Community-Based Participatory Research: Cross-Sectional Study Understanding Malaria in Rural Northern Uganda
Received: 27-Dec-2022 / Manuscript No. jcmhe-22-79326 / Editor assigned: 29-Dec-2022 / PreQC No. jcmhe-22-79326 (PQ) / Reviewed: 12-Jan-2023 / QC No. jcmhe-22-79326 / Revised: 17-Jan-2023 / Manuscript No. jcmhe-22-79326 (R) / Published Date: 24-Jan-2023 DOI: 10.4172/2168-9717.1000794
Abstract
Objective: Community-Based Participatory Research (CBPR) is founded on the principle of recognizing community members as equal research partners in order to best understand and address their health needs. Recognizing the scarcity of CBPR in global malaria elimination efforts, this study trained youth in Lira, Uganda to collect data on self-reported malaria prevalence, access to prevention tools, and perceptions around behaviors to prevent malaria in their local communities.
Methods: Recruited Youth Public Health Ambassadors (YPHA) received training through comprehensive workshops on public health topics such as WASH, vector borne diseases, and public health surveillance techniques. YPHAs distributed long lasting insecticide treated nets (LLINs) and collected data from 512 households on malaria behaviors, knowledge, and attitudes. Results from the surveys were analyzed using Qualtrics, Microsoft Excel, and SPSS software.
Results: Households reported owning fewer mosquito nets per household than recommended by the WHO, with only 5.71% of households of >9 people reporting an adequate number of nets. Most respondents recognized the value of sleeping under net, but reported barriers to doing so. Households in Aromo subcounty were 70% more likely to report using nets in the past 7 days than households in Ayami. Households with pregnant females were more likely to report using nets in the preceding week, with their odds increased by 63% compared to households with non-pregnant members. Households reporting sleeping under nets as “not effective” were 75% less likely to use nets in the past 7 days compared to those who reported sleeping under nets as “effective.”
Conclusion: The data highlight the need for improved access to LLINs, especially in homes with pregnant women/young children, and for further community discussions on barriers to net use. It supports CBPR’s pivotal role in empowering affected communities to minimize the burden of malaria in northern Uganda.
Keywords: CBPR; Plasmodium; Mosquito net; Insectic
Abbreviations
(USC GRIT Lab) University of Southern California Global Research, Implementation, and Training Lab; (RUFC) Ray United FC; (CCI) Children’s Chance International; (UNCST) Uganda National Council for Science and Technology; (CBPR) Community- Based Participatory Research, Implementation, and Training; (LLIN) Long-lasting Insecticide-treated Nets; (IRS) Indoor Residual Spraying; (IPT) Intermittent Preventive Therapy; (MIS): Uganda Malaria Indicator Survey; (VHT) Village Health Team
Introduction
Malaria prevention and control has received considerable attention and cross-sectoral support in Uganda. The Ugandan Ministry of Health and international partners such as the President’s Malaria Initiative, the Global Fund, and the United States Peace Corps have long championed a robust agenda to eliminate malaria. There have been numerous efforts to reduce the burden of malaria via long lasting insecticide treated nets (LLINs), indoor residual spraying (IRS), treatment with artemisinin-based therapies, and intermittent preventive therapy (IPT) [1].
The impact of this investment has been seen through Uganda’s decreasing malaria mortality rate [2]. However, malaria remains the second largest cause of death in the country, unchanged since 2009, and is one of five countries that account for over half of the malaria cases worldwide [2,3]. Moreover, although mortality decreased from 6,100 to 5,027 deaths between 2015 and 2019, incidence increased from 7 to 13 million [2].
Griffing et al. describes how Brazil’s history of malaria controls and current struggles are linked to historically colonist-enforced biological and ecological methods that lacked local community engagement [4]. The failure to substantially reduce malaria in Uganda may be similarly due in part to malaria prevention interventions which are not informed by specific community needs or behaviors.
Community-Based Participatory Research (CBPR) is an evidence based research method well suited to respond to this shortcoming and build local ownership of malaria prevention and control. The purpose of CBPR is to engage community members as active and equal partners in research, allowing them to investigate issues of concern in their own communities [5]. In doing so, CBPR initiates more accurate analysis and effective response to public health issues. CBPR principles include building on community strengths, facilitating an equitable partnership in all research phases, fostering capacity building among all partners, focusing on the local relevance of public health problems, disseminating results to all partners, and committing to long term sustainability [6].
Pursuing these principles, the University of Southern California Global Research, Implementation, and Training (USC GRIT) Lab, nonprofit Ray United FC (RUFC), Lira-based Children’s Chance International (CCI), and the United States Peace Corps partnered on a public health initiative using CBPR approach to assess the efficacy, usage, and attitudes towards common malaria prevention tools in Lira, Uganda. This paper outlines the methods used to prepare for and carry out the CBPR study, describes the study results, and discusses the implications of both the results and the research process.
Methods
Background preparation
In an effort to build local public health capacity and drive ownership of public health activity in Northern Uganda, RUFC and CCI launched a youth focused empowerment and training program in January 2021. The goal of the program was to train the youth in public health concepts and skills so that they could serve as data collectors, community educators, and advocates. Thirty youth aged 17-22 years were recruited from 3 sub counties (Agweng, Ayami, and Aromo) in Lira District, Uganda to serve as Youth Public Health Ambassadors (YPHA). To begin the process of selecting youth ambassadors from these sub counties, CCI community volunteers based in their respective sub counties reached out to local council representatives at the subcounty and village levels and explained the study, its objectives, and the selection process. The CCI volunteers met with parents and youth to share information about the program, and those expressing interest were taken through the recruitment requirements and key objectives, including age, availability, ability to read and write in both English and Lango Language, willingness to volunteer, and commitment to community work. In an effort to encourage female empowerment in the community, more girls were recruited for the YPHA program. Selection and recruitment of youth was done through a rigorous but transparent process chaired by local council and chairpersons, all parents, and CCI Community Volunteers. Strategies included interviews, riddles and brainstorming exercises, and speeches made in front of the selection team.
After selection, the youth ambassadors received basic public health education through a series of workshops led by RUFC staff (primarily public health students from Makerere University) and student researchers in the USC GRIT lab (who joined via Zoom). The first workshop, held in February 2021, included interactive lessons on vector-borne disease, sanitation and hygiene, sexual and reproductive health, risky behaviors, and mental health. At the end of the first workshop, the YPHAs participated in a DELPHI exercise to identify priority issues in their communities [7]. Through this exercise, the YPHAs identified malaria amongst the top public health priorities in their region. A second workshop, held in April 2021, focused on teaching public health data collection methods. During this workshop, the YPHAs and trainers developed the methodologies and tools to collect information to better understand and address the gaps in malaria control measures and prevention efforts.
Study design and sample
Under the guidance of RUFC and CCI staff and volunteers, and with technical support from USC GRIT Lab, the YPHAs carried out a cross-sectional survey of households in Agweng, Ayami, and Aromo sub counties on World Malaria Day, April 25, 2021. The Lango region in which these 3 sub counties are situated has had a consistently high malaria burden according to the 2019 Uganda Malaria Indicator Survey [8,9]. Village council leaders in each subcounty helped to identify potential participants in the study from households with community members most susceptible to malaria morbidity and mortality, such as pregnant mothers, children under 5, families with orphans and vulnerable children, people with disabilities, and the elderly (aged 60+). Potential participants were encouraged to attend a central World Malaria Day event to receive LLINs. YPHAs, paired with RUFC and CCI staff, obtained written consent in the local language from each head of household who agreed to complete the survey when collecting their LLINs.
Adapted from existing tools including the Peace Corps’ standard malaria survey, the YPHA survey included internationally standardized questions addressing access to resources, daily preventive practices, and attitudes towards malaria and malaria prevention efforts [8,10]. Male or female heads of household filled out a census giving information on each household member, including their age, sex, and use of mosquito nets over the past week. After being surveyed, each household received Peace Corps donated LLINs, the amount of which was adjusted according to the number of household members. Survey questions and consent forms were reviewed and approved by the USC Institutional Review Board, Gulu University Institutional Review Board, and the Uganda National Council for Science and Technology (UNCST).
Data management and analysis
Surveys were recorded on paper at the sites of data collection and then entered onto Qualtrics by RUFC volunteers [11]. Following data collection, student researchers at the USC GRIT Lab carried out initial data analysis using Microsoft Excel (2021) and IBM SPSS Statistics for Windows version 27 [12]. Results were shared with, and interpreted by, the YPHAs in a third data analysis and dissemination workshop.
Results
Data were collected from 512 households in the Lira district of Uganda. 27.22% of households had pregnant women, and 77.22% of households had children under 10. The population surveyed was predominantly subsistence farmers living in grass huts, obtaining food from their own gardens. Typical household meal ingredients were starches (84.53%) and beans (95.97%), with much lower reported rates of other proteins (7.63%), greens (57.63%), and fruits (19.07%). The majority of households reported spraying their compounds with insecticide 2-3 times per year (58.86%) and reported owning nets with large holes (67.37%). Although 84.32% of households reported knowing how to use their nets properly, 33.47% reported using their nets for other purposes such as fishing and livestock (Table 1).
| Demographic Value | Total | Agweng | Aromo | Ayami | |
|---|---|---|---|---|---|
| Household Type | Permanent (concrete) | 5.86% | 3.74% | 4.79% | 12.61% |
| Semi-Permanent (mud hut, brick with tin roof) | 10.35% | 11.68% | 11.64% | 3.60% | |
| Temporary (grass hut) | 83.79% | 84.58% | 83.56% | 83.78% | |
| Household Size | 1-2 Persons | 12.71% | 14.95% | 6.12% | 13.51% |
| 3-4 Persons | 34.32% | 37.85% | 30.61% | 32.43% | |
| 5-6 Persons | 28.60% | 23.83% | 36.05% | 31.53% | |
| 7+ Persons | 24.16% | 23.36% | 27.21% | 22.52% | |
| Household Members | Households with pregnant women | 27.22% | 22.90% | 24.49% | 39.64% |
| Households with children under 10 | 77.22% | 76.17% | 80.27% | 75.68% | |
| Source of Household Income | Subsistence Farming | 94.35% | 97.66% | 89.80% | 97.30% |
| Commercial Farming | 2.53% | 1.40% | 3.40% | 0.90% | |
| Petty Business | 1.56% | 0.00% | 3.40% | 1.80% | |
| Other (e.g. wages, remittances, nongovernmental aid) | 1.55% | 0.93% | 3.40% | 0.00% | |
| Household Religion | Roman Catholic | 44.44% | 53.27% | 44.22% | 27.93% |
| Pentecostal | 28.46% | 25.70% | 22.45% | 36.94% | |
| Anglican | 25.54% | 18.22% | 31.97% | 35.14% | |
| Muslim | 0.58% | 0.93% | 0.68% | 0.00% | |
| Other | 0.97% | 1.87% | 0.68% | 0.00% | |
| Household Source of Food | Own Gardens/Fields | 81.80% | 92.02% | 70.55% | 77.48% |
| Purchase at Market | 17.03% | 6.10% | 28.77% | 22.52% | |
| Collected from the Bush | 0.78% | 1.41% | 0.68% | 0.00% | |
| Aid Service | 0.39% | 0.47% | 0.00% | 0.00% | |
| Household typical meal ingredients | Starch (posho, rice, cassava) | 84.53% | 86.45% | 89.12% | 74.77% |
| Protein 1 (beans) | 95.97% | 95.79% | 95.92% | 96.40% | |
| Protein 2 (chicken, beef) | 7.63% | 6.07% | 4.08% | 15.32% | |
| Greens | 57.63% | 64.02% | 57.14% | 45.95% | |
| Fruits | 19.07% | 23.36% | 21.09% | 8.11% | |
| Household reported frequency of insecticide spray | 12 times per year | 23.89% | 23.36% | 18.37% | 31.53% |
| 2-3 times per year | 58.56% | 50.93% | 70.75% | 55.86% | |
| Never | 8.46% | 6.54% | 10.88% | 8.11% | |
| Not sure | 9.09% | 19.16% | 0.00% | 4.50% | |
| Households reported nets with large holes | Yes | 67.37% | 50.93% | 80.27% | 81.98% |
| No | 26.69% | 49.07% | 19.73% | 18.02% | |
| Households reported knowledge of proper net use | Yes | 84.32% | 78.50% | 90.48% | 87.39% |
| No | 12.71% | 21.50% | 9.52% | 12.61% | |
| Households reported using nets for other purposes (fishing, livestock) | Yes | 33.47% | 28.50% | 30.61% | 46.85% |
| No | 63.98% | 71.50% | 69.39% | 53.15% | |
Table 1: Household Demographics and Malaria Tools.
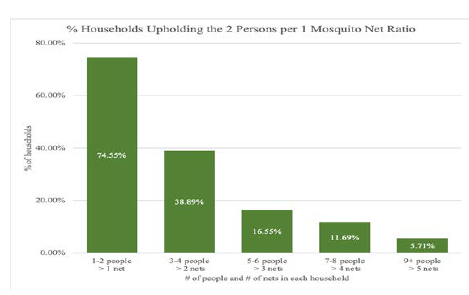
The percentage of households with at least one net for every two people decreased as the number of people in each household increased. While 74.55% of households with 1-2 people had at least one net, only 5.71% of households with over 9 people had at least 5 nets (Figure 1).
Nearly half of all respondents reported using mosquito nets ≥ 5 nights in the preceding week. The highest percentages of consistent net use were found among older individuals, while youth ≥ 10 years of age were the least likely to have consistently slept under a net in the past week. Age (p=0.01) and pregnancy status (p<0.001) were statistically significantly associated with frequency of net use, with people over 60 years old and pregnant women reporting higher usage of mosquito nets (Table 2).
| % of individuals reporting their mosquito net use in the past 7 days | Always (≥ 5 nights) | Sometimes (≤ 4 nights) | Never | Don’t know | P |
|---|---|---|---|---|---|
| Total | 47.20% | 14.19% | 17.83% | 20.78% | |
| Sex | 0.255 | ||||
| Female | 48.95% | 13.95% | 17.58% | 19.51% | |
| Male | 45.26% | 14.48% | 18.12% | 22.13% | |
| Pregnancy Status | 0.01 | ||||
| Pregnant | 59.04% | 11.70% | 15.43% | 13.83% | |
| Not Pregnant | 46.17% | 14.43% | 18.02% | 21.38% | |
| Age | |||||
| 0-10 years old | 44.39% | 14.35% | 19.30% | 21.96% | |
| 11-20 years old | 41.69% | 14.90% | 19.77% | 23.64% | |
| 21-40 years old | 53.51% | 14.05% | 15.50% | 16.94% | |
| 41-60 years old | 56.25% | 12.50% | 13.64% | 17.62% | |
| 61+years old | 61.04% | 10.39% | 11.69% | 16.88% | |
Table 2: Frequency of mosquito net use by Sex, Pregnancy Status, and Age.
93.40% of respondents believed it was “very effective” to use nets to prevent malaria, although 44.70% of respondents believed it was still very likely for a pregnant woman who sleeps under an insecticide treated net (ITN) every night to get malaria. 80.30% of respondents recognized malaria as a serious risk for pregnant women, although commonly cited reasons why pregnant women reported not sleeping under nets were: discomfort from heat (45.78%), inability to get comfortable (34.6%), and inability to breathe as well (14.98%). The most commonly cited reasons why children less than 5 years had difficulty sleeping under nets were: lack of room (37.13%), inability to sleep as well (31.86%), and difficulty with the size and hanging of nets (22.14%) (Table 3).
| Total | ||
|---|---|---|
| Effectiveness of sleeping under a mosquito net to avoid malaria | Very | 93.40% |
| Somewhat | 4.47% | |
| None | 1.91% | |
| Likelihood a pregnant women will get malaria in the next 6 months if they sleep under an ITN every night | Very | 44.70% |
| Somewhat | 12.92% | |
| None | 42.37% | |
| Level of risk if a pregnant person gets malaria | Very | 80.30% |
| Somewhat | 7.84% | |
| None | 11.86% | |
| Advantages of having babies and small children sleep under a mosquito net | Less likely to get malaria | 81.01% |
| Better sleep | 30.17% | |
| Less risk of death | 17.09% | |
| Less risk of anemia or other health effects | 10.55% | |
| Other (i.e. healthier babies) | 6.12% | |
| Advantages of sleeping under a mosquito net while pregnant | Less likely to get malaria | 81.43% |
| Better sleep | 28.90% | |
| Less risk of death | 21.31% | |
| Less risk of early delivery or miscarriage | 24.26% | |
| Other (i.e. healthier babies) | 7.59% | |
| Difficult for babies and small children to sleep under a mosquito net | Can't sleep alone/Not enough room | 37.13% |
| Can’t sleep as well | 31.86% | |
| Difficulty with nets (difficult to hang, too big/small) | 22.14% | |
| Can’t easily touch child | 8.86% | |
| Can't breathe as well | 0% | |
| Too hot | 0% | |
| Other | 10.55% | |
| Difficult for pregnant mothers to sleep under a mosquito net | Can't sleep alone/Not enough room | 0% |
| Can’t sleep as well (can’t get comfortable in one place) | 34.60% | |
| Difficulty with nets (difficult to hang, too big/small) | 8.23% | |
| Can’t see other children | 2.74% | |
| Can't breathe as well | 14.98% | |
| Too hot | 45.78% | |
| Other | 8.02% |
Table 3: Behaviors, knowledge, and attitudes toward malaria and mosquito nets; advantages and difficulties of babies/small children and pregnant women sleeping under mosquito nets.
After adjusting for sex, presence of a pregnant woman, and attitude on net effectiveness, households in Aromo sub-county were 70% more likely to self-report using mosquito nets in the past 7 days than households in Ayami subcounty. Households with pregnant females were more likely to self-report using nets ≥ 5 nights in the preceding week, with their odds increased by 63% compared to households with non-pregnant members. Adjusting for sex, presence of a pregnant woman, and subcounty, households reporting sleeping under nets as being “not effective” were 75% less likely to use nets in the past 7 days compared to those who reported sleeping under nets as being “effective” (Table 4).
| Variables | Self-Reported Mosquito Net Use in Past 7 Days | ||
|---|---|---|---|
| Reference: Self-reported “≥ 5 nights” of net use in past 7 days | |||
| Predictor | OR | P Value | 95% CI |
| Sex | |||
| Female | 1.5 | 0.05 | 0.988-2.24 |
| Pregnant woman in the household | 1.6 | 0.03 | 1.05-2.51 |
| Effectiveness of sleeping under a malaria net (Not Effective) | 0.3 | 0.04 | 0.08-0.9 |
| Subcounty | |||
| Agweng | 1.1 | 0.72 | 0.67-1.78 |
| Aromo | 1.7 | 0.06 | 0.98-2.93 |
| (1) Compared with Males; (2) Compared with Non-Pregnant members of household; (3) Compared with people who reported sleeping under a malaria net is effective; (4) Compared with Ayami subcounty Reported from head of the household |
|||
Table 4: Variables related to net use in past 7 days.
Discussion
The data collected through the YPHA study provide valuable insight into the current status of malaria prevention in three sub counties of Lira District, Uganda. A number of key takeaways emerged from the findings, including the influence of household status on malaria prevention and disease outcomes, the lack of access to and maintenance of LLINs, and the attitudes and behaviors that leave household members at greater risk of malaria infection.
The study found, unsurprisingly, that the vast majority of residents reside in temporary grass huts and rely on subsistence farming from their personal gardens or fields for food, both of which are found to increase exposure to mosquitoes, subsequently increasing risk of malaria infection [13-15]. Low rates of vegetable and fruit consumption also raise concerns regarding malnutrition, which has been linked in various studies to immune dysfunction and malaria severity [16,17]. These findings point to the broader need for socio-economic development, infrastructure investment, and nutrition programs to reduce the prevalence and impact of malaria in the region. The three sub counties are among the most disenfranchised regions of Lira district. Furthermore, the apparent difference in housing, nutrition, household size, pregnancy status, and net use/ knowledge between the three sub counties emphasizes the necessity of sub county specific interventions.
While previous studies have reported that over half of households in the Lango region have at least 1 net for every 2 people [8], the YPHA study found that averages were much lower for households with >3 members and that nearly no households with >9 members had sufficient nets. These large households are likely to house small children and young pregnant women; however, the YPHA data indicate that older occupants in such households are far more likely to be prioritized and sleep under the available nets than younger and more vulnerable occupants. Consequently, the varying net to number of people in the household ratio requires more reflective assessment and highlights the need to target families with children less than 5 years of age and pregnant mothers.
Finally, while the YPHA study findings are consistent with existing data demonstrating greater net use in the Lango region amongst households compared to overall Ugandan averages [8], they also revealed a substantial number of households had defective nets, were unaware of how to properly hang them, or were using them for other purposes than intended. Moreover, while respondents indicated that they believed nets were effective, they were far less confident that net use was sufficient to avoid malaria infection, especially among pregnant women. Consequently, participants may not have believed using nets was worth the reported challenges related to their use, including discomfort and reduced sleep. These findings reinforce the importance of sociological and psychological frameworks of positive norm shaping in influencing malaria preventive behaviors [18], particularly in guiding additional community training to address net use hesitancy and ensure nets are effectively implemented once distributed.
There were a number of limitations to the YPHA study. One primary limitation is potential self-report bias on reporting of key variables such as malaria infection, use of nets for all members of their household, and frequency of insecticide spray. For these reasons, key variables may be over or underreported, and the accuracy of results are limited by recall bias or lack of information. However, utilizing self-reported information gives unique insight into the community perception of the prevalence of malaria. Compared to existing data collected in the 2018-19 Uganda Malaria Indicator Survey (MIS) [8], for example, our surveyed participants had much higher self-reported malaria infection in the past 6 months. This may reflect general confusion about the clinical definition and diagnosis of malaria, as opposed to other illnesses present in the communities. Such confusion is important to recognize, as it could influence the population’s attitudes of both the dangers of malaria and the measures needed to prevent it. As such, the YPHA study findings are valuable in suggesting that barriers to accurate malaria testing, diagnosis, and education force communities to rely on less accurate self-diagnosis methods.
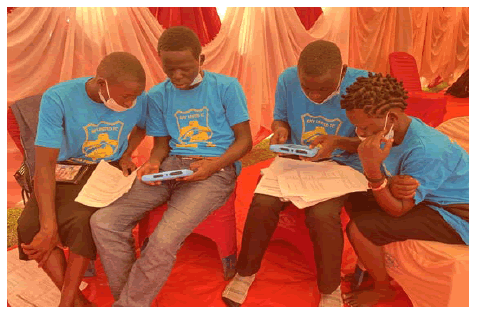
Ultimately, while the study findings represent useful contributions to malaria scholarship and should inform local malaria efforts in the Lira District, the distinguishing feature of this study was its utilization of CBPR approach not commonly used in malaria research. Malaria interventions worldwide remain heavily saturated with hierarchical practices in which external organizations focus on quantity and breadth of reach over understanding the unique needs of communities and engaging in sustainable collaboration. This results in consistently poor outcomes and a lack of overall progress in reducing the burden of malaria in heavily impacted communities. The YPHA programs, alternatively, sought to build on community strengths by democratizing the research process and empowering young leaders to collect, analyze, and share their own community’s attitudes and behaviors (Figures 2 and 3). While community health workers called Village Health Teams (VHTs) already exist as the first level of the health system [19], existing studies indicate how VHTs face difficulties both serving as health workers and making a living for themselves and their families [20,21]. Training youth as public health ambassadors in their communities is an effort to complement and support the work of VHTs who have many existing responsibilities.
Furthermore, the toll of COVID-19 and the recent Ebola outbreak has led global health leaders and Uganda's health minister to emphasize once again the need to invest in health workers and address the health worker shortage [22]. Engaging youth is a concrete step towards inspiring the nation's future generations of health workers, from VHTs to nurses and physicians, to strengthen Uganda's health infrastructure. In alignment with this vision to empower youth, following the collection and analysis of the study data, the YPHA presented their results to their local community leaders, district officials, and the public through in person events, workshops, radio and other media outlets. They also presented their findings and advocated for further investment from members of the Ugandan Parliament, Ministry of Health, and Makerere University School of Public Health (Figures 4 and 5).
The study was made possible by facilitating equitable partnerships in all research phases through long held relationships with the community based organization CCI in northern Uganda, continuous collaboration with local community leaders and youth, support from Ugandan RUFC staff and volunteers, partnership with Peace Corps, input on our study design and implementation from academics well-versed in health equity, and involvement of public health students from Makerere University and the USC GRIT Lab. These partnerships have and will continue to benefit all stakeholders in the future. The success of the partnership, for example, has already resulted in an expanded YPHA-lead community health assessment, including collecting additional data from households, adolescents, schools, and health facilities.
While many organizations may be eager to follow similar community-based practices, utilizing CBPR methods often requires longer investment in time and resources throughout the research and intervention process. In addition, the difficulty of receiving prominent federal grants and publishing peer reviewed studies of geographically limited CBPR studies often disincentivizes traditional academic researchers from initiating such projects. Yet, CBPR should be considered as a critical approach to decolonizing global health practice with the potential to make lasting impacts on community health many times greater than previous research models. More research is needed to evaluate the impact of CBPR studies on participating stakeholders and communities. The YPHA program is currently undergoing an in depth evaluation of its inputs, outputs and outcomes.
Conclusion
The YPHA CBPR study in Lira, Uganda collected valuable data accentuating the high rates of malaria infection and weaknesses in current prevention practices throughout the impacted communities. Amidst many findings, the data pointed to the need for
a) Increased education on prevention pathways, including sanitation and nutrition,
b) Improved access to and use of LLINs, especially in more rural communities and within large multi-generational households
c) Discussion with community members, particularly mothers, on their hesitancies of sleeping under nets when pregnant or of having their children sleep under nets.
Rather than relying on outside researchers and health workers, this study uniquely empowered youth in the community to survey and assess their own community’s needs. The quality of the study results point to the great promise of CBPR in accurately identifying the barriers to effective malaria prevention in specific communities and also in aiding community-driven solutions.
Looking forward, we recommend further research and development of CBPR, particularly in establishing evidence based practices and sharing case studies for CBPR youth empowerment and engagement. CBPR methods provide sustainable and ethical global health practices to pave the way to our future, and these methods will certainly be integral to the final push to eradicate malaria.
Funding
All funding for the study was provided by the non-profit organization Ray United FC.
Conflicts of Interest/Competing Interests
The authors report no competing interests.
Ethics Approval
Ethical approval for the Youth Public Health Ambassador study was received from the Institutional Review Board at the University of Southern California, Gulu University Institutional Review Board, and the Uganda National Council for Science and Technology.
Peace Corps Uganda has a standing Memorandum of Understanding with the Ugandan Ministry of Health, constituting approval of the use of Peace Corps tools.
Consent to Participate
Written consent was received from the youth ambassadors and their parents for their participation in the YPHA program. Written consent was received from the heads of surveyed households.
Consent for Publication
Written consent for publication of data was received from the heads of survey households. Written consent for publication of the youth ambassadors' photographs was obtained.
Availability of Data and Materials
The datasets used and analyzed during the current study are available from the corresponding author on reasonable request.
Acknowledgements
The authors wish to acknowledge Joseph Mwebe from the Peace Corps for his support. The authors would also like to thank the RUFC volunteers and Makerere University students for their contribution in Lira, including Emmanuel Balinda, Ojok Dennis, Kaitesi Allen, Abdul Wagwa, Yesigomwe Kennedy, Amperize Mathias, and Muvunyi Joseph. Finally, the authors would like to thank the public health students from the University of Southern California for their contribution to the study, including Sarah Phillips, Kathy Lam, Maya Spencer, Kayla Samimi, Ally Koh, Samantha Gillis, Kevin Huang, Nicole Malik, Eva Hartman, and Valeria Flores-Cadena.
Authors' Contributions
AJK assisted in the design of the survey instrument, data collection, data analysis, and was a major contributor in writing the manuscript. KG assisted in data analysis and in drafting the final manuscript. PT served as the overall study manager and oversaw design of the survey instrument, participant recruitment, participant training, and data collection. KO led participant recruitment and managed data collection. HW oversaw the development of the survey instrument, data collection, data analysis and the final manuscript. The Lira Youth Public Health Ambassadors were the primary data collectors and findings disseminators.
References
- Yeka A, Gasasira A, Mpimbaza A, Achan J, Nankabirwa J, et al. (2012) Malaria in Uganda: Challenges to control on the long road to elimination: I. Epidemiology and current control efforts. Acta Trop 121: 184-195.
[Crossref] [Google Scholar] [PubMed] [ResearchGate]
- Geneva: World Health Organization (2020) World malaria report: 20 years of global progress and challenges.
- GBD 2019 Diseases and Injuries Collaborators (2020) Global burden of 369 diseases and injuries in 204 countries and territories, 1990-2019: A systematic analysis for the Global Burden of Disease Study 2019. Lancet 396: 1204-1222.
[Crossref] [Google Scholar] [PubMed] [ResearchGate]
- Griffing SM, Tauil PL, Udhayakumar V, Silva-Flannery L (2015) A historical perspective on malaria control in Brazil. Memorias do Instituto Oswaldo Cruz 110: 701-718.
[Crossref] [Google Scholar] [PubMed] [ResearchGate]
- Viswanathan M, Ammerman A, Eng E, Garlehner G, Lohr KN, et al. (2004) Community-based participatory research: Assessing the evidence. Evidence report/technology assessment 99: 1-8.
[Crossref] [Google Scholar] [PubMed] [ResearchGate]
- Israel BA, Eng E, Schulz AJ, Parker EA (2012) Methods for community-based participatory research for Health. (2ndedn), John Wiley & Sons.
- Nasa P, Jain R, Juneja D (2021) Delphi methodology in healthcare research: How to decide its appropriateness. World J Methodol 11: 116-129.
[Crossref] [Google Scholar] [PubMed] [ResearchGate]
- Uganda National Malaria Control Division (NMCD), Uganda Bureau of Statistics (UBOS), and ICF (2020) Uganda Malaria Indicator Survey 2018-19. Kampala, Uganda, and Rockville, Maryland, USA.
- Kigozi SP, Kigozi RN, Sebuguzi CM, Cano J, Rutazaana D, et al. (2020) Spatial-temporal patterns of malaria incidence in Uganda using HMIS data from 2015 to 2019. BMC Public Health 20: 1913.
[Crossref] [Google Scholar] [PubMed] [ResearchGate]
- Peace Corps Uganda (2020) Annual Report: Malaria Net Distribution Form. Peace Corps.
- Qualtrics Inc. (2022) Qualtrics (Version April 2021). Provo (UT): Qualtrics Inc.
- IBM Corp (2022) IBM SPSS Statistics for Windows(Version 27.0) IBM Corps.
- Janko MM, Irish SR, Reich BJ, Peterson M, Doctor SM, et al. (2018) The links between agriculture, Anopheles mosquitoes, and malaria risk in children younger than 5 years in the Democratic Republic of the Congo: A population-based, cross-sectional, spatial study. Lancet Planet Health 2: e74-e82.
[Crossref] [Google Scholar] [PubMed] [ResearchGate]
- Ondiba IM, Oyieke FA, Ong'amo GO, Olumula MM, Nyamongo IK, et al. (2018) Malaria vector abundance is associated with house structures in Baringo County, Kenya. PloS One 13: e0198970.
[Crossref] [Google Scholar] [PubMed] [ResearchGate]
- Kaindoa EW, Finda M, Kiplagat J, Mkandawile G, Nyoni A, et al. (2018) Housing gaps, mosquitoes and public viewpoints: A mixed methods assessment of relationships between house characteristics, malaria vector biting risk and community perspectives in rural Tanzania. Malar J 17: 298.
[Crossref] [Google Scholar] [PubMed] [ResearchGate]
- Das D, Grais RF, Okiro EA, Stepniewska K, Mansoor R, et al. (2018) Complex interactions between malaria and malnutrition: A systematic literature review. BMC Med 16: 186.
[Crossref] [Google Scholar] [PubMed] [ResearchGate]
- Bourke CD, Berkley JA, Prendergast AJ (2016) Immune dysfunction as a cause and consequence of malnutrition. Trends Immunol 37: 386–398.
[Crossref] [Google Scholar] [PubMed] [ResearchGate]
- Perkins JM, Krezanoski P, Takada S, Kakuhikire B, Batwala V, et al. (2019) Social norms, misperceptions, and mosquito net use: A population-based, cross-sectional study in rural Uganda. Malar J 18: 189.
[Crossref] [Google Scholar] [PubMed] [ResearchGate]
- Dowhaniuk N (2021) Exploring country-wide equitable government health care facility access in Uganda. Int J Equity Health 20: 38.
[Crossref] [Google Scholar] [PubMed] [ResearchGate]
- Pandya S, Hamal M, Abuya T, et al. (2022) Understanding Factors That Support Community Health Worker Motivation, Job Satisfaction, and Performance in Three Ugandan Districts: Opportunities for Strengthening Uganda's Community Health Worker Program. Int J Health Policy Manag
[Crossref] [Google Scholar] [PubMed] [ResearchGate]
- Mays DC, O'Neil EJ, Mworozi EA, et al. (2017) Supporting and retaining Village Health Teams: An assessment of a community health worker program in two Ugandan districts. Int J Equity Health 16: 129.
[Crossref] [Google Scholar] [PubMed] [ResearchGate]
- Aceng J, Kerry V, Kyobe HB (2022) Commentary: Uganda urgently needs help to stop the ebola outbreak in its tracks. Fortune.
Citation: Kim AJ, Guy K, Tumuhimbise P, Odur K, Wipfli H, et al. (2023) Community- Based Participatory Research: A Cross-Sectional Study Understanding Malaria in Rural Northern Uganda. J Community Med Health Educ 12:794. DOI: 10.4172/2168-9717.1000794
Copyright: © 2023 Kim AJ. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Select your language of interest to view the total content in your interested language
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 5334
- [From(publication date): 0-2023 - Nov 16, 2025]
- Breakdown by view type
- HTML page views: 4760
- PDF downloads: 574