Research Article Open Access
Comparative Study between Continuous Thoracic Epidural vs. Thoracic Spinal Anaesthesia in Breast Surgery
Abdalla Mohamed Ahmed*, Hosny Ali, Osama Helal and Tarek Sobhi
Department of Anesthesiology, Al-Azhar University, Egypt
- *Corresponding Author:
- Abdalla Mohamed Ahmed
Department of Anesthesiology, Al-Azhar University
Cairo, Egypt
Tel: 0201001574386
E-mail: mohammedelsokkary1@yahoo.com
Received date: May 04, 2017; Accepted date: June 14, 2017; Published date: June 20, 2017
Citation: Ahmed AM, Ali H, Helal O, Sobhi T (2017) Comparative Study between Continuous Thoracic Epidural vs. Thoracic Spinal Anaesthesia in Breast Surgery. J Pain Relief 6:292. doi:10.4172/2167-0846.1000292
Copyright: © 2017 Ahmed AM, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Pain & Relief
Abstract
Objective: The aim of this work is to compare between thoracic epidural anesthesia (TEA) and segmental thoracic spinal anesthesia (TSA) conducted for breast surgeries as regard to hemodynamic changes (blood pressure, heart rate, oxygen saturation, ETCO2), postoperative pain control, postoperative analgesic requirements, surgeon satisfaction, postoperative ambulation time and perioperative complication.
Setting: Al-Hussein and Sayed Galal hospitals.
Patients and Methods: This work was done upon 40 female patient undergoing breast surgeries. Patients were divided randomly into 2 equal groups according to the type of anesthetic technique had been chosen. Group I were anaesthetized by thoracic epidural anesthesia and group II by segmental thoracic spinal anesthesia.
Results: Recovery and ambulation time was more or less equal in the both groups. This is important since the patient can readily return to her family and social environment and can decrease the cost of the procedure, although this was not specifically assessed in this study. Post-operative pain was compared at the time 0, 1, 2, 4 and 8 hour by using VAS.
Conclusion: We found that epidural blockade a preferred choice of anesthetic management for breast surgery.
Keywords
Continuous thoracic epidural anaesthesia; Thoracic spinal anaesthesia; Breast surgery
Introduction
In the last years incidence of breast cancer, as well as the need of surgical treatment has increased, different surgical intervention which ranging from simple mastectomy to total mastectomy associated with axillary exploration to remove lymph nodes for staging or immune- chemical testing is still necessary, also cosmetic and reconstructive breast augmentation is a frequently performed surgical procedure [1].
Epidural anesthesia is a central neuro-axial block technique with many applications. Improvements in equipment, drugs and technique have made it a popular and versatile anesthetic technique with applications in surgery, obstetrics and pain control. Nesmith et al. performed thoracic epidural anesthesia for breast cancer surgery. Adequate postoperative analgesia attenuates stress response and prevents unnecessary patient discomfort. It may also decrease morbidity, postoperative hospital length of stay and thus cost [2].
Different regional techniques have been attempted during breast surgery, including thoracic epidural and thoracic paravertebral block. However, the delayed onset of block, patchy sensory block, and large volume of local anesthetic used with potential risk for local anesthetic toxicity and difficulty in insertion are still issues of concern when applying these techniques during breast surgery [3].
Recently segmental thoracic spinal anesthesia has been used for laparoscopic cholecystectomy was practiced by (Zundert et al.) who inject (7.5 mg bupvacin and 25 μg fentanyle) at lower thoracic region (T9-T10) [4].
A recent study by (Mahmoud et al.) depended on the fact that the posterior subarachnoid space is wider at the mid-thoracic region (T5- T6) compared with the upper and lower thoracic regions (Imbelloni et al.) and do segmental thoracic spinal anesthesia at mid thoracic region [5].
Advantages as was practiced without any great difficulty, there is no blockade of the lower extremities, i.e. little caudal spread. This means that a significantly larger portion of the body no venal dilation, and may offer a compensatory buffer to adverse changes in blood pressure intra-operatively [6]. The dosing of the anesthetic is exceedingly low, the degree of muscle relaxation achievable without central or peripheral respiratory or circulatory depression and the patients have motor control over their legs a high level of satisfaction [7].
We were concerned about three issues: the risk for spinal cord injury, cephalic spread of local anesthetic causing high or total block and hemodynamic or respiratory compromise due to block of cardio- accelerator fibers or intercostal nerves.
Patients and Methods
After ethical committee approval and informed consent from patients, this prospective, single blind randomized controlled study was carried out in Al-Azhar university hospitals on 40 female patients (ASA physical status I-II), scheduled for elective breast surgery, they were randomly allocated into two equal groups 20 patients each:
Group I (TEA): (thoracic epidural anesthesia).
Group II (TSA): segmental thoracic spinal anesthesia (T5-T6).
Patients excluded from this study
• Patient refusal
• Patients with systemic or local back infection.
• Patients with thoracic or cervical arthritis with neurological deficit.
• Patients with thoracic spine deformity.
• Patients with allergy to local anesthetic drugs.
• Patients with bleeding disorders.
Investigations required before surgery
• Complete blood picture.
• Bleeding time, prothrombin time, activated partial thromboplastin time and INR.
• Liver and kidney functions tests and random blood sugar.
• ECG.
Patient preparation
Patients were visited pre-operatively in order to take history, perform clinical examination, and review investigations including coagulation profile and to start a well-established doctor patient relationship. All patients were instructed how to be familiar with the visual analogue scale for pain and the modes of analgesia including their advantages, disadvantages and risks, Sedation with midazolam (2-3 mg IV) was given 15 min preoperative.
Equipments
• Intravenous cannulas size 18 gauge (Venocath, Hamburg, Germany).
• Syringes (20 cc, 10 cc, 5 cc, 3 cc and 1 cc) and adhesive tape.
• Intravenous infusion set.
• Epidural set (Prefix custom epidural anesthesia tray): with an 18-G Tuohy epidural needle and a 20 gauge epidural catheter.
• Spinal cut needles size 27 gauges (GMS)
• Sterilized towels and gauze.
Drugs:
• Fentanyl 100 μg/2 ml, Ampule, diluted with saline to a concentration of 10 μg/ml.
• Midazolam (dormicum) 5 mg/ml, Ampule, diluted with saline to a concentration of 1 mg/ml.
• Meperidine (Pethidine 50 mg/ml), Ampule (Misr CO - Egypt), diluted with saline to a concentration of 10 mg/ml.
• Isobaric bupivacaine 0.5%, Vial (Astra Zenica, Sweden).
• Lidocaine 2%, Vial (El-Nasr pharm., A.R.E.).
• Isoflurane (Forane), Bottle (Abbott, Egypt).
• Paracetamol 500 mg vial (perflgan).
• Ranitidine (Zantac) 25 mg/ml, Ampule.
• Ondansetron (Zofran) 4 mg, Ampule.
• Metoclopromide (Primperan) 10 mg, Ampule.
• Intralipid 20%, Bottle (Fresenius Kabi AB)
Emergency drugs:
• Atropine 1 mg/ml, Ampule, diluted with saline to a concentration of 0.2 mg/ml.
• Ephedrine 30 mg/ml, Ampule, diluted with saline to a concentration of 3 mg/ml.
• Adrenaline 1 mg/ml, Ampule.
• Crush Trolley emergency drugs, e.g. Antiarrythmic drugs & drugs for resuscitation.
• Intralipid 20%, Bottle (Fresenius Kabi AB).
• Anesthesia machine (Julian Dragger, MEC 2000 Fabius GS) with Mindry full patient monitor.
• Defibrillator (D.C.) shock machine.
Patient monitoring
• For all patients monitoring was started before application of anaesthetic technique.
• Pulse oximetry.
• Non-invasive blood pressure monitoring every 5 minutes.
• Heart rate by 5-leads ECG with ST segment analysis.
• Capnography for end tidal CO2 measurement (ETCO2).
According to the anaesthetic technique, patients were randomly allocated into one of 2 groups
Group I: 20 patients received thoracic epidural anesthesia after meticulous explanation for all patients.
Technique for epidural insertion: Patient placed in sitting position, the back was sterilized with a povidone iodine solution. Either the midline or the paramedian approach was used. Under complete aseptic conditions, the skin and underlying tissues were infiltrated with 1.5 ml of 2% lidocaine solution at the site T6-T7. After 1-2 minutes, the Tuohy needle was advanced and epidural space was identified by loss of resistance to saline injection. Epidural catheter was then threaded through the needle and advanced for 3-5 centimeters upwards into the epidural space. The needle was withdrawn over the firmly gripped catheter that was then secured to the back with adhesive dressings and test dose was injected first 2 ml lidocaine 2%, then the local anaesthetic bupivacaine 0.5% 15 ml and 0.5 μg/kg fentanyl injected into epidural catheter, then patient returned to supine position maintained with 100% O2 by mask at rate 4-6 L/min.
Postoperative analgesia is maintained by paracetamol infusion, repeated boluses of on patients demand given to keep VAS<3.
Group II: Segmental thoracic spinal anaesthesia. 20 patients received segmental thoracic spinal anaesthesia after meticulous explanation for all patients. After cleansing the skin with antiseptic preparation, the skin of the puncture site was infiltrated with 1% lidocaine. Patients were placed on the lateral decubitus or sitting position and the puncture was performed via paramedian approach, at the T5-T6 or T6-T7 interspace in all patients, with a 27G cut needle (GMS). After piercing the ligamentum flavum, the needle's stylet was removed and the hub observed for free flow of CSF; once flow of clear CSF began, 1 ml of isobaric bupivacaine 0.5% in addition to 25 μg fentanyl were injected. The patient was then placed in supine position.
Postoperative analgesia: Postoperative patient's analgesia, for the two groups is maintained by paracetamol infusion given on recovery and repeated every 6 hours and increments of pethidine 50-100 mg I.V or I.M boluses on patients demand given to keep VAS<3.
Parameters of the study
• Hemodynamic changes: Heart rate, systolic, diastolic and mean arterial blood pressure.
• Respiratory changes: O2 saturation and end tidal CO2. Recorded data were collected before beginning of anesthesia (baseline) and 5 minutes interval intra-operatively for the first hour of surgery.
• Recovery time.
• Assessment of pain: Using the visual analogue pain score. The patient is simply asked to correlate the degree of his pain on a scale graded from 0 to 10 where 0=no pain and 10=sever pain at 0, 1, 2, 4, 8 hours.
• Postoperative analgesic requirements of paracetamol and if need additional doses of pethedine to keep VAS <3 for each group was calculated.
• Perioperative complication
• surgeon satisfaction
• Ambulation time
Results
Statistical methodology
Retrieved data were recorded on an investigative report form. The data were analyzed with SPSS® for Windows®, version 15.0 (SPSS, Inc, USA). Description of quantitative (numerical) variables was performed in form of mean, standard deviation (SD) and range. Description of qualitative (categorical) data was performed in the form of numbers and percent. Analysis of numerical variables was performed by using student’s unpaired t-test (for two groups) or ANOVA (for more than two groups). Analysis of categorical data was performed by using Fischer’s exact test and Chi-square test. Significance level was set at 0.05.
The present study included 40 patients divided into 2 groups (20 patients each). Patient’s characteristics were similar in age, sex, weight and height in the two groups (Table 1).
| Variables | Group I | Group II | t | p |
|---|---|---|---|---|
| Age (years) | 36 ± 11 | 33 ± 11 | 0.862 | 0.394 |
| Weight (kg) | 101 ± 56 | 109 ± 53 | 0.464 | 0.645 |
| Height (cm) | 165 ± 8.6 | 165 ± 9.2 | 0 | 1 |
Demographic study for age, weight and height there is no statistical significance between the two groups.
Table 1: Comparative study of age, weight and height between groups I and II.
Hemodynamic changes
Systolic Blood Pressure: Base-line systolic blood pressure (SBP) has showed no significant differences between the two groups. As regarding the changes in intraoperative (SBP), there was decrease in SBP in the two groups at time 5 and 10 minutes after induction of anesthesia, these results were more obvious in the 2nd group (TSA-group) than the 1st group (TEA-group) (Table 2).
| Time | Group I | Group II | Student t-test | |
|---|---|---|---|---|
| Mean ± SD | Mean ± SD | t | p-value | |
| Before | 130 ±9.8 | 125.5±7.3 | 1.647 | 0.108 |
| 5 | 116.6±5.9 | 102±3.7 | 9.376* | <0.001* |
| 10 | 100.5±3.7 | 90.7±4.5 | 7.523* | <0.001* |
| 15 | 99.5±3.6 | 90.8±4.2 | 7.034* | <0.001* |
| 20 | 100.9±4.4 | 94.3±3.5 | 5.250* | <0.001* |
| 25 | 102.9±5.2 | 94.6±6 | 4.675* | <0.001* |
| 30 | 105.9 ±5.2 | 100.4±2.7 | 4.198* | <0.001* |
| 35 | 108.5±4.2 | 103.6±2.6 | 4.436* | <0.001* |
| 40 | 114.3±4 | 107.2±3.8 | 5.755* | <0.001* |
| 45 | 116.2±4.5 | 110.8±3.3 | 4.328* | <0.001* |
| 50 | 121.3±4.8 | 113.3±3.6 | 5.963* | <0.001* |
| 55 | 126.9±3.6 | 119.6±3.6 | 6.412* | <0.001* |
| 60 | 128.7±2.6 | 122.3±2.6 | 7.784* | <0.001* |
Table 2: Systolic blood pressure (mean ± SD) of the two groups of patients in mmHg, before anesthesia (baseline) and 5 minute intervals within the first hour of surgery in the two groups.
| Time | Group I | Group II | Student t-test | |
|---|---|---|---|---|
| Mean ± SD | Mean ± SD | t | p-value | |
| Before | 83.5 ± 3.9 | 85.6 ± 2.9 | 1.932 | 0.061 |
| 5 | 69.7 ± 3.5 | 64.2 ± 4.2 | 4.499* | <0.001* |
| 10 | 61.4 ± 2.7 | 47.8 ± 3.3 | 14.265* | <0.001* |
| 15 | 58.7 ± 3.1 | 50.05 ± 3.5 | 8.274* | <0.001* |
| 20 | 57.6 ± 3.2 | 53 ± 2.2 | 5.298* | <0.001* |
| 25 | 61 ± 2.7 | 57.9 ± 1.8 | 4.272* | <0.001* |
| 30 | 64.7 ± 2.1 | 60.8 ± 2.7 | 5.099* | <0.001* |
| 35 | 68.5 ± 2.1 | 63.05 ± 2.1 | 8.207* | <0.001* |
| 40 | 70.9 ± 1.6 | 65 ± 1.3 | 12.799* | <0.001* |
| 45 | 74.3 ± 1.6 | 68.9 ± 1.9 | 9.722* | <0.001* |
| 50 | 75.05 ± 1.7 | 71.15 ± 1.3 | 8.150* | <0.001* |
| 55 | 77.1 ± 2.02 | 73.2 ± 2.02 | 6.105* | <0.001* |
| 60 | 78.9 ± 2.05 | 74.6 ± 1.1 | 8.266* | <0.001* |
Table 3: Diastolic blood pressure (mean ± SD) of the 2 groups of patients in mmHg, before anaesthesia (baseline) and 5-minute intervals within the first hour of surgery in the 2 groups.
Diastolic Blood Pressure: As regard preoperative diastolic blood pressure (DBP) of the two groups, there was no significant difference. At 5 min after induction of anesthesia technique, there was significant difference between the two groups. While at time of 10 min and 15 min (after IPI), there is highly significant differences between the two groups. The mean of DBP was decrease in the two groups, but this decrease was higher in the 2nd group (TSA-group) than the 1st group (Table 3).
Mean arterial Blood Pressure: As regard preoperative mean blood pressure of the two groups, there was no significant difference. The maximum decrease of systolic blood pressure showing group II than group I at 5, 10, 15 min of surgery and then systolic blood pressure gradually rises to reach nearby the pre-operative level (Table 4).
| Time | Group I | Group II | Student t-test | |
|---|---|---|---|---|
| Mean ± SD | Mean ± SD | t | p-value | |
| Before | 99.10 ± 5.50 | 98.20±6.80 | 0.460 | 0.648 |
| 5 | 81.30 ± 2.80 | 71.90±1.50 | 13.234* | <0.001* |
| 10 | 75.30 ± 2.40 | 57.20±2.10 | 25.382* | <0.001* |
| 15 | 71.30 ± 2.30 | 61.50±2.00 | 14.379* | <0.001* |
| 20 | 72.80 ± 2.30 | 64.50±2.00 | 12.178* | <0.001* |
| 25 | 73.50 ± 2.10 | 66.50±1.30 | 12.675* | <0.001* |
| 30 | 77.40 ± 2.10 | 70.30±1.80 | 11.480* | <0.001* |
| 35 | 80.00 ± 1.20 | 72.90±2.10 | 13.128* | <0.001* |
| 40 | 82.20 ± 1.80 | 75.30±2.50 | 10.017* | <0.001* |
| 45 | 84.60 ± 2.70 | 78.60±3.00 | 6.648* | <0.001* |
| 50 | 87.10 ± 2.00 | 83.00±3.20 | 4.859* | <0.001* |
| 55 | 88.90 ± 2.60 | 85.10±2.40 | 4.803* | <0.001* |
| 60 | 90.50 ± 1.50 | 86.90±2.30 | 5.863* | <0.001* |
Table 4: Mean blood pressure (mean ± SD) of the 2 groups of patients in mmHg, before anesthesia (baseline) and 5-minute intervals within the first hour of surgery in the 2 groups.
Heart Rate: As regard the heart rate there was no statistically significant difference (p>0.05) between the baseline of the two groups, but there is high statistically significant increase of mean value heart rate in 5 min intervals within the first hour of surgery in groups I and II compared to baseline (Table 5).
| Time | Group I | Group II | Student t-test | |
|---|---|---|---|---|
| Mean ± SD | Mean ± SD | t | p-value | |
| Before | 75.20 ± 3.70 | 76.60 ± 2.60 | 1.385 | 0.174 |
| 5 | 73.00 ± 2.70 | 86.65 ± 2.80 | 15.694* | <0.001* |
| 10 | 71.75 ± 1.80 | 89.55 ± 3.20 | 21.682* | <0.001* |
| 15 | 68.20 ± 1.60 | 90.20 ± 2.70 | 31.439* | <0.001* |
| 20 | 68.00 ± 1.60 | 90.70 ± 2.10 | 38.452* | <0.001* |
| 25 | 66.30 ± 1.70 | 90.15 ± 2.40 | 36.266* | <0.001* |
| 30 | 66.25 ± 1.70 | 90.45 ± 2.70 | 33.920* | <0.001* |
| 35 | 70.45 ± 1.30 | 89.75 ± 1.40 | 45.178* | <0.001* |
| 40 | 72.15 ± 1.50 | 89.25 ± 1.50 | 36.050* | <0.001* |
| 45 | 71.90 ± 1.20 | 90.10 ± 1.10 | 49.999* | <0.001* |
| 50 | 73.15 ± 1.20 | 90.10 ± 1.20 | 44.667* | <0.001* |
| 55 | 72.40 ± 1.50 | 90.60 ± 1.50 | 38.369* | <0.001* |
| 60 | 71.75 ± 1.30 | 91.10 ± 1.20 | 48.913* | <0.001* |
Table 5: Heart rate (mean ± SD) before anesthesia (baseline) and 5-minute intervals within the first hour of surgery in the two groups of patients, (beat/min).
Respiratory changes
O2 saturation: Table 6 shows no statistically significant difference of the mean values of O2 saturation (p>0.05) between the baseline of two groups of patients and the same, there is no statistically significant different of the mean values of O2 saturation of 5 min interval within the first hour of surgery in the two groups.
| Time | Group I | Group II | Student t-test | |
|---|---|---|---|---|
| Mean ± SD | Mean ± SD | t | p-value | |
| Before | 98.85 ± 0.70 | 97.80 ± 0.70 | 4.743* | <0.001* |
| 5 | 97.05 ± 0.70 | 98.05 ± 0.70 | 4.518* | 0.001* |
| 10 | 98.50 ± 0.60 | 97.40 ± 0.50 | 6.299* | <0.001* |
| 15 | 97.40 ± 0.50 | 98.40 ± 0.60 | 5.726* | <0.001* |
| 20 | 98.25 ± 0.70 | 97.00 ± 0.70 | 5.647* | <0.001* |
| 25 | 97.50 ± 0.70 | 98.85 ± 0.80 | 5.679* | <0.001* |
| 30 | 98.95 ± 0.70 | 97.55 ± 0.50 | 7.278* | <0.001* |
| 35 | 97.05 ± 0.80 | 97.80 ± 0.80 | 2.965* | 0.005* |
| 40 | 98.80 ± 0.80 | 98.95 ± 0.70 | 0.631 | 0.532 |
| 45 | 98.80 ± 0.80 | 97.20 ± 0.70 | 6.731* | <0.001* |
| 50 | 97.15 ± 0.70 | 97.90 ± 0.70 | 3.388* | 0.002* |
| 55 | 98.20 ± 0.60 | 98.85 ± 0.60 | 3.426* | 0.002* |
| 60 | 98.70 ± 0.70 | 97.10 ± 0.70 | 7.228* | <0.001* |
Table 6: Peripheral oxygen saturation (%) mean ± SD, before anaesthesia (baseline) and 5-minute intervals within the first hour of surgery in the two groups of patients.
End tidal CO2: In end tidal CO2 show no statistically significant difference of the mean values of end tidal CO2 (P>0.05) between baseline values of two groups of patients, also no statistically significant difference of the mean values of 5 min interval within the first hour of surgery in the two groups as show in Table 7.
| Time | Group I | Group II | Student t-test | |
|---|---|---|---|---|
| Mean ± SD | Mean ± SD | t | p-value | |
| Before | 36.85 ± 1.50 | 35.85 ± 1.30 | 2.253* | 0.030* |
| 5 | 35.65 ± 0.70 | 34.65 ± 0.70 | 4.518* | <0.001* |
| 10 | 34.95 ± 1.60 | 36.95 ± 1.50 | 4.078* | <0.001* |
| 15 | 35.75 ± 1.40 | 35.75 ± 1.30 | 0.0 | 1.000 |
| 20 | 36.60 ± 1.30 | 36.60 ± 1.00 | 0.0 | 1.000 |
| 25 | 37.55 ± 1.40 | 37.55 ± 1.30 | 0.0 | 1.000 |
| 30 | 35.00 ± 0.80 | 34.00 ± 0.80 | 3.953* | <0.001* |
| 35 | 37.65 ± 1.10 | 36.65 ± 1.10 | 2.875* | 0.007* |
| 40 | 35.00 ± 0.10 | 36.00 ± 0.20 | 20.00* | <0.001* |
| 45 | 36.35 ± 0.70 | 34.35 ± 0.70 | 9.035* | <0.001* |
| 50 | 37.85 ± 0.70 | 35.85 ± 0.70 | 9.035* | <0.001* |
| 55 | 35.40 ± 1.30 | 36.40 ± 1.30 | 2.433* | 0.020* |
| 60 | 37.60 ± 1.40 | 34.60 ± 1.40 | 6.776* | <0.001* |
Table 7: End tidal CO2 (mmHg) of the two groups of patients in mean ± SD, before anaesthesia (baseline) and 5-minute intervals within the first ho¬ur of surgery.
Recovery time
In Table 8, there is statistically significant increase of the mean value of recovery time in group I compared to group II. There is significant change between the two groups as regard recovery time.
| Recovery time (minutes) | Student t-test | |||
|---|---|---|---|---|
| Range | Mean ± SD | t | p-value | |
| Group I | 3.5-5.5 | 4.628 ± 0.620 | 17.163* | <0.001* |
| Group II | 7.5-9.5 | 8.488 ± 0.792 | ||
| t, p: t and p-values for Student t-test for comparing between the two groups; p<0.05 S; *p<0.001 HS; p>0.05 NS p>0.05=no significant p<0.01=highly significant p<0.05=significant |
||||
Table 8: Recovery time (minutes) from discontinuation of anaesthesia until the full recovery of patients in the two groups of patients (mean ± SD).
Post-operative VAS assessment
Post-operative pain was compared at the time 0, 1, 2, 4 and 8 hour by using VAS. At the time (immediately after finishing surgery) 14 patients (70%) in group I and 15 patient (75%) in group II scored 0 and 6 patient (30%) in group I, 5 patients (25%) in group II scored 1. One hour after surgery, (12 patients (60%) in group I and 15 patient (75%) in group II scored 0, while 5 patients (25%) in group I and 4 patients (20%) in group II scored I and 3 patients (15%) in group I and 4 patients (20%) in group II scored 2. Two hours after surgery, ( 2 patients (10%) in group I, 3 patients (15%) in group II scored 0, 16 patients (80%) in group I, 17 patients (85%) in group II scored 1 and 2 patients (10%) in group I scored 2. Four hours after surgery, (15 patients (75%) in group I, 16 patients (80%) in group II scored 1. 4 patients (20%) in group I, and 3 patients (15%) in group II scored 2. One patient (5%) in group I, and 1 patient (5%) in group II scored 3 (Tables 9 and 10).
| Assessment Time | Score | Group (I) | Group (II) | ||
|---|---|---|---|---|---|
| No. | % | No. | % | ||
| 0 | 0 1 2 3 4 5 6 |
14 6 - - - - - |
70% 30% - - - - - |
15 5 - - - - - |
75% 25% - - - - - |
| 1 | 0 1 2 3 4 5 6 |
12 5 3 - - - - |
60% 25% 15% - - - - |
15 4 1 - - - - |
75% 20% 5% - - - - |
| 2 | 0 1 2 3 4 5 6 |
2 16 2 - - - - |
10% 80% 10% - - - - |
3 17 - - - - - |
15% 85% - - - - - |
| 4 | 0 1 2 3 4 5 6 |
- 15 4 1 - - - |
- 75% 20% 5% - - - |
- 16 3 1 - - - |
- 80% 15% 5% - - - |
| 8 | 0 1 2 3 4 5 6 |
- - 8 4 4 4 - |
- - 40% 20% 20% 20% - |
- - 8 4 4 4 - |
- - 50% 20% 20% 10% - |
Table 9: Postoperative VAS 0, 1, 2,4 and 8 hour in the two groups of patients.
| Assessment Time | Group I | Group II | t | p-value |
|---|---|---|---|---|
| 0 | 0.30 ± 0.47 | 0.25 ± 0.44 | 0.347 | 0.730 |
| 1 | 0.55 ± 0.76 | 0.30 ± 0.57 | 1.177 | 0.245 |
| 2 | 1.00 ± 0.46 | 0.85 ± 0.37 | 1.136 | 0.263 |
| 8 | 1.30 ± 0.57 | 1.20 ± 0.52 | 0.580 | 0.566 |
Table 10: Postoperative VAS at 0, 1, 2 and 8hour (mean ± SD) in the two groups of patients.
Post-operative analgesic requirement
There is significant difference between the two groups as regard postoperative analgesic requirement (Table 11).
| postoperative analgesic requirement | Student t-test | |||
|---|---|---|---|---|
| Range | Mean ± SD | t | p-value | |
| Group I | 4.8-8.3 | 10.535 ± 1.655 | 0.235 | 0.816 |
| Group II | 4.7-9.2 | 10.406 ± 1.820 | ||
Table 11: Comparison between groups as regards postoperative analgesic requirement.
Perioperative complications
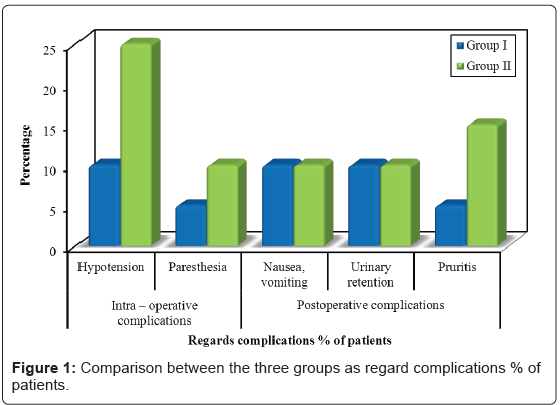
There is significant difference between the two groups as regards hypotension (p<0.05). There is no significant difference between the two groups as regards postoperative nausea and vomiting (p<0.05). Paresthesia occurred one case in group I, two patients in group II during initial insertion of the spinal needle; these symptoms responded to needle withdrawal and not leading to any postoperative sequelae or neurological deficits. There was no significant difference between two groups as regard to urinary retention, (p>0.05). There was no significant difference between the two groups as regards pruritis (Table 12) (Figure 1).
| Variables | Group I (TEA) | Group II (TSA) | Chi – square test | ||
|---|---|---|---|---|---|
| p-value | Significance | ||||
| Intra-operative complications | Hypotension | 2 (10%) | 5 (25%) | FEp=0.407 | NS |
| Paresthesia | 1 (5%) | 2 (10%) | FEp=1.000 | NS | |
| Postoperative complications | Nausea, vomiting | 2 (10%) | 2 (10%) | FEp=1.000 | NS |
| Urinary retention | 2 (10%) | 2 (10%) | FEp=1.000 | NS | |
| Pruritis | 1 (5%) | 3 (15%) | FEp=0.605 | NS | |
| FE: Fisher Exact for Chi square test | |||||
Table 12: Comparison between the two groups as regards complications % of patients.
Ambulation time
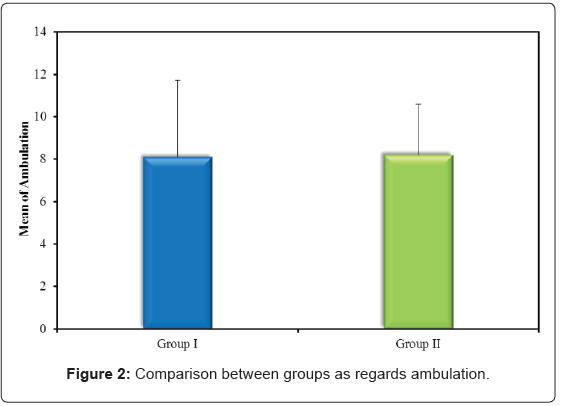
There is no significant difference between the two groups (Table 13) (Figure 2).
| Ambulation | Student t-test | |||
|---|---|---|---|---|
| Range | Mean ± SD | t | p-value | |
| Group I | 2.7-18.7 | 8.107 ± 3.604 | 0.114 | 0.910 |
| Group II | 3.5-12.6 | 8.217 ± 2.376 | ||
Table 13: Comparison between groups as regards ambulation time.
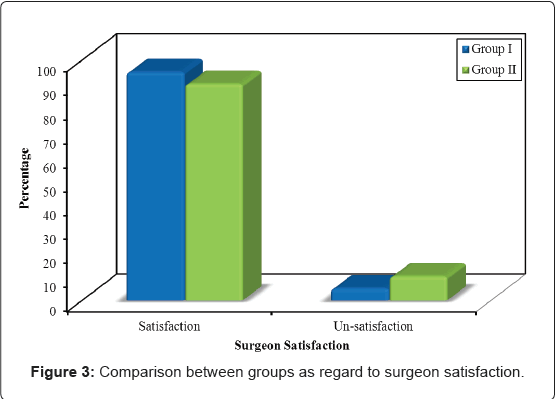
Surgeon satisfaction
The surgeons reported that there was good muscle relaxation and no technical problems and that both techniques of regonial anesthesia (Table 14) (Figure 3).
| Surgeon satisfaction | Group I Mean ± SD |
Group II Mean ± SD |
|---|---|---|
| Satisfaction | 19 (95%) | 18 (90%) |
| Un-satisfaction | 1 (5%) | 2 (10%) |
| Total | 20 (100%) | 20 (100%) |
| Chi-square test | 0.360 | |
| FEp-value | 1.000 (NS) | |
| FE: Fisher Exact for Chi square test | ||
Table 14: Comparison between groups as regards Surgeon satisfaction.
Discussion
The results obtained in this work are to be compared with related researches done by others. Results in agreement or not are to be analyzed in more details to find the explanations for them. More over evaluation and applications of these results are to be discussed taking into consideration the basic anatomical, physiological and pharmacological bases. Regional anesthesia can be considered as a valid option for patients with breast surgery. There are several advantages regional anesthesia. Since the patient is awake there is early detection of complications. Also it provides excellent post-operative analgesia with a lower incidence of post-operative nausea and vomiting.
This work aimed to compare between thoracic epidural anaesthesia (TEA) and segmental thoracic spinal anaesthesia (TSA) for breast surgeries as regard to hemodynamic changes (BLP, HR, oxygen saturation, ETCO2), postoperative pain control, postoperative analgesic requirements, surgeon satisfaction, postoperative ambulation time and perioperative complication. After ethical committee approval and informed consent from patients, this prospective, single blind randomized controlled study was carried out in Al-Azhar university hospitals on 40 female patients (ASA physical status I-II), scheduled for elective breast surgery, they were randomly allocated into two equal groups 20 patients each:
Group I (TEA): (thoracic epidural anaesthesia).
Group II (TSA): segmental thoracic spinal anaesthesia (T5-T6).
Epidural anesthesia is one of the most versatile and extensively utilized regional anaesthetic techniques. It is used not only for surgery, but also for obstetrics and trauma as well as acute, chronic and cancer pain states. Thoracic epidural anaesthesia (TEA) has been consistently shown to provide excellent pain relief, to facilitate early ambulation. Many used regional anaesthesia alone for laparoscopic cholecystectomy in patients with chronic obstructive airway disease [4,8,9]. It has been also used in other studies, alone for laparoscopic cholecystectomy in healthy patients [4,10,11].
Different regional techniques have been attempted during breast surgery; including thoracic epidural [1] and thoracic paravertebral block [3]. However, the delayed onset of block, patchy sensory block, and large volume of local anesthetic used with potential risk for local anesthetic toxicity are still issues of concern when applying these techniques during breast surgery. Jonnesco et al. described the use of spinal anesthesia for surgeries in the skull, head, neck, and the thorax. The punctures were performed between the 1st and the 2nd thoracic vertebrae, which resulted in good analgesia for the head, neck, and upper limbs [12]. Recently segmental thoracic spinal anesthesia has been used for laparoscopic cholecystectomy was practiced by [1] and abdominal surgeries, we depended on the fact that the posterior subarachnoid space is wider at the mid-thoracic region compared with the upper and lower thoracic regions and do segmental thoracic spinal anesthesia at mid thoracic region (T5-T6) [13].
Advantages, there is no blockade of the lower extremities, i.e. little caudal spread. This means that a significantly larger portion of the body no venal dilation, and may offer a compensatory buffer to adverse changes in blood pressure intra-operatively [6], the dosing of the anesthetic is exceedingly low, the degree of muscle relaxation achievable without central or peripheral respiratory or circulatory depression and the patients have motor control over their legs during the surgery, which in turn means many patients exhibit a high level of satisfaction with the technique and decreased anxiety [7].
We were concerned about three issues: The risk for spinal cord injury, cephalad spread of local anesthetic causing high or total block and hemodynamic or respiratory compromise due to block of cardio accelerator fibers or intercostal nerves. Concerning the first issue, we depended on the fact that the posterior subarachnoid space is wider at the mid-thoracic region compared with the upper and lower thoracic regions. Imbelloni et al., who performed MRI of the thoracic spine in 50 patients. They found that the posterior dural-spinal cord distance was significantly greater at the mid-thoracic region (T5=5.8 ± 0.8 mm) compared with the upper (T2=3.9 ± 0.8 mm) and lower thoracic levels (T10=4.1 ± 1.0 mm) [13]. Another anatomical study performed by Lee et al. showed very similar results. In their study, they performed MRI of the thoracic and lumbar spines in the supine, laterally recumbent, and sitting (head-down) positions. They found that the separation of the dura mater and spinal cord is greatest posterior in the middle thoracic region compared with the upper and lower thoracic levels for all three positions. These results encouraged us to perform the block at the T5 level to minimize the risk of injuring the spinal cord [7].
Concerning the second and third issues, we chose to exclude patients with a BMI more than 35 kg/m2 and height less than 160 cm to minimize factors that may contribute to a higher spread of block and minimize dose and volume duo to the amount of CSF at thoracic levels is diminished compared to lumbar and cervical levels and the thoracic nerve roots are very slight compared to segments above and below [14]. Thus, there is less anesthetic dilution per segmental unit of distance from the site of injection, and the roots are easily blocked due to their small size, both factors predicting efficient blockade of these segments. Encouraged by these studies, we decided to restudy the feasibility of thoracic epidural anaesthesia (TEA) and segmental thoracic spinal anaesthesia techniques for patients undergoing breast surgery.
Results
Our study results showed that all patients under (thoracic epidural anaesthesia) and segmental thoracic spinal anaesthesia tolerated the procedure well. In the present study, the values of systolic, mean and diastolic blood pressure were decreased considerably in (groups I and II) at the first 15 minutes of surgery, then on subsequent readings 20, 25, 30 up to 60 minutes there was gradual returning of blood pressure toward the baseline.
The cardiovascular effects of neuroaxial blocks are similar in some ways to the combined use of intravenous α-1 and β-adrenergic blockers: decreased heart rate and arterial blood pressure. The sympathectomy that accompanies the technique depends on the height of the block, with the sympathectomy typically described as extending for two to six dermatomes above the sensory level with spinal anaesthesia and at the same level with epidural anaesthesia [15].
This result causes venous and arterial vasodilatation, but because of the large amount of blood in the venous system (approximately 75% of total blood volume), the venodilatation effect predominates because of the limited amount of smooth muscle in venules, whereas the vascular smooth muscle on the arterial side of the circulation retains a considerable degree of autonomous tone. After neuraxial block-induced sympathectomy, if normal cardiac output is maintained, total peripheral resistance should decreased only 15% to 18% in normovolemic healthy patients even with near total sympathectomy. Thus preloading with 15 ml/kg crystalloid solution in healthy patients may partially compensate for the pooling of blood in the venous capacitance vessels for sympathetctomy. Thus prevention of hypotension involves rapidly increasing plasma volume immediately before and during administration of the block [16].
The significant decrease in blood pressure (systolic, mean and diastolic) that we detected in this study is actually not only attributed to the effect of epidural anaesthesia which had its maximum sympathetic blockade in the first 15-20 minutes of surgery but also due to induction of general anaesthesia. Then the effect of sympathetic block of epidural anaesthesia was gradually decreased returning back the blood pressure toward the baseline. Gramatica et al. reported that all 29 patients of his study under thoracic epidural anaesthesia. The blood pressure and heart rate remained stable during the procedure [8]. Pursnani et al. reported in his study of laparoscopic cholecystectomy performed under TEA in patients with chronic respiratory disease that all patients under thoracic epidural anaesthesia had no change in their cardio-respiratory status all over the procedure [9]. The present study did not detect any significant differences between the baseline and 5-minutes intervals within the first hour of surgery in the two groups as regard O2 saturation measured by pulse oximetry.
The pulse oximetery showed non-significant changes between groups intraoperatively all over the procedure. Oxygen saturation (SPO2) was >96% all over the procedure in the groups. This was in accordance with Warner et al. and Liu et al. who showed that thoracic epidural anaesthesia may improve postoperative pulmonary function in part by enhancing diaphragmatic function by attenuating reflex spinal inhibition of diaphragmatic activity as well as by preserving hypoxic pulmonary vasoconstriction in poorly ventilated segments [17,18].
Popping et al. resulted from his study that epidural anaesthesia improves lung function and blood oxygenation, so protects against pneumonia following abdominal or thoracic surgery [19] Also, Tenenbein et al. they concluded from their study that TEA decreases postoperative pain and atelectasis and improves pulmonary function in patients undergoing coronary artery bypass surgery [20]. All these studies were in agree with my study that thoracic epidural anaestheisa doesn’t affect respiration.
There was no significant change in end tidal CO2 at the first hour of surgery in all groups. Comparing end tidal CO2 at zero time and 5 minutes intervals in groups I and II, group showed no significant difference in the mean values all over the first hour of surgery. This is in agreement with the results obtained by [21].
Shenkman et al. observed gradual rising of end tidal CO2 when they allowed morbidly obese patient who received epidural anaesthesia to breath spontaneously during abdominal surgery. This was explained by the supine position and the paralysis of abdominal muscles in those morbidly obese patients [22]. By comparing mean values of end tidal CO2 in groups I and II we found that no change in end tidal CO2. There is significant change between groups as regard recovery time as there is significant increase of the mean value of recovery time in group I compared to group II.
The primary reason for using an epidural analgesia is to provide optimal pain relief. This study found a significant reduction in the pain experienced after breast surgery. Seventy percent of the TEA patients experienced no pain or only mild pain at all times postoperatively. (TEA) appeared to provide superior pain relief at all times while being administered [23].
Zingg et al. who studied the influence of TEA on postoperative pain relief and ileus after laparoscopic colorectal resection, he concluded that TEA provides a significant benefit in terms of less analgesic consumption, better postoperative pain relief [24].
In our study there was no significant difference between both groups regarding postoperative analgesic requirement. Pain was easily controlled with paracetamol infusion in groups I and II which means that good postoperative pain relief with thoracic epidural anesthesia and thoracic spinal group.
Paresthesia occurred one case in group I, two patients in group II during initial insertion of the spinal needle; these symptoms responded to needle withdrawal and not leading to any postoperative sequelae or neurological deficits. Paresthesia can occur with any technique of spinal anesthesia, but are of potentially greater significance when the needle is inserted above the termination of the spinal cord. The low potential for cord damage with this technique was given in the earlier case report by Zundert et al. [4] where it was noted that the thoracic segment of the cord lies anteriorly. Imbelloni et al. showed in their study that the incidence of paresthesia in a study with 300 patients subjected to thoracic spinal puncture at T10-11 was 4.67% in the cut needle and 8.67% in the pencil point needle group, and without sequelae, similar to the incidence reported by other investigators in lumbar spinal anesthesia [13]. There was no significant difference between two groups as regard to urinary retention, (p>0.05). There was no significant difference between the two groups as regards pruritis.
In our study there was no significant difference between groups as regards ambulation time. Early ambulation in obese patients is very important as they have increased incidence of deep venous thrombosis and pulmonary embolism also obesity is a major risk factor for sudden postoperative death from massive pulmonary thrombo-embolism so
early ambulation protects them from these risks.
Conclusion
Thoracic epidural block was an adequate option for mastectomy, among its advantages, the quality of postoperative analgesia and shorter recovery time with the consequent early hospital discharge can be mentioned.
References
- Belzarena SD (2008)Comparative Study between thoracic epidural block and general anesthesia for oncologic mastectomy. Rev Bras Anestesiol 58: 561-568.
- Nesmith RL, Herring SH, Marks MW, Speight KL, Efird RC, et al. (1990)Early experience with high thoracic epidural anesthesia in outpatient submuscular breast augmentation. AnnPlastSurg 24: 299-303.
- Klein SM, Bergh A, Steele SM, Georgiade GS, Greengrass RA (2000)Thoracic paravertebral block for breast surgery. AnesthAnalg 90:1402-1405
- Van Zundert AA, Stultients G, Jakimowicz JJ, Van den Borne BE, van der Ham WG, et al. (2006)Segmental spinal anaesthesia for cholecystectomy in a patient with severe lung disease. Br J Anaesth 96: 464-466.
- Mahmoud AA, Hussein HA, Girgis K, Kamal AM, Nafady HA (2014) The novel use of spinal anesthesia at the mid-thoracic level: A feasibility study. Egypt J CardiothoracAnesth8: 21-26.
- Monk TG, Saini V, Weldon BC, Sigl JC (2005)Anesthetic management and one-year]mortality after noncardiac surgery. AnesthAnalg 100: 4-10.
- Lee RA, Van Zundert AA, Botha CP, Lataster LM, Van Zundert TC, et al. (2010)The anatomy of the thoracic spinal canal in different postures: A magnetic resonance imaging investigation. RegAnesth Pain Med 35:364-369.
- Gramatica L Jr, BrasescoOE, Mercado Luna A,Martinessi V, Panebianco G, et al. (2002) Laparoscopic cholecystectomy performed under regional anaesthesia in patients with obstructive pulmonary disease. SurgEndosc 16: 472-475.
- Pursnani KC, Bazza Y, Calleja M, Mughal MM (1998) Laparoscopic cholecystectomy under epidural anesthesia in patients with chronic respiratory disease. SurgEndosc 12: 1082-1084.
- Langenberg CJM, Huygan F, Go PMNYH, Gouma DJ (1992) Thoracic epidural anaesthesia for laparoscopic cholecystectomy. Regional Anaesth 17: 35.
- Hamad MA, Ibrahim El-Khattary OA (2003)Laparscopic cholecystectomy under spinal anaesthesia with nitrous oxide pneumoperitoneum: A feasibility Study. SurgEndsoc 17: 1426-1428.
- Maurer K, Ekatodramis G, Rentsch K, and Borgeat A(2002)Interscalene and infraclavicular block for bilater distal radius fracture. AnesthAnalg94:450-452.
- Imbelloni LE, Pitombo PF, Ganem EM (2010)The incidence of paresthesia and neurologic complications after lower spinal thoracic puncture with cut needle compared to pencil point needle. Study in 300 patients. J AnesthClin Res 1: 1-4.
- Mcleod GA and Cumming C (2004)Thoracic epidural anesthesia and analgesia. ContinEducAnaesthCrit Care Pain 4:16-19.
- Greene NM (1981) Physiology of spinal anesthesia, (3rdedn.) Williams and Wilkins. Baltimore.
- Tetzlaff EJ (1996)Epidural and caudal blocks. In: Morgan GE, Mikhail MS editors. Clinical Anesthesiology (2ndedn.) Appleton & Lang; pp:221-244.
- Warner D, Warner M and Ritman E (1996) Human chest wall function during epidural anesthesia. Anesthesiology 1996; 85:761-73.
- Liu SS, Bernards CM (2002)Exploring the epidural trail. RegAnesth Pain Med 27:122-124.
- Popping DM, Elia N, Marret E, Remy C, Tramer MR (2008) Protective effects of epidural analgesia on pulmonary complications after abdominal and thoracic surgery: A meta-analysis. Arch Surg 143: 990-999.
- Tenenbein PK, Debrouwere R, Maguire D, Duke PC, Murhead B, et al. (2008)Thoracic epidural analgesia improves pulmonary function in patients undergoing cardiac surgery. Can J Anaesthe 55: 344-350.
- Zerah F, Harf A, Perlemuter L, Lorino H, Lorino AM, et al. (1993) Effects of obesity on respiratory resistance.Chest 103: 1470-1476.
- Shenkman Z, Shir Y, Brodsky JB (1993): Perioperative management of the morbidly obese patient. Br J Anesthesia 70:349.
- Royse C, Royse A, Soeding P (2003)Prospective randomized trial of high thoracic epidural analgesia for coronary artery bypass surgery. Ann ThoracSurg 75:93-100.
- Zingg U, Miskovic D, Haeml CT, Ernil L, Oertli D, et al. (2009) Influence of thoracic epidural analgesia on postoperative pain relief and ileus after laparoscopic colorectal resection: Benefit with epidural analgesia. SurgEndosc 23: 276-282.
Relevant Topics
- Acupuncture
- Acute Pain
- Analgesics
- Anesthesia
- Arthroscopy
- Chronic Back Pain
- Chronic Pain
- Hypnosis
- Low Back Pain
- Meditation
- Musculoskeletal pain
- Natural Pain Relievers
- Nociceptive Pain
- Opioid
- Orthopedics
- Pain and Mental Health
- Pain killer drugs
- Pain Mechanisms and Pathophysiology
- Pain Medication
- Pain Medicine
- Pain Relief and Traditional Medicine
- Pain Sensation
- Pain Tolerance
- Post-Operative Pain
- Reaction to Pain
Recommended Journals
Article Tools
Article Usage
- Total views: 4222
- [From(publication date):
July-2017 - Mar 31, 2025] - Breakdown by view type
- HTML page views : 3321
- PDF downloads : 901