Comparing the Type of Delays in Oral Cancer: A Systematic Review and Meta-Analysis
Received: 07-Jan-2022 / Manuscript No. JCD-22-51341 / Editor assigned: 10-Jan-2022 / PreQC No. JCD-22-51341(PQ) / Reviewed: 24-Jan-2022 / QC No. JCD-22-51341 / Revised: 28-Jan-2022 / Manuscript No. JCD-22-51341(R) / Accepted Date: 31-Jan-2022 / Published Date: 04-Feb-2022 DOI: 10.4172/2476-2253.1000137
Abstract
Aims: This meta-analysis aims to explore the types of delays which are generally found in the patients suffering from oral cancer at different point times from onset of symptoms to initiation of appropriate treatment. It compares the mean delay time of head and neck cancer patients from different studies.
Methods: A comprehensive systematic literature search was carried out to find studies published from 2000 to 2020 from different database. We searched online databases z- library, Google Scholar PubMed, and Embase for articles which were dealing with oral (head and neck cancer). The language of literature included is English. We have used three delays classified as primary, secondary and tertiary delay. On the basis of inclusion and exclusion criteria, studies are included in the study. Studies having mean, SD and median delay time were considered. For the conduction of meta-analysis, forest plot is constructed and the mean delay in any type of delay is compared with one another.
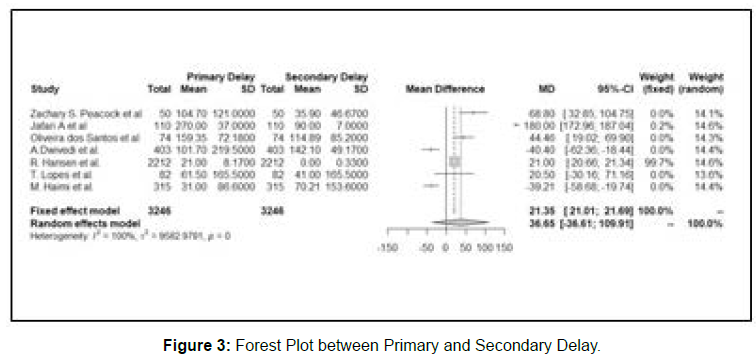
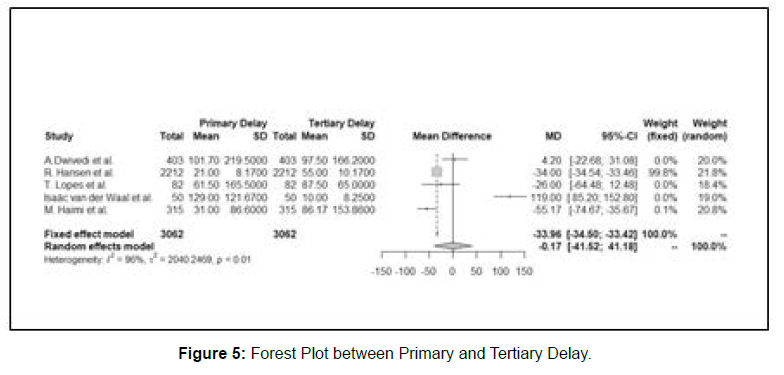
Results: Overall, 10 studies comprising of 4344 patients met our inclusion criteria and are included in our study. The studies in which primary delay data was available were 9 comprising of 3769 cases. For secondary delay, 8 studies and 3864 cases were taken in which data for mean, range and median delay was available. For tertiary delay secondary 5 studies and 2344 cases were taken in which data for mean, sd, range and median delay was available. The mean for primary delay was 55.91, for secondary delay was 33.39 and for tertiary delay was 55.17. The Forest Plot for the comparisons of Primary vs Secondary, Secondary vs Tertiary and Primary vs Tertiary is also plotted to compare between the means of the different delays.
Conclusions: It is clear from the above results that: Primary Delay > Tertiary Delay > Secondary Delay. Efforts should be made in making the people aware about the symptoms of oral cancer and the factors causing it. People should be educated about the health outcomes and results which are caused due to delay in consulting with the specialist as soon as possible.
Keywords: Oral Cancer; Head and neck cancer; Delays in oral cancer; Patients delay; Diagnostic delay; Treatment delay
Keywords
Oral Cancer; Head and neck cancer; Delays in oral cancer; Patients delay; Diagnostic delay; Treatment delay
Introduction
Cancers are generally categorized as one of the most major problems of human beings; however, oral cancer, especially in some specific regions such as South and Central Asia, is a recognized problem. Oral cancer has one of the lowest five-year survival rates among the major types of cancers, including breast, skin, testis, prostate, uterus, and urinary bladder cancers with survival rates of 50% or less . Early diagnosis is crucial for improving the survival rate. If the detected lesions are small localized and treated efficiently at initial stage; survival rates of 70 to 90% can be achieved [1].
Although oral cancer occurs in a part of the body that is readily accessible for early detection, most lesions are not diagnosed until they have reached advanced stages. For example, SCC in oropharynx has the same symptoms as pharyngitis and viral tonsillitis, and it may be confused with these diseases if the involved patients have been visited by a general practitioner and consequently this may be one of the main reasons of diagnosis and treatment delay.
In oral cancer, approximately 30% of patients wait for more than three months after symptom appraisal to seek help from a health care professional; this delay after symptom appraisal is an important determinant of prognosis and results in decreased survival rates [2]. Detecting oral cancer at an early stage is the most effective means of improving survival and reducing severe outcomes from the disease. Research also suggests that patient delay is influenced by symptom interpretation, knowledge of oral cancer, psychosocial factors as coping responses and barriers to seek help such as problems with access and their social circumstances and responsibilities.
Taken as a group, head and neck cancers (HNC) account for 4% of all cancers arising in Europe and are the eighth leading cause of cancer death worldwide. England has significantly lower age- and sexstandardised survival rates than other Northern and Central European countries, especially for laryngeal cancer, with over half (54%) diagnosed with regional or metastatic disease at diagnosis [3]. Five- Year survival is significantly better for localised (69%) than for regional (34%) or metastatic (8%) disease; it is thus important to understand the pathway to diagnosis and any factors which may influence its duration. Waiting time for diagnostic work-up and start of treatment may cause increased tumour growth, progressive disease stage and a poor outcome for head and neck cancer (HNC) patients.
Material and methods
Different articles which are published earlier present different definition of the delays in case of oral (Head and Neck cancer). In our article we have used the term Primary delay which is the time period between the onset of the first symptom of oral cancer and the meeting of the patient with the first medical practitioner. Generally, in other articles this delay is often referred to as Patient’s Delay. The Patient delay ranges from 7 days to 2 years in many articles reviewed as the patients are not themselves aware about the symptoms and treat it as a minor issue [4].
The second type of delay present in our article is Secondary delay. It is defined as the time period between the medical practitioner becoming aware of the problem and the correct diagnosis of the cancer. This delay generally includes two types of sub delays:
Doctor’s Delay: When the doctor is not able to judge the potential of the symptoms as they are minor.
Diagnostic Delay: Time period between doctor knowing the seriousness of the disease and its correct diagnosis. The third type of delay present in our article is Tertiary delay. It is often referred to as treatment delay which is the delay between correct diagnosis of disease and its correct treatment (Figure 1).
Search strategy
The study was conducted in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines. The online databases (PubMed, Embase, Google Scholar and z-library) from 2000 till 2020 were searched [5]. We did not impose any language restriction at the time of initial search. We also searched the reference list of included studies and earlier narrative/systematic reviews on the topic. The search strategy and the number of publication results corresponding to them is enumerated in Table 1.
| Search Database | Search Strategy | Publications |
|---|---|---|
| Pubmed | (Oral cancer), (Neck and Head cancer), delay in diagnosis), types of delay, Patients delay, (Treatment Delay, (Doctor’s Delay), follow up delay, ( (Reasons for Delay) |
101 |
| Embase | (Oral cancer), (Neck and Head cancer), delay in diagnosis), types of delay, Patients delay, (Treatment Delay, (Doctor’s Delay), follow up delay, ( (Reasons for Delay) |
152 |
| Google scholar | (Oral cancer), (Neck and Head cancer), delay in diagnosis), types of delay, Patients delay, (Treatment Delay, (Doctor’s Delay), follow up delay, ( (Reasons for Delay) |
79 |
| Scopus | (Oral cancer), (Neck and Head cancer), delay in diagnosis), types of delay, Patients delay, (Treatment Delay, (Doctor’s Delay), follow up delay, ( (Reasons for Delay) |
140 |
Table 1: The search strategy used and the number of results obtained for the four scientific literature databases- PubMed, Embase, Google Scholar and SCOPUS.
Study selection
After pooling all the studies extracted from online databases and other sources with their abstract and other publication details in a single excel file, we first screened the study titles, abstract and other publication details like author, year of publication, journal name, etc. for duplication. Thereafter, the titles and abstract of the remaining studies were checked for eligibility based on our inclusion and exclusion criteria [6].
Inclusion and exclusion criteria
We selected studies which satisfied the following inclusion criteria: (1) Only those studies are considered which are published between 2000 and 2020 (2) Only those studies are considered which are dealing with head and neck cancer, (3) English-language articles only and (4) original articles only [7].
The following information is extracted from all the articles: - lead author, publication year, country of study, type of study, number of patients enrolled, mean, sd and median for primary delay, mean, sd and median for secondary delay, mean, SD and median for tertiary delay [8]. Also range and Inter Quartile Range wherever available was extracted All the data were extracted on a standardized excel file.
Results And Analysis
Literature search
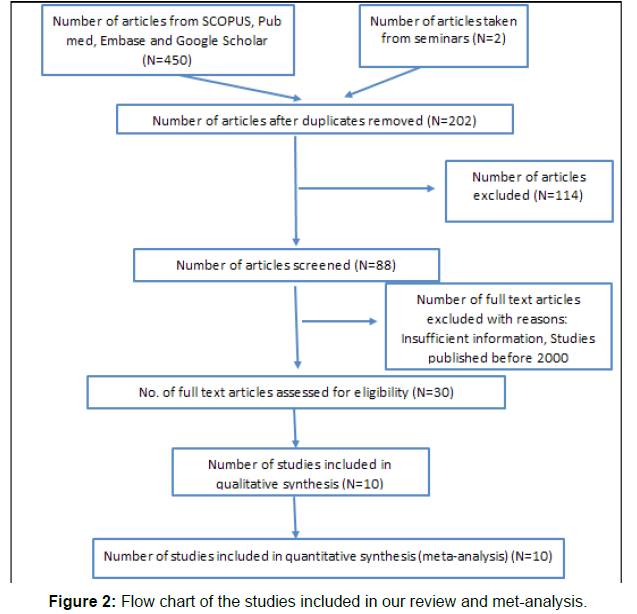
The search strategy used and the number of results obtained for the four scientific literature database- PubMed, Embase, z-library and Google Scholar- were as shown in Table 2. Four Fifty-Two (452) records were identified by the initial literature search, of which 250 were duplications. Then, out of remaining 202, 114 were excluded on the basis of title and abstract as per the exclusion criteria [9]. 30 full text articles were accessed for eligibility. Finally, 10 met our inclusion criteria and were included for systematic review and meta-analysis (Figure 2).
| Sr No | Author | Country | Year | Gender | Type of Study | Sample Size (Patients) |
Mean (days) |
Sd (days) |
|---|---|---|---|---|---|---|---|---|
| 1. | E. Grant et al. | Scotland | 2010 | Male=7 Female=8 |
Retrospective | 15 | 38.92 | 7.65 |
| 2. | Zachary S. Peacock et al. | San Francisco | 2008 | - | Cross -Sectional | 50 | 104.7 | 121 |
| 3. | Jafari A et al. | Iran | 2013 | Male=159 Female=97 |
Retrospective- Descriptive | 110 | 270 | 37 |
| 4. | Oliveira dos Santos et al. | Brazil | 2010 | Male=52 Female=22 |
Prospective – Cross-Sectional | 74 | 159.35 | 72.18 |
| 5. | A.Dwivedi et al. | India | 2012 | Male=161 Female=242 |
Cross-Sectional | 403 | 101.7 | 219.5 |
| 6. | R. Hansen et al. | Denmark | 2011 | - | Cohort Study | 2212 | 21 | 8.17 |
| 7. | T. Lopes et al. | Brazil | 2017 | Male=18 Female=82 |
Retrospective Cross-sectional | 82 | 61.5 | 165.5 |
| 8. | Isaäc van der Waal et al. | Netherlands | 2011 | - | Cross-Sectional | 50 | 129 | 121.67 |
| 9. | M. Haimi et al. | Israel | 2004 | - | Retrospective | 315 | 31 | 86.6 |
Table 2: Primary-delay study characteristics.
Study characteristics
The studies included in our studies were published between 1990 and 2020. Two of these studies were from India, two from Brazil and one each from Iran, Scotland, Netherlands, Israel, Denmark, San Francisco and Spain. There are Retrospective, Cross -Sectional, Retrospective- Descriptive, Prospective – Cross-Sectional and Cohort Study involved in our study [10]. The major characteristics of studies have been mentioned in Table 3-5. A total of 3311 patients in primary delay study, 3429 patients in Secondary delay and 3062 patients in tertiary delay study and evaluated. The number of patients amongst individual studies that were evaluated ranged from 15 to 2212 (Figure 3).
| Sr No | Author | Country | Year | Gender | Type of Study | Sample Size (Patients) |
Mean (days) | Sd (days) |
|---|---|---|---|---|---|---|---|---|
| 1. | Zachary S. Peacock et al. | San Francisco | 2008 | - | Cross -Sectional | 50 | 35.9 | 46.67 |
| 2. | Jafari A et al. | Iran | 2013 | Male=159 Female=97 |
Retrospective- Descriptive | 110 | 90 | 7 |
| 3. | José L. Lopez-Cedrúna et al. | Spain | 2020 | Retrospective-Hospital Based | 183 | 107 | 85.2 | |
| 4. | Oliveira dos Santos et al. | Brazil | 2010 | Male=52 Female=22 |
Prospective – Cross-Sectional | 74 | 114.89 | 85.2 |
| 5. | A.Dwivedi et al. | India | 2012 | Male=161 Female=242 |
Cross-Sectional | 403 | 142.1 | 49.17 |
| 6. | R. Hansen et al. | Denmark | 2011 | - | Cohort Study | 2212 | 0 | 0.33 |
| 7. | T. Lopes et al. | Brazil | 2017 | Male=18 Female=82 |
Retrospective Cross-sectional | 82 | 41 | 165.5 |
| 8. | M. Haimi et al. | Israel | 2004 | - | Retrospective | 315 | 70.21 | 153.6 |
Table 3: Secondary-delay study characteristics.
| Sr No | Author | Country | Year | Gender | Type of Study | Sample Size (Patients) |
Mean (days) |
Sd (days) |
|---|---|---|---|---|---|---|---|---|
| 1. | A.Dwivedi et al. | India | 2012 | Male=161 Female=242 |
Cross-Sectional | 403 | 97.5 | 166.2 |
| 2. | R. Hansen et al. | Denmark | 2011 | - | Cohort Study | 2212 | 55 | 10.17 |
| 3. | T. Lopes et al. | Brazil | 2017 | Male=18 Female=82 |
Retrospective Cross-sectional | 82 | 87.5 | 65 |
| 4. | Isaäc van der Waal et al. | Netherlands | 2011 | - | Cross Sectional | 50 | 10 | 8.25 |
| 5. | M. Haimi et al. | Israel | 2004 | - | Retrospective | 315 | 86.17 | 153.86 |
Table 4: Tertiary-delay study characteristics.
| Study | ① | ② | ③ | ④ | ⑤ | Score |
|---|---|---|---|---|---|---|
| E. Grant et al. | 2 | 1 | 1 | 2 | 2 | 8 |
| Zachary S. Peacock et al. | 2 | 1 | 1 | 2 | 1 | 7 |
| A.Dwivedi et al. | 2 | 1 | 2 | 2 | 2 | 9 |
| R. Hansen et al. | 2 | 1 | 1 | 2 | 2 | 8 |
| T. Lopes et al. | 2 | 1 | 1 | 2 | 2 | 8 |
| Isaäc van der Waal et al. | 2 | 1 | 1 | 2 | 2 | 8 |
| M. Haimi et al. | 2 | 2 | 1 | 2 | 2 | 9 |
| José L. Lopez-Cedrúna et al. | 2 | 2 | 2 | 2 | 2 | 10 |
| Oliveira dos Santos et al. | 2 | 1 | 1 | 2 | 2 | 8 |
| Jafari A et al. | 2 | 2 | 2 | 2 | 1 | 9 |
| Note: ① A clearly stated aim; ② Inclusion of consecutive patients; ③ Prospective collection of data; ④ Endpoints appropriate to the aim of the study; ⑤ Unbiased assessment of the study endpoint. The items are scored 0 (not reported), 1 (reported but inadequate), or 2 (reported and adequate). The global ideal score being 10 for non-comparative studies | ||||||
Table 5: Bias risk assessment.
Based on the Oxford Centre for Evidence-based Medicine Levels of Evidence32, all the 10 studies were graded as shown in Table 4. Risk of bias assessment was done for all studies as per Cochrane Risk of Bias assessment tool 2 (RoB2). Risks of bias in all the domains were low (except the domain of bias due to deviations from intended interventions where it was “some concerns” [11].
Outcomes
Secondary vs tertiary delay: There is a significant difference between the means in primary and secondary delay (Mean Difference (MD) = -17.81, CI = -73.61 – 38.00, I2=98%, p<0.01) for Random Effect Model and (Mean Difference (MD) = -54.92, CI = -55.35 – 54.50, I2=98%, p<0.01) for Fixed Effect Model (Figure 4).
Primary and tertiary delay: There is a significant difference
between the means in primary and secondary delay (Mean Difference (MD) = -0.17, CI = -41.52 – 41.18, I2=96%, p<0.01) for Random Effect Model and (Mean Difference (MD) = -33.96, CI = -34.50 – -33.42, I2=96%, p<0.01) for Fixed Effect Model (Figure 5).
Discussion
Head and neck cancer usually manifests as squamous cell carcinomas of the upper aero digestive tract. The rates of death associated with head and neck cancer continue to be high (a 5-year relative survival rate of 33%–62% according to the site of the tumour) be because the disease is often undiagnosed until it is at an advanced stage. [12]. Whether and to what extent this is due to failures in the initial diagnosis in primary care is unknown. The research on head and neck cancer has generally lacked a primary care perspective. Statistics describing the overall occurrence of cases (e.g., they constitute about 5% of all cancers in the West; some 40 000 new cases occur each year in the United States) fail to give a good idea of how often a general practitioner sees a new case. Similarly, the main symptoms are well known, but how often they occur are not [13]. Misdiagnoses are frequent, but it is unclear whether this is because physical examination of the region is technically demanding, particularly the laborious indirect visualization of the nasopharynx and larynx with small mirrors [14].
Methods of diagnosing oral cancer
There are various methods by which mouth/oral cancers may be detected. Some of the most common methods are Physical Examination and Biopsy. In Physical Examination a doctor or a dentist will examine the patient’s lips and mouth to check any abnormalities. In Biopsy, a tissue from the suspicious area is taken out using a cutting tool or a needle and taken to the laboratory for analysing cancerous or precancerous activity [15].
Extent of cancer
Determining the extent (stage) of cancers helps a doctor in deciding the treatment procedure for the cancer patient. There are four stages in oral cancers indicated in roman letters I through IV. There are certain methods which involve Endoscopy in which doctor may pass a small, flexible camera equipped with a light down the patient’s throat to look for signs that cancer has spread beyond mouth or not. Other procedure involves certain Imaging Test PET (Positron Emission Tomography) scans, MRI, CT scans to determine the level of cancer extent and its spread [16].
Treatment Types
Surgery: A surgeon may cut away the tumor and some of the healthy tissues surrounding the tumor to ensure all of the cancer cells have been removed. Smaller cancers may be removed through minor surgery while larger tumors may require more-extensive procedures. In some of the cases the cancer has spread in the lymph nodes in the neck. In such cases neck dissection is done by a surgeon to remove all the lymph nodes in which cancer is spread [17].
Radiation Therapy: Radiation therapy uses high energy beam X rays and protons to kill the cancer cells. It is most often delivered from a machine outside a patient’s body. Radiation therapy is often used after surgery. But sometimes it might be used alone if the patient has an early-stage mouth cancer. In other situations, radiation therapy may be combined with chemotherapy. This combination increases the efficiency of chemotherapy.
Chemotherapy: It is a treatment that uses chemicals to kill cancer cells. Chemotherapy drugs can be given alone, in combination with other chemotherapy drugs or in combination with other cancer treatments. Chemotherapy may increase the effectiveness of radiation therapy, so the two are often combined. It also has certain side effects depending on the chemotherapy drug received by the patient. The common side effects are vomiting, fatigue, nausea etc. [18].
Oral cancer remains a lethal disease for over 50% of the patients diagnosed annually largely reflected by the fact most cases are in advanced stages at the time of detection [19]. This is despite easy accessibility for regular mouth examination. Awareness of risk factors and symptom recognition by patients is a crucial factor in determining survival rates, as early detection greatly improves the chances of survival, morbidity and patients’ quality of life.
Reasons for delay
There are many of reasons why people do not visit physicians soon after noticing symptoms. One of the main reasons is financial barrier that exists for many patients who are at risk of developing oral cancer. Increased access to health care, including dental care, for uninsured patients likely would allow for more frequent detection of early-stage cancers. Government agencies, universities and dental clinics have made attempts to diagnose cancer early, via population screening and the use of various visual and chemical detection methods. Attempts to diagnose oral cancer early are not practically easy and does not meet any epidemiologic guidelines for a successful screening program; attempts to implement such programs generally have not been effective [20].
Delays can be prevented by
In general, for those considering a regional or national screening program, the following are needed:
• An identifiable and diagnosable disease that is an important health problem.
• Availability of an accepted treatment for patients with recognized disease.
History of the disease should be adequately known. Natural history of disease refers to the progression of a disease process in an individual over time, in the absence of treatment. A simple, cost-effective and reliable test for the disease that has acceptable rates. Rapid tests, also known as rapid diagnostic tests or RDTs, are easy-to-use tests that provide quick results, usually in 20 minutes or less [21]. Screening of disease that improves the outcome. The factor that influences the patient delay is education of the public. Health care providers must place greater emphasis on educating patients about the importance of visiting a clinician as soon as oral symptoms develop. They can visit a dentist or a physician. Public education efforts must also continue to encourage patients to avoid high-risk behaviours as tobacco or alcohol use. Cancer is to institute a self-examination campaign similar to the monthly breast self-examination campaign. Patients without symptoms might visit a general dentist every six months and a physician every year [22].
Conclusion
Any self-examination conducted between these intervals might result in early detection of the cancer and increase visits to the health care professionals before symptoms develop. A visual examination of the oral cavity in a mirror on a monthly basis would be fairly easy to perform and could result in the detection of some lesions. Patients would be instructed to lift up their tongues to view the floor of the mouth, move the tongue to the right and left of the mouth to evaluate the lateral surfaces and pull both cheeks laterally to examine the vestibules, gingivae and buccal mucosa [23]. Self-examination has the potential to enable patients to detect asymptomatic cancers at early stages. Not only does self-examination increase the frequency with which the oral cavity is screened, but it is done at no burden to the health care system beyond patient education.
India is home to 17% of the global population. On the contrary, cancer mortality due to head and neck cancer is widespread in the South East Asia region [24]. The rising demand for cancer care, along with the rising cost of treatment due to the introduction of several new treatment technologies has imposed a challenge to the health system in India. Most of the cancer treatment in India is provided at tertiary care hospitals, as its treatment requires intensive treatment therapies which are only available at the level of these facilities [25].
Conflict of interest
Nil
Source of finding
None
References
- Mousavi SM, Donlou M, Haj Sadeghi N (2006) Guideline of records and report of cancer 102-134.
- Pisani P, Parkin DM, Bray F, Ferlay J (1999) Estimates of the worldwide mortality from 25 cancers in 1990. Int J Cancer 83:18-29.
- Clegg LX, Feuer EJ, Midthune DN, Fay MP, Hankey BF (2002) Impact of Reporting Delay and Reporting Error on Cancer Incidence Rates and Trends 1-9.
- Ries LAG, Eisner MP, Kosary CL, Hankey, BF, Clegg LX, et al. (1999) SEER: cancer statistics review 45.
- 1973-1996: Cancer Statistics Review. NCI 21- 65.
- Mousavi SM, Gouya MM, Ramazani R, Davanloo M, Hajsadeghi N, et al. (2008) National Cancer Registry Report 2005-2006 67-71.
- Dent Br, Facial Ortho (2015) “Delayed Diagnosis and Treatment of Oral Cancer.” Dental Abstracts 60:330-331.
- Scott SE, McGurk M, Grunfeld EA (2007) The process of symptom appraisal: cognitiveand emotional responses to detecting potentially malignant oral symptoms. J Psychosom Res 62:621–630.
- Gatta G, Botta L, Sánchez MJ, Anderson LA, Pierannunzio D, et al. (2015) Prognoses and improvement for head and neck cancers diagnosed in Europe in early 2000s: the EUROCARE-5 population-based study. Eur J Cancer 51:2130–2143.
- Seoane JL, Takkouche B., Varela-Centelles P, Tomás-Carmona I, Seoane-Romer J, et al. (2012) Impact of delay in diagnosis on survival to head and neck carcinomas: a systematic review with meta-analysis. Clin Otolaryngol 37:99–106.
- Allgar VL, Oliver SE, Chen H, Oviasu O, Johnson MJ, et al. (2019) Time Intervals from First Symptom to Diagnosis for Head and Neck Cancers: An Analysis of Linked Patient Reports and Medical Records from the UK. Cancer Epidemiol 59:37–45.
- Carlsen AH, Eriksen JG, Godballe C, Johansen J, Sørensen JA, Bjørndal K (2019) Impact of Age, Comorbidity, and WHO Performance Status on Delay of Treatment in Patients Undergoing Fast-Track Work-up for Head and Neck Cancer. J Geriatr Oncol 10:259–264.
- Moher D, Liberati A, Tetzlaff J, Altman DG, Group P (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. J clinical epidemiol 62:1006–1012.
- Franceschi S, Levi F, Vecchia C (1992) Decline in 5-year survival rates for cancer of head N and neck. Lanc 340:347.
- Muir C, Weiland L (1995) Upper aero digestive tract cancers. Canc 75:147-153.
- Brenner H (2002) Long-term survival rates of cancer patients achieved by the end of the 20th century: a period analysis. Lanc 360:1131-1135.
- Grant E, Silver K, Bauld L, Day R, Warnakulasuriya S (2010) The Experiences of Young Oral Cancer Patients in Scotland: Symptom Recognition and Delays in Seeking Professional Help. Br Dent J 208:465–471.
- Kujan O, Glenny AM, Duxbury AJ, Thakker N, Sloan P (2003) Screening programmes for the early detection and prevention of oral cancer. Cochrane Database Syst Rev CD004150.
- Kujan O, Glenny AM, Duxbury J, Thakker N, Sloan P (2005) Evaluation of screening strategies for improving oral cancer mortality: a Cochrane systematic review. J Dent Educ 69:255-265.
- Wilson J.M.G, Jungner G (1968) Principles and Practice of Mass Screening for Disease. Geneva: World Health Organization.
- Peacock ZS, Pogrel MA, Schmidt BL (2008) Exploring the Reasons for Delay in Treatment of Oral Cancer. J Am Dent Assoc 139:1346–1352.
- Ferlay J, Soerjomataram I, Ervik M, Forman D, Bray F, et al. (2015) GLOBOCAN 2012: Estimated Cancer Incidence and Mortality Worldwide in 2012 v1.0. IARC.
- Smith BD, Pan IW, Shih YCT, Smith GL, Harris JR, et al. (2011) Adoption of IntensityModulated Radiation Therapy for Breast Cancer in the United States. J Natl Cancer Inst 103:798-809.
- Sheets NC, Wheeler SB, Kohler RE, Fried D, Brown PM, et al. (2013) Costs of care in a matched pair comparison of intensity-modulated radiation therapy (IMRT) versus conventional radiation therapy (CRT) for the treatment of head and neck cancer. Am J Clin Oncol 37.
- Chauhan AS, Prinja S, Ghoshal S, Verma R, Oinam AS (2018) Cost of Treatment for Head and Neck Cancer in India. PLoS ONE 13: e0191132.
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Citation: Sajjad SA (2022) Comparing the Type of Delays in Oral Cancer: A Systematic Review and Meta-Analysis. J Cancer Diagn 6: 137. DOI: 10.4172/2476-2253.1000137
Copyright: © 2022 Sajjad SA. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 2304
- [From(publication date): 0-2022 - Apr 26, 2025]
- Breakdown by view type
- HTML page views: 1813
- PDF downloads: 491