Research Article Open Access
Comparison between Task - Oriented Training and Proprioceptive Neuromuscular Facilitation Exercises on Lower Extremity Function in Cerebral Palsy-A Randomized Clinical Trial
Chandan Kumar1* and Priyanka Ostwal2
1Department of Physiotherapy, School of Allied Health Sciences, Sharda University, India
2MPT (Pediatrics), Sharda University, India
- *Corresponding Author:
- Chandan Kumar Associate Professor, Department of Physiotherapy, School of Allied Health Sciences, Sharda University, Neurological Physiotherapy, C-20, Delhi Police Housing Society, Sector PI-1, Greater Noida, UP 201308, India, Tel: +918087518006; E-mail: ptchandan221@yahoo.co.in
Received date: April 18, 2016; Accepted date: May 10, 2016; Published date: May 25, 2016
Citation: Kumar C, Ostwal P (2016) “Comparison between Task - Oriented Training and Proprioceptive Neuromuscular Facilitation Exercises on Lower Extremity Function in Cerebral Palsy-A Randomized Clinical Trial”. J Nov Physiother 6:291. doi:10.4172/2165-7025.1000291
Copyright: © 2016 Kumar C, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Novel Physiotherapies
Abstract
Background and objective: The large majorities of children with Cerebral Palsy (CP) have difficulty in walking; demonstrate poor balance control, that leads to poor gait and reaching movement as the maintenance of stability is critical to all movements. There are various approaches and strategies to improve gait, balance and lower extremity function, Task-Oriented Training and Proprioceptive Neuromuscular Facilitation exercises are one of them. Therefore, this study aims to compare the effect of Task-Oriented Training and Proprioceptive Neuromuscular Facilitation exercises on lower extremity function in children with cerebral palsy.
Material and method: Thirty patients who fulfilled the inclusion criteria were randomly allocated into two groups. Group A -Task- Oriented Training, Group B- Proprioceptive- Neuromuscular Facilitation. Exercises with 15 patients in each group. All the patients were evaluated with Pediatric Balance Scale, and Gait parameters- Gait Velocity, Stride length and Cadence at pre and post treatment level.
Results: When comparison of pre and post intervention values of Pediatric Balance Scale and Gait parameters was done, significant difference was found (P<0.001) in both groups. When comparison was done at post intervention level for Pediatric Balance Scale and Gait parameters, significant result was found (P<0.001) for Stride Length and cadence and non-significant results for Pediatric Balance Scale and Gait velocity.
Conclusion: From finding of this study it was concluded that both Task-Oriented Approach and Proprioceptive Neuromuscular Facilitation Exercises are beneficial in improving lower extremity function in children with cerebral palsy.
Keywords
Cerebral palsy; Proprioceptive neuromuscular facilitation; Task-oriented training; Lower extremity function; Balance
Introduction
Cerebral palsy (CP) is defined as an “umbrella term covering a group of non-progressive, but often changing, motor impairment syndromes secondary to lesions or anomalies of the brain arising in the early stages of its development” [1]. Despite the lack of consensus on a definition of CP, three elements are recurring: (i) brain lesion, (ii) onset at birth or early child years, and (iii) impaired motor control. A well-cited definition of CP defines CP as: ‘‘a group of disorders of the development of movement and posture, causing activity limitations that are attributed to non-progressive disturbances that occurred in the developing fetal. The motor disorders of CP are often accompanied by disturbances of sensation, perception, cognition, communication, behavior, by epilepsy and by secondary musculoskeletal problems’’ [2].
Cerebral palsy (CP) is the most common cause of physical disability in childhood, with an estimated incidence of 2.11 per 1000 live births [3]. Cerebral Palsy incidence rate keeps rising, partly due to greater numbers of premature infants who are surviving and longer overall survival [4].
Diplegic CP patients exhibit weak postural balance control ability and less standing stability compared with hemiplegic cerebral palsy patients [5]. Population-based study indicates that people with CP have proprioception deficits in all limbs [6]. Stiff knee in swing, equinus, and intoeing were all seen in more than 50% of the subjects of the diplegic groups. Increased hip flexion and crouch were also present in more than 50% of the subjects in the diplegic [7]. The large majorities of children with CP have difficulty in walking, demonstrate poor balance control: that leads to poor gait and reaching movement as the maintenance of stability is critical to all movements [8]. The ability to walk is a major concern of the parents of children with CP, and improving or maintaining this ability is often considered to be the primary focus of most therapeutic interventions addressing the motor problems seen in children with spastic diplegia [7].
There are various approaches and strategies; to improve gait and balance, and thus to improve lower extremity function. Commonly used approaches in treatment of children with CP are Neurodevelopmental Treatment (NDT) [9-11], Task-oriented Training [12] and Proprioceptive Neuromuscular Facilitation [13], Conductive Education (CE) by Andras Peto [14-17], Reflex Locomotion Therapy by Vojta [18], The Patterning Method by Doman and Delacato [19], Sensory Integration by Ayres [20], Therapeutic Horse Riding or Hippotherapy and Aquatic Therapy or Hydrotherapy are frequently used therapies for children with CP [21-23]. Among the methods currently used in rehabilitation of children with CP seem to be leading are Task-oriented Training and Proprioceptive Neuromuscular Facilitation Exercises for improving balance and gait.
Task-oriented training is defined as the repetitive training of significant, functional activities or element of such activities, to acquire well-organized and effective motor skill [24]. The task-oriented Training approach is based on a systems model of motor control and contemporary motor learning theories. This approach focuses on interactions between the sensorimotor system components of strength, endurance, range of motion, coordination, sensory awareness, postural control, and perceptual skills, and uses the concepts of degrees of freedom and control parameters [25]. With the emergence of the task-oriented approach, the focus of therapy in rehabilitation has shifted from eliminating deficits to enhancing function across all performance domains by emphasizing fitness, function, participation, and quality of life [26].
Proprioceptive Neuromuscular Facilitation (PNF) integration pattern stimulates the proprioceptors within the muscle and tendon to enhance the performance, flexibility and balance; it is generally effective in maximizing the reaction of exercise unit by increasing the coordination which reacts to the stimulations in muscular strength and flexibility [27].
Therapists rebuild the movement and function of the limbs rendered paretic due to paralysis or paresis by guiding a specific movement pattern (diagonal or spiral direction) for concomitant muscle contractions with reversal, stabilization, repetition or combination techniques. The motor control or movement pattern facilitated by the therapist follows a sequence of static/dynamic and assistive-active-resistant progressions for regaining motor control and enhancing the muscle strength of the paretic limbs of patients. The PNF procedures are often accompanied by verbal/visual and tactile feedback to facilitate muscle contraction and motor control in terms of many techniques, such as joint approximation, traction, irradiation or overflow [28]. The facilitated progression due to the PNF procedures follows a hierarchical process from mobility to stability, then controlled mobility to skillful movement. If various patterns are applied simultaneously, more force can be used, thereby affecting muscle strength and stability further.
Both the Task-Oriented Training and Proprioceptive Neuromuscular Facilitation strategies has been proven to improve lower extremity function and it is important to note that these techniques differ in the manner in which they approach the problem. We do not have much evidences available about comparison between Task-Oriented Training and Proprioceptive Neuromuscular Facilitation exercises. Thus perspective of this study is to find out better treatment strategy and to compare a 4 weeks Task Oriented Training or Proprioceptive Neuromuscular Facilitation will improve lower extremity function in children with cerebral palsy.
The aim of the present study is to find out effectiveness of Task- Oriented Training and Proprioceptive Neuromuscular Facilitation exercises on improving balance, gait and lower extremity function in children with cerebral palsy as well as to find out better intervention strategies between both approaches in improving balance, gait and Lower extremity function.
Materials and Methods
This study was a Single Blinded Randomized clinical trial of total 30 Patients to compare between Task-Oriented Training and Proprioceptive Neuromuscular Facilitation exercises in improving balance, gait and Lower extremity function. We recruited subjects from Neuroscience department of Physiotherapy, MGM Hospital, Other hospitals and private clinics of Aurangabad. Participants were randomly selected into the study following simple random sampling using Lottery method. Total duration of study was 12 months and duration of intervention was 4 weeks.
Inclusion criteria were Children diagnosed as Diplegic cerebral palsy of both gender, aged between 5–12 years. They were having sufficient co-operation and cognitive understanding to participate, able to communicate and follow the instructions, able to perform sit-to- stand task and walking with or without walking devices, having spasticity range between 1 and 1+ grade according Modified Ashworth Scale and there was no limitation of lower extremities ranges of motion.
Exclusion Criteria Were Unstable seizures, receiving any treatment for spasticity or surgical procedures up to 3 months (for botulinum toxin type A injections) or up to 6 months (for orthopedic surgery) prior to the study (or planned during the study period). Children were suffering from other diseases that interfered with training, Presence of shortening or deformities of the ankle, knee and/or hip joints that prevented the children from keeping their feet on the ground, hindered them from maintaining the standing position, or made it impossible for them to independently perform an STS movement; and having difficulty maintaining an upright position without support for more than 30 seconds.
Materials utilized in this study were Record or Data Collection Sheet, Consent Form Mattress, Watch, Pediatric Balance Scale, Inch tape, 10 meter walk test, chair, Ink Pad and Stools.
Outcome measures
1. Pediatric berg balance: The Pediatric Balance Scale (PBS), a modification of Berg’s Balance Scale, was developed as a balance measure for school-age children with mild to moderate motor impairments. The PBS has been demonstrated to have good test-retest and interrater reliability (ICC 3, 1 = 0.997) when used with school-age children with mild to moderate motor impairments [29,30].
2. 10 meter walk test: This is a validated test for the clinical evaluation of walking speed. The subject was asked to walk at her/his self-selected walking speed along the central 10 m of a 14-m walkway. A digital stopwatch was used to time the walks [31,32].
3. Gait parameters: Stride length (cm), cadence (steps/min), velocity (m/min) [33].
Procedure
Step 1) All the subjects from specified source of data were assessed and those who fulfilled inclusion criteria were taken up for the study.
Step 2) All thirty subjects were randomly allocated in to two groups, Group A (Task Oriented Training) and Group B (Proprioceptive Neuromuscular Facilitation PNF), with 15 subjects in each.
Step 3) The procedure was explained to parents of all the children and written informed consent from the parents was taken.
Step 4) Each child was evaluated for their functional ability using the PBS, 10 meter walk test and Gait parameters prior to commencement of training.
During the pre-assessment session footprints of all the children were taken with the help of ink on chart paper. The ink was put on the feet of child with the help of a piece of cloth and child was asked to walk on the chart paper fixed on the floor. For the measurement of stride length 2 footprints of affected sides from the middle portion of each walking trial were analyzed.
Stride length
The stride length was measured from the heel of the affected foot to the heel of the same foot when it again contacts the ground with the help of a measuring tape/scale.
Cadence
The cadence i.e. steps per minutes were counted with the help of stop watch.
Gait velocity
Gait velocity was studied at comfortable walking speeds. The mean of 3 repeated walking speed measurements was calculated in order to reduce measurement error.
Step 5) Group A was given task oriented training: 45 minutes for 6 days/ week. Children in this group received
1) Standing and reaching in different directions for objects located beyond arm’s length to promote loading of the lower limbs and activation of lower limb muscles;
(2) Sit-to-stand from various chair heights to strengthen the lower limb extensor muscles;
(3) Stepping forward and backward onto blocks of various heights to strengthen the lower limb muscles;
(4) Stepping sideways onto blocks of various heights to strengthen the lower limb Muscles;
(5) Forward step-up onto blocks of various heights to strengthen the lower limb muscles;
(6) Heel raise and lower while maintaining in a standing posture to strengthen the plantar flexor muscles.
Each task was given 5 min in duration for each exercise class. Children were being encouraged to work as hard as possible at each workstation and were also be given verbal feedback and instructions aimed at improving performance. The progression of the task was considered according to each child’s ability. Progressions were include increasing the number of repetitions completed within 5 min at a workstation and increasing complexity of the exercise performed at each workstation, such as the distance reached in standing, reducing the height of the chair during sit-to stand, and the height of the blocks [34].
Group B were given Proprioceptive Neuromuscular Facilitation Exercises (PNF) for 45 minutes 6 days /week. The elements of PNF, such as manual contact, stretch, resistance, and verbal cuing, were incorporated into the treatment scheme.
Subjects were trained in accordance with the principles of PNF method. Improving methods included specific activity PNF conditioning correct gait. These were: in the sitting position:
1) Stabilizing Position (Sitting, Active),
2) Symmetrical Movements of the Pelvis (Rocking),
3) The Movements of the Head, Neck, Torso in the Direction of Flexion and Extension,
4) Asymmetrical Movements of the pelvis back and forth,
5) A Combination of Shoulder and Pelvic Movements,
6) Movements of The Torso in front of the detachment buttocks from the floor (standing up), 7) Back to Side in The Standing Position: to stabilize the position by approximation,
8) Diagonal Movement of Body Weight (balance),
9) Able to Stride, standing with one leg in the activity, walk forward, backward, sideways gait [13].
All the patient treated by specialized Neuro- Physiotherapist (post graduate in Neuroscience Physiotherapy), additionally he also holds the certificated for applying PNF approach. One physiotherapist who was blinded to study and group allocation used all outcome measures in the study.
Ethical approval
Before beginning the study an approval from the ethical committee of MGM’s Institute of Health Sciences, Aurangabad was taken.
Data Analysis
• Data was analyzed and tabulated with SPSS version 22nd (Statistical Package for Social Sciences) for windows and Microsoft Office Excel-2007. Mean, standard Deviation, Degree of freedom, confidence level, P value and significance were calculated to express the results.
• Unpaired’ t test has been done for Inter Group Comparison of Pediatric balance test (PBS), Step Length, Gait Velocity and Cadence in between Group at Pre and Post intervention level.
• Paired’ t test has been done for Intra –Group Comparison of Pediatric balance test (PBS), Step Length, Gait Velocity and Cadence in between Group at Pre and Post intervention level. The significant (Probability-P) has been considered as 0.05.
• Levene’s Test for has been used Equality of Variances for two groups.
Results
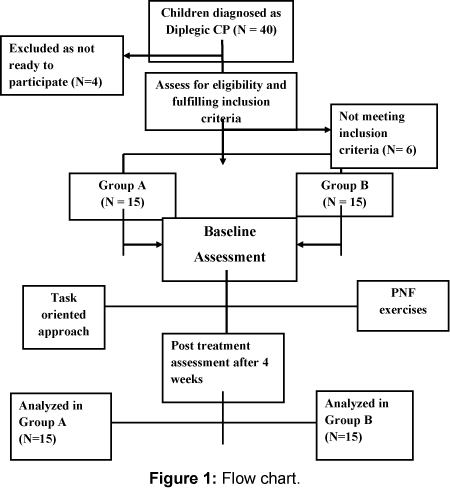
• 40 children were assessed for eligibility. Out of which 4 children were excluded because they refused to participate in study, 6 children were not meeting the inclusion criteria. Total 30 children were randomized and divided in to two groups. Group A (N= 15) (Task-Oriented Training), Group B (N=15) (Proprioceptive Neuromuscular Facilitation Exercises).
• Total of 16 males and 14 females were participated in the study. In group A there were 9 males and 6 females and in group B there were 7 males 8 females. In group A Total 5 children had pre-natal causes for cerebral palsy whereas 10 reported postnatal. In group B 8 children had prenatal and 7 postnatal causes responsible for cerebral palsy.
Discussion
The aim of present study was to compare the effect of Task-Oriented Training and Proprioceptive Neuromuscular Facilitation exercises in improving lower extremity function in children with cerebral palsy.
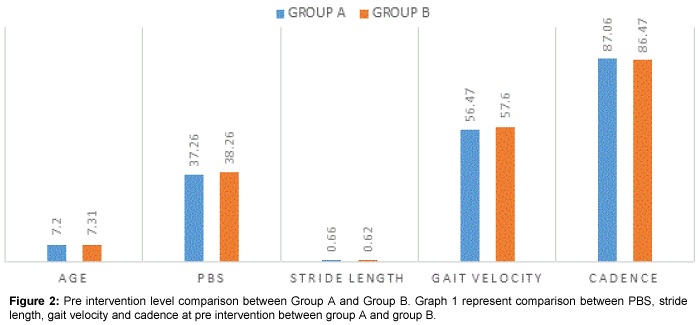
When analysis was done for demographic information of the participants, no statistically significant difference was found showing that subjects were matched for baseline characteristics. There was no significant difference between PBS, Stride Length, Gait Velocity and Cadence score at pre-intervention, which shows that two groups are statistically matched at baseline level as shown in Tables 1 and 2, Figures 1 and 2.
| Group A (Mean ± SD) | Group B (Mean ± SD) | P-value | Df | t value | S/NS | ||
|---|---|---|---|---|---|---|---|
| Age | 7.20 ±1.50 | 7.31 ± 1.44 | .884 | 28 | 0.198 | NS | |
| Male | 9 | 7 | |||||
| Female | 6 | 8 | |||||
| Causes of CP | Prenatal | 5 | 8 | ||||
| Postnatal | 10 | 7 | |||||
| PBS | 37.26 ± 3.47 | 38.26 ± 4.27 | .487 | 28 | 0.703 | NS | |
| Stride length | 0.66 ± 0.054 | 0.62 ±0.041 | .486 | 28 | 2.557 | NS | |
| Gait velocity | 56.47 ± 5.50 | 57.60±5.26 | .569 | 28 | 0.568 | NS | |
| Cadence | 87.06±6.46 | 86.47±4.58 | .771 | 28 | 0.293 | NS | |
Table 1: Demographic data of children. P<0.05* shows a statistically significant result. NS- Non Significant, S- Significant. The above table showing demographic and baseline characteristics of both the groups.
| F-Value | SIG. | |
|---|---|---|
| Preage | .084 | .774 |
| Pre PBS | 1.95 | .173 |
| Pre stride length | .389 | .538 |
| Pregait velocity | .005 | .945 |
| Precadence | 2.93 | .098 |
Table 2: Levene’s test for equality of variances. Above table shows test for equality of variance.
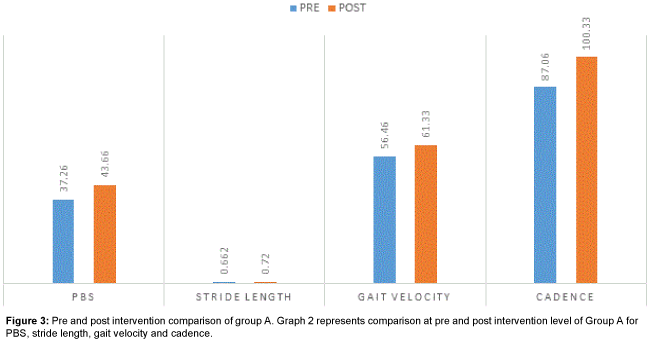
When comparison was done between pre and post intervention level for group A, the values of PBS, Gait velocity, Stride Length and Cadence were significant as evident in Table 3 and Figure 3, which suggest that Task Oriented Training is effective in improving lower extremity function. Result of this study is supported by the study of Frimpong et al. [35] who concluded that Task-oriented circuit training improved ambulatory functions of stroke survivors in the acute stage. It is also supported by systematic review conducted by Wevers et al. [36] This meta-analysis supports the use of task-oriented circuit class training to improve gait and gait-related activities in patients with chronic stroke.
| GROUP A | PRE (Mean ± SD) | POST (Mean ± SD) | P value | df | t value | S/NS |
|---|---|---|---|---|---|---|
| PBS | 37.27± 3.48 | 43.67±2.77 | 0.000 | 14 | -12.22 | S* |
| Stride length | 0.66±0.055 | 0.74±0.046 | 0.000 | 14 | -12.77 | S* |
| Gait velocity | 56.47 ± 5.50 | 61.33±4.93 | 0.000 | 14 | -9.28 | S* |
| Cadence | 87.07±6.46 | 100.33±2.94 | 0.000 | 14 | -12.60 | S* |
Table 3: Pre and post intervention comparison of group a for pbs, stride length, gait velocity and cadence. P<0.05* shows a statistically significant result. NS- Non Significant, S- Significant. Above table shows the pre and post intervention level comparison of group A for PBS, stride length, gait velocity and cadence, the result shows significant result.
Task oriented exercises have efficiency to improve balance, strength and functional mobility. Finding of this study is also matched with study done by Kumar et al. [37] who studied to determine the efficacy of task related circuit training on functional mobility and balance in children with spastic Diplegic type of cerebral palsy. This study suggests that task oriented circuit training is more effective as compared to the conventional training for the functional mobility and balance in spastic Diplegic cerebral palsy children. The improvement in balance can also be supported by the study done by Bo Hyun Kim et al. [38] who examined the effect on stroke patients of a task-oriented training program for trunk control ability, balance and gait. This study demonstrated that task-oriented training after a stoke can improve the trunk control ability, balance and gait, which be effective in stroke rehabilitation.
This may be because task specific training in rehabilitation focuses on improvement of performance in functional tasks through goal-directed practice and repetition. The focus is on training of functional tasks rather than impairment, such as with muscle strengthening and muscle weakness is a primary limiting factor in ambulation in children with cerebral palsy.
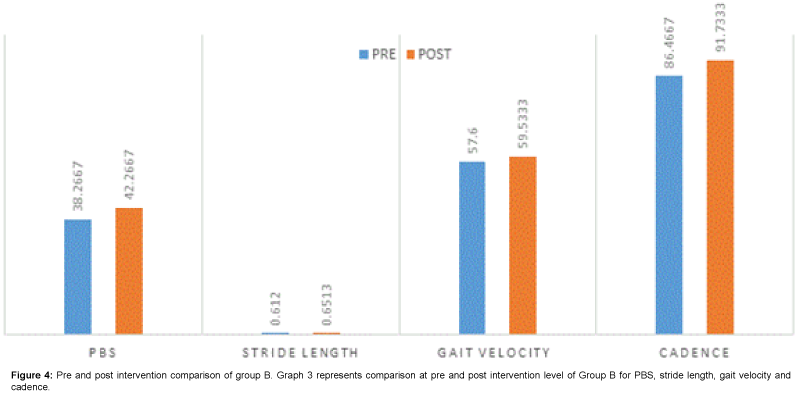
When comparison was done between pre and post intervention level for group B, The PBS, Gait velocity, Stride Length and Cadence scores were statically significant as evident in Table 4 and Figure 4, Which suggest that Proprioceptive Neuromuscular Facilitation (PNF) is also effective in improving lower extremity function (Balance and Gait Parameters).
| Group B | Pre (Mean ± SD) | Post (Mean ± SD) | P value | df | t value | S/NS |
|---|---|---|---|---|---|---|
| PBS | 38.27 ± 4.27 | 42.27 ± 4.86 | .001 | 14 | -4.273 | S* |
| Stride length | 0.62 ±0.042 | 0.69 ± .046 | .000 | 14 | -8.7 | S* |
| Gait velocity | 57.6±5.26 | 59.53 ± 5.29 | .000 | 14 | -6.80 | S* |
| Cadence | 86.47±4.58 | 91.73±3.88 | .000 | 14 | -11.92 | S* |
Table 4: Pre and post intervention comparison of group b for pbs, stride length, gait velocity and cadence. P<0.05* shows a statistically significant result. NS-Non Significant, S- Significant. Above table shows the pre and post intervention level comparison of group B for PBS, stride length, gait velocity and cadence, the result shows significant result.
Results of this study is in agreement with study of Co Akosile et al. [39] who investigated the effect of an 8-week proprioceptive neuromuscular facilitation (PNF) treatment programmes on the functional ambulation of post-stroke individuals and concluded that PNF technique led to improvement in the functional ambulation of post stroke individuals.
A study done by Agnieszka Radziminska et al. [13] in which the effectiveness of the concept of PNF, proprioceptive neuromuscular facilitation paving work to improve the gait pattern in people (children and adults) with cerebral palsy was studied. An additional objective was to assess the impact of therapy on: ranges of motion in the joints of the lower limbs, improving the activity of preparing for gait, pathological gait pattern change. They concluded that PNF therapy method by science-specific methods of preparing for the activity of walking, improves the control of posture, which results in improving the efficiency of gait in persons with cerebral palsy. This favors finding of present study since our gait parameters improved significantly.
Another study completed by Deletis et al. [40] explained in detail about neuromuscular mechanism. They stated that in PNF position, sensory inputs from the periphery leads to stronger excitation of the cortical areas, leading to variations in the thresholds of a number of motor neurons, which was reflected in the motor evoked potentials. This was further supported by a study of Benecke et al. [41] which reported that the amount of sensory input coming from the periphery was greater in PNF position than in normal position, which induces changes in the excitability of the pyramidal tract and the final motor pathways.
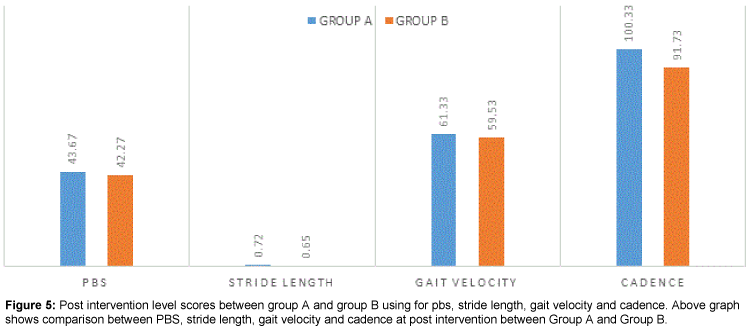
When post intervention comparison was done between group A and group B it was found that there was significant difference between both the groups on Stride length and cadence scores, whereas non-significant difference was found in PBS and Gait velocity scores as it is shown in Table 5 and Figure 5. Result of this study suggest that Task Oriented training group is better in improving stride length and cadence but both the intervention strategies are equally effective in improving balance and gait velocity of cerebral palsy child after 4 weeks of intervention.
| Group A (Mean ± SD) | Group B (Mean ± SD) | P Value | df | t value | S/NS | |
|---|---|---|---|---|---|---|
| PBS | 43.67 ± 2.77 | 42.27 ± 4.86 | .341 | 28 | 0.97 | NS |
| Stride length | 0.74 ± 0.046 | 0.68 ± .044 | .002 | 28 | 3.44 | S* |
| Gait velocity | 61.33±4.93 | 59.53 ± 5.29 | .344 | 28 | 0.963 | NS |
| Cadence | 100.33 ± 2.94 | 91.73 ± 3.88 | .000 | 28 | 6.84 | S* |
Table 5: Post intervention level scores between group a and group b for pbs, stride length, gait velocity and cadence. P<0.05* shows a statistically significant result. NS-NonSignificant, S- Significant. Above table shows the Post-intervention level comparison between group A and B for PBS, Stride Length, Gait velocity and Cadence, the result shows Significant Difference for stride length and cadence between both the groups but Non significant result for PBS and Gait Velocity.
There are various studies done in past to see effect of proprioceptive neuromuscular facilitation (PNF) exercise program on balance, lower extremity function and gait components and most of all having positive results [42-45].
The reason for better balance and lower extremity function in Proprioceptive Neuromuscular Facilitation (PNF) group may be due to the way it utilizes the different proprioceptive information for stimulating nerve and muscles function by utilizing distinct helical form pattern which is based on functional components to aid reaction of motor system located in muscles and joints, and turn human movements into patterns for various uses such as exercise intervention. Improvement of balance ability might have resulted from facilitation of proprioceptive sense, leading to change in various supports leads to increase in stability of joints. PNF have various exercises aim to improve stability and mobility components, once the desired stability components are achieved it mobility component further helps to improve function and later allows physiotherapist to work on skills components of patient. Ankle stability is required to treat instability in standing or walking and can be improved with extension of calf muscles. Ankle stability in this study might have been improved by the following activities: (1) Sit to stand (2) weight bearing activities for the ankle joint, and (3) activities for proprioceptive sensibility. As balance and ankle stability might have improved this would have further added for increase in gait speed.
Better scores in stride length and cadence in task oriented training group is matches with results of previous studies done to find out effectiveness of Task oriented training in improving balance and mobility functions [46-48].
This could be explained by better stability around both hip and knee that increases stability in stance so the subjects were able to take longer stride, which makes it easier for the ankle plantar flexors to push off actively. The increased stride length, cadence and push off corresponds well with the increase in muscle strength around the hips, knee and ankle. This may be due to task oriented training emphasizes specific training of motor control in everyday activities and represents a shift away from facilitation of movement and exercise therapy [12,49- 51]. Animal studies have demonstrated that task-specific training (e.g. skilled reaching task) can restore function by using spared (non-affected) parts of the brain which are generally adjacent to the lesion [52]. This involves intensive periods of task practice using shaping and progressive increments in task difficulty, feedback and encouragement [53].
Both PNF and Task Oriented training work on functional components, but task oriented training while taking functional components takes account of principles of specificity which allow therapist to work on specific components which is lacking or missing, in this study we follow this principle. It is recognized that ‘movement emerges from an interaction between the individual, the task, and the environment in which the task is being carried out.’ Wu et al. [54] concluded that the use of real and functional objects might be an effective way of facilitating efficient, smooth and coordinated movement with the impaired arm after stroke. This might be the reason why stride length and cadence has improved, but increased cadence and stride length finding unable to reflect on gait velocity components which may be due to limited 4 weeks’ duration of intervention.
No Children in either group reported adverse effects/discomfort with intervention. Children reported significant improvements in Gait and balance following Task- Oriented Approach and Proprioceptive Neuromuscular Facilitation Exercises. The Children in both groups showed significant improved lower extremity functions & clinical improvements too were evident.
Conclusion
The findings of the present study have important clinical implications for developing effective interventions in children with cerebral palsy when compared with conventional physiotherapy treatment for improving Balance and Gait. Task– Oriented Training and Proprioceptive Neuromuscular Facilitation can be easily incorporated in any rehabilitation technique. These approaches may be useful and promising intervention for other types of Cerebral Palsy and various neurological conditions such as Stroke, Parkinson’s disease, Multiple Sclerosis, and even in patients of Balance Disorders and Gait impairments who are at high risk of falls.
This study also has some Limitation, these are Small sample size, Shorter treatment duration i.e. only for 4 weeks, there was No follow up after 4 weeks of intervention and Repetition of each task was not fixed, progression was considered according to each child’s capacity. In future Follow up studies with larger sample size and longer duration can be done on other type of cerebral palsy, stroke, Parkinson’s disease & Multiple Sclerosis by keeping fixed number of repetition to see effect of Task- Oriented Approach and Proprioceptive Neuromuscular Facilitation.
From finding of this study it is concluded that both Task-Oriented Training and Proprioceptive Neuromuscular Facilitation Exercises both are beneficial in improving balance lower extremity function in children with cerebral palsy. However, children treated with Task – Oriented Approach showed benefit in terms of improvement in Stride length and Cadence as compared to Children treated with Proprioceptive Neuromuscular Facilitation Exercises who showed equal benefit in terms of improvement in Balance and Gait Velocity after 4 weeks of intervention.
References
- Mutch L, Alberman E, Hagberg B, Kodama K, Perat MV (1992) Cerebral palsy epidemiology: where are we now and where are we going? Dev Med Child Neurol 34: 547-551.
- Bax M, Goldstein M, Rosenbaum P, Leviton A, Paneth N, et al. (2005) Proposed definition and classification of cerebral palsy, April 2005. Dev Med Child Neurol 47: 571-576.
- Oskoui M, Coutinho F, Dykeman J, Jetté N, Pringsheim T (2013) An update on the prevalence of cerebral palsy: a systematic review and meta-analysis. Dev Med Child Neurol 55: 509-519.
- Wilson-Costello D, Friedman H, Minich N, Fanaroff AA, Hack M (2005) Improved survival rates with increased neurodevelopmental disability for extremely low birth weight infants in the 1990s. Pediatrics 115: 997-1003.
- Rojas VG, Rebolledo GM, Muñoz EG, Cortés NI, Gaete CB, et al. (2013) Differences in standing balance between patients with diplegic and hemiplegic cerebral palsy. Neural Regen Res. 8: 2478-2483.
- Wingert JR, Burton H, Sinclair RJ, Brunstrom JE, Damiano DL (2009) Joint-Position Sense and Kinesthesia in Cerebral Palsy. Arch Phys Med Rehabil 90: 447-453.
- Wren TA, Rethlefsen S, Kay RM (2005) Prevalence of specific gait abnormalities in children with cerebral palsy: influence of cerebral palsy subtype, age, and previous surgery. J Pediatr Orthop 25: 79-83.
- Shumway Cook A, Woollacott MH (2001) Motor Control. 2nd edtn, Lippincott Williams &Williams, Philadelphia, USA.
- Brown GT, Burns SA (2001) The efficacy of neurodevelopmental treatments in children: a systematic review. Br J Occup Ther 64: 235-244.
- Butler C, Darrah J (2001) Effects of neurodevelopmental treatment (NDT) for cerebral palsy: an AACPDM evidence report. Dev Med Child Neurol 43: 778-790.
- Tirosh E, Rabino S (1989) Physiotherapy for children with cerebral palsy. Evidence for its efficacy. Am J Dis Child 143: 552-555.
- Salem Y, Godwin EM (2009) Effects of task-oriented training on mobility function in children with cerebral palsy. Neurorehabilitation 24: 307-313.
- Radziminska A, Srokowski G, Bulatowicz I, Kazmierczak U, Strojek K, et al. (2012) Assessment of The PNF Method Influence On Gait Parameters Improvement in Persons with Cerebral Palsy. Journal of Health Sciences.
- Darrah J, Watkins B, Chen L, Bonin C; AACPDM (2004) Conductive education intervention for children with cerebral palsy: an AACPDM evidence report. Dev Med Child Neurol 46: 187-203.
- Pedersen AV (2000) Conductive education - a critical appraisal. Adv Physiother 2: 75-82.
- Ludwig S, Leggett P, Harstall C (2000) Conductive education for children with cerebral palsy. Edmonton, Alberta Heritage Foundation for Medical Research (AHFMR).
- French L, Nommensen A (1992) Conductive education evaluated: future directions. Aust Occup Ther J 39: 17-24.
- Lim H, Kim T (2013) Effects of vojta therapy on gait of children with spastic diplegia. J Phys Ther Sci 25: 1605-1608.
- Cohen HJ, Birch HG, Taft LT (1970) Some considerations for evaluating the Doman-Delacto "patterning" method. Pediatrics 45: 302-314.
- Bumin G1, Kayihan H (2001) Effectiveness of two different sensory-integration programmes for children with spastic diplegic cerebral palsy. Disabil Rehabil 23: 394-399.
- Anttila H, Suoranta J, Malmivaara A, Mäkelä M, Autti-Rämö I (2008) Effectiveness of physiotherapy and conductive education interventions in children with cerebral palsy: a focused review. Am J Phys Med Rehabil 87: 478-501.
- Hur JJ (1995) Review of research on therapeutic interventions for children with cerebral palsy. Acta Neurol Scand 91: 423-432.
- Kunz R, Autti-Rämö I, Anttila H, Malmivaara A, Mäkelä M (2006) A systematic review finds that methodological quality is better than its reputation but can be improved in physiotherapy trials in childhood cerebral palsy. J Clin Epidemiol 59: 1239-1248.
- Horak FB (1990) Assumptions Underlying Motor Control for Neurologic Rehabilitation, In. Jodi Crompton, Christine Imms, Anne T McCoy, et al. (2007) Group-based task-related training for children with cerebral palsy: a pilot study. Phys Occup Ther Pediatr 27: 43-65.
- Flinn N (1995) A task-oriented approach to the treatment of a client with hemiplegia. Am J Occup Ther 49: 560-569.
- Rensink M, Schuurmans M, Lindeman E, Hafsteinsdóttir T (2009) Task-oriented training in rehabilitation after stroke: systematic review. J Adv Nurs 65: 737-754.
- Klein DA, Stone WJ, Phillips WT, Gangi J, Hartman S (2002) PNF training and physical function in assisted-living older adults. J Aging Phys Act 10: 476-488.
- Chen JC, Shaw FZ (2014) Progress in sensorimotor rehabilitative physical therapy programs for stroke patients. World J Clin Cases 16: 316-326.
- Franjoine MR1, Gunther JS, Taylor MJ (2003) Pediatric Balance Scale: A Modified Version of the Berg Balance Scale for the School-Age Child with Mild to Moderate Motor Impairment. Pediatr Phys Ther 15: 114-128.
- Her JG, Woo JH, Ko JY (2012) Reliability of the Pediatric Balance Scale (PBS) in the Assessment of the Children with Cerebral Palsy. Phys Ther Sci 24: 301-305.
- Chrysagis N, Skordilis EK, Koutsouki D (2014) Validity and clinical utility of functional assessments in children with cerebral palsy. Arch Phys Med Rehabil 95: 369-374.
- Pirpiris M, Wilkinson AJ, Rodda J, Nguyen TC, Baker RJ, et al. (2003) Walking speed in children and young adults with neuromuscular disease: Comparison between two assessment methods. Journal of Pediatric Orthopaedics 23: 302-307.
- Wade DT (1992) Measurement in Neurological Rehabilitation. Oxford University Press, United Kingdom.
- Yang YR, Wang RY, Lin KH, Chu MY, Chan RC (2006) Task-oriented progressive resistance strength training improves muscle strength and functional performance in individuals with stroke. Clin Rehabil 20: 860-870.
- Frimpong E, Olawale OA, Antwi DA, Antwi-Boasiako C, Dzudzor B (2014) Task-oriented circuit training improves ambulatory functions in acute stroke: a randomized controlled trial. Journal of Medicine and Medical Sciences 5: 169-175.
- Wevers L, van de Port I, Vermue M, Mead G, Kwakkel G (2009) Effects of Task-Oriented Circuit Class Training on Walking Competency After Stroke A Systematic Review. Stroke 40: 2450-2459.
- Kumar C, Kataria S (2013) Effectiveness of Task Oriented Circuit Training on Functional Mobility and Balance in Cerebral Palsy. Indian Journal of Physiotherapy and Occupational Therapy 7: 23-28.
- Kim BH, Lee SM, Bae YH, Yu JH, Kim TH (2012) The Effect of a Task-oriented Training on Trunk Control Ability, Balance and Gait of Stroke Patients. J Phys Ther Sci 24: 519-522.
- Akosile CO, Adegoke BAO, Johnson OE, Maruf FA (2011) Effects of Proprioceptive Neuromuscular Facilitation Technique on the Functional Ambulation of Stroke Survivors. Journal of The Nigeria Society of Physiotherapy 18: 1-2.
- Deletis V, Dimitrijevic MR, Sherwood AM (1987) Effects of electrically induced afferent input from limb nerves on the excitability of the human motor cortex. Neurosurgery 20: 195-197.
- Benecke R, Meyer BV, Gohmann M, Conrad B (1988) Analysis of muscle responses elicited by transcranial stimulation of the corticospinal system in man. Electroencephalography and Clinical Neurophysiology 69: 412-422.
- Pereira MP, Goncalves M (2012) Proprioceptive Neuromuscular Facilitation Improves Balance and Knee Extensors Strength of Older Fallers. ISRN Rehabilitation.
- Khanal D, Singaravelan RM, Khatri SM (2013) Effectiveness of Pelvic Proprioceptive Neuromuscular Facilitation Technique on Facilitation of Trunk Movement in Hemiparetic Stroke Patients. IOSR Journal of Dental and Medical Sciences 3: 29-37.
- Kumar S, Kumar A, Kaur J (2012) Effect of PNF Technique on Gait Parameters and Functional Mobility in Hemiparetic Patients. Journal of Exercise Science and Physiotherapy 8: 67-73.
- Wang RY (1994) Effect of proprioceptive neuromuscular facilitation on the gait of patients with hemiplegia of long and short duration. Phys Ther 74: 1108-1115.
- Katz-Leurer M, Rotem H, Keren O, Meyer S (2009) The effects of a ‘home-based’ task-oriented exercise programme on motor and balance performance in children with spastic cerebral palsy and severe traumatic brain injury. Clin Rehabil 23: 714-724.
- Kim Y, Lee BH (2013) Clinical Usefulness of Child-centered Task-oriented Training on Balance Ability in Cerebral Palsy. J Phys Ther Sci 25: 947-951.
- Kumban W, Amatachaya S, Emasithi A, Siritaratiwat W (2013) Effects of task-specific training on functional ability in children with mild to moderate cerebral palsy. Dev Neurorehabil 16: 410-417.
- Pang MY (2014) Task-specific and impairment-based training improve walking ability in stroke. J Physiother 60: 110.
- Dean CM, Richards CL, Malouin F (2000) Task-Related Circuit Training Improves Performance of Locomotor Tasks in Chronic Stroke: A Randomized, Controlled Pilot Trial. Arch Phys Med Rehabil 81: 409-417.
- Salbach NM, Mayo NE, Wood-Dauphinee S, Hanley JA, Richards CL (2004) A task-orientated intervention enhances walking distance and speed in the first year post stroke: a randomized controlled trial. Clin Rehabil 18: 509-519.
- Nudo RJ, Milliken GW (1996) Reorganization of movement representations in primary motor cortex following focal ischemic infarcts in adult squirrel monkeys. J Neurophysiol 75: 2144-2149.
- Wolf SL, Blanton S, Baer H, Breshears J, Butler AJ (2002) Repetitive task practice: a critical review of constraint-induced movement therapy in stroke. Neurologist 8: 325-338.
- Wu CY, Trombly CA, Lin KC, Tickle-Degnen L (2000) A kinematic study of contextual effects on reaching performance in persons with and without stroke: influences of object availability. Arch Phys Med Rehabil 81: 95-101.
Relevant Topics
- Electrical stimulation
- High Intensity Exercise
- Muscle Movements
- Musculoskeletal Physical Therapy
- Musculoskeletal Physiotherapy
- Neurophysiotherapy
- Neuroplasticity
- Neuropsychiatric drugs
- Physical Activity
- Physical Fitness
- Physical Medicine
- Physical Therapy
- Precision Rehabilitation
- Scapular Mobilization
- Sleep Disorders
- Sports and Physical Activity
- Sports Physical Therapy
Recommended Journals
Article Tools
Article Usage
- Total views: 15984
- [From(publication date):
June-2016 - Jul 19, 2025] - Breakdown by view type
- HTML page views : 14562
- PDF downloads : 1422