Research Article Open Access
Comparison between Tai Chi and Balance-Strength Training Exercise to Decrease Fear of Fall and Improving Balance and Functional Mobility in Elderly
Chandan Kumar*Department Of Physiotherapy, School of Allied Health Sciences, Sharda University, Neurological Physiotherapy, India
- *Corresponding Author:
- Chandan Kumar
Department Of Physiotherapy, School of Allied Health Sciences
Sharda University, Neurological Physiotherapy, India
Tel: +918087518006
E-mail: ptchandan221@yahoo.co.in
Received date: February 11, 2017; Accepted date: April 24, 2017; Published date: May 01, 2017
Citation: Kumar C (2017) Comparison between Tai Chi and Balance-Strength Training Exercise to Decrease Fear of Fall and Improving Balance and Functional Mobility in Elderly. J Nov Physiother 7:350. doi: 10.4172/2165-7025.1000350
Copyright: © 2017 Kumar C. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Novel Physiotherapies
Abstract
Background of the study: Falls in older people are a common and important problem that can have devastating consequences for individuals and their support networks. The purpose of this trial is to compare the effect of two types of exercise, Tai Chi versus Balance and strength training (BS Training) to reduce fear of fall and to improve balance and functional mobility in elderly.
Method: It was a two-group, single-blind, randomized clinical trial in subjects, and aged 60-80 years old. They were divided in 2 equal groups; Group A was Tai Chi group and Group B was B.S. training group. Exercises were given for both the groups 5 days in a week for 8 weeks, Study outcome include fear of fall (Fall Efficacy Scale- FES), Balance (Berg Balance Scale -BBS) and Function Mobility (Timed up and go test -TUG).
Result: There were significant reduction in fear of fall and improvement in balance & functional Mobility in both the groups after 8 weeks of intervention. Tai Chi group had better effect as compare to the Balance-Strength training group in reducing fear of fall & improving Functional Mobility.
Conclusion: This study demonstrate that Tai Chi have better beneficial effects in reducing fear of fall and improving balance & functional mobility as compared to Balance-Strength training in elderly after 8 weeks of intervention.
Keywords
Tai Chi; Balance-strength training; Fall; Elderly; Balance; Fear of fall; Functional mobility
Introduction
Worldwide, about 424,000 individuals die each year from falls, of which the vast majority are in low- and middle-income countries, and a further 37.3 million falls require medical attention [1]. Falls in the elderly are considered one of the most serious and expensive public health problems in terms of morbidity, mortality, and enormous costs to health and social services. Worldwide, approximately 28 to 35% of people of 65 years of age fall each year, increasing to 32-42% for those over 70 years [2-4]. Fall prevention is currently emphasized by the public health system because it is considered an indicator of the quality of service provided to the elderly [5]. Falls are considered a geriatric syndrome that is associated with extrinsic and intrinsic factors. The extrinsic causes are usually related to the home environment such as rugs, stairs, and poor lighting. While the intrinsic causes are related to an impairment in balance or gait, muscle weakness, decreased visual acuity, cognitive deficits, the presence of chronic disease, postural hypotension or the use of psychotropic medication [5-7].
Exercise is an obvious choice as a fall prevention intervention because impaired muscle strength and poor postural control are known to increase the risk of falling and are amendable to change with exercise [8,9]. Common Physiotherapy intervention for falls is Strength Training [10], Balance Training [11], Endurance Training [12], Perturbation Training [13] and Tai Chi [14]. The rehabilitation of falls prevention mostly concentrate on Balance & strength Training. The basic principles of strength training involve manipulations of no of repetitions, sets, exercise and force to cause desired change in strength, primarily focus on strengthening of anti-gravity muscles of lower extremity and trunk muscles. The benefits of strength training include increase muscle strength in elderly and postural support in elderly.
Exercise programs that challenge balance is more effective in preventing falls than programs that do not challenge balance. Balance training starts from the static balance then progresses to the dynamic balance [11].
Tai chi exercise is a type of exercise that mainly used for improving the strength and balance. There are 8 different postures of the Tai chi (yang type). Yang type is used because it is easy to understand and easy to perform [15]. There are various studies available which provide evidence that both the balance and strength training and Tai chi is effective in improving balance and functional mobility in elderly [10,11,16,17]. There is lack of evidence which compare the better strategies between these two interventions. There is a need of study to find out better treatment strategies between Tai Chi and balancestrength training to improve balance, functional mobility and to reduce fear of fall.
Aim of study
To find out better interventions strategies between tai chi and balance-strength training exercises in reducing fear of fall and improving balance and functional mobility in elderly.
Methodology
This study was a Single Blinded Randomized clinical trial of total 60 subjects. We recruited subjects from Matoshri old Age Home, MGM Physiotherapy OPD, MGM Hospital, and Others old age homes in Aurangabad. Participants were randomly selected into the study following simple random sampling using Lottery method. Total duration of study was 12 months and duration of intervention was 8 weeks.
Inclusion Criteria were Subjects with minimum 2 history of fall in last 6 months, aged between 60 to 80 years and both genders. They we’re having capacity to walk independently had MMSE (Mini mental state examination) score greater than 23 and willing to participate in study.
Exclusion Criteria were any medical condition or disability that prevented participation in an exercise program, such as-Cancer, kidney disease, a recent fracture, uncontrolled diabetes, seizure disorder, Cardiovascular-related problems that prohibited exercise. Subjects with neurological problems that affect the balance, had fainting or dizzy spells and reported any cognitive, behavioral and perceptual problems excluded from study.
Intervention
Group A (Eight-form easy tai chi): The eight-form Easy Tai Chi follows a gradual, simple-to-difficult progression with the movement execution beginning with upper body motion (involving arm, shoulder, and trunk movements) and minimal demands on postural control. A general plan for an in-class practice session of Easy Tai Chi involve the following components (Table 1) [17].
| Form | Movement Direction And Number of Repetations |
| 1. Commencing form | Both hands rise to shoulder level |
| 2.Curving back arms (Repulse Monkey) | Right, left; 3 times each side |
| 3.Stepping sideways and moving arms (Grasp Peacock's Tail: ward off,rollback, press, push) | To the left, then to the right |
| 4.Moving hands (Wave Hands Like Clouds) | Left side leads, 3 times |
| 5.Diagonal strides (Fair Lady Works at shuttles | Left, then right |
| 6.Standing on one leg (Golden Cock Stand on one leg) | Right, then left |
| 7.Stepping and pushing (Brush Knees and twist step) | Left, then right |
| 8.closing form | Both hands fall to the side, left leg drawn to the right leg. |
Table 1: Names of the Forms in Eight-Form Easy Tai Chi [17].
Total exercise session involved 10 min warm-up, 30 min of practicing Easy Tai Chi movements/postures, and a 5 min cool-down. Five-minute breaks between practices should be there for the cool down.
Group B (Balance and strength training exercise): The Balance strength training program used in study to improve neuromuscular function (strength, balance and gait) and reduced fall risk factor [18]. This program complies with the American College of Sports Medicine (ACSM) recommendations for progressive resistance training for older adults is 10 Minutes warm up period, there are 8-10 exercises can be done for 8-12 repetitions 5 Minutes cool down period for 1-3 sets. Lower body strengthening exercises by using muscle groups and movement involved in everyday activities (chair rises, sit to stand, heel raise, toe raises, half squatting, lunges, forward, lateral, backward, walking) [19]. The balance exercise involves standing with decreased base, graded reaching in standing, stepping in different directions (Table 2).
| Type A) Strength Exercises | B) Balance Exercise |
| 1.Sit-to-stand- for progression and variety: | 1.Standing with decreased base- for progression: |
| Making it harder: | Making it harder: |
| • lowering the height | • Feet together and level |
| • don’t use hands to push off, cross arms across chest | • Semi-tandem stance |
| • changing the nature of the surface (e.g. softer chair) | • Tandem stance |
| • ask the person to stand up with most weight on one leg- the other leg can be placed in front or on a stool to ensure this | • Stand on one leg |
| Making it easier: | • Maintain position for longer 10seconds |
| • place a table in front of or beside the person for hand support | • Close eyes10seconds |
| • Give feedback to enable the task to be successfully completed (e.g. feet back behind your knees, move your shoulders forward) | Making it easier: |
| • structure the environment to assist performance e.g. markers on floor to show foot position. | • place a table beside the person for hand support |
| 2.Heel raises- v for progression and variety: | 2.Graded reaching in standing- v for progression: |
| Making it harder: | Making it harder: |
| • decrease hand support | • Foot placement-narrower, step standing |
| • hold the raise for longer | • Reaching further |
| • One leg at a time | • Reaching in different directions |
| • use a wedge to increase the range of motion | • Reaching down to a stool or the floor |
| Making it easier: | • Reaching for heavier objects |
| • place a table on one or both sides of the person for hand support or use their walking aid. | • Reaching for a full cup of water |
| 3.Toe rise–standing on a toe place a table on both the side of subject to prevent fall | • Standing on a softer surface e.g. foam rubber mat |
| 4.Half- squats sliding down a wall- | • Stepping while reaching |
| v for progression and variety: | Making it easier: |
| Making it harder: | • place a table beside the person for hand support |
| • increasing step height | • give feedback to enable the task to be successfully completed (e.g. keep your hips forward) |
| • adding weight (either vest or belt) | • structure the environment to enhance performance e.g. markers on floor to show foot position, an object to move hips towards. |
| • decrease hand support | Stepping in different directions-for progression: |
| • Step up and over block | Making it harder: |
| Making it easier: | • Narrow foot position |
| • place a table on one or both sides of the person for hand support or use their walking aid. | • Longer steps |
| Along with these exercises was an assessment of walking aids and a gait re-education program. | • Faster steps |
| • Step over objects | |
| • Choice component e.g. step forward with left foot | |
| • Incorporate pivoting on the non-stepping foot | |
| • Use different colours, numbers of letters or a clock face or coins as targets for variety | |
| Making it easier: | |
| • place a table beside the person for hand support | |
| All exercises were given 8 to 12 repetitions, duration for 5 minutes each and 5 times per week. | |
Table 2: Balance and strength training exercise.
There was 10 minutes’ warm up period before starting the exercise. The exercise range from 1-3 sets. In a single set 8-12 repetitions for the strength training and balance exercise. Total time requires was 40 to 45 minutes and 5 minutes’ rest period was there in between the exercises.
The all above exercises are given for 5 days in a week for 8 weeks. Physiotherapist who was blinded to study and group allocation used all outcome measures in the study.
An approval from MGM’s Institute of Health Sciences ethical committee was taken before starting the study. The Protocol number of Ethical Committee Approval was MGM-ECRHS/2015/211.
Outcome measures
• Fall efficacy scale: This scale is used for measure fear of fall in older persons. Fall efficacy scale, on scale from 1 to 10, with 1 being very confident and 10 being not confident at all. A total score of greater than 70 indicates that the person has fear of fall. Fall efficacy scale is reliable method to find out the fear of fall among elderly people [20,21].
• Berg balance scale 14 item scale, having 56 components designed to measure balance of the older Adults in a clinical setting. The berg balance scale is reliable and valid measure that is used to assess characteristic of balance [22,23].
• Time up and go test: this scale is used to assess the functional mobility of the subject. Person who ever performing this test should wear the light foot wear and stand from a chair and walks for 3 meter. Time up and go scale is having good reliability and validity to assess the functional mobility in old age patients [24,25].
Procedure
• Step 1: All the patients from specified source of data were assessed and those who fulfilled inclusion criteria participated in the study.
• Step 2: All sixty patients were randomly allocated in to two groups, Group A (Tai Chi Exercises) and Group B (Strength and Balance Training exercises), with 30 in each.
• Step 3: The procedure is explained to subjects and written informed consent have been taken.
• Step 4: All patients evaluated on the Berg Balance Scale, Time up and go test and fall efficacy scale at the base line before start the intervention.
• Step 5: In Group A Tai chi exercises, was given.
• Step 6: In group B balance and strength training exercises was given.
Therapist who used the outcome measure at pre and post intervention level was blinded to study and group division.
An approval from MGM’s Institute of Health Sciences ethical committee was taken before starting the study. The Protocol number of Ethical Committee Approval was MGM-ECRHS/2014/132.
Data Analysis
Data was analyzed and tabulated using SPSS version 20th (Statistical Package for Social Sciences). Mean, Standard deviation, degree of freedom, confidence interval, P value and significance were calculated to express the results.
Unpaired ‘t’ test has been done for Inter-Group Comparison of Berg balance Scale (BBS), Timed Up and Go Test (TUG) and Fall Efficacy Scale (FES) in between Group A and Group B for Pre-and Post- Interventional Values.
Levene’s Test for has been used Equality of Variances for two groups.
Paired t-test has been done for Intra-Group Comparison of BBS, TUG and FES within group A and Group B for Pre-and Post- Interventional Values.
The significant (Probability-P) has been selected as 0.05.
Result
Total 65 subjects were selected and out of which 3 were excluded because they refused to participate in the study and 2 were not able to complete the intervention of 8 weeks, so total 60 subjects were randomly allocated for intervention of 8 weeks, according to criteria in group A and group B, 30 patients in each group.
A total of 35 males and 25 females participated in the study. In Group A, 64% were male and 36% were females whereas in Group B, 54% were males and 46% were females. In total subjects 14% subjects were having intrinsic risk factor, 86% were having extrinsic risk factor in group A and group B respectively. In all subjects 31% were having Hypertension, 13% were having Diabetes mellitus and 55% were having no risk factor (Table 3).
| Group A | Group B | df | T Value | P Value | ||
| Age | 69.50 ± 5.46 | 68.30 ± 5.03 | 58 | 0.885 | 0.453# | |
| Gender | Male | 19 (64%) | 16 (54%) | |||
| Female | 11 (36%) | 14(46%) | ||||
| Risk factors | Intrinsic | 4(14%) | 4(14%) | |||
| Extrinsic | 26(86%) | 26(86%) | ||||
| Hypertension | 19 (31%) | |||||
| Diabetes Mellitus | 8 (13%) | |||||
| None | 33 (55%) | |||||
Table 3: Demographic detail of population.
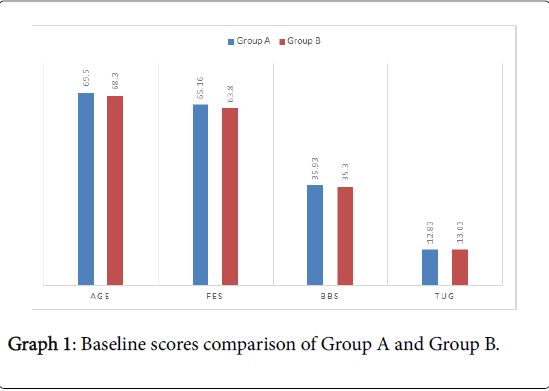
Table 4 shows baseline score comparison of FES, BBS and TUG in group A and group B, there is no significant difference.
| Outcome Measures | Group A | Group B | df | t value | P Value |
| FES | 65.16± 4.72 | 63.80± 5.97 | 58 | 0.983 | 0.330# |
| BBS | 35.93±3.71 | 35.30±2.94 | 58 | 0.731 | 0.467# |
| TUG | 12.83 ± 0.83 | 13.03±2.22 | 58 | -0.462 | 0.646# |
| P<0.05* shows a statistically not significant result. | |||||
| # for non-significance. | |||||
Table 4: Baseline scores comparison of Group A and Group B.
Graph 1 shows baseline score comparisons of Group A and Group B which suggest both the group were matched for baselines.
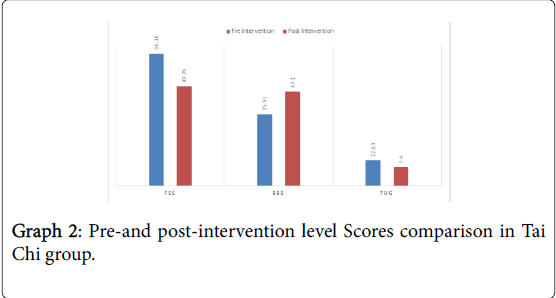
Graph 2 shows comparison of pre-and post-level scores in Group A.
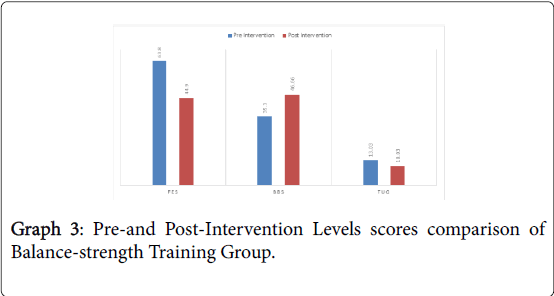
Table 6 shows Comparison of pre-and post-intervention level scores of FES, BBS and TUG in Group B, which suggest there is significant difference from pre-to post intervention level.
Graph 3 shows Pre-and Post-Intervention Level scores comparison in Group B.
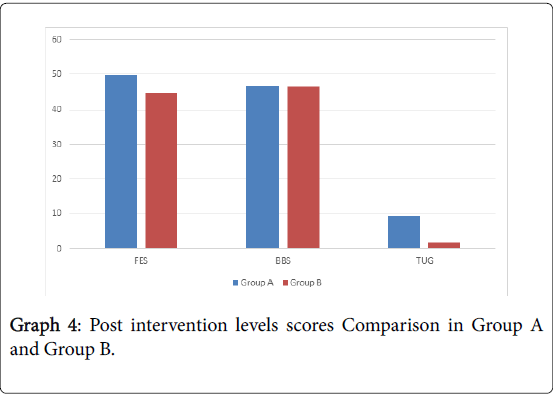
Table 7 shows the post intervention values of FES, BBS and TUG in group A and B, there is no significant change in BBS and there is significant change in FES and TUG respectively.
Graph 4 shows the post intervention values of FES, BBS and TUG in between group A and B, there is no significant change in BBS and there is significant change in FES and TUG.
Discussion
Analysis of the data was done first at baseline level, among both the groups, then pre-and post-intervention level comparison was done for both the groups and in last post intervention level comparison was done between groups A and group B.
Demographic information of participants, for groups showing that subjects were matched for baseline characteristics as it seen in Table 3 and graph 1. Age, Gender distribution and risk factor among subjects in the groups is shown in Table 3.
When analysis was done at pre-intervention level between both the groups, it was found that there was statically no significant difference between FES, BBS and TUG scores between both the groups, as it is shown in Table 3 and graph 1, which suggest that both the group were matched for baseline.
When comparison was done at pre-and post-intervention level for group A, it was found that there was statistically significant difference for BBS, TUG and FES score at post intervention level as it in Table 5 and Graph 2 respectively. This shows that Tai Chi balance training exercises are effective in improving balance, improves functional mobility and reduces the fear of fall.
| Pre-Intervention | Post Intervention | df | t value | P Value | |
| FES | 65.16 ± 4.72 | 49.76±1.27 | 29 | 17.63 | 0.001* |
| BBS | 35.93 ± 3.71 | 47.10±3.41 | 29 | -13.79 | 0.001* |
| TUG | 12.83 ± 0.83 | 9.40±0.49 | 29 | 21.9 | 0.001* |
| P<0.05* shows a statistically significant result | |||||
Table 5: Pre-and post-intervention level Scores comparison in Tai Chi group.
Finding of this study is supported by study done by Tousignant et al. [26] to find out Efficacy of supervised Tai Chi exercises versus conventional physical therapy exercises in fall prevention and they concluded that Tai Chi exercises as part of a rehabilitation program seem to be a more effective alternative to the conventional physical therapy exercises for this specific population [26].
Fuzhong et al. [27] is concluded a study in which they concluded that practicing Tai Chi regularly may help develop balance mechanisms and minimize instability to counter potentially destabilizing body positions, or to overcome environmental hazards in older individuals at risk of falling. Improved functional balance through Tai Chi training is associated with subsequent reductions in fall frequency in older persons [27].
When comparison was done at pre-and post-intervention level in group B, it was found that there is statistically significant difference between FES, BBS and TUG scores at post intervention level as it is shown in Table 6 and graph 3, which shows that balance-strength training is also effective in improving functional mobility and balance and reducing fear of fall after 8 weeks of intervention.
| Outcome Measures | Pre-Intervention | Post –Intervention | df | t value | P Value |
| FES | 63.80 ± 5.97 | 44.90±5.18 | 29 | 15.05 | 0.001* |
| BBS | 35.30 ± 2.94 | 46.66±2.84 | 29 | -14.66 | 0.001* |
| TUG | 13.03 ± 2.22 | 10.03±0.99 | 29 | 10.73 | 0.001* |
| P<0.05* shows a statistically significant result | |||||
Table 6: Pre-and Post-Intervention Levels scores comparison of Balance-strength Training Group.
Finding of this study is similar to study done by on Effects of strength and balance training on the mobility, fear of falling and grip strength of elderly female fallers who concluded that Balance training consisting of virtual reality and strengthening exercises proved to be an effective tool to reduce the fear of falling and to improve the mobility of elderly female fallers, and may be an acceptable treatment for the prevention of falls and balance recovery [28].
In the present study, significant improvement in reducing fear of fall and improving balance & mobility was observed in the faller group after the Balance -strength training program. These results can be explained by the fact that an intervention comprising balance and strength training responsible for maintaining postural stability, increases the recruitment of motor neurons, muscle fatigue resistance and hypertrophy (mainly type II fibers), thus improving muscle strength, muscle reaction time, coordination, balance and mobility factors are important for the prevention of falls [29,30]. Muscle strengthening (performed in a conventional manner or incorporated into ADL) appears to be essential to fall prevention; all of the highquality studies showed a reduction in falls [31,32].
Another study conducted on “balance & strength training exercise” in elderly populations and concluded that it improves the balance. This study shows better effect on the antigravity muscles it not only improves the strength, but maintains the strength of muscles also [33].
When comparison was done at post intervention level between the group A and group B, it was found that there was statistically significant difference in FES & TUG but there was no significant difference in BBS as it is shown in Table 7 and graph 4. Which shows that Tai chi is more effective in improving functional mobility and reducing fear of fall as compared to balance-strength training.
| Outcome Measures | Group A | Group B | df | t value | P Value |
| FES | 49.76±1.27 | 44.90±5.18 | 58 | 4.99 | 0.001 * |
| BBS | 47.10 ±3.41 | 46.66±2.84 | 58 | 0.534 | 0.596 # |
| TUG | 9.40±0.49 | 10.03±0.99 | 58 | -3.1 | 0.003 * |
| P<0.05* shows a statistically not significant result | |||||
| #for non-significance | |||||
Table 7: Post Intervention Levels Scores Comparison of Group A and Group B.
Finding of this study is supported by the intervention of Kerri m winter stone et al on women with cancer the purpose of the GET FIT (Group Exercise Training for Functional Improvement after Treatment) trial is to compare the efficacy of two distinct types of exercise, tai chi versus strength training, to prevent falls in women who have completed treatment for cancer. This study conclude that the Tai chi exercise have better effect on improving balance and strength in women who have completed the treatment of cancer, it helps to maintain the strength [34].
Although balance(BBS) improvements were equally seen in both the groups but greater amount of improvement in functional mobility and reducing fear of fall was noted in group A (Tai Chi) after 8 weeks of intervention. There was significant difference between group A and B on reducing fear of fall (FES) and improving functional Mobility (TUG). Therefore, the null hypothesis is rejected and thus the alternate hypothesis is accepted.
This study conclude that the Tai chi exercise have better effect on improving balance and strength. The better improvement in Tai Chi group is done as Tai Chi is a moderate intensity exercise that is beneficial to flexibility, and balance control; it improves muscle strength and reduces the risk of falls in the elderly. There is much evidence from clinical trials and exercise intervention for the beneficial effects of Tai Chi exercise on balance-strength in elderly people [35].
Tai Chi exercise is having effect on balance, stability, and strength. Tai Chi exercise demands precise joint movement, stability and balance. In performing Tai Chi, the roles of the muscles continually change between those of stabilizers and movers, weight-bearers and non-weight bearers, and between contraction and relaxation. It has been suggested that the practice of Tai Chi may increase the repertoire of motor programs stored in the brain, and therefore serve to train the various balance systems to promote greater steadiness. Cross sectional studies have provided positive evidence that Tai Chi has beneficial effects on balance and flexibility [17,36].
Li reported that Tai Chi practitioners were significantly better at performing right and left single leg stances with their eyes open and heel to the walking than non-practitioners [36]. The beneficial effects of low intensity Tai Chi exercise on the maintenance or gains in the balance and strength of older adults has also been shown by Wolfson et al. [37] they concluded that Tai Chi intervention has helped alleviate joint pain and has increased strength, flexibility [37].
Poor balance capacity, decreased muscle strength and flexibility, and the changes in gait that come with ageing are some of the risk factors associated with falls, Tai Chi exercise emphasizes continuous slow movement, with small to large expressions of motion, unilateral to bilateral shifts of body weight, the progressive flexion of the knees, and rotation of the trunk, head, and extremities. These movement components seem to help to reduce the risk factors of falling. The regular practice of Tai Chi could reduce the loss of bone mass density in the elderly [38].
The improved muscle activation in conjunction with decreased fear of falling may explain the improved performance of elderly fallers in the TUG test.
Clinical Implication
This study has important clinical implication for developing balance and strength in subjects with fall by incorporating Tai Chi exercise when compared with Strength - Balance Training for reducing fear of fall and to improves balance & functional mobility.
Limitations
Small sample size, so the result cannot be generalized.
Treatment effectiveness was examined only 8 weeks after treatment. No follow up was taken, whether improvements in motor functions can be attained after cessation of treatment.
Future Research
Future clinical trial study can be carried out on a larger sample size with long term follow up.
A similar study can be conducted with some objective measure to find of changes in strength, reaction time, static & dynamic balance components and gait parameters.
Further studies are needed to investigate the long-term effects of Strength - Balance Training in elderly population when compared with Tai Chi exercise.
Conclusion
This study demonstrate that Tai Chi have better beneficial effects in reducing fear of fall & and improving balance & functional Mobility as compared to Balance-Strength training in elderly after 8 weeks of intervention.
References
- World Health Organization (WHO) (2007) WHO global report on falls prevention in older age. Geneva: WHO2007.
- Cao ZB, Maeda A, Shima N, Kurata H, Nishizono H (2007) The effect of a 12-week combined exercise intervention program on physical performance and gait kinematics in community-dwelling elderly women. J PhysiolAnthropol 26:325-332.
- Carregaro RL, Toledo AM (2008) Efeitosfisiológicos e evidênciascientíficas da eficácia da fisioterapiaaquática. Rev Mov1:23-27.
- Kumar SJ, Vendhan GV, Sachin A, Tiwari M, Sharma VP (2008) Relationship between fear of falling, balance impairment and functional mobility in community dwelling elderly. Indian J Phys Med Rehabil19:48-52.
- Rubenstein LZ, Powers CM, MaClean CH (2001) Quality indicators for the management and prevention of falls and mobility problems in vulnerable elders. Ann Intern Med 135:686-693.
- Garcia RR,Gelsi TA, Sabaté ACC (2007) A percepção dos fatores de riscoparaquedasem um grupo de idosas. Rev Bras CiênSaúdeIII:41-51.
- Lord SR, Menz HB, Tiedemann A (2003) A physiological profile approach to falls risk assessment and prevention. PhysTher83:237-252.
- Howe TE, Rochester L, Neil F, Skelton DA, Ballinger C (2011) Exercise for improving balance in older people. Cochrane Database Syst Rev.
- Liu CJ, Latham N (2009) Progressive resistance strength training for improving physical function in older adults. Cochrane Database Syst Rev.
- Sherrington C, Whitney JC, Lord SR, Herbert RD, Cumming RG, et al. (2008) Effective Exercise for the Prevention of Falls: A Systematic Review and Meta- Analysis. Journal of the American Geriatrics Society 56: 2234-2243.
- Sherrington C, Tiedemann A, Fairhall N, Close JCT, Lord SR (2011) Exercise to prevent falls in older adults: an updated meta-analysis and best practice recommendations. NSW Public Health Bulletin 22: 78-83.
- Buchner DM, Cress ME, de Lateur BJ, Esselman PC, margherita AJ, et al. (1997) The effect of strength and endurance training on gait, balance, fall risk, and health services use in community-living older adults. J Gerontol A BiolSci Med Sci52: M218-224.
- Mansfield A, Peters AL, Liu BA, Maki BE (2007) A perturbation-based balance training program for older adults: study protocol for a randomised controlled trial.BMC Geriatrics 7: 12.
- Hackney ME, Wolf SL (2014) Impact of tai chi chu'an practice on balance and mobility in older adults: An integrative review of 20 years of research. Journal of geriatric physical therapy 37: 127-135.
- Shaw JM, Snow (1998) Weighted vest exercise improves indices of fall risk in older women. Journals of Gerontology 53A: 53-58.
- Logghe IH, Verhagen AP, Rademaker AC, Bierma-Zeinstra SM, van Rossum E, et al.(2010) The effects of Tai Chi on fall prevention, fear of falling and balance in older people: A meta-analysis. Preventive Medicine Preventive Medicine 51: 222-227.
- Liu H, Frank A (2010) Tai Chi as a Balance Improvement Exercise for Older Adults: A Systematic Review. Journal of Geriatric Physical Therapy33: 103-109.
- Li F, Fisher KJ, Harmer P, Shirai M (2003) A Simpler Eight-Form Easy Tai Chi for Elderly Adults. J Aging and Physical Activity 11: 206-218.
- Schmitz KH, Courneya KS, Matthews C (2010) American college of sports medicine roundtable on exercise guidelines for cancer survivors. Med Sci Sports Exerc 42: 1409-1426.
- Tinetti MD, Richman (1990) "Falls efficacy as a measure of fear of falling." Journal of gerontology 45: P239-243.
- SchepensS (2012) Relationship between Fall-Related Efficacy and Activity Engagement in Community-Dwelling Older Adults: A Meta-Analytic Review. Am J OccupTher66: 137-148.
- Conradsson M, Lundin-Olsson L, Lindelof N, Littbrand H, Malmqvist L, et al. (2007) "Berg balance scale: intrarater test-retest reliability among older people dependent in activities of daily living and living in residential care facilities." Physical Therapy 87: 1155-1163.
- Shumway-Cook A, Baldwin M, Polissar NL, Gruber W (1997) "Predicting the probability for falls in community-dwelling older adults." Physical Therapy 77: 812-819.
- Cook S (2000) Predicting the probability for fall in community dwelling older adults using time up and go test.Phys therapy 80: 896-903.
- Nordin E, Rosendahl E (2006) Timed ''Up & Go'' Test: Reliability in Older People Dependent in Activities of Daily Living focus on cognitive status. Physical Therapy86: 646-655.
- Tousignant M, Corriveau H, Roy PM, Desrosiers J, Dubuc N, Hébert R (2013) Efficacy of supervised Tai Chi exercises versus conventional physical therapy exercises in fall prevention for frail older adults: a randomized controlled trial. DisabilRehabil 35: 1429-1435.
- Fuzhong Li , Harmer P , Fisher KJ , Mcauley E (2004) Tai Chi: Improving Functional Balance and Predicting Subsequent Falls in Older Persons. Medicine& Science In Sports & Exercise pp.: 2046-2052.
- Prata MG (2015) Marcos Eduardo Schleicher -Effects of strength and balance training on the mobility, fear of falling and grip strength of elderly female fallers. journal of bodywork & Movement Therapy 19: 646-650.
- Casale R, Rainold A, Nilsson J, Bellotti P (2003) Can continuous physical training counteract aging effect on myoelectric fatigue? A surface electromyography study application. Arch Phys Med Rehabil 84: 513-517.
- Karinkanta S, Nupponen R, Heinonen A, Pasanen M, Sievanen H, et al.(2012) Effects of exercise on health-related quality of life and fear of falling in home-dwelling older women. J Aging Phys Activity 20: 198-214.
- Clemson l, Singh MAF, Bundy A, Cumming RG, Manollaras K, et al. (2012) Integration of balance and strength training into daily life activity to reduce rate of falls in older people (the LiFE study): randomised parallel trial. BMJ 345:4547-4547.
- Clemson L, Singh MF, Bundy A, Cumming RG, Weissel E, et al. (2010) LiFE pilot study: a randomised trial of balance and strength training embedded in daily life activity to reduce falls in older adults. AustOccupTher J 57:42-50.
- Wai-mun Pin T (2007)Balance and strenght training exercise in elderly. Report number 19:6273.
- Winters-Stone KM, Li F, Horak F, Luoh SW, Bennett JA, et al. (2012) Comparison of tai chi vs. strength training for fall prevention among female cancer survivors: study protocol for the GET FIT trial. BMC Cancer 577:232-236.
- Leung DPKM (2011) Tai Chi as an Intervention to Improve Balance and Reduce Falls in Older Adults: A Systematic and Meta-analytical Review. Alternative Therapies in Health and Medicine 17:40-48.
- Li JX, Hong Y, Chan Br KM (2001) Tai chi: physiological characteristics and beneficial effects on health. J Sports Med 35:148-156.
- Wolfson L, Whipple R, Derby C, Judge J, King M, et al. (1996) Balance and strength training in older adults: intervention gains and Tai Chi maintenance. J Am GeriatrSoc 44:498-506.
- Kirsteins AE, Dietz F,Hwang SM(1991)Evaluating the safety and potential use of a weight-bearing exercise, Tai-Chi Chuan, for rheumatoid arthritis patients. Am J Phys Med Rehabil 70:136-141.
Relevant Topics
- Electrical stimulation
- High Intensity Exercise
- Muscle Movements
- Musculoskeletal Physical Therapy
- Musculoskeletal Physiotherapy
- Neurophysiotherapy
- Neuroplasticity
- Neuropsychiatric drugs
- Physical Activity
- Physical Fitness
- Physical Medicine
- Physical Therapy
- Precision Rehabilitation
- Scapular Mobilization
- Sleep Disorders
- Sports and Physical Activity
- Sports Physical Therapy
Recommended Journals
Article Tools
Article Usage
- Total views: 5865
- [From(publication date):
June-2017 - Apr 02, 2025] - Breakdown by view type
- HTML page views : 4804
- PDF downloads : 1061