Comparison between the Significant of Antenatal Pelvic Floor Exercises and Non-Intervention in Preventing Urinary Incontinence: A Systematic Literature Review
Received: 26-Oct-2017 / Accepted Date: 03-Nov-2017 / Published Date: 04-Nov-2017 DOI: 10.4172/2165-7025.1000369
Abstract
Background: Urinary incontinence is a common symptom observed in modern times, which may affect 7-37% of women aged 20-39 and 9-39% after the age of 60. Pregnancy and natural delivery are important risk factors increasing the likelihood of incontinence. Conservative intervention such as pelvic floor muscle training (PFMT) is superior in preventing and treating urinary incontinence.
Purpose: In the current systematic review we evaluated 10 randomized control study that present the impact of pelvic floor muscle training on the occurrence and intensity of urine leakage in women in four different periods: during pregnancy, until 8 weeks postpartum, up to three to 12 months, and up to 6-8 years after child birth. In addition, we presented the best available evidence for the efficacy and effectiveness of antenatal pelvic floor muscle training in preventing and treating the urinary incontinence rather than non-intervention.
Data source: PubMed, Cochrane library, BMJ Group, BioMed Central, Wiley online library.
Study selection: 10 randomized, control trials (RCTs) published in English from 2001-2016.
Data extraction: Incontinence due to other causes other than childbirth.
Data synthesis: The study focus on pelvic floor exercise versus non-intervention for the antenatal women, incontinence must be as a result of childbirth, and randomized control study.
Limitation of the study: The reviewed studies are limited to 10 randomized control trials.
Conclusion: There is significant evidence that pelvic floor muscle training (PFMT) is superior in preventing and treating urinary incontinence as compared to non-intervention.
Keywords: Antenatal pelvic floor exercise; Non-intervention; Urinary incontinence; Pelvic floor exercise training
Introduction
Urinary incontinence as defined by the International Continence Society is the complain of any involuntary leakage of urine [1-3]. The world Health Organization (WHO) has classified UI as one of the ten major health problems of present times among women [4]. Causes of UI can be divided into: dysfunction of the bladder or urethra, and neurological or gynecological causes. Gynecological components include: the weakening of pelvic floor muscles, gynecological and obstetrical operations and pelvic organ prolapse [5]. Existing evidence indicates that both natural delivery, as well as the pregnancy itself [6] has a prominent impact on the functioning of pelvic floor muscles and the occurrence of urinary incontinence. SUI occurs when intra-vesical pressure exceeds urethral closure pressure in the absence of a detrusor contraction. SUI may be due to bladder neck hyper-mobility or poor urethral closure pressure [7]. The pelvic floor muscles (PFM) function to elevate the bladder, preventing descent of the bladder neck during rises in intra-abdominal pressure and to occlude the urethra. The theoretical basis for physical therapy to treat SUI is to improve PFM function by increasing strength, coordination, speed and endurance [5] in order to maintain an elevated position of bladder neck during raised intra-abdominal pressure with adequate urethral closure force [8]. Since 1992, conservative management of SUI has been promoted by the US Department of Health and Human Services (AHCPER) as first –line treatment for SUI for its efficacy, low cost and low risk [9].
According to Boyle [10], up to a third of women have urinary incontinence while about a 10th of them have stool incontinence after delivery. Urinary incontinence is a major clinical problem with profound effects on the quality of life and day-to-day activities of the affected women. It’s physically debilitating and socially incapacitating, with loss of self-confidence, helplessness, depression and anxiety all related to its occurrence. Affected women suffer social stigma and are withdrawn socially. As a result their productivity is significantly reduced and may lose interest in life.
Chiarelli P [11] indicates that the prevalence of urinary incontinence among women increases during young adult life: a study with over 40000 women estimated a prevalence of 12.8% in women aged 18-22 years, 36.1% in women aged 40-49, and 35% in women aged 70-74 years.
The severity of urinary incontinence varies in severity ranging from mild, moderate to severe forms. These levels of incontinence require different approaches in management in terms of duration and intensity. Epidemiological studies have shown an association between more severe forms of urinary incontinence and assisted vaginal deliveries or birth of high birth weight neonates which suggest the potential for an intervention promoting continence that is targeted at women who have just given birth [4].
According to the National Association for Continence (NAFC), pelvic floor exercises (PFEs) or pelvic floor muscle training (PFMT), also called Kegel exercises, are essential parts of behavioral treatment techniques that help increase bladder control and decrease bladder leakage. Though the technique requires conscious effort, consistent discipline, and a lifetime commitment, PFEs have been shown to improve mild to moderate urge and stress incontinence. When performed regularly and correctly, they strengthen bladder support, and build control and endurance to help improve, regain and maintain bladder and bowel control.
As such, health workers usually recommend pelvic floor exercise both during pregnancy and after childbirth. This aims at both preventing and treating fecal and urinary incontinence. Physiotherapists train expectant women who are expected to undertake the exercise several times a day in order to strengthen her pelvic floor muscles. This review will summarize the recent published data on the use of pelvic floor muscle training in preventing and treating urinary incontinence in prepost- natal women.
Methodology
Data source
The studies identified from PubMed, Cochrane library, BMJ Group, Biomed Central, Wiley online library, and manual search of reference lists from systematic reviews and the proceedings of the International Continence Society (available at www.annals.org).
Study selection
One investigator independently decided on study eligibility according to recommendations from the Scottish intercollegiate Guideline developer handbook for systematic reviews of interventions to include original publications of randomized controlled trials (RCTs) that were published in English form from 2001- March 2016. Full texts of the RCTs that examined the effects of pelvic floor muscle training on urinary incontinence in pre-post-natal.
The study excluded secondary data analysis, case reports, case series, and RCTs that did not report patient outcomes.
Assessment of methodological quality
The quality of study was analyzed by using the following criteria: participant selection, length and loss of follow-up, use of intentionto- treat principle, masking of the treatment status, randomization scheme, adequacy of randomization and allocation concealment, and justification of sample size. Several strategies were used to reduce bias, including a comprehensive literature search for published evidence in several databases, a search of reference lists of systematic reviews and proceeding of the International Continence Society. The quality of the selected studies was assessed using a standard grading system, as Scottish Intercollegiate guideline network (SIGN, 2012). Evidence table can be found at Appendix 1 &2.
Since the methodological quality was dependent the trial reports contained in the selected studies, this assessment might have been influenced by the quality of the corresponding reports. In some cases, it was disappointing that some studies did not sufficiently describe the randomization process. Thus, it was difficult to ascertain whether there was sufficient concealment. Regardless, it was encouraging that more than two-thirds of the selected studies used blinded outcomes inspectors, given the trouble of blinding treatment providers and participants to PFMT. Overall, the share of withdrawals and dropout was between 0% and 20%, which provides for a desirable methodological quality. Sample sizes for most of the studies were small to moderate. This means that the selected studies used methodologies that are relatively easy to apply. Also, as expected of small sample studies, they provided a significantly accurate representation of the larger population [12]. This aspect of the selected studies ensured a high methodological quality for this study.
Methodological quality was also affected by the age of the selected studies. The more recent studies, for instance, considering the trial reports, tended to be less likely to be biased as compared to the older ones. Of all the selected studies, those that were found to be more likely to be biased recorded the largest treatment effect as compared to the studies which were found to be less likely to be biased. This affected the methodological quality since it represents a possible overestimation of treatment effect. It is also important to note that this trend was particularly observed in the selected studies with insufficient concealment of random allocation.
Also, the methodological quality would be higher if the testers who carried out the outcomes of incontinence study would have carefully chosen a primary outcome measure that was relevant to women, selected secondary methods to include a range of domains, and chose standardized tools with recognized responsiveness, reliability, and validity.
Data synthesis
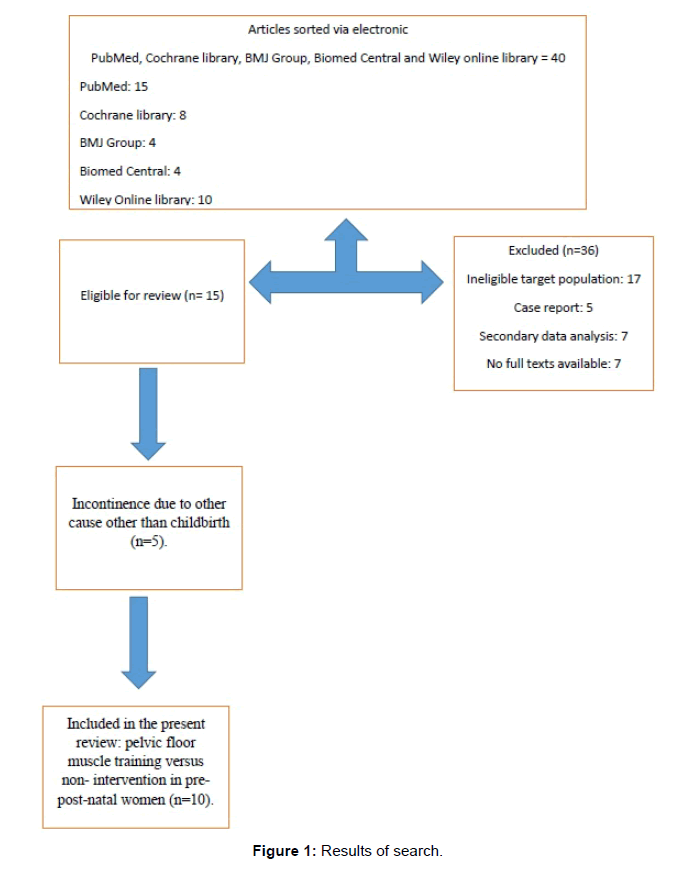
Forty one articles were selected from electronic bibliographies and screened for retrieval (n=41). Thirty sex articles were excluded for not meeting the selection criteria (n=36) such as ineligible target population or case report or secondary data analysis, or no full texts available. The resultant was fifteen randomized control trials full articles (n=15). Five articles were exempted for not meeting the inclusion criteria (n=5) such as incontinence due to other cause other than childbirth. The ten most appropriate articles were left (n=10) (Figure 1).
Summaries of the studies included in the review are provided in Table 1. Studies are presented the information about the level of evidence; population, interventions investigated, outcome measures and information of determine the generalizability of the study findings.
| Bibliographic citation | Study type & Evi. Lev | Population | Intervention/ comparison | Follow-up time | Outcome measures | Effect size |
|---|---|---|---|---|---|---|
| Aqur, et al. [10]: The long-term effectiveness of antenatal pelvic floor muscle training; 8-year follow up of a randomized controlled trial. Published in British journal of Obstetrics and gynaecology 2008 July | RCTs ++ | Participant in RCT of antenatal PFMT 8years previously. 170 out of the 230 women responded | 68.4% reported continuing with PFMT exercise as taught. Versus 31.6% stopped PFMT | 8 years | Directly asking about the presence of stress urinary incontinence (SUI) and quality of life | The significant improvement in postnatal SUI originally shown in the PFMT compared with controls (19.2% versus 32.7%, P=0.02) at 3 months was not evident 8 years later (35.4 % versus 38.8%, P=0.7). |
| General Comments: The study design is good but there is no proof that the women actually continued with PFMT as trained. The study findings can be generalized to the pregnant population. The study gives verified figures with confidence intervals and significant P-Values. | ||||||
| Boyle, et al. [11] Pelvic floor muscle training for prevention and treatment of urinary and fecal incontinence in antenatal and postnatal women. | RCTs + | 8485 women (4231 on PFMT, 4254 control) | Pelvic floor muscle training(PFMT), versus Non-intervention (usual antenatal or postnatal care) | 12 months | Presence, reduction or absence of urinary incontinence | Pregnant women without UI on PFMT were less likely to report UI up to six months after delivery (30% less, risk ratio (RR) 0.71, 95% CI 0.58 to 0.95, combined results of 5 studies) than non-intervention . Postnatal women with UI 3 months after delivery on PFMT, 40% were less likely to report UI 12 months after delivery (RR0.60 , 95%CI, 0.35 to 1.03. combined results of 3 trials) as compared to non- intervention. |
| General Comments: The study is good designed. There is improved function with intervention on postnatal women. There is treatment integrity and inter observer agreement. Results in scientific terms with P-Value and confidence intervals well evaluated. It can be generalized on the pregnant population. | ||||||
| Glazener, et al. [13] RCT of conservative management of postnatal urinary and fecal incontinence: six year follow up | RCTs + | 747 women with urinary incontinence, 516 (69%) followed up for 6years | Active conservative treatment (PFMT) at 5, 7 and 9 months after delivery versus Standard postnatal care | 6 years | Presence, reduction or absence of Urinary and faecal incontinence, performance of PFMT | At 1 year, UI improvement, 60% versus 69% controls, faecal incontinence 4% versus 11% control. At 6 years 76% versus 79%, (95% CI for difference in means- 10.2% to 4.1%) for UI. (12%vs 13%, -6.4% to 5.1%) for faecal incontinence irrespective of subsequent obstetric event. |
| General Comments: Study Design is good. But there is no proof that the women actually will continue with PFMT. Results in scientific terms with P-Value and confidence intervals well evaluated. Can be generalized to the pregnant population. | ||||||
| Glazener, et al. [3] Conservative management of persistent postnatal urinary and faecal incontinence | RCT + | 747 women with urinary incontinence 3 months postnatal. 371 randomly allocated to intervention, 376 to control. | Reinforcement of pelvic floor muscle training by exercise at 5, 7 and 9 months after delivery supplemented with bladder training where appropriate at 7 and 9 months. Versus Standard postnatal care for the control | 9 months | Primary; persistence and severity of urinary incontinence 12 month postnatal. Secondar; change in co-existing fecal incontinence, Use of pads per day, rating of UI severity with visual analogue scale wellbeing, anxiety, depression and performance of pelvic floor exercise. | Women on PFMT had significantly less UI (59.9%) versus 69%, a difference of 9.1% (95% CI 1% to 17.3%, P=0.037) for any incontinence. Severe incontinence, 19.7% versus 31.8%, a difference of 12.1% (4.7% to 19.6%,P=0.002). fecal Incontinence was also less common, 4.4% versus 10.5% Difference of 6.1% (6.1% To 10.8%, P=0.012. At 12 months women in intervention group were more likely to be performing PFMT (79%) versus (48%) P<0.001 visual analogue scale, wellbeing, anxiety, depression and performance of pelvic floor exercise. incontinence was also less common, 4.4% versus 10.5% difference of 6.1% (6.1% to 10.8%, P=0.012. At 12 months, women in intervention group were more likely to be performing PFMT (79%) versus (48%), P<0.001 |
| General Comments: the study design is good; there is treatment integrity, results in scientific terms with P-Value and confidence intervals well evaluated. Can be generalized for the pre-pot-natal population as the sample is representative and intervention inexpensive. | ||||||
| Hatice Kahyaoglu, et al. [14] Effect of pelvic floor muscle exercise on pelvic floor muscle activity and voiding functions during pregnancy and postpartum period. | RCT + | 60 pregnant women. 30 women on PFMT, 30 women on control group. | PFMT versus no PFMT | 28 Weeks, 36-38 of pregnancy, and postpartum weeks 6-8. | Urinary Distress Inventory (UDI-6), Incontinence Impact Questionnaires (IIQ-7), The Overactive Bladder Questionnaires (OBQ-q). Voiding function were measured using uroflowmetry and three day voiding diaries. Using perineometry device to measure muscle power of the pelvic | Pelvic floor muscle strength improved in the training group compared to the control group (P<0.001). The UDI-6 and OAB-q scores did not change during week 36-38 of pregnancy. UDI-6 and OAB-q scores were improved during postpartum weeks 6-8 (P<0.05). Voiding Functions Were negatively affected in both groups, decreasing during weeks 36-38 of pregnancy and improving during the postpartum period. visual analogue scale, wellbeing, anxiety, depression and performance of pelvic floor exercise. incontinence was also less common, 4.4% versus 10.5% difference of 6.1% (6.1% to 10.8%, P=0.012. At 12 months, women in intervention group were more likely to be performing PFMT (79%) versus (48%), P<0.001 |
| General Comments: the study design is good; there is treatment integrity, results in scientific terms with P-Value and confidence intervals well evaluated. The outcome measurements are excellent and validated. Can be generalized for the pre-pot-natal population as the sample is representative and intervention inexpensive. | ||||||
| Hay-Smith, et al. [15] Pelvic floor muscle training for prevention and treatment of urinary and fecal incontinence in antenatal and postnatal women. Cochrane database System review 2008 October | RCTs ++ | 6181 women pregnant and postnatal women (3040 PFMT, 3114 Controls) | PFMT versus No PFMT, usual antenatal care | 12 months | Primary self-reported Urinary and fecal incontinence Secondary QOL Questionnaires, Symptoms of severity. | Women without UI at baseline, PFMT reduced UI in late pregnancy >34 weeks by 56% (RR 0.44, 95% CI 0.3 to 0.65) and 30% less up to 6months postpartum and mid- postpartum (RR 0.71,95% CI 0.52 to 0.97) Postnatal women with UI 3months post-delivery, on PFMT reported 20% UI 12 months after Delivery (RR 0.79, 95% CI 0.70 to 0.90) |
| General Comments: The study invalid as the result of improvements were made by subjective observation, the results are applicable since the study is randomized, and subject are women with incontinence after delivery. It can be generalized to pre-post-natal women population. | ||||||
| Ko, et al. [16] A randomized controlled trial of antenatal pelvic floor exercises to prevent and treat urinary incontinence | RCTs ++ | 300 pregnant women | 200 women were randomly assigned PFMT The remaining 100 were non-intervention group (usual antenatal care | Up to 6 months postpartum | Measured by Urogenital Distress Inventory-6 (UDI-6), Incontinence Impact Questionaire-7(IIQ-7), and self-reporting. | During late pregnancy and postpartum period, PFMT Exercise group had significantly lower total UDI-6 and IIQ-7 scores. Self-report rate of urinary incontinence was also less than in control. |
| General Comments: The study is strongly designed, but no indication of treatment integrity. Results collected by standard scientific tool so no bias, but no numerical values. The result could be generalized for pre-pot-natal population. It consistent with PFMT reduces UI. | ||||||
| Morkved, et al. [17] Pelvic floor muscle training during pregnancy to prevent urinary incontinence: a single-blind randomized controlled trial. Obstetric gynecol. 2003 Feb. 101 (2): 313-9 | RCTs + | 301 healthy nulliparous women(148 intevention,153 control) | 12 week intensive PFMT during pregnancy Versus Customary information | Up to 3 months postnatal | Primary-self reported UI Secondary-pelvic floor muscle strength | 32% of training group reported UI compared to 48% control at 36 weeks gestation (P=0.007), and 20% versus 32% 3months after delivery (P=0.018). Strength of Pelvic floor muscle was significantly higher in training group at 36 weeks (p=0.008) and 3 months after delivery (P=0.048) |
| General Comments: good quality with internal validity, there is treatment integrity, results in scientific terms with P-Value and confidence intervals well evaluated. Applicable to the pre-post –natal population. | ||||||
| Reilly, et al. [18] Prevention of postpartum stress incontinence in primigravidae with increased bladder neck mobility | RCTs ++ | 268 primigravidaat 20weeks gestation. Median age 28years (16 to 47 years) | 139 on supervised pelvic floor exercises monthly from 20 wks to birth Versus Non-intervention (usual antenatal care) | 20 weeks gestation to 3 months postpartum | Subjective reporting of stress incontinence 3 months postpartum. Pelvic floor strength, using perineometry, and bladder neck mobility measured by perinea ultrasound. | 19.2% of women in the supervised pelvic floor exercise had postpartum stress incontinence, compared with 32.7% in the non-intervention (control) group.(RR 0.59 {0.37 -0.92}) |
| General Comments: the study is good quality, there is treatment integrity and the sample is randomized. There is no bias in the outcome measure it is standardized. The group on PFMT significantly improved as compared to untreated group. The result can be generalized to pre-post-natal population. | ||||||
| Stafne, et al. [19] Does regular exercise including pelvic floor muscle training prevent urinary incontinence during pregnancy? | RCTs + | 855 pregnant women between 20 and 36 weeks | Intervention was a 12-week exercise program including PMFT. One weekly Versus Controls received normal antenatal care | From 20 weeks’ gestation to 36 weeks’ gestation | Self-reported urinary and fecal incontinence after intervention period (at 32-36 weeks gestation). | 11% of the women in the intervention reported any weekly urinary incontinence compared to 19% of the non-intervention group (P=0.004). 3% of women in the intervention reported fecal incontinence versus 5% in non-intervention. |
| General Comments: the study is high quality with interval validity, but the study is in doubt as it does not show the outcomes that were as a result of PFMT. There is treatment integrity and the study method is valid with P-Value indicated. The result can be generalized to the pre-pot-natal population. | ||||||
Table 1: Best evidence. Evidence table (Mackway, et al. nd.)
Ten RCTs (n=10) were included. All studies reported adequacy of randomization, discussed participant selection, length and loss of follow up, use of intention-to-treat principle, and masking of the treatment status for both subjects and investigators. Seven RCTs reported adequate allocation concealment. There are marked heterogeneity in the type and intensity of interventions in both groups. All the studies used validated measurement tools.
One RCT (n=170) reported significant improvement in postnatal urinary incontinence, who participated in the PFMT compared with control group (19.2% versus 32.7% P=0.02), but no statistically significant effect at 3 months and they found significant difference between the groups at 8 years 35.8% versus 38.8% (P=0.7).
Second RCT (n=8485) reported a statistically significant reduction in sever incontinence in the intervention group at 12 months after delivery (response rate, RR 0.60, 95% confidence interval, CI: 0.35 to 1.03). The third RCT (n=747) found a statistically significant improvement in urinary incontinence in the intervention group 60%versus 69% control group at one year follow –up, and fecal incontinence 4% versus 11% control group. With significant ongoing difference over 6 years followup 76%versus 79% (95% CI: 10.2% to 4.1% for urinary incontinence, 12% versus 13%- 6.4% to 5.1%for fecal incontinence).
The fourth RCT reported statistically significant reduction in urinary incontinence by 59.9%in the intervention group versus 69% control group (95% CI: 1% to 1.7% P=0.037). Fecal incontinence in the intervention group improved by 19.7% versus 31.8% control group (4.7% to 19.6% P=0.002). The fifth RCT (n=6181), which reported a statistically significant reduction in incontinence in the intervention group at 34 weeks of pregnancy (RR0.44, 95%, CI: 0.52 to 0.97), and 20% less up to 12 months postnatal (RR 0.79, 95% CI: 0.70 to 0.90).
The fifth RCT (n=60) reported a decrease in UDI-6 and OAB-q scores in intervention group versus the control group during postpartum weeks 6-8 (P<0.05). Voiding functions were decreased during weeks 36-38 of pregnancy and improving during the postpartum period. And the pelvic floor muscle strength improved in the training group versus the control group.
The seventh RCT (n=300) reported a decrease in UDI-6 and IIQ- 7 scores in intervention group versus the control group. The seventh RCT (n=301) reported 32% of training group had urinary incontinence compared to 48% control group at 36 weeks of pregnancy (P=0.007) and 20% versus 32% at 3 months after delivery (P=0.018).
The ninth RCT (n=268) reported 19.2% of women in the supervised pelvic floor exercise had post-natal stress incontinence compared to 32.7% in the non-intervention group (RR0.59 “0.37-0.92”). The ninth RCT (n=855) reported that 11% of the women in the intervention group had urinary incontinence versus 19% of control group (P=0.004), and 3% had fecal incontinence in the intervention group versus to 5% in the control group.
Discussion
This systematic review reports the evidence of PFMT intervention in the treatment and prevention of urinary incontinence in pre-postnatal women from full text studies published in English during the last 15 years. The quality of most of the RCTs was good; participants were not excluded from the analysis of outcomes, and randomized was adequate. However, allocation concealment was not addressed in three studies. Variations in outcome measures rather than RCT quality resulted in heterogeneity between studies.
Despite extensive efforts to standardize outcome assessment for urinary incontinence [4]. The included RCTs measured a variety of outcomes, including adherence to PFMT, self-reported symptoms, signs, and improvement; severity of urinary/ fecal incontinence as assessed by pad number/day, voiding functions were measured, and conditionspecific quality of life. The measurement of outcomes was inconsistent across the studies. Another factor which may influence outcome is the degree to which subjects actually comply with the treatment program prescribed and adhered to the PFMT. Subject compliance or adherence was infrequently and generally poorly reported with no standardized, validated or reliable approach to its assessment.
The following is a summary of the discussion regarding the overall completeness and applicability of evidence in the selected studies.
Outcomes measures and reporting
Some of the studies did not provide data in ways that could apply to meta-analysis or did not provide data for any of the pre-indicated outcomes of interests. Some challenges include reporting a measure of central tendency and leaving out a measure of dispersion, and inaccurate values for P without additional supporting information [5]. In the end, there was an overall lack of consistency in the most of the outcomes measures applied and reported in the selected studies. In other words, there were no particular outcomes that were shared among the trials, while at the same time, similar outcomes were measured and recorded in various ways [2]. Also, there was no validity and reliability testing conducted for some of the continence outcomes. As a result, it was difficult to carry out adequate comparisons between studies.
Most of the selected studies reported adverse effects of other approaches and only a few gave such a report for PFMT. In fact, the only adverse effect associated with PFMT was discomfort with training, which can be reversed by simply stopping the training programme [13-16]. Even though randomized trials are not the most suitable means of addressing safety, none of the selected studies suggest that PFMT is likely to be harmful.
Implications for practice
The findings of the selected studies suggest that PFMT brings about better outcomes as compared to non-treatment and other inactive treatment for treating urinary incontinence. In the cases where PFMT was used, the women were more likely to experience improvement or get cured entirely [5,16]. These women also reported fewer leakage episodes per day, better quality of life, and have less urine leakage on short pad tests as compared to non-treatment.
Most of the selected studies imply that treatment, especially in self-reported cases, has a greater impact for women with urinary incontinence taking part in a closely monitored PFMT programme for no less than three months [5]. Additionally, age does not matter can, therefore, not reduce the effect of treatment in urinary incontinent women in trials; the outcomes for older women were similar to those of younger women.
The selected studies imply suggest that the treatment effect is magnified if the PFMT programme is focused on valid psychological principles. For a successful programme, the right contraction has to be confirmed and recorded before the training, and the participants are monitored and supported to continue with the programme [7,13]. There is an overall widespread endorsement among the selected studies that PFMT should be integrated into the first line conservative management programmes for women with urinary incontinence.
However, most of the selected studies lack follow up past the completion of the treatment programme. Therefore, it would be difficult to establish the long-term results from the application of PFMT [5,17-20]. Regardless, some of the studies hold that long-term outcomes of PFMT are significantly greater when the participants are supervised for no less than three months. If the participant continues with the programme for an extended period, the treatment effect is likely to be enhanced accordingly or at least remain constant.
From the conclusions of the selected studies, there are a few considerations for future research on this topic. First, studies would need to consider the choice and reporting of secondary outcome measures [5]. Second, they would need to consider the choice of primary outcomes that matter to women, subsequent assessment of sample size, and the size of least clinically important effect.
Conclusion
Overall, there is evidence for the widespread recommendation for use of pelvic floor muscle training in preventing and treating urinary incontinence for pre-post-natal women as compared to nonintervention in Table 2. The limited nature of follow-up beyond the end of treatment in the majority of the published studies means that the long-term effects may be greater in women participating in supervised PFMT for at least three months. Continued adherence to training may be associated with maintained or increased treatment effect, but this hypothesis needs further testing. There is a need for at least one large, well conducted, and explicitly reported randomized trial, comparing PFMT with a control to investigate the longer-term clinical effectiveness of PFMT.
| Considered judgment table | ||
|---|---|---|
| Key question: Are antenatal pelvic floor exercises significantly better than non-intervention in preventing urinary incontinence? | ||
| 1.Quality of evidence: Ten studies have surveyed the significance of pelvic floor muscle training exercises in preventing and treating urinary incontinence both in late pregnancy and after delivery. All the studies were of good quality methodologically and have reduction in urinary incontinence or regaining of continence as the primary end point. | ||
| 2. Applicability: The evidence is fully applicable as it shows PFMT reduces existing urinary incontinence as well as significantly reducing its occurrence in pregnancy | ||
| 3. External validity: It is reasonable to generalize the results of all the 10 studies in the target population and the general population as the integrity of the studies is safeguarded and a sizeable randomized sample of the population with similar characteristics used. | ||
| 4 Consistency: There is a high degree of consistency in the available evidence. There is no study that demonstrated conflicting results. | ||
| 5. Quantity of evidence: All the studies included had evidence that was statistically significant and with significant impact in reduction of urinary incontinence. | ||
| 6. Clinical impact: Pelvic floor muscle training if implemented both correctly and consistently will have a great impact in urinary incontinence reduction during late pregnancy and early postpartum period as compared to normal antenatal and postnatal care. It also significantly reduces existing urinary incontinence in postnatal women. There are no indicated risks of the intervention in the evidence available. | ||
| 7. Other factors: There were no other factors taken into consideration when assessing evidence base. | ||
| 8. Evidence statement: In an expectant lady without urinary incontinence, starting them on pelvic floor muscle training exercise with good supervision at between gestation weeks 20 and 34 ,will significantly reduce episodes of urinary incontinence in late pregnancy and early postpartum. In a postpartum woman with urinary incontinence, pelvic floor muscle exercise will significantly reduce incontinence by 6 to 12 months. In the long run, there is no significant difference between control and PFMT. | Evidence level 1++ 1+ |
|
| 9.Reccommendation: Prenatal women should actively participate in PFMT to reduce late pregnancy and postnatal urinary and fecal incontinence. Post-natal women with stress incontinence should enroll for PFMT early enough (within 3 months) to enhance the prognosis of incontinence reduction. | A B | |
Table 2: Comparative summary of best evidence.
Given that most of the selected studies do not report any follow up beyond the completion of the treatment programme, it is difficult to determine the lasting outcomes from the application of PFMT.
In conclusion, pelvic floor exercises are beneficial and have no significant adverse effects. Substantially and durable improvements in continence can be achieved, when the patient is appropriately selected and the exercises are adequately performed.
References
- Viktrup L, Rortveit G, Lose G (2006) Risk of stress urinary incontinence twelve years after the first pregnancy and delivery. Obstet Gynecol 108: 248-254.
- Haylen BT, de Ridder D, Freeman RM, Swift SE, Berghmans B, et al. (2010) An international urogyencological Association/ International Continence Society joint report on the terminology for female pelvic floor dysfunction. Int Urogynecol J 21: 5-26.
- Glazener CM, Herbison GP, Wilson PD, MacArthur C, Lang GD, et al. (2001) Conservative management of persistent postnatal urinary and faecal incontinence: randomized controlled trial. BMJ 323: 593-596.
- Abrams P, Cardozo L, Khoury S, Wein A (2005) Incontinence. In: Proceedings from the 3rd edtn. International Consultation on Incontinence. Paris health publications 2: 798-1677.
- Chow SC, Wang H, Shao J (2007) Sample size calculations in clinical research. CRC press.
- The Joanna Briggs Institute best Practice information sheet: the effectiveness of pelvic floor muscle exercises on urinary incontinence in women following childbirth. Nursing & Health Sciences, Wiley online Library, USA.
- Allhadadi K, Tostes R, Webb R (2009) Female sexual dysfunction: therapeutic options and experimental challenges. Cardiovasc Hematol Agents Med Chem 7: 260-269.
- Cichonska M, Maciag D, Zboina B, Latawiec I, Krawczyk W (2013) The assessment of women’s knowledge concerning urinary incontinence. Zdrowie I dobrostan 4: 45-64.
- Christoper JK, Paul DP (2014) Incontinence is treatable-even-curable-for both men and women.
- Aqur WI, Steggles P, Waterfield M, Freeman RM (2008) The long-term effectiveness of antenatal pelvic floor muscle training; 8-year follow up of a randomized controlled trial. BJOG 115: 985-990.
- Boyle R, Hay-Smith EJ, Cody JD, Morkved S (2012) Pelvic floor muscle training for prevention and treatment of urinary and fecal incontinence in antenatal and postnatal women. Cochrane Database Syst Rev 10: CD007471.
- Chiarelli P (2001) Promoting urinary continence in women after delivery: randomized controlled trial. BMJ 324: 1241.
- Glazener CM, Herbison GP, McArther C, Grant AM, Wilson PD (2005) RCT of conservative management of postnatal urinary and faecal incontinence: six year follow up. BMJ 330: 337.
- Kahyaoglu H, Kaplan PK (2015) Effect of pelvic floor muscle exercise on pelvic floor muscle activity and voiding functions during pregnancy and postpartum period. Neurourol Urodyn 35: 417-422.
- Hay-Smith J, Morkved S, Fairbrother KA, Herbison GP (2008) Pelvic floor muscle training for prevention and treatment of urinary and faecal incontinence in antenatal and postnatal women. Cochrane database systematic review 8: CD007471.
- Ko PC, Liang CC, Chang SD, Lee JT, Chao AS, et al. (2011) A randomized controlled trial of antenatal pelvic floor exercises to prevent and treat urinary incontinence. Int Urogynecol J 22: 17-22.
- Morkved S, Bo K, Schei B, Salvesen KA (2003) Pelvic floor muscle training during pregnancy to prevent urinary incontinence: a single-blind randomized controlled trial. Obstet Gynecol 101: 313-319.
- Reilly ET, Freeman RM, Waterfied MR, Waterfield AE, Steggles P, et al. (2002) Prevention of postpartum stress incontinence in primigravidae with increased bladder neck mobility. BJOG 109: 68-76.
- Stafne SN, Salvesen KA, Romundstad PR, Tojusen IH, Morkved S (2012) Does regular exercise including pelvic floor muscle training prevent urinary incontinence during pregnancy. BJOG 119: 1270-1280.
- Mason L, Roe B, Wong H, Davies J, Bamber J (2010) The role of antenatal pelvic floor muscle exercises in prevention of postpartum stress incontinence; a randomized controlled trial. J Clin Nurs 19: 2777-2786.
Citation: Alfarra N (2017) Comparison between the Significant of Antenatal Pelvic Floor Exercises and Non-Intervention in Preventing Urinary Incontinence: A Systematic Literature Review. J Nov Physiother 7: 369. DOI: 10.4172/2165-7025.1000369
Copyright: © 2017 Alfarra N. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 3702
- [From(publication date): 0-2017 - Apr 02, 2025]
- Breakdown by view type
- HTML page views: 2928
- PDF downloads: 774