GP (2005) Improved diagnostic accuracy with 16-row multi-slice computed tomography coronary angiography. J Am Coll Cardiol 45: 128-132.
- Mollet NR, Cademartiri F, Nieman K (2004) Multislice spiral computed tomography coronary angiography in patients with stable angina pectoris. J Am Coll Cardiol 43: 2265-2270.
- Cademartiri F, Mollet NR, Lemos PA (2005) Impact of coronary calcium score on diagnostic accuracy for the detection of significant coronary stenosis with multislice computed tomography angiography. Am J Cardiol 95: 1225-1227.
- Budoff MJ, Dowe D, Jollis JG, Gitter M, Sutherland J, et al. (2008) Diagnostic performance of 64-multidetector row coronary computed tomographic angiography for evaluation of coronary artery stenosis in individuals without known coronary artery disease: Results from the prospective multicenter ACCURACY (Assessment by Coronary Computed Tomographic Angiography of Individuals Undergoing Invasive Coronary Angiography) trial. J Am Coll Cardiol 52: 1724-1732.
- Hoffmann U, Moselewski F, Nieman K, Jang IK, Ferencik M, et al. (2006) Noninvasive assessment of plaque morphology and composition in culprit and stable lesions in acute coronary syndrome and stable lesions instable angina by multidetector computed tomography. J Am Coll Cardiol 47: 1655-1662.
- Leber AW, Knez A, Becker A, Becker C, Reiser M, et al. (2005) Visualising noncalcified coronary plaques by CT. Int J Cardiovasc Imaging 21: 55-61.
- Lin F, Shaw LJ, Berman DS, Callister TQ, Weinsaft JW, et al. (2008) Multidetector computed tomography coronary artery plaque predictors of stress-induced myocardial ischemia by SPECT. Atherosclerosis 197: 700-709.
- Kaplan S, Aronow WS, Ahn C, Lai H, DeLuca AJ, et al. (2008) Prevalence of an increased ascending thoracic aorta diameter diagnosed by two-dimensional echocardiography versus 64-multislice cardiac computed tomography. Am J Cardiol 101: 119-121.
- Castorina S, Riccioli V (2007) Heart, aorta, peripheral and supra aortic trunks imaging realized by MSCT 64. Our experience. Ital J Anat Embryol 112: 131-143.
- Cook SC, Raman SV (2007) Unique application of multislice computed tomography in adults with congenital heart disease. Int J Cardiol 19: 101-106
- Dodd JD, Rieber J, Pomerantsev E (2008) Quantification of nonculprit coronary lesions: comparison of cardiac 64-MDCT and invasive coronary angiography. Am J Roentgenol 191: 432-438.
- Zhang S, Levin DC, Halpern EJ, Fischman D, Savage M, et al. (2008) Accuracy of MDCT in assessing the degree of stenosis caused by calcified coronary artery plaques. AJR Am J Roentgenol 191: 1676-1683.
- Lorenz CH, Johansson LO (1999) Contrast-enhanced coronary MRA. J Magn Reson Imaging 10: 703-708.
- Davidson CJ, Fishman RF, Bonow RO (1997) Cardiac catheterization: Heart disease (5th edn.) WB Saunders, Philadelphia. pp: 177-203.
- Foo TK, Saranathan M, Hardy CJ, Ho VB (2000) Coronary artery magnetic resonance imaging: A patient-tailored approach. Top Magn Reson Imaging 11: 406-416.
- Danias PG, Edelman RR, Manning WJ (1998) Coronary MR angiography. Cardiol Clin 16: 207-225.
- Dodge JT, Jr. Brown BG, Bolson EL, Dodge HT (1992) Lumen diameter of normal human coronary arteries. Influence of age, sex, anatomic variation, and left ventricular hypertrophy or dilation. Circulation. 86: 232-246.
- Taylor AM, Jhooti P, Wiesmann F, Keegan J, Firmin DN, et al. (1997) MR navigator-echo monitoring of temporal changes in diaphragm position: Implications for MR coronary angiography. J Magn Reson Imaging 7: 629-636.
- Manning WJ, Edelman RR (1995) Coronary MR angiography. Radiology 195: 875-876.
- Wielopolski PA, Manning WJ, Edelman RR (1995) Single breath-hold volumetric imaging of the heart using magnetization-prepared 3-dimensional segmented echo planar imaging. J Magn Reson Imaging 5: 403-409.
- Manning WJ, Li W, Edelman RR (1993) A preliminary report comparing magnetic resonance coronary angiography with conventional angiography. N Engl J Med. 328: 828-832.
- Duerinckx AJ, Urman MK (1994) Two-dimensional coronary MR angiography: Analysis of initial clinical results. Radiology 193: 731-738.
- Pennell DJ, Bogren HG, Keegan J, Firmin DN, Underwood SR (1996) Assessment of coronary artery stenosis by magnetic resonance imaging. Heart 75: 127-133.
- Hofman MB, Paschal CB, Li D, Haacke EM, van-Rossum AC, et al. (1995) MRI of coronary arteries: 2D breath-hold vs. 3D respiratory-gated acquisition. J Comput Assist Tomogr 19: 56-62.
- Post JC, van-Rossum AC, Hofman MB, Valk J, Visser CA (1996) Three-dimensional respiratory-gated MR angiography of coronary arteries: Comparison with conventional coronary angiography. AJR Am J Roentgenol 166: 1399-1404.
- Kim WY, Danias PG, Stuber M, Flamm SD, Plein S, et al. (2001) Coronary magnetic resonance angiography for the detection of coronary stenoses. N Engl J Med 345: 1863-1869.
- Muller MF, Fleisch M, Kroeker R, Chatterjee T, Meier B, et al. (1997) Proximal coronary artery stenosis: Three-dimensional MRI with fat saturation and navigator echo. J Magn Reson Imaging 7: 644-651.
- Nikolaou K, Huber A, Knez A, Becker C, Bruening R, et al. (2002) Intraindividual comparison of contrast-enhanced electron-beam computed tomography and navigator-echo-based magnetic resonance imaging for noninvasive coronary artery angiography. Eur Radiol 12: 1663-1671.
- Kessler W, Achenbach S, Moshage W, Zink D, Kroeker R, et al. (1997) Usefulness of respiratory gated magnetic resonance coronary angiography in assessing narrowings 50% in diameter in native coronary arteries and in aortocoronary bypass conduits. Am J Cardiol 80: 989-993.
- Bunce NH, Pennell DJ (2001) Magnetic resonance of coronary arteries. Eur Radiol 11: 721-731.
- Shinnar M, Fallon JT, Wehrli S, Levin M, Dalmacy D, et al. (1999) The diagnostic accuracy of ex-vivo MRI for human atherosclerotic plaque characterization. Arterioscler Thromb Vasc Biol 19: 2756-2761.
- Yuan C, Beach KW, Smith LH, Jr. Hatsukami TS (1998) Measurement of atherosclerotic carotid plaque size in-vivo using high resolution magnetic resonance imaging. Circulation 98: 2666-2671.
- Vliegen HW, Doornbos J, de-Roos A, Jukema JW, Bekedam MA, et al. (1997) Value of fast gradient echo magnetic resonance angiography as an adjunct to coronary arteriography in detecting and confirming the course of clinically significant coronary artery anomalies. Am J Cardiol 79: 773-776.
- White RD, Caputo GR, Mark AS, Modin GW, Higgins CB (1987) Coronary artery bypass graft patency: Noninvasive evaluation with MR imaging. Radiology 164: 681-686.
- Hundley WG, Morgan TM, Neagle CM, Hamilton CA, Rerkpattanapipat P, et al. (2002) Magnetic resonance imaging determination of cardiac prognosis. Circulation 106: 2328-2333.
- Mankad S, Khalil R, Kramer CM (2003) MRI for the diagnosis of myocardial ischemia and viability. Curr Opin Cardiol 18: 351-356.
- Ikonen AE, Manninen HI, Vainio P, Hirvonen TP, Vanninen RL, et al. (2003) Three-dimensional respiratory-gated coronary MR angiography with reference to x-ray coronary angiography. Acta Radiol 44: 583-589.
- Van-der-Wall EE, Vliegen HW, de-Roos A, Bruschke AV (1995) Magnetic resonance imaging in coronary artery disease. Circulation 92: 2723-2739.
Relevant Topics
- Acupuncture
- Acute Pain
- Analgesics
- Anesthesia
- Arthroscopy
- Chronic Back Pain
- Chronic Pain
- Hypnosis
- Low Back Pain
- Meditation
- Musculoskeletal pain
- Natural Pain Relievers
- Nociceptive Pain
- Opioid
- Orthopedics
- Pain and Mental Health
- Pain killer drugs
- Pain Mechanisms and Pathophysiology
- Pain Medication
- Pain Medicine
- Pain Relief and Traditional Medicine
- Pain Sensation
- Pain Tolerance
- Post-Operative Pain
- Reaction to Pain
Recommended Journals
Article Tools
Article Usage
- Total views: 8186
- [From(publication date):
September-2017 - Apr 02, 2025] - Breakdown by view type
- HTML page views : 7224
- PDF downloads : 962