Comparison between the Effect of Different Durations of Cryotherapy and Stretching on Hamstring Flexibility
Received: 01-Apr-2019 / Accepted Date: 15-Apr-2019 / Published Date: 22-Apr-2019 DOI: 10.4172/2165-7025.1000409
Abstract
Background: The hamstring is a biarticular postural muscle that flexes the knee, extends the hip, and plays a role in activities, such as walking, running, climbing stairs, and jumping. Hamstring shortening is associated with a high incidence of muscle strain, patellofemoral pain, and poor gait. Precooling and static stretching have been used to increase connective tissue viscoelasticity and improve muscle flexibility. Studies have shown that the application of ice may provide improvements in hamstring flexibility over heat or stretching alone. However, insufficient scientific data exist regarding the effectiveness of different durations of cooling combined with static stretching on muscle flexibility.
Methods: To help explore the effects of different durations of cryotherapy and stretching on muscle flexibility, four experimental conditions of cold pack applications were compared on different days with two days in between the experimental conditions. The purpose of this study was to compare 5, 10, 15, and 20 minutes of cold pack application followed by hamstring stretching on muscle flexibility in 25 healthy subjects. A randomized withinsubjects design was used to compare the changes before and immediately after cold pack application and stretching in popliteal angle measurement. Stretching was conducted for 30 seconds and repeated three times.
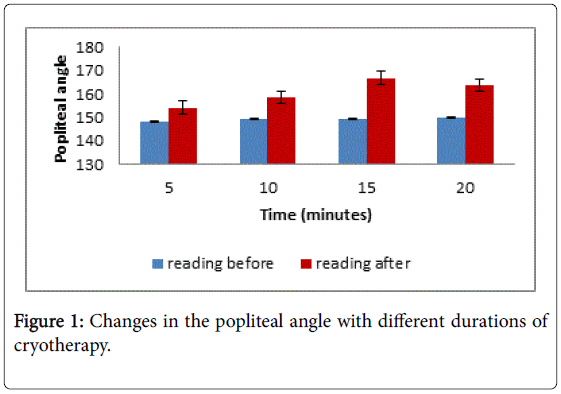
Results: Analysis of variance revealed a significant main effect for time demonstrated in an increased popliteal angle measurement. All groups showed significant differences in the popliteal angle measurement before and after cold pack administration. Additionally, although 15 minutes resulted in the highest measured popliteal angle among the four conditions, the post hoc test showed that this change was statistically significant from 5 and 10 minutes but not from 20 minutes.
Conclusion: The results infer that short cold pack application has limited effectiveness in altering muscle flexibility and that durations of 15 and 20 minutes are better employed for superior outcomes.
Keywords: Cold pack; Popliteal angle; Static stretch; Treatment duration
Abbreviations
ROM: Range of Motion; HML: Hamstring Muscle Length; PA: Popliteal Angle; CP: Cold Pack
Introduction
The hamstring is a biarticular postural muscle composed laterally from the biceps femoris longus and brevis, while semimembranosus and semitendinosus compose the medial muscle mass. The hamstring is most active in the transition from swing to stance during gait cycle. It works to flex the knee and extend the hip, and depending on the muscle mass contracted, i.e., medial or lateral, knee flexion can be associated with medial or lateral rotation of the knee [1]. The hamstring also contributes to axial rotation of the tibia and provides active resistance to the anterior glide of the tibia on the femur, hence playing a role in maintaining knee stability [1,2]. Poor posture, monotonous one-sided movement, and lack of activity, injury, or pain all could lead to muscle dysfunction and shortening [3]. Decreased muscle length can alter the moment arm and performance [1], leading to abnormal posture and pain [3]. Shortening of the hamstring is associated with a high incidence of muscle strain [4], patellofemoral pain [5], and poor gait [6].
Loss of muscle flexibility can be detected through diminished capacity of a muscle in response to mechanical stress and a lowered Range of Motion (ROM) as a consequence [7]. Physical therapists routinely assess Hamstring Muscle Length (HML) to assess muscle flexibility and its involvement in function [8,9]. The HML measurement is obtained indirectly by obtaining the angular measurement of unilateral hip flexion with the knee extended or via the Popliteal Angle (PA) by measuring the unilateral passive knee extension with the hip flexed to 90° [2].
The application of a Cold Pack (CP) is a therapeutic intervention that is widely used in clinical and rehabilitative settings. It is used to decrease pain in musculoskeletal and postoperative conditions, regulate the hemostatic and inflammatory phases, aid in tissue repair and recovery [10], prevent pathological changes in cartilage caused by contracture [11], improve aerobic and anaerobic capacities [12,13], and increase volitional muscle activation [14].
Precooling and static stretching (cooling tissues before exercise) have been used to increase joint ROM, as it is believed to have an effect on the mechanical properties of the muscle and in increasing connective tissue viscoelasticity [15,16]. This will both enhance performance and decrease the severity and frequency of injuries [17]. However, stretching can be hindered by pain or muscle reflex response. As such, when cryotherapy is applied to the muscle intended to be stretched, it can reduce nerve conduction velocity, result in lower muscle spindle discharge [18], inhibit muscle reflex, and optimize muscle flexibility [19].
Studies have shown that application of ice may provide enhanced short-term improvements in HML over heat or stretching alone [17]. However, deciding the optimal timing for application remains a dilemma for therapists. Some research papers have used as little as 10 minutes of cryotherapy application [20], while electrophysical agents textbooks recommend a duration of 15-20 minutes [21] or sometimes 20-30 minutes of application [22]. Such conflict makes it difficult for therapist to reach an informed clinical decision. Insufficient published data exist regarding the effectiveness of different durations of cooling combined with static stretching [23]. Evidence of the effect of cooling on tissue compliance is still debatable and conflicting; therefore, further research on this topic is imperative [24].
The present investigation aimed to compare the effects of different durations of cryotherapy followed by static stretching on muscle length in the lower limbs using PA as an indicator. We hypothesized that CP application for 20 minutes followed by static stretching for 30 seconds would yield superior effects compared with CP applications of 5, 10, and 15 minutes.
Materials and Methods
Subjects
Twenty-five healthy participants (15 men and 10 women, age 22 ± 3 years, height 164.7 ± 9.9 cm, weight 65.4 ± 13.9 kg) were recruited to participate in the study. Subjects were excluded from the study if they had any of the standard contraindications to cryotherapy [10] or any orthopedic conditions that limited lower limb ROM, such as osteoarthritis or recent fracture, or if they were participating in any other stretching protocol.
Ethical approval was granted by institute ethical committee. All subjects were informed about the benefits and risks of the study and provided informed written consent before participating in the study.
Procedure
All testing and measurement procedures were performed in the electrotherapy lab of the Physical Therapy Department of Kuwait University. Participants’ demographic data were obtained during the first session after they provided consent. The order of the CP applications was randomized based on the blinded selection of a protocol sequence paper slip that was generated using an online randomizer (https://www.randomizer.org/). Each subject chose a slip of paper that contained a random sequence of treatment times (5 minutes, 10 minutes, 15 minutes, 20 minutes), and this was the order by which patients commenced their treatment sessions. Participants attended four sessions with two days in between each session to avoid a latent effect of the CP from the previous application.
Participants underwent a screening test for sensation prior to CP application. The sensation test included a thermal sensitivity test and a cold urticaria test, which are the basic international prerequisites for safe CP application (Belanger, 2010). During each session, the participants received one of the following applications: 5, 10, 15, or 20 minutes of CP followed by static stretching.
A trained physical therapist used a standard universal goniometer to measure the PA in supine position [20]. Reliability of the examiner using the goniometer in repeated measurement was established prior to commencing the study. A standard commercial CP (28 cm × 36 cm) covered with one wet towel was placed on the posterior aspect of the dominant thigh and stabilized with a restraining strap. The participants were instructed to refrain from movement and that to not sleep or touch the CP, and they were required to inform the therapist of any abnormal feeling during CP application, such as pain, irritation, or itching.
The maximal passive PA was measured before CP application (preintervention) and immediately following the stretching exercise (postintervention). To perform the stretching, participants were asked to stand on one leg, raise the other leg, and place it onto the bed. They were instructed to lean forward until moderate tolerable discomfort was felt on the posterior thigh. This position was maintained for 30 seconds [25]. The PA was measured with participants in a supine position with their hip and the knee held in 90 degrees of flexion; the knee was then extended until it felt tight, and the angle between the thigh and the calf was measured.
Statistical Analyses
The independent variable was the duration of CP application, which included four time intervals (5, 10, 15, and 20 minutes), and the dependent variable was the measurement of the PA. The descriptive variables are expressed as a mean with standard deviation or range.
Baseline equivalence of the PA angle was tested to ensure similarity of the PA measurement before analysis. A repeated-measures analysis of variance was used to assess differences between the groups’ mean values, and the Bonferroni post hoc test was used to identify the level of significance between the groups. The significance level (0.05) was determined a priori. Statistical analyses were performed using SPSS, version 20 (IBM Corp., Armonk, NY, USA).
Results
Twenty-five subjects (15 male and 10 female) participated in this study. Demographic data of the participants are presented in Table 1.
| Male participants | Female participants | |||||||
|---|---|---|---|---|---|---|---|---|
| n = 15 | n = 10 | |||||||
| Min | Max | Mean | SD | Min | Max | Mean | SD | |
| Age (years) | 18 | 30 | 22.53 | 3.81 | 20 | 22 | 21.3 | 0.67 |
| Height (cm) | 160 | 186 | 170.8 | 8.02 | 151 | 164 | 155.7 | 3.74 |
| Weight (kg) | 57 | 86.9 | 74.22 | 8.4 | 41 | 68 | 52.2 | 9.1 |
| BMI | 16.65 | 30.11 | 25.16 | 3.18 | 15.67 | 29.05 | 21.48 | 4.14 |
SD: Standard Deviation; Min: Minimum; Max: Maximum; BMI: Body Mass Index
Table 1: Participant demographic data.
Given that the four different tests were conducted on different days, baseline equivalence was tested to ensure similarity of the PA measurement before conducting the trial. Mauchly’s test of sphericity indicated that the assumption of sphericity had not been violated, χ2 (3)=0.578, and p=0.631, indicating no significant difference between the baseline (pre-intervention) knee measurement in any of the four conditions.
All groups displayed a mean increase in ROM under the four durations of cryotherapy, although the magnitude of this change varied between the groups (Table 2).
| 5 minute | 10 minute | 15 minute | 20 minute | |
|---|---|---|---|---|
| Mean intervention of pre-intervention PA (°) | 148.4 | 149.16 | 149.6 | 149.64 |
| Mean reading of post-intervention PA (°) | 154.08 | 158.54 | 164.58 | 163.6 |
| Minimum change in the PA measurement (°) | -8 | -4 | 0 | 0 |
| Maximum change in the PA measurement (°) | 17 | 34 | 57 | 42 |
| Mean overall PA change (°) | 5.68 | 9.38 | 17.18 | 13.24 |
| SD | 7.92 | 7.89 | 9.52 | 8.6 |
| % change | 3.8 | 6.3 | 10 | 9.3 |
SD: Standard Deviation; PA: Popliteal Angle; Min: Minimum; Max: Maximum
Table 2: Mean change in the measurement of the PA between different durations as measured by a goniometer and other related measurements.
The percentage of change in the PA angle was measured using an online percentage change calculator (https:// www.skillsyouneed.com/num/percent-change.html), which computes the percentage of changes and subtracts this from the baseline value and multiplies by 100. There was a significant main effect of time between the groups (F(3, 72,485)=8.460, p<0.001). Post hoc Bonferroni testing revealed the following multiple comparisons to be statistically different: 5 and 15 minutes (p<0.001), 5 and 20 minutes (p<0.01), and 10 and 15 minutes (p<0.001). However, there was no significant difference between 5 and 10 minutes (p=0.397), and 15 and 20 minutes (p=0.644). Further findings can be found in Table 3.
| STD error | sig | 95% confidence interval | ||
|---|---|---|---|---|
| Lower | Upper | |||
| 5-10 minute | 2.40807 | 0.766 | -10.1874 | 2.7874 |
| 5-15 minute | 2.40807 | 0 | -17.9874 | -5.0126 |
| 5-20 minute | 2.40807 | 0.013 | -14.0474 | -1.0726 |
| 10-15 minute | 2.40807 | 0.01 | -14.2874 | -1.3126 |
| 15-20 minute | 2.40807 | 0.63 | -2.5474 | 10.4274 |
*The mean difference is significant at the 0.05 level.
Multiple comparisons were made using the post hoc Bonferroni test.
Table 3: Results of the pairwise comparisons of the interventions.
The results from the 15 minute application were significantly different from the PA reading at 5 and 10 minutes. The 20 minute CP application yielded significantly different PA results compared to 5 and 10 minute applications, but both 15 and 20 minute treatments did not result in statistically significant results from each other.
Although changes in PA were comparable between the 15 and 20 minute CP application, the largest increase in the PA was recorded during the 15-minute treatment duration, followed by 20 minutes (Figure 1). Interestingly, six participants demonstrated a decrease in ROM after a 5 minute CP application and stretching, and two participants exhibited a similar decrease in ROM with a 10 minute CP application. The 15 and 20 minute CP applications did not result in such findings, and no reduction in ROM was noted (Table 2).
Discussion
Our study is the first to compare the effect of four different durations of CP application on hamstring muscle flexibility. The main finding of the study was that CP application for 15 and 20 minutes can be effective and yield better outcomes than shorter applications of 5 or 10 minutes if the therapeutic aim of the intervention is to stretch muscles. Although 15 and 20 minutes resulted in statistically significant outcomes, which were reflected in the knee ROM measurement, careful examination of the magnitude of increase between the two durations revealed a larger increase with the 15 minute treatment duration (mean increase in PA 17.18° ± 9.52, compared to mean increase of 13.24° ± 8.60 with 20 minutes). This response may indicate that 15 minutes resembles the peak after which the cooling effect starts to decrease. According to Watson [26], exogenous energy acts as a trigger to stimulate, enhance, or activate particular physiological events, which will eventually result in the therapeutic effects required. However, for such effects to happen, therapists should utilize the concept of windows of opportunity, a theory based on matching the magnitude of the applied energy to the diseased structure, as the response is seen to be dose dependent. Varying the dose could alter findings and may lead to improvement or sometimes deterioration [27,28]. A higher dose, or in our case – a longer time frame, does not always equate with superior outcomes, as was demonstrated in the works of Hughes et al. [29] and Vinck et al. [30]. The findings herein seem to support this concept. However, further exploration is warranted.
Stretching techniques are effective interventions to improve ROM, as they could improve muscle viscoelasticity and increase stretch tolerance [31]. In the current study, using a CP for as little as 5 minutes resulted in an average increase of 3.8% in PA. These results were in agreement with those of Park et al. [32] who reported a favorable gain in muscle length after 3 minutes of CP application. The increase in ROM after the application of CPs could be due to the decrease in the uncomfortable sensation associated with muscle stretching, hypoalgesic effect of cooling, increase in the pressure pain threshold, and reduction in stretch sensitivity [32,33]. The cooling agent and decrease in tissue temperature may have facilitated all these aforementioned conditions.
Interestingly, some participants in the current study experienced reduced ROM following shorter CP applications (5, 10 minutes). Six subjects out of the 25 demonstrated a decrease in PA range after 5 minutes of CP application and stretching, while only two in the 10 minute group exhibited similar decrease in the PA range. Such a decrease in the PA range did not occur with the longer CP application times (15 and 20 minutes). Measuring the temperatures of the CP and skin before CP application and determining the thermal dose could aid in justifying these observations objectively. Future studies are needed to address the reasons underpinning the decrease in ROM observed herein. Such knowledge will facilitate an increased understanding of the physiology and mechanism of cryotherapy and expedite informed practice. The findings of the study, however, do not support our hypothesis that 20 minutes of CP application followed by stretching is more beneficial than CP applications of shorter durations (15, 10, and 5 minutes).
This study has some limitations. First, our study included healthy subjects who had no symptoms or injuries. Thus, further studies need to be conducted in a patient population. Second, the inclusion of a stretching only group would have facilitated a more robust understanding of the findings. Despite the recorded increase in the measurement due to stretching, one might question its therapeutic/ clinical use in individuals and argue whether the measured change is due to the stretching effect alone and not the cryotherapy application. The absence of a stretching only group prevents the authors from making any inferences.
Practical implications
It is of paramount importance that therapeutic applications and clinical decisions in healthcare be guided by the best available evidence. Furthermore, in order to optimize treatment outcomes, guidelines and practice policies should be substantiated by support derived from experimentation. The duration of CP application has been used for decades based on empirical evidence and as suggested by many textbooks without a scientifically researched background.
Our study is the first to compare the effect of different cryotherapy applications on muscle stretching. Inarguably, cryotherapy is an effective treatment and a treatment of choice when muscle stretching is the desired outcome. The current study encourages clinicians to use 15 or 20 minutes as their routine application and refrain from using durations such as 5 and 10 minutes because of their limited effectiveness.
Conclusion
The application of CPs for duration of 15 or 20 minutes followed by static stretching resulted in a significant increase in passive ROM of the knee. Applying CPs for shorter durations provided no significant advantage.
Acknowledgment
The authors would like to thank all the participants for their time and effort. The authors declare no conflicts of interest, financial or otherwise. The experiment complies with the current laws of the country.
References
- Oatis C (2017) Kinesiology the mechanics and pathomechanics of human body. 3rd edtn, Wolters Kluwer, South Holland, Netherlands.
- Norkin C, White D (2016) Measurement of joint motion: a guide to goniometery. 4th edtn, FA Davis Company, Philadelphia, Pennsylvania.
- Evjenth O, Hamberg J (1989) Auto Stretching. The complete manual of specific stretching, Alfta Rehab Forlag, Sweden.
- Wan X, Qu F, Garrett W, Liu H, Yu B (2017) The effect of hamstring flexibility on peak hamstring muscle strain in sprinting. J Sport Health Sci 28: 283-289.
- White LC, Dolphin P, Dixon J (2009) Hamstring length in patellofemoral pain syndrome. Physiotherapy 95: 24-28.
- Whitehead CL, Hillman SJ, Richardson AM, Hazlewood ME, Robb JE (2007) The effect of simulated hamstring shortening on gait in normal subjects. Gait Posture 26: 90-96.
- Bandy WD, Irion JM, Briggler M (1997) The effect of time and frequency of static stretching on flexibility of the hamstring muscles. Phys Ther 77: 1090-1096.
- Somers M (2009) Spinal cord injury: functional rehabilitation. 3rd ed., Upper Saddle River, New Jersey, Prentice Hall.
- Magee D (2008) Orthopedic physical assessment. 5th ed, Saunders Elsevier, Missouri.
- Belanger A (2010) Therapeutic electrophysical agents: evidence behind practice. 2nd ed, Lippincott Williams & Williams, Baltimore, Maryland.
- Kojima S, Watanabe M, Hoso M (2015) The effect of cryotherapy for the prevention of contracture. Physiotherapy 101: 779-780.
- Ranalli GF, DeMartini JK, Casa DJ, McDermott BP, Armstrong LE, et al. (2010) Effect of body cooling on subsequent aerobic and anaerobic exercise performance: a systematic review. J Strength Cond Res 24: 3488-3498.
- Duffield R, Green R, Castle P, Maxwell N (2010) Precooling can prevent the reduction of self-paced exercise intensity in heat. Med Sci Sports Exerc 42: 577-584.
- Pietrosimone BG, Hart JM, Ingersoll CD (2009) Effects of focal knee joint cooling on spectral properties of rectus femoris and vastus lateralis electromyography. Athletic Training Sports Health Care 1: 154-161.
- Knight CA, Rutledge CR, Cox ME, Acosta M, Hall SJ (2001) Effect of superficial heat, deep heat, and active exercise warm-up on the extensibility of the plantar flexors. Phys Ther 81: 1206-1214.
- Taylor BF, Waring CA, Brashear TA (1995) The effects of therapeutic application of heat or cold followed by static stretch on hamstring muscle length. J Orthop Sports Phys Ther 21: 283-286.
- Brodowicz GR, Welsh R, Wallis J (1996) Comparison of stretching with ice, stretching with heat, or stretching alone on hamstring flexibility. J Athl Train 31: 324-327.
- Magalhães F, Junior AR, Meneses HT, Moreira Dos Santos RP, Rodrigues EC, et al. (2015) Comparison of the effects of hamstring stretching using proprioceptive neuromuscular facilitation with prior application of cryotherapy or ultrasound therapy. J Phys Ther Sci 27: 1549-1553.
- Burke DG, Holt LE, Rasmussen R, MacKinnon NC, Vossen JF, et al. (2001) Effects of hot or cold water immersion and modified proprioceptive neuromuscular facilitation flexibility exercise on hamstring length. J Athl Train 36: 16-19.
- Malanga G, Nadler S (2006) Musculoskeletal physical examination: an evidence-based approach, Elsevier Mosby, Philadelphia, Pennsylvania.
- Bell G, Prentice W (2018) Infrared Modalities. In Prentice W, Therapeutic Modalities in Rehabilitation, McGraw hill education, New York, pp: 295-312.
- Denegar C, Perrin D (2000) Cold and superficial heat. In Denegar C, Perrin D, Therapeutic modalities for athletic injuries, Human Kinetics, Champaigen, pp 100-123.
- Lin YH (2003) Effects of thermal therapy in improving the passive range of knee motion: comparison of cold and superficial heat application. Clin Rehabil 17: 618-623.
- Bleakley CM, Costello JT (2013) Do thermal agents affect range of movement and mechanical properties in soft tissue? A systematic review. Arch Phys Med Rehabil 94: 149-163.
- McAlee R, Charland J (2014) Facilitated stretching. 4th ed, Human Kinetics Publisher, Champaign, Illinois.
- Watson T (2010) Narrative review: key concepts with electrophysical agents. Phys Ther Rev 15: 351-359.
- Fabrcic T, Balden C, Machado A, Caffaro L, Masson I, et al. (2018) Collagen fibers in the healing process of rat Achilles tendon rupture using different times of ultrasound therapy. Adv Wound Care (New Rochelle) 7: 114-120.
- Robertson V (2002) Dosage and treatment response in randomized clinical trials of therapeutic ultrasound. Phys Ther Sport 3: 124-133.
- Hughes N, Bennett M, Johnson M (2013) An investigation into the magnitude of the current window and perception of transcutaneous electrical nerve stimulation (TENS) sensation at various frequencies and body sites in healthy human participants. Clin J Pain 29: 146-153.
- Vinck EM, Cagnie B, Cornelissen M, Declercq H, Cambier D (2003) Increased fibroblast proliferation induced by light emitting diode and low power laser irradiation. Lasers Med Sci 18: 95-99.
- Morse CI, Degens H, Seynnes OR, Maganaris CN, Jones DA (2008) The acute effect of stretching on the passive stiffness of the human gastrocnemius muscle tendon unit. The J Physiol 586: 97-106.
- Park KN, Kwon OY, Weon JH, Choung SD, Kim SH (2014) Comparison of the effects of local cryotherapy and passive cross-body stretch on extensibility in subjects with posterior shoulder tightness. J Sports Sci Med 13: 84-90.
- Anaya-Terroba L, Arroyo-Morales M, Fernández-de-Las-Peñas C, Diaz-Rodriguez L, Cleland JA (2010) Effects of ice massage on pressure pain threshold and electromyography activity post exercise: randomized controlled crossover study. J Manipulative Physiol Ther 33: 212-219.
Citation: Almandil M, Alenzi N, Aleid H (2019) Comparison between the Effect of Different Durations of Cryotherapy and Stretching on Hamstring Flexibility. J Nov Physiother 9: 409. DOI: 10.4172/2165-7025.1000409
Copyright: © 2019 Almandil M, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 3366
- [From(publication date): 0-2019 - Apr 02, 2025]
- Breakdown by view type
- HTML page views: 2583
- PDF downloads: 783