Pilot Study Open Access
Community-based Health Education to Decrease Pediatric Obesity
Sullivan K and Planas JA*School of Nursing, Fairfield University, USA
- *Corresponding Author:
- Jessica Alicea-Planas
Phd, RN, MPH, School of Nursing
Fairfield University
USA
Tel: 0112032544000
E-mail: jplanas@fairfield.edu
Received date: October 26, 2016; Accepted date: December 06, 2016; Published date: December 16, 2016
Citation: Sullivan K, Planas JA (2016) Community-based Health Education to Decrease Pediatric Obesity. J Community Med Health Educ 6: 489. doi:10.4172/2161-0711.1000489
Copyright: © 2016 Sullivan K, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Community Medicine & Health Education
Abstract
Background: Pediatric obesity is a significant health problem affecting 41 million children under the age of five in the United States, with African-American and Latino children being disproportionately affected. Obesity often leads to chronic disease and has contributed to escalating healthcare expenses in the United States. Early interventions targeted at parents are a piece of the solution to this complex problem.
Methods: This pilot study evaluated the impact of a community-based nutrition education program ("My Plate for My Family, developed by the Supplemental Nutrition Assistance Program) on parents' (N=16) self-efficacy to make healthy choices for their families. An urban preschool in Southwest CT was used as the community partner.
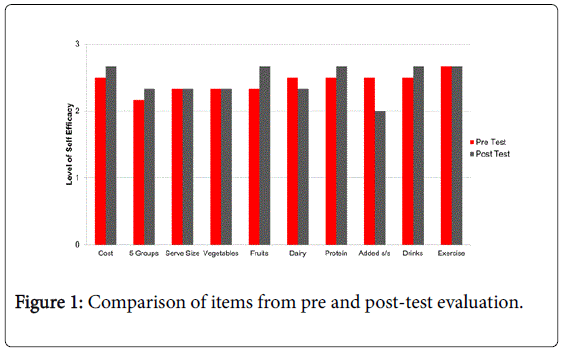
Results: Although there was no statistical difference in the pre and post-test scores, items specific to drinks, fruits and protein, as well as cost, demonstrated small increases in parental self-efficacy.
Conclusions: With the emphasis being placed on including children in the learning process to create healthy lifestyles, implementing community-based health education programs for parents at the child's school seems ideal. Future recommendations would include suggesting health care practitioners consider the advantages of working together with early childhood education centers as strategic partners in the fight against pediatric obesity
Keywords
Pediatric obesity; Nutrition education; Parental involvement; Community-based health education
Introduction
Obesity is a health problem affecting a vast majority of the world��?s population. The World Health Organization [WHO] [1] notes that obesity affects 1.9 billion adults and 41 million children under the age of five worldwide, with the United States being no exception. In fact, within the last thirty years, there has been a two to three-fold increase in pediatric obesity in the U.S. [2] with estimates reporting that the health care system spends $190 billion annually on this issue [3]. Children who are overweight tend to become overweight or obese adults, often leading to chronic health problems that include diabetes, heart disease, asthma and arthritis.
Despite being labeled as one of the most common chronic problems in pediatrics, obesity is preventable and various health care organizations have put forth a call to action to affect the rising rates of obesity. Healthy People 2020 stress the importance of good nutrition, physical activity and healthy body weight, stating that each of these factors is key to maintaining a person��?s health and preventing complications later in life. The Institute of Medicine [IOM], in its early childhood obesity prevention policies, also conveys the need for awareness of the nation��?s nutritional wellbeing and provides guidelines for nutritional intake to achieve adequate nourishment. Moreover, the IOM has made the health and development of youth and families one of their top priorities, highlighting the importance of education regarding health promotion and disease prevention. The Center for Disease Control concurs in its Global Health Strategy, further emphasizing the importance of healthy choice interventions in public health, with a specific focus on underserved communities.
Nearly 1/3rd of children between the ages of 2-19 that live in the United States are overweight or obese, with Hispanics and African Americans comprising 41% of those struggling with this complex disease [4]. Numerous circumstances have been described as contributing to pediatric obesity in the United States including: poor nutrition, a decrease in physical activity with an increase in sedentary lifestyle activities, as well as parental knowledge and living environments [5,6]. Suggested factors associated with increased obesity rates in African- American and Hispanic populations also include lower socioeconomic status, uninsured or underinsured, parent��?s weight status and their perception of being overweight or obese [7]. Research demonstrates that interventions performed in early childhood contribute to the development of healthy lifestyle behaviors that are more likely to be maintained into adulthood [2]. Multicomponent interventions that include nutrition education and physical activity, targeting the entire family have been most successful in decreasing pediatric obesity [8].
Engaging parents, as well as the community, also improves the sustainability of health related education [9]. The literature supports involving parents as active participants in these types of interventions to enhance the level of success [6,10]. The health education provided to parents should be multi-layered. This would include, not only information regarding healthier nutrition choices (such as limits on fast foods, sugary drinks and high fat foods), but also guidance on how to engage children in physical activity (and limit time spent watching TV and playing video games) [11]. Additionally, parents��? beliefs, practices and level of control over a child��?s lifestyle choices is essential [6] and should be considered in health promotion/health education programs.
The purpose of this pilot was to determine if community based health education regarding nutrition and physical activity would enhance a parent��?s self-efficacy to provide improved lifestyle choices for their children. Self-efficacy refers to a person's beliefs in their capability to execute a task in order to reach a specific goal. Bandura��?s [12] Social Cognitive Theory (SCT) has four components including: selfobservation, self-evaluation, self-reaction and self-efficacy. Specific to self-efficacy, Bandura discusses four determinant factors: mastery of experiences, social modeling, social persuasion and psychological responses as integral. Educational interventions, such as the My Plate for My Family, have the ability to influence these factors by providing parents with resources that allow them to be able to model healthier nutritional behaviors for their children. If given the proper tools (i.e. education and skills) to support a healthier lifestyle within their home, parents will gain the confidence to model and eventually master the behaviors for their children. Within the context of health promotion, Bandura��?s SCT emphasizes the importance of interdisciplinary collaboration, more specifically incorporating parents and the community [13]. These concepts guided the design of the study.
Methods
A community-based partnership was developed with a local food bank that was in the process of implementing a program with urban preschools aimed at improving parental knowledge related to nutrition and access to healthier food options. A main objective of the program was to increase the nutritional value of foods available to lower income families. They designed a mobile food truck that traveled to designated preschools twice a month and offered fresh fruits, vegetables and dairy and meat options for participating families. The parents were afforded the opportunity to ��?shop� on the truck after they participated in various nutrition educational sessions that occurred over the course of six months.
Six of the twelve educational sessions were used for this pilot, designed as a four-part interactive educational series. In collaboration with the food truck, the curriculum chosen for the health education component of the intervention was entitled ��?My Plate for My Family� designed by the Supplemental Nutrition Assistance Program [SNAP] and the United States Department of Agriculture (USDA) (available in the public domain). This material was created for use with lowerincome families and aimed to teach the importance of physical activity, encourage parents to eat healthier foods and communicate how parents can engage children through example [14]. One of the program goals was to enhance parental self-efficacy to facilitate healthier choices for them and their families. Providing the participants with various skills (via education and food availability) will contribute to meeting this target. The content of the four health education sessions was as follows:
â�?¢ Session one provided education on the five food groups with an interactive discussion on what specific types of culturally appropriate foods are included in each group, with an emphasis on whole grains and proteins.
â�?¢ Session two included a brief summary of the prior week and a comprehensive discussion of dairy, as well as fats, sugar and sodium. Specific strategies discussing how to limit these items was reviewed. There was also a portion of the class dedicated to teaching parents how to read food labels.
â�?¢ Session three focused on fruits and vegetables, with a review of dairy as reinforcement. This session also incorporated a discussion on appropriate serving sizes for each of the food groups various tools that could be used to gauge proportions.
â�?¢ Session four emphasized physical activity and included an interactive dialogue among participants regarding how they can exercise in various community settings, ways to incorporate activity into their daily routines and how to decrease sedentary lifestyle behaviors.
The health education was provided to parents prior to their entering the mobile food truck. The informed consent form was reviewed with participants and written consent was obtained prior to any data collection. A pre-test was completed prior to session one of the series. The post-test was completed by participants two weeks after session four of the series was offered. Throughout the sessions, participants also received family friendly handouts (available in Spanish and English) containing a review of the topics discussed, as well as recipes to help incorporate what they learned with foods they were receiving from the mobile food truck. Spanish-speaking students from a local university volunteered to assist in interpretation, facilitating for the Spanish speaking parents. Participation in the educational sessions was encouraged but not required, in order for parents to be eligible to access food from the mobile food truck. The study was reviewed and approved by university Institutional Review Board.
The tool used to evaluate self-efficacy was adapted from the Parental Self-efficacy for Enacting Healthy Lifestyles in Children Scale [15] with permission. The original tool measured the self-efficacy of parents with regards to healthy diet and physical activity and had 34 questions (a reliability coefficient of 0.94). Time constraints necessitated that the survey be reduced to ten questions specific to the topics being reviewed in the curriculum. Adaptations for a lower literacy population were done as recommended by D��? Alonzo [16]. Specifically, the self-efficacy scale was adjusted from a ten-point scale to a three-point scale: 1=Not Sure; 2=Somewhat Sure; 3=Very Sure. Although the use of a threepoint scale decreases the variability of responses, it is deemed reliable when evaluating group versus individual data [16]. The adapted tool went through the process of forward and back translation (English- Spanish) as per WHO recommendations.
Participant inclusion criteria were parents or guardians of preschoolers attending the designated site, greater than seventeen years old, gender and ethnicity were nonexclusive. Participant attendance in all six sessions was needed in order to be included in the pre and posttest evaluation. SPSS (v21) was used to perform univariate and bivariate statistics (Figure 1).
Results/Discussion
The original sample consisted of sixteen participants (N=16); two identified as male and fourteen female, ranging in age from 23-44 years old. The self-identified racial and ethnic composition of the participants included eleven Hispanic, two African American, one White and two as other. Eleven of the participants completed the consent and pre-test in Spanish and five in English. The average number of children per household was three, with 50% of the children being under the age of five (Table 1). A total of eight participants (n=8) completed the post-test, with six being able to be paired with the pretest.
| Variable | N(%) | M/Range |
|---|---|---|
| Gender | ||
| Male | 2(12.5) | |
| Female | 14(87.5) | |
| Age | 31/ 23-44 | |
| 18-25 | ||
| 26-35 | 10(62.5) | |
| Over 35 | 3(18.7) | |
| Ethnicity | ||
| Hispanic | 11(68.8) | |
| African American | 2(12.5) | |
| White | 1(6.2) | |
| Other   | 2(12.5) | |
| Language | ||
| English | 5(31.2) | |
| Spanish | 11(68.8) | |
| Number of Children | 3.0/1-5 | |
| 0-5 | 24(50) | |
| 6-10 | 14(29) | |
| Over 11 | 10(21) |
Table 1: Characteristics of participants.
A paired sample t-test was conducted to compare the total selfefficacy score of the participants before and after the intervention. There was no significant difference for pretest results (M=24.16, SD=3.71) compared to post test results (M=24.66, SD=2.5); t (5)=0.406, p>0.05. A pre to post-test analysis of individual questions revealed growth in participant's self-efficacy to provide low cost meals (Q1), provide from the five food groups (Q2), understand the correct amount of fruits/protein (Q5,Q7), and recognize the importance of serving water or fat free milk, instead of juice or soda (Q9). Questions related to physical activity (Q10) daily serving size (Q3) and serving of vegetables (Q4) demonstrated no change in responses pre to post evaluation. There was a reduction in self-efficacy in questions related to daily dairy serving (Q6) as well as added salts and sugars (Q8).
Perceived self-efficacy is considered a significant motivator of behavior change. Bandura conceptualized perceived self-efficacy as perceived operative capability, which centers less on what someone has and more on the belief in what someone can do with the resources one can gather [17]. Fittingly, working with lower-income families, health education focusing on strengthening their self-confidence to model healthy behaviors within the construct of their individual realties is critical. This intervention aimed to provide parents with information that was relatable, using foods that could be found in local grocery stores and discussing common barriers to providing healthy low-cost meal options. Once the information was provided in a way that gave them knowledge of how to share it with their children, analyses was done to see if their overall confidence in modeling these behaviors was increased. While small sample size was a limitation to overall statistical significance, more than half of the items on the pre to post evaluations demonstrated an increase in parental self-efficacy, which is encouraging. Of the more commonly discussed topics, like ��?number of daily servings for vegetables� and ��?physical activity�, it is possible that these areas were already well understood and for this reason there was not an increase in self-efficacy. The items that saw a decrease in selfefficacy were directly related to those topics reviewed in session two. Due to the language barrier it is possible that the use of labels added confusion to the understanding of these concepts.
Limitations
Program evaluation at all sites was completed by the local food bank, in collaboration with a local University. Lack of consistent attendance by participants was a significant limitation at all sites. Inconsistency in levels of attendance inhibited getting a larger sample size for analysis of pre and posttest results, and small sample size should be considered a limitation of this pilot study. Possible reasons for this challenge included the timing of the program (one hour after child drop off at the preschool), compounded by a lack of transportation for participants. It is believed that if the educational component started right at the time of drop off there would have been a larger and more consistent rate of attendance. Additionally, those who chose to accept the benefits of the mobile food truck revealed it was hard to carry all of the items back to their residence after shopping on the truck. Within this urban setting and centralized location, the majority of the parents walk to drop off and pick up their child. Parent work schedules and transportation availability will be considered with future programming.
Conclusions
Early childhood education has been documented to have positive effects on a child��?s life. It is also during these formative years that children learn eating habits that will influence health outcomes for decades after. In order to combat the rising rates of pediatric obesity, targeting a younger population is key. Preschool age children are directly affected by the actions of their parents and thus can learn through health education provided to parents [18]. With the emphasis being placed on including children in the learning process to create healthy lifestyles, implementing a community-based health education programs for parents at the child��?s school seems ideal.
This pilot study reinforced the notion that collaborative health education efforts, between various community partners and early childhood education centers, are possible. Future recommendations would include suggesting health care practitioners consider the advantages of working together with this strategic partner. Increasing enrollment rates for subsequent programs is necessary in order to statistically evaluate the impact of these community partnerships and future iterations of this research might include a parallel group design with both a control and intervention group.
The continual presence of health disparities mandates responsiveness by various sectors that influence health. Collaboration within at risk communities is of utmost importance. Initiating health promotion discussions during early childhood can empower parents to nurture the youth. As the parent��?s understanding of prevention and healthier lifestyles improve, we hope to see a decline in pediatric obesity rates in the future.
References
- World Health Organization (2016) Obesity and overweight.
- Burke RM, Meyer A, Kay C, Allensworth D, Gazmararian JA (2014) A holistic school-based intervention for improving health-related knowledge, body composition, and fitness in elementary school students: An evaluation of the HealthMPowers program. Int J BehavNutrPhys Act 11: 78.
- Cawley J, Meyerhoefer C (2012) The medical care costs of obesity: an instrumental variables approach. J Health Econ 31: 219-230.
- National Institute of Health (2012) Obesity and overweight statistics.
- Faguy K (2016) Obesity in children and adolescents: health effects and imaging implications. RadiolTechnol 87: 279-298.
- Grossklaus H, Marvicsin D (2014) Parenting efficacy and its relationship to the prevention of childhood obesity. PediatrNurs 40: 69-86.
- Figueroa R, Sosa E, Cordova A, Wilmoth S, He M, et al. (2014) Health communication and obesity prevention in Hispanic communities: a qualitative exploration of media��?s roles. J Research Obes 2014: 1-18.
- Coppock JH, Ridolfi DR, Hayes JF, St Paul M, Wilfley DE (2014) Current approaches to the management of pediatric overweight and obesity. Curr Treat Options Cardiovasc Med 16: 343
- Brotman LM, Dawson-McClure S, Huang KY, Theise R, KanboukasD , et al. (2012) Early childhood family intervention and long term obesity prevention among high risk minority. Pediatrics 129: 621-628.
- Jurkowski JM, Lawson HA, Green LL, Wilner PG, Davison KK (2014) The empowerment of low-income parents engaged in a childhood obesity intervention. Fam Community Health 37: 104-118.
- Kelly SA, Melnyk BM (2008) Systematic review of multicomponent interventions with overweight middle adolescents: Implications for clinical practice and research. Worldviews Evid Based Nurs 5: 113-135.
- Bandura A (1977) Social learning theory. Englewood Cliffs NJ Prentice Hall pp: 247.
- Bandura A (1998) Health promotion from the perspective of SCT. Psychol Health 13: 1-33.
- United States Department of Agriculture (2015) Supplemental nutritional education program- education.
- Decker JW (2012) Initial development and testing of a questionnaire of parental self- efficacy for enacting healthy lifestyles in their children. J Spec PediatrNurs 17: 147-158.
- D��?Alonzo KT (2011) Evaluation and revision of questionnaires for use among low-literacy immigrant Latinos. Rev Lat Am Enfermagem 19: 1255-1264.
- Bandura A (2007) Much ado over a faulty conception of perceived self-efficacy grounded in faulty experimentation. J SocClin Psycho 26: 641-658.
- Jang M, Chao A, Whittemore R (2015) Evaluating intervention programs targeting parents to manage overweight and obesity: A systematic review using the Re-aim Figueroa framework. J PediatrNurs 30: 877-887.
Relevant Topics
- Addiction
- Adolescence
- Children Care
- Communicable Diseases
- Community Occupational Medicine
- Disorders and Treatments
- Education
- Infections
- Mental Health Education
- Mortality Rate
- Nutrition Education
- Occupational Therapy Education
- Population Health
- Prevalence
- Sexual Violence
- Social & Preventive Medicine
- Women's Healthcare
Recommended Journals
Article Tools
Article Usage
- Total views: 4303
- [From(publication date):
December-2016 - Apr 07, 2025] - Breakdown by view type
- HTML page views : 3421
- PDF downloads : 882