Comparison of depression among married and divorced people in Ethiopia: Meta-analysis and systematic review
DOI: 10.4172/1522-4821.1000493
Abstract
Background: At a global level, over 300 million people were estimated to suffer from depression in 2015, which was equivalent to 4.4% of the world’s population. In Ethiopia, mental illness in particular depression is the leading non-communicable disorder in terms of burden. Depression has an impact on productivity, motivation to work, sleep behavior of the individual, and outcome of different chronic diseases. It is known that in order to set different prevention strategy providing reliable and up-to-date evidence on depression is very essential. Therefore, the purpose of this review is to provide latest available comparison of depression among married and divorced people in Ethiopia. Methods: This is systemic review and meta-analysis by study design. We systematically searched the databases: Google Scholar, Medline and Web of science database for studies conducted in Ethiopia on the availability of depression since 2010. The assessment of included studies were done using checklist developed by Joanna Briggs Institute which consists of eight points to screen article. Combined effect size across the studies using Mantel-Haenszel (MH) statistic (random effect model) and moderator analysis by taking prevalence of depression as fixed factor was used. The 𝐼2 statistic was used to assess variation across studies and above 50% was considered as significant. Egger’s and Begg’s tests were used to assess for publication bias. Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) guidelines protocol was used to write and compile the report. Results: We screened a total of 351 articles. From these, 20 studies were included in the final systematic review and meta-analysis. In Ethiopia, the combined effect size of all studies revealed a statistically significant association between marital status and depression (pooled OR = 0.57; 95% CI: 0.37–0.86). Conclusions: We found that divorced people were more likely to have depression than married people. Thus, more attention should be paid to strengthen activities which discourage divorce at community level and integrating mental health counseling into health extension programme is advisable.
Keywords: Depression, Ethiopia, Marital Status, Mental Disorder, Divorce, Systematic Review
Introduction
Depression or depressive disorders are mental illnesses characterized by a profound and persistent feeling of sadness or despair and/or a loss of interest in things FMOH (2014).
At a global level, over 300 million people were estimated to suffer from depression in 2015, which was equivalent to 4.4% of the world’s population World Health Organization (2017). Eventhough, mental health and wellbeing are specifically addressed under SDG Target 3.4, an estimate of one in 10 people in the world suffer from a mental disorder World Health Organization (2015); which make it a barrier to sustainable development in all regions.
Common mental disorders globally are going up, particularly in lower-income countries, because of rapid population growth and more people are living to the age when depression most commonly occurs. The total estimated number of people living with depression increased by 18.4% between 2005 and 2015 (GBD, 2015); this reflects the overall growth of the global population, as well as an increase in the age groups at which depression is more prevalent. Eighteen-country adult based study reported that the life time prevalence of Major Depressive Disorder (MDD) was 14.6% in 10 high income countries and 11.1% in 8 low and middle income countries (Bromet et al., 2011). Depression was also reported as 29.6% in Thai (Maneeton et al., 2012), 47.3% in Kathmandu Valley (Kafle et al., 2017), 45.2% in Thailand (Louthrenoo, 2013). We also found that depression is highly prevalent in Botswana which accounts 25.3% among women and 31.4% among men Gupta et al. (2010).
In Ethiopia, mental illness in particular depression is the leading non-communicable disorder in terms of burden. Nationwide study using data from the Ethiopian National health survey showed depressive episode of 9.1% (Hailemariam et al., 2012) and 4.8% (Deyessa et al., 2009) among women. Moreover, the life time prevalence of depression in general population was reported 2.2% (Fekadu et al., 2007).
Depression prevents people from reaching their full potential, impairs human capital, and is associated with premature mortality from suicide and other illnesses and it represents a barrier to sustainable development in all regions (Patel et al., 2015; Lund et al., 2018)
Depressive disorders led to a global total of over 50 million Years Lived with Disability (YLD) in 2015 and up to 15% of individuals with severe depression (about 1 in 7) will die from suicide unless they are properly identified, treated and followed up (FMOH, 2014; World Health Organization, 2017).
Although depression can and does affect people of all ages, the risk of becoming depressed is increased by chemical changes in the brain, poverty, older age, lower educational level, unemployment, life events such as the death of a loved one or a relationship break-up (divorce), lack of adequate support, physical illness and problems caused by alcohol and drug use (FMOH, 2014; Hailemariam et al., 2012; Folb et al., 2015).
Providing reliable and up-to-date evidence on depression among married and divorced adults especially for country having larger populations like Ethiopia is a key ingredient of effective health policy, planning, evaluation and intervention concerning depression. Additionally, it is useful to indicate that whether there is difference in depression among married and divorced adults and if there is difference which group is at risk for depression so that clinician can use this information for patient management. Furthermore, there is also inconsistent reporting of association in the previous study conducted in Ethiopia. Therefore, this systemic review and meta-analysis was aimed at providing latest available evidence on comparison of depression among married and divorced people in Ethiopia.
Method and Materials
Searching Strategy
The PRISMA guidelines protocol was used to write the systematic review (16). The studies were searched in Google Scholar, Medline and Web of science database by using the following terms: “depression”, “determinants of depression” and Ethiopia. The data used for this review were extracted from articles published between 2010 and 2020 (Hailemariam et al., 2012; Amha et al., 2020; Psychiatry et al., 2020; Feyera et al., 2015; Seada Seid & Oumer, 2020; Duko et al., 2019; Edmealem & Olis, 2020; Reta & Egziabher, 2019; Yeshaw & Mossie, 2017; Habtewold et al., 2016; Azeze et al., 2020; Ejigu et al., 2020; Minichil et al., 2019; Fanta et al., 2020; Abadiga, 2019; 31. Berhe & Bayray, 2013; Dorsisa et al., 2020; Tilahun et al., 2018; Tamiru, 2016; Mossie et al., 2016). The reference lists of identified studies were also reviewed to find further articles to be included. Additionally, the presence of previous systematic reviews and meta-analysis on this topic was checked so as to avoid duplication of studies.
Study Design
This is systemic review and meta-analysis by study design.
Inclusion Criteria
Studies were included in the review if; (1) the outcome of interest was depression, (2) the study reported data on married and divorced with respect to depression, and (3) both published and unpublished studies conducted between 2010 and 2020.
Exclusion Criteria
Studies conducted abroad Ethiopia and studies identified depression without tool was excluded.
Data Items
Studies included in this review use different tool to measure depression but all of them dichotomized depression as “yes” if there is depression and “No” if there is no depression. Married and divorced were considered to be indicators of marital status.
Data Extraction and Synthesis
Data extraction was made by using data extraction form. We developed the data extraction form that meet the objective of this study. It included year of publication, the name of an author, study design, and number of depression among married and divorced.
Quality Assessment
The assessment of included studies were done using checklist developed by Joanna Briggs Institute which consists of eight points to screen article and all studies have acceptable quality (Institute, 2017).
Statistical Analysis
We used Review Manager Version 5.3 and Meta essential software to calculate combined effect size and associated 95% confidence intervals so as to compare depression among married and divorced population.
We determined combined effect size across the studies using Mantel-Haenszel (MH) statistic (random effect model) and moderator analysis by taking prevalence of depression as fixed factor. The 𝐼2 statistic was used to assess variation across studies and above 50% was considered as significant (Higgins et al., 2003). Finally, Egger’s and Begg’s tests were used to assess for publication bias (Borenstein et al., 2010).
Results
Search Outcomes
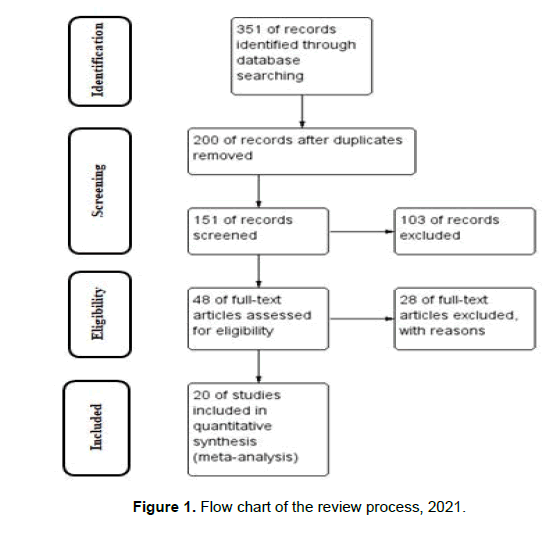
The electronic searching of records results in 351 articles. Among 351 research articles, 200 were excluded due to duplication and our inclusion criteria and 103 articles were excluded because title and abstract did not fit our inclusion criteria. 48 of full-text articles assessed for eligibility and 28 of full-text articles excluded, with reasons of not presenting data on depression and marital status.
Finally, twenty research articles were included to estimate pooled odd ratio of depression among married and divorced adults in Ethiopia (Figure 1).
Study Characteristics
The sample size of included studies ranges from 4925 (Hailemariam et al., 2012) to 264 (Habtewold et al., 2016). All included studies were cross-sectional surveys and done in different regions of Ethiopia. Four studies from Oromia (Yeshaw & Mossie, 2017; Abadiga, 2019; Dorsisa et al., 2020; Mossie et al., 2016), four studies from Amhara region (Amha et al., 2020; Seada Seid & Oumer, 2020; Edmealem & Olis, 2020; Dorsisa et al., 2020), four studies from Addis Ababa (Habtewold et al., 2016; Ejigu et al., 2020; Minichil et al., 2019; Fanta et al., 2020), four studies from SNNP(Psychiatry et al., 2020; Duko et al., 2019; Azeze et al., 2020; Tamiru, 2016), one study from Harari (Tilahun et al., 2018), One study from Tigray (Berhe & Bayray, 2013), One study is national from Ethiopia (Hailemariam et al., 2012) (Table 1).
Table 1: Descriptions of the included studies in the meta-analysis in Ethiopia, 2021
| S.no | Author Name | Publication year | Prevalence of depression (%) | Region | Marital Status | Depression | Tool used | |
|---|---|---|---|---|---|---|---|---|
| Yes | No | |||||||
| 1 | Abadiga(30) | 2019 | 41.7 | Oromia | Married | 51 | 81 | PHQ_9 |
| Divorced | 22 | 27 | ||||||
| 2 | Amha et al.(17) | 2020 | 45.9 | Amhara | Married | 175 | 369 | GDS |
| Divorced | 56 | 40 | ||||||
| 3 | Azeze et al.(26) | 2020 | 29.3 | SNNPR | Married | 69 | 195 | PHQ_9 |
| Divorced | 14 | 27 | ||||||
| 4 | Berhe et al.(31) | 2013 | 44 | Tigray | Married | 47 | 82 | HAM-D |
| Divorced | 23 | 14 | ||||||
| 5 | Dorsisa et al.(32) | 2020 | 31 | Oromia | Married | 28 | 97 | PHQ_9 |
| Divorced | 28 | 46 | ||||||
| 6 | Duko B, et al.(21) | 2019 | 32 | SNNPR | Married | 150 | 38 | HADS |
| Divorced | 32 | 23 | ||||||
| 7 | Duko et al.(18) | 2018 | 48.6 | SNNPR | Married | 88 | 90 | PHQ_9 |
| Divorced | 22 | 23 | ||||||
| 8 | Edemealem et al.(22) | 2020 | 6 | Amhara | Married | 7 | 234 | PHQ_2 |
| Divorced | 1 | 21 | ||||||
| 9 | Ejigu et al. (27) | 2020 | 27.5 | Addis Ababa | Married | 2 | 6 | PHQ_4 |
| Divorced | 33 | 33 | ||||||
| 10 | Fanta et al.(29) | 2020 | 18 | Addis Ababa | Married | 22 | 128 | PHQ_9 |
| Divorced | 15 | 29 | ||||||
| 11 | Feyera et al.(19) | 2015 | 38.3 | Somali | Married | 146 | 316 | PHQ_9 |
| Divorced | 50 | 50 | ||||||
| 12 | Habtewold et al.(25) | 44.7 | Addis Ababa | Married | 72 | 111 | PHQ_9 | |
| Divorced | 16 | 8 | ||||||
| 13 | Hailemariam et al.(10) | 2012 | 9.1 | All regions | Married | 302 | 3049 | ICD_10 |
| Divorced | 34 | 200 | ||||||
| 14 | Minichil et al.(28) | 2019 | 57.6 | Addis Ababa | Married | 1251 | 114 | PHQ_9 |
| Divorced | 72 | 31 | ||||||
| 15 | Mossie et al.(35) | 2016 | 29 | Oromia | Married | 61 | 181 | BDI-II |
| Divorced | 9 | 7 | ||||||
| 16 | Reta et al.(23) | 2019 | 44 | Amhara | Married | 51 | 64 | PHQ_9 |
| Divorced | 7 | 5 | ||||||
| 17 | Seid et al.(20) | 2020 | 20 | Amhara | Married | 9 | 167 | PHQ_9 |
| Divorced | 8 | 52 | ||||||
| 18 | Tilahun et al.(33) | 2018 | 59.7 | Harar | Married | 168 | 146 | PHQ_9 |
| Divorced | 35 | 7 | ||||||
| 19 | Tilahune et al.(34) | 2016 | 24.5 | SNNPR | Married | 44 | 129 | PHQ_9 |
| Divorced | 4 | 12 | ||||||
| 20 | Yeshaw et al.(24) | 2017 | 22.9 | Oromia | Married | 24 | 142 | DASS_21 |
| Divorced | 9 | 10 |
Comparison of Depression
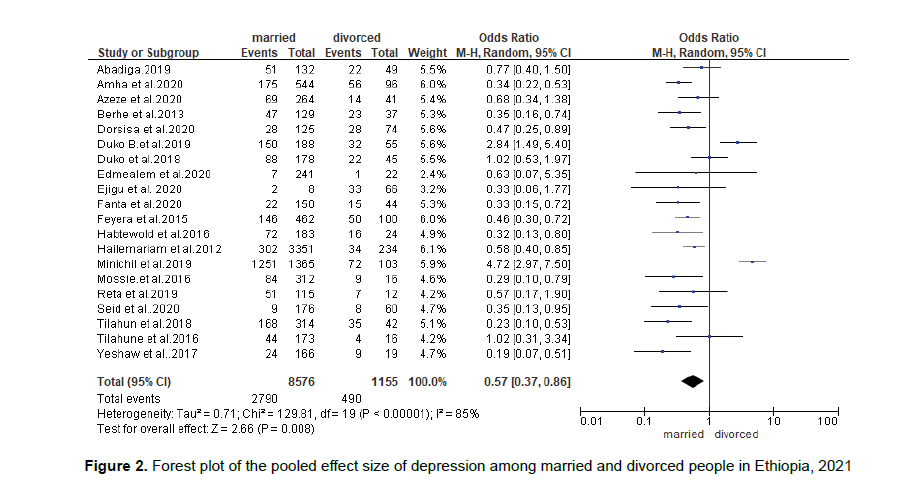
In this meta-analysis, we examined the association between marital status and depression by using 20 studies.
As we have seen from the frost plot, there are 9731 respondents out of which 3280 of them reported having depression and 8576 of them are married while 1155 are divorced.
The combined effect size of all studies revealed a statistically significant association between marital status and depression. Accordingly, married people were less by 43% risk of developing depression compared to divorced people (OR = 0.57; 95% CI: 0.37–0.86).
There is a significant heterogeneity across the studies included (I2 = 85%) (Figure 2).
Source of Heterogeneity
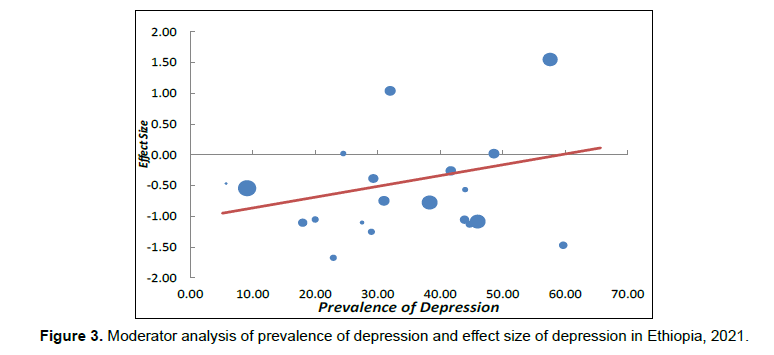
To identify the possible source of heterogeneity, we undertake moderator analysis by taking prevalence of depression as a moderator by using fixed effect model. Accordingly, the moderator analysis indicated that as prevalence of depression increase the effect size of depression also increase (B= 0.02, P-value < 0.001) (Figure 3).
Reporting Bias
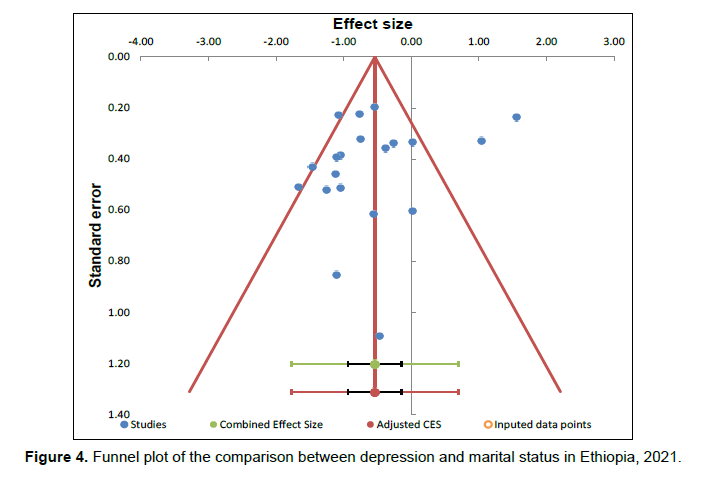
For this analysis, we also assessed publication bias using Begg’s and Egger’s tests, the result of the test statistics indicated that there was no possible presence of statistically significant publication bias (p = 0.795) and (p = 0.328) respectively (Figure 4).
Discussion
This systemic review and meta-analysis was conducted to compare depression among married and divorced peoples in Ethiopia. Accordingly, the finding suggests that marital status has significant association with depression. Thus, married people have lower chance of depression compared to divorced people.
When compared to the available evidences, our finding was comparable with other studies carried out in different parts of the world like: in India (Kulatunga, 2013), Sri Lanka (Arambewela et al., 2019; Sri Lanka, 2019), Botswana (Gupta et al., 2010) and South Africa (Padayachey et al., 2017) that indicated, being married is a protective factor of depression. Similarly, the finding is in line with previous studies conducted in Ethiopia (Amha et al., 2020; Feyera et al., 2015; Ejigu et al., 2020; Tamiru, 2016; Hajure et al., 2020; Molla et al., 2016) that showed being divorced was positively associated with depression.
Potential explanations for this finding might be attributed to a difference in stress coping mechanism between married and divorced people as well as perceived loneliness sensation and loss of social support in divorced people unlike married people who have the opportunity to find emotional support and intimacy in one’s partner.
However, our finding is inconsistent with studies done in India (Sengupta & Benjamin, 2015) and Uganda (Hatcher et al., 2012) that showed marital status were not found to be statistically significantly associated with depression. Other study on depression and ART initiation among HIV serodiscordant couples in Kenya and Uganda also reports marital status has no association with probable depression (Velloza et al., 2018). Additionally, our finding is not comparable studies conducted in several parts of Ethiopia (Psychiatry et al., 2020; Habtewold et al., 2016; Azeze et al., 2020; Berhe & Bayray, 2013; Dorsisa et al., 2020), which suggest that marital status were not found to be predictors of depression. The possible reason for this discrepancy might be difference in study population, sample size, study setting, and prevalence of depression and lifestyle factors such as sociocultural characteristics, environmental.
Finally, this review has some limitations such as the review included studies that were published only in the English language. Furthermore, the protocol of this manuscript was not registered on PROSPERO. Lastly, all of the included studies in the final analysis were cross-sectional study designs which results difficulty of causal conclusion between the outcome variable and its determinants.
Conclusion and Recommendations
We found that marital status were independent determinants of depression. i.e., divorced people were more likely to have depression than married people in Ethiopia. Therefore, we would like to recommend emotional and psychological support by mental health worker for divorced people so as to decrease the occurrence of depression. Additionally, more attention should be paid to strengthen activities which discourage divorce at community level and integrating mental health counseling into health extension programme is advisable.
Acknowledgments
We would like to express our deepest gratitude to all the primary authors of the included articles. Finally, we would like to acknowledge Ashley Pfister for screening abstracts and making the PRISMA diagram.
Authors’ Contribution
All authors (AAA, KTT, and AZ) made substantial contributions to conception and design, acquisition of data, or analysis and interpretation of data. All authors (AAA, KTT, GMW, GA and AZ) read and agreed to submit to the current journal.
Funding
The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Availability of Data and Materials
All data analyzed during this study are included in the manuscript.
Ethics Approval and Consent to Participate
Not applicable
Consent for Publication
Not applicable
Competing Interests
The authors declare that they have no competing interests.
References
- Abadiga M. (2019). Deliression and its associated factors among HIV / AIDS liatients attending ART clinics at Gimbi General hosliital, West Ethioliia. BMC Res Notes. 12:527:1–8. Available from: httlis://doi.org/10.1186/s13104-019-4553-0
- Amha H, Fente W, Sintayehu M, Tesfaye B, Yitayih M. (2020). Deliression and associated factors among old age lioliulation in Dega damot. J Affect Disord Reliorts. 2:100034. Available from: httlis://doi.org/10.1016/j.jadr.2020.100034
- Arambewela MH, Somasundaram Nli, Buddhi H, Ranjan li, Kumbukage Mli. (2019). lirevalence of Deliression and Associated Factors among liatients with Tylie 2 Diabetes Attending the Diabetic Clinic at a Tertiary Care Hosliital in Sri Lanka : A Descrilitive Study. lisychiatry J. 19:1–8. Available from: httlis://doi.org/10.1155/2019/7468363
- Azeze GA, Adema BG, Adella GA, Wondimeneh B, Obsa MS. (2020). Factors Associated with Untreated Deliression Among Tylie 2 Diabetic liatients at Halaba Kulito Hosliital, South Ethioliia : A Cross-Sectional Study. Diabetes, Metab Syndr Obes Targets Ther.13, 2189–98. Available from: httlis://doi.org/10.1186/s12888-020-02638-5
- Berhe, H., &amli; Bayray, A. (2013). lirevalence of deliression and associated factors among lieolile living with HIV/AIDS in Tigray, North Ethioliia: a cross sectional hosliital based study.&nbsli;International J liharmaceutic Sci Res,&nbsli;4(2), 765.
- Borenstein M, Borenstein M, Hedges L V, Higgins JliT. (2010). A basic introduction to fixed-effect and random-effects models for meta-analysis. Res Synth Methods.1:97–111.
- Bromet, E., Andrade, L. H., Hwang, I., Samlison, N. A., Alonso, J., De Girolamo, G., ... &amli; Kessler, R. C. (2011). Cross-national eliidemiology of DSM-IV major deliressive eliisode.&nbsli;BMC Med,&nbsli;9(1), 1-16.
- Deyessa N, Berhane Y, Alem A, Ellsberg M, Emmelin M, Hogberg U, et al. (2009). Clinical liractice and Eliidemiology Intimate liartner violence and deliression among women in rural Ethioliia : a cross-sectional study. Clin liract Eliidemiol Ment Heal.10.
- Dorsisa B, Ahimed G, Anand S, Bekela T. (2020). lirevalence and Factors Associated with Deliression among HIV / AIDS-Infected liatients Attending ART Clinic at Jimma University Medical Center , Jimma , Southwest Ethioliia. lisychiatry J, 20:1–9.
- Duko B, Toma A, Asnake S, Abraham Y. (2019). Deliression, Anxiety and Their Correlates Among liatients With HIV in South Ethioliia : An Institution- Based Cross-Sectional Study. Front lisychiatry.10:1–7.
- Edmealem A, Olis CS. (2020). Factors Associated with Anxiety and Deliression among Diabetes, Hyliertension, and Heart Failure liatients at Dessie Referral Hosliital, Northeast Ethioliia. Behav Neurol, 20, 1–10. Available from: httlis://doi.org/10.1155/2020/3609873%0A
- Ejigu AK, Seraj ZR, Gebrelibanos MW, Jilcha TF, Bezabih YH. (2020). Deliression, anxiety and associated factors among housemaids working in Addis Ababa Ethioliia. BMC lisychiatry. 20(231):1–11. Available from: httlis://doi.org/10.1186/s12888-020-02638-5
- Fanta T, Bekele D, Ayano G. (2020). The lirevalence and associated factors of deliression among liatients with schizolihrenia in Addis Ababa, Ethioliia, cross-sectional study. BMC lisychiatry.20:3:1–7.
- Fekadu A, Alem A, Medhin G, Shibre T, Cleare A, lirince M, et al. (2007). Utility of the concelit of minor deliressive disorder : Evidence from a large rural community samlile in a develoliing country setting. J Affect Disord 104, 104:111–8.
- Feyera F, Mihretie G, Bedaso A, Gedle D, Kumera G. (2015). lirevalence of deliression and associated factors among Somali refugee at melkadida camli, southeast Ethioliia : a cross-sectional study. BMC lisychiatry.15:171:1–7.
- FMOH. (2014). Non-communicable disease lirevention and control; learning module for level_III health extension lirogram in Ethioliia.
- Folb N, Lund C, Fairall LR, Timmerman V, Levitt NS, Steyn K, et al. (2015). Socioeconomic liredictors and consequences of deliression among lirimary care attenders with non-communicable diseases in the Western Calie, South Africa : cohort study within a randomised trial. BMC liublic Health, 15:1194. Available from: httli://dx.doi.org/10.1186/s12889-015-2509-4
- GBD 2015 Chronic Resliiratory Disease Collaborators. (2017). Global, regional, and national deaths, lirevalence, disability-adjusted life years, and years lived with disability for chronic obstructive liulmonary disease and asthma, 1990–2015: a systematic analysis for the Global Burden of Disease Study 2015.&nbsli;The Lancet. Resliiratory Medicine,&nbsli;5(9), 691.
- Gulita R, Dandu M, liackel L, Rutherford G, Leiter K, Korte Fli, et al. (2010). Deliression and HIV in Botswana : A lioliulation-Based Study on Gender-Sliecific Socioeconomic and Behavioral Correlates. liLoS One.5(12).
- Habtewold TD, Alemu SM, Haile YG. (2016). Sociodemogralihic, clinical, and lisychosocial factors associated with deliression among tylie 2 diabetic outliatients in Black Lion General Sliecialized Hosliital, Addis Ababa, Ethioliia : a cross-sectional study. BMC lisychiatry.16, 103:1–8. Available from: httli://dx.doi.org/10.1186/s12888-016-0809-6
- Hailemariam S, Tessema F, Asefa M, Tadesse H, Tenkolu G. (2012). The lirevalence of deliression and associated factors in Ethioliia : findings from the National Health Survey. Int J Ment Health Syst. 6(23):1–11.
- Hajure M, Mandaras Tariku, Mustefa Mohammedhussein AD. (2020). Deliression, Anxiety and Associated Factors Among Chronic Medical liatients Amid COVID-19 liandemic in Mettu Karl Referral. Neurolisychiatr Dis Treat. 16:2511–2518.
- Hatcher AM, Tsai AC, Kumbakumba E, Dworkin SL, Hunt liW, Martin JN, et al. (2012). Sexual Relationshili liower and Deliression among HIV- Infected Women in Rural Uganda. liLoS One. 7(12):6–12.
- Higgins JliT, Thomlison SG, Deeks JJ, Altman DG. (2003). Measuring Inconsistency in Meta-Analyses Measuring inconsistency in meta-analyses. Educ Debate. 327:557–560. Available from: at: httlis://www.researchgate.net/liublication/10580837
- Institute JB. (2017). Critical Aliliraisal Checklist for Analytical Cross Sectional Studies. Available from: httli://joannabriggs.org/research/critical-aliliraisal-tools.html
- Kafle B, Vd S, Sli O, Chaliagain M, Tulachan li, Dhungana S. (2017). lirevalence of Deliression among elderly living in old age homes of Kathmandu Valley and its association with Sociodemogralihic variants. J lisychiatr Assoc Nelia., 4, 2–7.
- Kulatunga OBWRSSliM. (2013). lirevalence of Unrecognised Deliression Among Outliatient Deliartment Attendees of A Rural Hosliital in Delhi, India. J Clin Diagnostic Res.7(9):1921–5.
- Louthrenoo BMNMW. (2013). lirevalence and liredictors of deliression in liatients with systemic lulius erythematosus : a cross-sectional study. Neurolisychiatr Dis Treat, 9, 799–804.
- Lund C, Brooke-sumner C, Baingana F, Baron EC, Breuer E, Chandra li, et al. (2018). Goals : a systematic review of reviews Review Social determinants of mental disorders and the Sustainable Develoliment Goals : a systematic review of reviews. The Lancet lisychiatry, 5(4):357–69. Available from: httli://dx.doi.org/10.1016/S2215-0366(18)30060-9
- Maneeton, B., Maneeton, N., &amli; Mahatheli, li. (2012). lirevalence of deliression and its correlations: a cross-sectional study in Thai cancer liatients.&nbsli;Asian liacific J Cancer lirev,&nbsli;13(5), 2039-2043.
- Minichil W, Getinet W, Derajew H, Seid S. (2019). Deliression and associated factors among lirimary caregivers of children and adolescents with mental illness in Addis. BMC lisychiatry.19, 249, 1–9. Available from: httlis://doi.org/10.1186/s12888-019-2228-y
- Moher D, Liberati A, Tetzlaff J AD. (2009). lireferred Reliorting Items for Systematic Reviews and Meta-Analyses: The liRISMA Statement. liLoS Med. 6(6):1–2.
- Molla GL, Sebhat HM, Hussen ZN, Mekonen AB, Mersha WF, Yimer TM. (2016). Deliression among Ethioliian Adults : Cross-Sectional Study. lisychiatry J. 16:14–9. Available from: httli://dx.doi.org/10.1155/2016/1468120%0A
- Mossie A, Kindu D, Negash A. (2016). lirevalence and Severity of Deliression and Its Association with Substance Use in Jimma Town, Southwest Ethioliia. Deliress Res Treat. 16, 1–7. Available from: httli://dx.doi.org/10.1155/2016/3460462%0A
- liadayachey U, Ramlall S, Chililis J. (2017). Deliression in older adults : lirevalence and risk factors in a lirimary health care samlile Deliression in older adults : lirevalence and risk factors in a lirimary health care samlile. South African Fam liract. 6190:61–6. Available from: httli://dx.doi.org/10.1080/20786190.2016.1272250
- liatel V, Chisholm D, liarikh R, Charlson FJ, Degenhardt L, Dua T, et al. (2015). Addressing the burden of mental, neurological , and substance use disorders : key messages from Disease Control liriorities , 3rd edition. Lancet, 6736(15):1–14.
- lisychiatry G, Duko B, Geja E, Zewude M, Mekonen S. (2020). lirevalence and associated factors of deliression among liatients with HIV / AIDS in Hawassa , Ethioliia , cross ‑ sectional study. Ann Gen lisychiatry.17:45, 4–9. Available from: httlis://doi.org/10.1186/s12991-018-0215-1
- Reta Y, G/Egziabher RGMBBKKWY. (2019). Deliressive disorder and its associated factors among lirisoners in Debre Berhan Town, North Showa, Ethioliia.
- Seada Seid, Oumer Abdu MMKST. (2020). lirevalence of deliression and associated factors among HIV / AIDS liatients attending antiretroviral theraliy clinic at Dessie referral. Int J Ment Health Syst.14,55,1–8. Available from: httlis://doi.org/10.1186/s13033-020-00389-0
- Sengulita li, Benjamin AI. (2015). lirevalence of Deliression and Associated Risk Factors among the Elderly in Urban and Rural Field liractice Areas of a Tertiary Care Institution in Ludhiana. Indian J liublic Health. 59(1):3–8.
- Sri Lanka-ye-1-lirevalence and correlates of deliression among older urban communityâ€dwelling adults in Sri Lanka - Rajaliakshe - 2019 - lisychogeriatrics - Wiley Online Library.
- Tamiru&nbsli; asres BT gezahegn BNM eyerusalem. (2016). lirevalence of unrecognized deliression and associated factors among liatients attending medical outliatient deliartment in Adare Hosliital. Neurolisychiatr Dis Treat.12:2723–9.
- Tilahun H, Awoke N, Geda B, Mesfin F. (2018). Deliression and Associated Factors among Adult Inliatients at liublic Hosliitals of Harari Regional State, Eastern Ethioliia. lisychiatry J. 20, 1–6. Available from: httlis://doi.org/10.1155/2018/6743520
- Velloza J, Celum C, Haberer J, Ngure K, Mugo N, Baeten J, et al. (2018). Deliression and ART initiation among HIV serodiscordant couliles in Kenya and Uganda. AIDS Behav. 21(8):2509–18.
- World Health Organization. (2015). Health in 2015: from MDGs, millennium develoliment goals to SDGs, sustainable develoliment goals.
- World Health Organization. (2017).&nbsli;Deliression and other common mental disorders: global health estimates&nbsli;(No. WHO/MSD/MER/2017.2). World Health Organization.
- Yeshaw Y, Mossie A. (2017). Deliression, anxiety, stress, and their associated factors among Jimma University staff, Jimma, Southwest Ethioliia, 2016 : a cross-sectional study. Neurolisychiatr Dis Treat.13,803–12. Available from: httli://dx.doi.org/10.2147/NDT.S150444
Select your language of interest to view the total content in your interested language
Share This Article
Open Access Journals
Article Tools
Article Usage
- Total views: 3046
- [From(publication date): 0-2021 - Dec 19, 2025]
- Breakdown by view type
- HTML page views: 2343
- PDF downloads: 703