Research Article Open Access
Comparing the Prevalence and Drug Treatment Rates of Diabetes, Hypertension and Dyslipidemia between Japan and Brazil, using 2013 National Health Surveys
Angelo Jose Goncalves Bos1*, Luisa Braga Jorge1, Joel Hirtz do Nascimento Navarro1, Leticia Farias Gerlack2, Josemara de Paula Rocha1, Gabriela Guimaraes Oliveira1, Jessika Cefrin1, Vanessa Cuentro1, Claudine Lamanna Schirmer1 and Maria Marina Serrao Cabral11Institute of Geriatrics and Gerontology, Pontifical Catholic University of Rio Grande do Sul, Brazil
2National University of Brazilia, Brazil
- Corresponding Author:
- Angelo Jose Goncalves Bos
Institute of Geriatrics and Gerontology, Pontifical
Catholic University of Rio Grande do Sul, Brazil
Tel: + 555133536229
E-mail: angelo.bos@pucrs.br
Received Date: September 29, 2015 Accepted Date: December 04, 2015 Published Date: December 11, 2015
Citation: Bos AJG, Jorge LB, Navarro JHN, Gerlack LF, Rocha JP, et al. (2015) Comparing the Prevalence and Drug Treatment Rates of Diabetes, Hypertension and Dyslipidemia between Japan and Brazil, using 2013 National Health Surveys. J Clin Diabetes Pract 1:103. doi:10.4172/jcdp.1000103
Copyright: © 2015 Bos AJG et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at
Abstract
Diabetes and other Non-Communicable Diseases (NCD) are public health concerns in both developed and developing countries. Brazil and Japan have made publically available National Health Surveys focus also in the prevalence of NCD, among them Diabetes, Hypertension and Dyslipidemia. This study offers a unique opportunity to understand the prevalence of NCD in economically different countries exploring also the drug use for those conditions. The results showed that the Japanese population has higher prevalence of all conditions, but Brazil presented a quite substantial number of participants who never checked for those conditions, mainly for dyslipidemia. Japanese survey did not check for that information. Treatment rate was higher in the Brazilian population but the specific mortality rate for both Diabetes and Hypertension was also higher in this country. We concluded that NCD are frequent health problems in both countries. Brazil has improved the access to medication to NCD conditions, although it still has a much higher mortality rate. The treatment of NCD is not only performed through drug treatment but also by public health education which seems to be more effective performed in the Japanese population.
Keywords
Diabetes; Hypertension; Dyslipidemia
Introduction
Non-Communicable Diseases (NCD) have reached epidemic proportions in both developed and developing countries causing higher mortality and disability rates [1]. They do not have a single cause, but are a result of an interaction of risk factors that can be classified as genetic (biologic predisposition) and environmental. The most frequent environmental and modifiable risk factors for NCD are Hypertension (HTN), Diabetes Mellitus (DM) and Dyslipidemia. These three risk factors can easily be identified and controlled at primary health care setting [1]. Thus, Public Health Providers have established as a priority to detect and treat those factors.
Since 2003, Japanese Ministry of Health Labor and Welfare (JMHLW) has conducted a population based nationwide health and nutrition survey [2]. With a similar methodology, in 2013 Brazilian Institute of Statistics and Geography (IBGE), in collaboration with the Ministry of Health, has also conducted a population based nationwide health survey [3]. Both Japanese and Brazilian National Health Surveys explored the prevalence of HTN, DM and Dyslipidemia, including the question about the use or not of medication to control those risk factors. Thus, the present study aims to compare the prevalence and treatment rates for HTN, DM and Dyslipidemia in both countries representing a developed (Japan) and a developing (Brazil) country.
Methods
The Japanese National Health and Nutrition Survey is an annually investigation, with its methodological approach published quite recently by Ikeda et al. [4]. It is a cross-sectional survey conducted every November by a household interview and blood sample collection, conducted by the JMHLW. Local Health Centers conducted the surveys coordinated by the local governments. In this study we used the information of the prevalence to Diabetes, Hypertension and Dyslipidemia and the medication use for those conditions from the publication report published in March 2015 by the JMHLW [2]. In Japan, the participants were selected from a list of families identified in a previous survey (Comprehensive Survey of Living Conditions) conducted between June and July. The number of investigated districts was 300 with 5,422 families. Families moved outside of the district after first survey was excluded, they added up to 127 families. During the interview, the participants answered the question “Have you ever told by a Medical Doctor that you have …” for Hypertension, Diabetes and Dyslipidemia. Treatment information followed the same approach. We obtained the data on mortality (primary cause of death) for Japan by visiting the website of the Communications Statistics Bureau of the Ministry of Internal Affairs [5].
Brazilian National Health Survey was implemented in 2013. It is also a household interview and also planned a blood sample collection. The blood sample collection, due to financial limitations, was not conducted in the whole sample. The sample comprised three stages: primary sample units which contained the households (second stage) and finally for each household an 18 years and older resident was selected (Selected Adult Resident), which is the third sample stage. Brazilian National Health Survey involved 62,986 households and 60,202 participants aged 18 or older (Selected Adult Resident). The organization and coordination of the work was conducted by the IBGE. The interviews were performed using PDA (Personal Digital Assistance). The selected adult resident answered a complete interview on his or her health status and lifestyle together with height, weight, waist circumference and blood pressure measurements. For the prevalence of HTN, DM and Dyslipidemia the participants answered the question “Have you ever told by a Medical Doctor or other health professional that you have ….”, followed by a question regards to current drug treatment. Raw data from the Brazilian National Health Survey became public available in June 2015 and was downloaded on an ASCII (American Standard Code for Information Interchange) file from the IBGE website [3]. We converted the ASCII data to Microsoft Excel format for analysis. We obtained data on mortality from the official website of the Brazilian Ministry of Health, which provides information on the primary cause of death by age at specific year [6].
Since the present investigation is secondary analysis of two databases, the authors did not have any personal information from the participants. The information used from both Brazilian and Japanese surveys is freely available, not requiring any authorization from Internal Review Board. The authors had access only to the information about Brazilian Survey which was approved by the National Commission of Ethics in Research of the National Council of Brazilian Health [7]. As mentioned before, all Japanese information came from published work [2,5].
Data received descriptive statistical analysis using the statistical package Epi Info™ 7.0. Available for free download on the Internet, provided by the Center for Disease Control and Prevention of the US Government.
Results
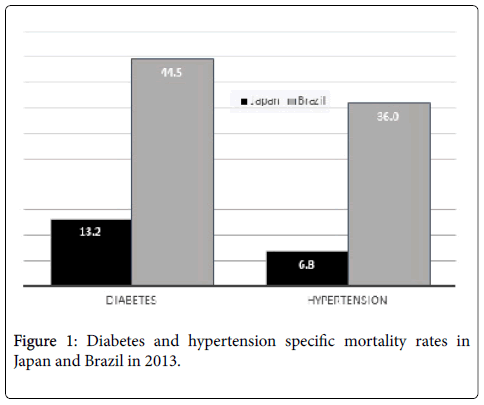
Table 1 shows the results of both surveys on the prevalence of and medication use for hypertension. Younger age groups were more frequent in Brazil and older age groups in Japan. Hypertension was similar in both countries until the age of 49. Age groups 50 year of older presented a higher prevalence in Japan, ranging from 42% to 74% (in Brazil ranged from 34% to 53%). Diabetes, on Table 2, was similar in both countries. The higher percent difference observed at the 60 to 69 year-old (Brazil 17%, Japan 19%). Table 3 shows the data for dyslipidemia, which was higher in younger Brazilian groups and in the older Japanese groups. The lower prevalence of these health conditions could be influenced by the fact that, in Brazil, 11% never checked for Diabetes, 14% never checked for Dyslipidemia and 2.5 never checked for hypertension. In all three risk factors the frequency of treatment (by means of drug use) was higher in the Brazilian group on all ages. Figure 1 shows the specific mortality rates of Diabetes and Hypertension in Japan and Brazil in 2013.
| Age group | No | Yes | Treatment | |
|---|---|---|---|---|
| 20 – 29(%) | Brazil | 11092(96.4%) | 411(3.6%) | 134(32.6%) |
| Japan | 747(96.6%) | 33(3.4%) | 3(10.8%) | |
| 30 – 39 (%) | Brazil | 12599(93.0%) | 1284(7.0%) | 743(57.9%) |
| Japan | 1555(89.9%) | 192(10.1%) | 20(13.6%) | |
| 40 – 49 (%) | Brazil | 8956(80.9%) | 2227(19.1%) | 1652(74.2%) |
| Japan | 1497(80.2%) | 432(19.8%) | 102(20.2%) | |
| 50 – 59 (%) | Brazil | 5871(66.3%) | 3017(33.7%) | 2502(82.9%) |
| Japan | 1302(57.8%) | 1027(42.2%) | 384(36.1%) | |
| 60 – 69 (%) | Brazil | 3248(52.8%) | 2917(47.2%) | 2612(89.5%) |
| Japan | 1583(41.7%) | 2295(58.3%) | 1356(59.8%) | |
| 70 + (%) | Brazil | 2282(46.7%) | 2607(53.3%) | 2367(90.8%) |
| Japan | 1121(25.8%) | 3277(74.2%) | 2411(72.4%) | |
| TOTAL(%) | Brazil | 44048(79.1%) | 12463(20.9%) | 10010(80.3%) |
| Japan | 7805(53.9%) | 7256(46.1%) | 4276(58.5%) |
Table 1: Prevalence of hypertension and treatment rate in Brazil and Japan by age group (2013).
| Age group | No | Yes | Treatment | |
|---|---|---|---|---|
| 20 – 29(%) | Brazil | 9917(99.3%) | 66(0.7%) | 34(51.5%) |
| Japan | 2666(99.3%) | 18(0.7%) | 4(22.2%) | |
| 30 – 39 (%) | Brazil | 12244(98.8%) | 241(1.9%) | 149(61.8%) |
| Japan | 4189(98.0%) | 93(2.0%) | 27(29%) | |
| 40 – 49 (%) | Brazil | 9719(95.3%) | 507(4.7%) | 368(72.6%) |
| Japan | 4248(95.7%) | 219(4.3%) | 88(40.2%) | |
| 50 – 59 (%) | Brazil | 7394(88.9%) | 918(11.1%) | 727(79.2%) |
| Japan | 4106(87.2%) | 562(12.8%) | 303(53.9%) | |
| 60 – 69 (%) | Brazil | 4896(83.1%) | 998(16.9%) | 847(84.9%) |
| Japan | 5105(80.8%) | 1241(19.2%) | 783(63.1%) | |
| 70 + (%) | Brazil | 3793(80.9%) | 898(19.1%) | 767(85.4%) |
| Japan | 6085(79.3%) | 1565(20.7%) | 1103(70.5%) | |
| TOTAL(%) | Brazil | 47963(93.3%) | 3628(6.3%) | 2892(79.7%) |
| Japan | 26399(88.1%) | 3698(11.9%) | 2308(62.4%) |
Table 2: Prevalence of diabetes and treatment rate in Brazil and Japan by age group (2013).
| Age group | No | Yes | Treatment | |
|---|---|---|---|---|
| 20 – 29(%) | Brazil | 9053(96.1%) | 368(3.9%) | 152(41.3%) |
| Japan | 696(95.8%) | 39(4.2%) | 4(6.9%) | |
| 30 – 39 (%) | Brazil | 11065(91.8%) | 986(8.2%) | 541(54.9%) |
| Japan | 1552(93.7%) | 104(6.3%) | 9(7.2%) | |
| 40 – 49 (%) | Brazil | 8535(85.4%) | 1460(14.6%) | 974(66.7%) |
| Japan | 1680(92.4%) | 157(7.6%) | 56(32%) | |
| 50 – 59 (%) | Brazil | 6322(77.5%) | 1834(22.5%) | 1405(76.6%) |
| Japan | 1841(83.6%) | 357(16.4%) | 230(59.3%) | |
| 60 – 69 (%) | Brazil | 4260(73.2%) | 1557(26.8%) | 1306(83.9%) |
| Japan | 2626(72.3%) | 1000(27.7%) | 753(75.8%) | |
| 70 + (%) | Brazil | 3576(77.4%) | 1047(22.6%) | 906(86.5%) |
| Japan | 2681(65.7%) | 1364(34.3%) | 1026(77.9%) | |
| TOTAL(%) | Brazil | 42811(85.5%) | 7252(14.5%) | 5284(72.9%) |
| Japan | 11076(78.9%) | 3021(21.1%) | 2078(69.3%) |
Table 3: Prevalence of dyslipidemia and treatment rate in Brazil and Japan by age group12 (2013).
Discussion
Considering the importance of health promotion, early diagnosis and control of HTN, DM and Dyslipidemia are important for the reduction and prevention of possible complications from these NCD. In this sense, the objective of this study was to compare two population-based studies conducted in Brazil and Japan in relation to the prevalence and treatment of those conditions. The results are considered the estimation rates for both countries regards to the diagnosis and the treatment.
In Japan, the prevalence of DM had increased significant, resulting mainly from the adult population aging. Between 1988 and 2011 the prevalence of DM among both sexes and all age groups generally remained unchanged, but men over 70 years or more had significant increases in prevalence over time. In 2010 the prevalence of DM in women was 6.1% for men, 9.9% and 7.9% in the general population and it is believed that the values increase in 2030, reaching respectively 6.7% 13.1% and 9.8% [8]. Our study observed a higher prevalence of HTN, DM and Dyslipidemia in Japan. Brazilian survey also assessed the number of people who had never checked for blood pressure, hyperglycemia and blood lipids. The same data was not available in the Japanese survey so it is not possible to confirm if the lower prevalence of those conditions was related to a lower diagnose.
Discussion
Considering the importance of health promotion, early diagnosis and control of HTN, DM and Dyslipidemia are important for the reduction and prevention of possible complications from these NCD. In this sense, the objective of this study was to compare two population-based studies conducted in Brazil and Japan in relation to the prevalence and treatment of those conditions. The results are considered the estimation rates for both countries regards to the diagnosis and the treatment.
In Japan, the prevalence of DM had increased significant, resulting mainly from the adult population aging. Between 1988 and 2011 the prevalence of DM among both sexes and all age groups generally remained unchanged, but men over 70 years or more had significant increases in prevalence over time. In 2010 the prevalence of DM in women was 6.1% for men, 9.9% and 7.9% in the general population and it is believed that the values increase in 2030, reaching respectively 6.7% 13.1% and 9.8% [8]. Our study observed a higher prevalence of HTN, DM and Dyslipidemia in Japan. Brazilian survey also assessed the number of people who had never checked for blood pressure, hyperglycemia and blood lipids. The same data was not available in the Japanese survey so it is not possible to confirm if the lower prevalence of those conditions was related to a lower diagnose.
Adherence to treatment of hypertension and DM includes both continuous medication (when necessary) and the lifestyle modification, through the practice of physical exercises and modification of eating habits. The low rate of diagnosis and treatment adherence is responsible for the further development of health complications, social and decreased quality of life [9].
A Neville and cols observed that, comparing to Americans, Japanese patients with DM had better adherence to changes in lifestyle, glycemic control, less adhered to the medical regimen. Japanese with DM also accepted better diet and exercise recommendations [10]. In the guideline of evidence-based practices in the treatment of diabetes in Japan in 2013, the topic educating patients about diet therapy, exercise and improved lifestyle is encouraged at all stages of treatment [11].
Non-pharmacological actions are essential to controlling hypertension, dyslipidemia and other factors that may cause cardiovascular disease: healthy habits, dietary changes, elimination of alcohol and tobacco, physical exercise and loss of excess weight [12]. Patients with Hypertension have knowledge of the actions of treatment, but have trouble following non-pharmacological actions, because the changes that treatment requires lifestyle and also by entering into a "comfort zone" when use of drug treatment, thus judge unnecessary change in lifestyle that results in the non-drug treatment [12].
In Brazil, the study showed that adherence has become one of the biggest problems in medical practice due to their complexity. About 40% to 60% of patients do not make use of prescribed medication. This percentage increases as the lack of adherence relates to items such as lifestyle, emphasizing diet, sedentary lifestyle, smoking, alcohol consumption, among other factors [13].
In the last two decades, several countries have developed actions and programs for the prevention, detection and control of NCDs, with the challenge of reducing by 25% the mortality due to these diseases by 2025[14]. In Brazil, the Plan Strategic Actions for Confronting NCD 2011-2022 defines strategies and action priorities, and investments for the detection and control of NCD and their risk factors in the country [15]. One of the actions of the Plan refers to the expansion of pharmaceutical care and the free distribution of more than 15 drugs for hypertension and diabetes (antihypertensive, insulin, hypoglycemic agents, statins, etc.). In March 2011, the People's Pharmacy / Health program has not Price started offering drugs for hypertension and diabetes and currently more than 17,500 private pharmacies are already registered for the free distribution of these medicines [15].
The high frequency of participants using drugs to treat chronic diseases investigated in this survey may indicate an increased access to treatment for these diseases in Brazil. Tavares et al [16] is considered to have increased access to medicines for the treatment of chronic diseases is of great importance and can represent a major advance in Brazilian public policy, since it enables control of diseases, reduce morbidity, mortality and quality of life [15]. However, it is noteworthy that the drug should be only one component of comprehensive care in NCD, which include healthy eating, physical activity, reducing alcohol intake and no tobacco consumption [15].
Our study performed a secondary analysis of two National Health Surveys (Brazilian and Japanese). The analyzed presence of chronic diseases was based from self-reported information. The questions were “Do you have medical diagnosis or not”, and “Are you taking or not medicine for this disease”. This approach can cause bias since the answers depend on the respondent's memory. It also might be possible that a participant would think that he or she does not have such disease anymore because is not currently taking any medication or has not measured his or her blood pressure, or having a glycemic control or even not measuring the blood cholesterol. New analyzes should also address quality of life issues related to the presence of the diseases and the possible differences in treatment approach in both countries. Unfortunately, this data is not uniformly available in banks of data analyzed.
We concluded that NCD are frequent health problems in both countries. Brazil has improved the access to medication to NCD conditions, although it still has a much higher mortality rate. Drug treatment is not the only NCD control approach. Public Health Education seems to be more effective performed in the Japanese population.
References
- Schmidt MI, Duncan BB, Silva GA, Menezes AM, Monteiro CA, et al. (2011) Chronic non-communicable diseases in Brazil: burden and current challenges. Lancet 377: 1949-1961.
- Japan. Ministry of Health, Labor and Welfare. National Health and Nutrition Survey
- IBGE. National Health Survey – microdataaccessed in October 29, 2015.
- Ikeda N, Takimoto H, Imai S, Miyachi M, and Nishi N (2015) Data Resource Profile: The Japan National Health and Nutrition Survey (NHNS). Int JEpidemiol.
- Japan, Ministry of Internal Affairs and Communications Statistics Bureau, Health Statistics and Mortality
- Ministry of Health, Unique Health System, DATASUS, Vital Statitics, General Mortality [internet]. Brasilia, 2015.
- Brazil. Institute of Geography and Statistics - IBGE. National Health Survey - 2013: health status, life style and chronic diseases perceptions - Brazil, Regions and Federal Unities [Internet]. Rio de Janeiro: IBGE; 2014. 181 p.
- Charvat H, (2015) Impact of population aging on trends in diabetes prevalence: A meta-regression analysis of 160,000 Japanese adults. Journal of Diabetes Investigation 6: 533–542.
- Mendes LVP, Luiza VL, Campos MR (2014) Rational use of medicines by individuals with diabetes mellitus and arterial hypertension in the municipality of Rio de Janeiro, Brazil. Cienc. saudecoletiva 19: 929-941.
- Neville SE,(2009) Diabetes in Japan: a review of disease burden and approaches to treatment. Diabetes/metabolism research and reviews 25: 705–716.
- Tajima N, (2015) Evidence-based practice guideline for the treatment for diabetes in Japan 2013. Diabetology International 6: 151–187.
- Massinga LT, Portella MRP (2015) Fatoresdeterminantes da adesão de hipertensos a condutadietoterápica. Rev de Atenção à Saúde 13: 37-45.
- Barbosa RG, Lima NK (2006) Índices de adesãoaotratamento anti-hipertensivo no Brasil e mundo. Rev Bras Hipertens 13: 35-38.
- Alleyne G, Binagwaho A, Haines A, Jahan S, Nugent R, et al. (2013) Embedding non-communicable diseases in the post-2015 development agenda. Lancet 381:566-74.6.
- Malta DC, Silva Junior JB (2013) O plano de açõesestratégicaspara o enfrentamento das doençascrônicasnãotransmissíveis no Brasil e a definição das metasglobaispara o enfrentamentodessasdoençasaté 2025,umarevisão. EpidemiolServSaude 22:151-64.
- Tavares NUL, Costa KS, Mengue SS, Vieira MLFP, Malta DC, et al. (2015) Uso de medicamentosparatratamento de doençascrônicasnãotransmissíveis no Brasil: resultados da PesquisaNacional de Saúde, 2013. EpidemiolServSaúde 24: 315-323.
Relevant Topics
Recommended Journals
Article Tools
Article Usage
- Total views: 13019
- [From(publication date):
April-2016 - Jul 15, 2025] - Breakdown by view type
- HTML page views : 11986
- PDF downloads : 1033